Abstract
Purpose
To compare quality of life (QOL) in myopic patients who underwent photorefractive keratectomy (PRK) with that of myopic spectacle or contact lens users.
Methods
This observational comparative study was performed on 102 low to moderate myopic patients who had undergone PRK at least 6 months ago and 106 myopic spectacle or contact lens wearers. Vision related QOL and its correlation with demographic variables, visual acuity and refractive status were compared between the two groups. QOL was measured using a validated translated version of the Visual Function Questionnaire (VFQ-25) which contains 25 questions in 12 subscales with a total score of zero to 100.
Results
Mean total QOL score was 97.0±4.4 and 86.1±10.7 in PRK and nonsurgical groups respectively [mean difference (d)=11, P<0.001]. The difference was independent of age, sex, education or marital status (P>0.05). Overall, 10 out of 12 QOL subscales were significantly higher in the PRK group (P<0.001) especially general vision (d=23.8), general health (d=22.2), driving (d=19.3), role difficulties (d=14.6), distance activities (d=13.8) and mental health (d=13.7). Only color vision (d=1.6, P>0.9) and ocular pain (d=3.1, P=0.3) were not significantly different between the study groups.
Conclusion
Correction of myopia using PRK is associated with higher QOL scores in most subscales as compared to spectacle or contact lens wear.
Keywords: Quality of Life, Myopia, Refractive Surgical Procedures
INTRODUCTION
Uncorrected refractive errors are the main cause of low vision and the second cause of blindness worldwide,1 and can adversely impact quality of life (QOL).2Correction of refractive errors using spectacles is among the most cost-effective interventions.1On the other hand, refractive surgery is getting more popular as a safe and effective procedure such that it has become the most common elective surgical procedure worldwide.3
The role of laser in situ keratomileusis (LASIK) in the improvement of vision related QOL has been discussed in some studies mainly in developed countries.4-6Few researchers even argue that correction of myopia with contact lens or spectacles has a negative impact on QOL as compared to refractive surgery.7Photorefractive keratectomy (PRK) is currently the most commonly performed type of refractive surgery in Iran because it provides slightly better visual outcomes than other types of refractive surgery in low to moderate myopia.8Considering the increasing rate of refractive procedures, it is important to know whether they are a good substitute for non-surgical methods (glasses/contact lenses), and how they affect QOL, visual problems and life stresses.
This study was performed to compare QOL in myopic patients after PRK vs non-surgical methods of optical correction.
METHODS
This observational comparative study was performed on a consecutive sample of myopic patients with low to moderate myopia who were referred to a private eye clinic in Tehran from December 2009 to May 2010. The study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences and informed consent was obtained from all patients before enrollment in the study. Patients were 15 to 45 years of age. Subjects with any eye disease other than refractive errors, history of any ocular surgery and those with systemic disease that may affect vision such as diabetes mellitus or collagen vascular disease were excluded. Patients who underwent PRK by the same surgeon (HZ) at least 6 months ago were compared with an age-matched group of patients who used glasses or contact lenses.
Data collection was performed using the translated Persian version of the Visual Function Questionnaire (VFQ-25)9which has been developed and validated by standard methods including forward translation, back translation, evaluation of translation quality by bilingual speakers, and a pilot test.
The VFQ-25 contains 25 questions evaluating 12 main subscales of QOL including general health, general vision, ocular pain, near vision, distance vision, social function, mental health, role difficulty, dependency, driving, color vision and peripheral vision. Each question has multiple choices, which are scored on a five- or six-point Likert scale where higher scores represent better function. Each item is then converted into a 0 to 100 scale such that the lowest and highest possible scores are set at 0 and 100 points, respectively. Finally, items within the same subscale are averaged together to create the subscale score. Mean scores of all subscales is considered as the total QOL score.
The questionnaire was self-administered and a trained interviewer was available to provide explanations as required. However, the interviewers had no direct involvement in the medical care of patients. Demographic and eye examination data including uncorrected visual acuity (UCVA) and spherical equivalent (SE) were recorded. In the PRK group, preoperative visual acuity and SE were retrieved from the medical files.
Data analysis was performed using SPSS software version 17. Univariate statistical tests (Spearman Correlation, Mann-Whitney U and Kruskal-Wallis tests) were used to demonstrate the effect of demographic variables (age, sex, education, and marital status) on QOL. A general linear model adjusted for demographic characteristics was employed to evaluate the effect of PRK on total QOL score as compared to spectacles/contact lens correction of myopia. In addition Mann-Whitney test was used to compare different QOL subscales between the two groups. Significance level was set at P<0.05. Cronbach's alpha was used to assess internal consistency of questions in each subscale.
RESULTS
The study subjects included 102 patients in the PRK group and 106 patients in the spectacles/contact lens group. Overall, mean age of patients enrolled in the study was 28.4±6.8 (range: 15-45) years and 65.4% of subjects were female. Table 1compares the study groups in terms of demographic data, visual acuity and refractive status. The study groups were comparable in terms of age and marital status but sex, education level and visual status were significantly different between the two groups; the proportion of women and level of education were considerably higher, but baseline VA and SE were worse in the PRK group.
