Summary
Time resolved whole brain CT angiography (4D-CTA) is a novel imaging technology providing information regarding blood flow. One of the factors that influence the diagnostic value of this examination is the temporal resolution, which is affected by the gantry rotation speed during acquisition and the reconstruction interval during post-processing. Post-processing determines the time spacing between two reconstructed volumes and, unlike rotation speed, does not affect radiation burden. The data sets of six patients who underwent a cranial 4D-CTA were used for this study. Raw data was acquired using a 320-slice scanner with a rotation speed of 2 Hz. The arterial to venous passage of an intravenous contrast bolus was captured during a 15 s continuous scan. The raw data was reconstructed using four different reconstruction-intervals: 0.2, 0.3, 0.5 and 1.0 s. The results were rated by two observers using a standardized score sheet. The appearance of each lesion was rated correctly in all readings. Scoring for quality of temporal resolution revealed a stepwise improvement from the 1.0 s interval to the 0.3 s interval, while no discernable improvement was noted between the 0.3 s and 0.2 s interval.
An increase in temporal resolution may improve the diagnostic quality of cranial 4D-CTA. Using a rotation speed of 0.5 s, the optimal reconstruction interval appears to be 0.3 s, beyond which, changes can no longer be discerned.
Key words: multi detector row CT, 4D-CTA, cerebral, vascular
Introduction
A novel technology for imaging blood flow through the cranial blood vessels is time resolved whole brain CT angiography, or 4D-CTA 1-3. 4D-CTA provides a series of angiographic images during the passage of a contrast bolus and shows, in that respect, similarities to conventional catheter angiography 1-3. One of the parameters influencing the diagnostic value of time resolved imaging is its temporal resolution 4. In 4D-CTA, this resolution is determined by a combination of rotation speed and reconstruction interval. The first is a parameter of image acquisition, the second a parameter of image processing. During 4D-CTA imaging, a continuous stream of raw data is acquired using a set rotation speed. Subsequently, this raw data can be processed with varying reconstruction intervals, defined as the amount of time spacing between two reconstructed volumes. Therefore, changing the reconstruction interval does not affect radiation burden, as opposed to changing rotation speed.
The clinical use of 4D-CTA to depict the intracranial circulation continues to increase, and recent studies show promising results regarding the value of 4D-CTA in the diagnostic work-up of intracranial arteriovenous shunting lesions 5,6. However, to our knowledge, the optimal 4D-CTA reconstruction interval has not yet been assessed for any given rotation speed. We expect the smallest reconstruction interval to show most detail with regards to blood flow characteristics. This is especially important when assessing high-flow lesions such as arteriovenous malformations (AVMs) or dural arteriovenous fistulas (dAVFs). Although decreasing the reconstruction interval does not significantly increase post-processing time, it does come at higher computational and storage costs. Furthermore, since reconstructions are based on a limited amount of raw data, the positive effect of lowering the reconstruction interval may show a plateau at some stage. This study aims to find the optimal reconstruction interval using a rotation speed of 0.5 s, which is the rotation speed currently used in our clinical protocols.
Materials and Methods
The raw data were retrospectively collected from six patients who underwent 4D-CTA of the cranial blood vessels, using the Aquilion One 320-slice CT system (Toshiba Medical Systems). Raw data acquisition consisted of 15 s of continuous scanning with a rotation speed of 0.5 s and 80 kV, 240 mA tube settings. Under these conditions the arterial to venous passage of an intravenous contrast bolus was captured. Patients were diagnosed to harbour a dural arteriovenous fistula (high-flow dAVF, two cases), an arteriovenous malformation (high-flow AVM, two cases) or neither (two cases).
The raw data was processed four times, using pre-determined reconstruction-intervals of 0.2 s, 0.3 s, 0.5 s and 1.0 s. For each reconstruction interval, time resolved maximum intensity projection (MIP) runs were generated in lateral and anterior-posterior (AP) views, in accordance with the clinical imaging protocol used at our institution. The reconstructions were anonymized and rated by two blinded observers. Both observers frequently use 4D-CTA images in a clinical setting, one as a neurosurgeon and neuro-interventionalist (PWAW) and one as a radiologist and fellow neuro-interventionalist (BS).
The reconstructions were rated using a scoring sheet consisting of two parts. In the first part, the observers recorded whether an AVM or dAVF could be detected. If one of these was detected, it was subsequently rated using the Spetzler-Martin and Borden classifications, respectively 7,8. In the second part of the score sheet, the observers compared all four data sets of a single patient and graded the temporal resolution from 1 to 10, with 10 being the highest identifiable temporal resolution (Figure 1). The observers were requested not to assign the same grade twice within one patient. This grading was designed to find a preference for a certain reconstruction interval based on the ability to evaluate flow characteristics, e.g. flow direction in different vessel segments.
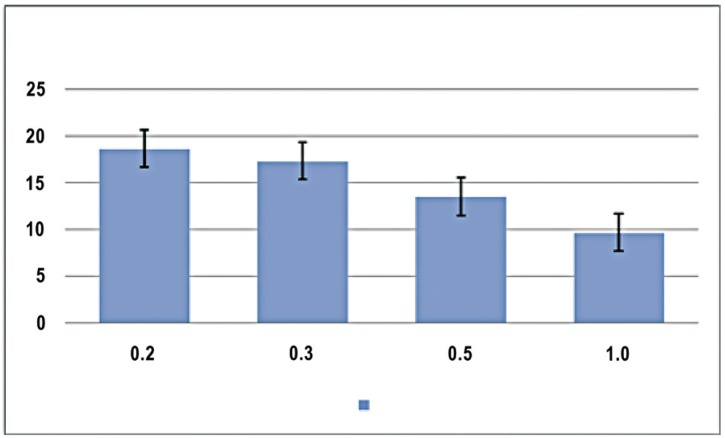
Figure 1.
Total temporal resolution score for each reconstruction interval. The Figure shows the total amount of points awarded by both readers to each reconstruction interval with respect to temporal resolution. It indicates that temporal resolution is inversely proportional to the reconstruction interval, with the largest improvement gained between the 1.0 s, 0.5 s and 0.3 s reconstruction intervals. The improvement gained between the 0.3 s and 0.2 s is substantially smaller and was judged too subtle to be clinically relevant by both readers.
Results
With regard to lesion detection, both observers detected all AVMs and dAVFs correctly in all reconstructions, regardless of the reconstruction interval. The same was true for the respective classifications.
With regard to temporal resolution grading, both observers gave highest grades to the 0.2 s reconstruction in all cases. The average score for this reconstruction interval was 9.25. Reconstructions made with an interval of 0.3 s were graded with an average score of 8.75, indicating only a small difference between the 0.2 and 0.3 s reconstruction intervals. The reconstructions with an interval of 0.5 and 1.0 s were rated much lower, with an average score of 6.75 and 4.83, respectively.
Discussion
During the acquisition of a 4D-CTA data set, there is a three-way trade-off between signal-to-noise ratio, radiation burden and gantry rotation speed. The latter determines, to some extent, the temporal resolution. However, during post-processing, the acquired data may be reconstructed at different reconstruction intervals to optimize the perceived temporal resolution.
This study aimed to find an optimal reconstruction interval in the post-processing of 4D-CTA data sets, acquired with a rotation speed of 0.5 seconds. All data sets were found to be sufficient for accurate diagnosis and grading in the six patients used for this analysis. Subjective grading of the temporal resolution was found to be inversely proportional to the reconstruction interval, as was expected. However, the difference between 0.2 s and 0.3 s intervals was judged to be too subtle to be of clinical relevance.
A drawback of this study was the inability to adequately blind the readers for the reconstruction interval, since lower reconstruction intervals yield reconstructed volumes containing more images. Another drawback was our current computational limit. A reconstruction interval of 0.2 s would yield a volume set of 75 images. However, our current software only allows volumes with a maximum of 50 images to be created, which resulted in the loss of part of the venous phase during image evaluation. Both observers experienced this to be a serious limitation. When choosing post-processing parameters, computational and storage costs (and limitations) need to be weighed against diagnostic benefit. Although all six tested datasets were diagnostically accurate, it is possible that more subtle lesions would have benefitted from the increase in temporal resolution with smaller reconstruction intervals. Larger numbers of cases will be needed to assess the full diagnostic potential of 4D-CTA in the diagnostic work-up of patients with arteriovenous shunting lesions 5,6. The aim of this study was limited to finding the optimal reconstruction interval for our current acquisition protocol, and the marked consistency in the results does enable conclusions in that regard. Given the fact that the difference between 0.2 s and 0.3 s intervals was extremely subtle and the 0.2 s interval resulted in the loss of part of the venous phase due to storage limitations, our results clearly favour a 0.3 s reconstruction interval.
Conclusions
Increasing temporal resolution may improve the diagnostic quality of 4D-CTA of the brain. Using a rotation speed of 0.5 seconds, the optimal reconstruction interval was found at 0.3 s, beyond which changes were no longer clearly discernable.
References
- 1.Siebert E, Bohner G, Masuhr F, et al. Neuroimaging by 320-row CT: is there a diagnostic benefit or is it just another scanner? A retrospective evaluation of 60 consecutive acute neurological patients. Neurological Sci. 2010;31:1–9. doi: 10.1007/s10072-010-0292-7. [DOI] [PubMed] [Google Scholar]
- 2.Siebert E, Bohner G, Dewey M, et al. 320-slice CT neuroimaging: initial clinical experience and image quality evaluation. Br J Radiol. 2009;82:561. doi: 10.1259/bjr/27721218. [DOI] [PubMed] [Google Scholar]
- 3.Brouwer P, Bosman T, Van Walderveen M, et al. Dynamic 320-section CT angiography in cranial arteriovenous shunting lesions. Am J Neuroradiol. 2010;31:767. doi: 10.3174/ajnr.A1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mutaf YD, Brinkmann DH. An investigation of temporal resolution parameters in cine-mode four-dimensional computed tomography acquisition. J App Clin Med Phys. 2008;9:2819. doi: 10.1120/jacmp.v9i4.2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Willems PWA, Brouwer PA, Barfett JJ, et al. Detection and classification of cranial dural arteriovenous fistulas using 4D-CTA. Initial experience. Am J Neuroradiol. 2010;31:49–53. doi: 10.3174/ajnr.A2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Willems PWA, Taeshineetanakul P, Schenk B, et al. The use of 4D-CTA in the diagnostic work-up of brain arteriovenous malformations. Neuroradiology. 2012;54:123–131. doi: 10.1007/s00234-011-0864-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986;65:476–483. doi: 10.3171/jns.1986.65.4.0476. [DOI] [PubMed] [Google Scholar]
- 8.Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. Neurosurg. 1995;82:166–179. doi: 10.3171/jns.1995.82.2.0166. [DOI] [PubMed] [Google Scholar]