Table 1.
Comparison of baseline characteristics of the study groups
| Parameter | Total | Group | P-value | ||
|---|---|---|---|---|---|
| Specs/CL | PRK | ||||
| Age (years)* | 28.4±6.8 | 28.2±7.3 | 28.6±6.2 | 0.44 | |
| Sex | |||||
| female | 139 (66) | 60(56) | 79(75) | 0.001 | |
| male | 73(34) | 47(44) | 26(25) | ||
| Marital Status | |||||
| single | 103 (49) | 57(54) | 46(44) | 0.17 | |
| married | 95(45) | 42(40) | 53(51) | ||
| divorced | 11(5) | 6(6) | 5(5) | ||
| widowed | 0(0) | 0(0) | 0(0) | ||
| Education | |||||
| none | 0(0) | 0(0) | 0(0) | 0.041 | |
| elementary | 1(0) | 1(1) | 0(0) | ||
| secondary | 3(1) | 2(2) | 1(1) | ||
| high school | 83(40) | 49(47) | 34(34) | ||
| academic | 118 (58) | 53(50) | 65(65) | ||
| SE (diopters) | |||||
| two eyes | -2.79±1.66 | -2.36±1.61 | -3.3±1.57 | <0.001 | |
| better eye | -2.59±1.64 | -2.13±1.58 | -3.13±1.54 | <0.001 | |
| VA (LogMAR) | |||||
| two eyes | 0.02±0.07 | 0.03±0.1 | 0±0.01 | 0.072 | |
| better eye | 0±0.04 | 0.01±0.05 | 0±0.03 | 0.007 | |
SE, spherical equivalent; VA, visual acuity; Specs/CL, spectacles and contact lenses; PRK, photorefractive keratectomy.
Mean±standard deviation
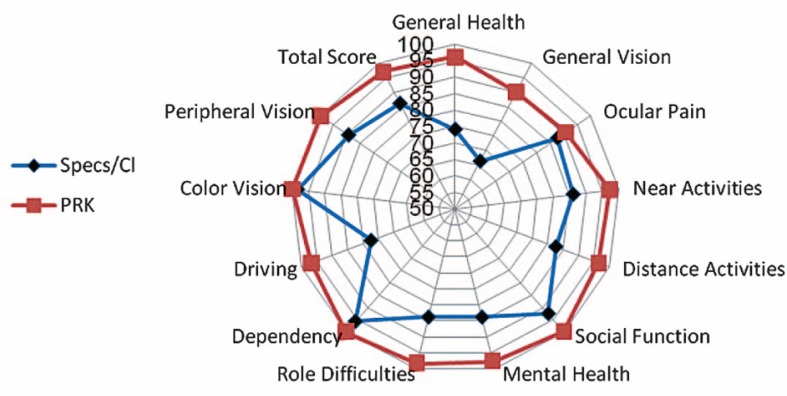
In all subscales, higher QOL scores were achieved in the PRK group (Table 2and Fig. 1). The greatest mean difference (d) in QOL subscales between the two groups were related to general vision (d=23.8), general health (d=22.2), driving (d=19.3), role difficulties (d=14.6), distance activities (d=13.8) and mental health (d=13.7). On the contrary, color vision (d=1.6, P>0.9) and ocular pain (d=3.1, P=0.3) were not significantly different between the study groups.
Table 2.
Quality of life scores in the study groups
| Subscales | Study groups (Mean±SD) | Difference | P-value | ||
|---|---|---|---|---|---|
| PRK (n=114) | Specs/CL (n=114) | Mean | (95% CI) | ||
| General Health | 96.2±12 | 74.1±24.4 | 22.2 | 17 to27.4 | <0.001 |
| General Vision | 90.1±17.3 | 66.3±23.2 | 23.8 | 18.2 to 29.4 | <0.001 |
| Ocular Pain | 90.9±13.3 | 87.8±17.6 | 3.1 | -1.2 to 7.4 | 0. 35 |
| Near Activities | 97.4±9.4 | 86.1±13.5 | 11.3 | 8.2 to14.5 | <0.001 |
| Distance Activities | 96.6±7.5 | 82.7±15 | 13.8 | 10.6 to 17.1 | <0.001 |
| Social Function | 99.9±0 | 92.7±15.6 | 7.2 | 4.2 to 10.2 | <0.001 |
| Mental Health | 97.7±5.4 | 84±16.3 | 13.7 | 10.4 to 17 | <0.001 |
| Role Difficulties | 98.5±4.1 | 84±20.5 | 14.6 | 10.5 to 18.6 | <0.001 |
| Dependency | 100±0 | 95.8±11.9 | 4.2 | 1.9 to 6.4 | <0.001 |
| Driving | 96.7±13.2 | 77.4±21.9 | 19.3 | 13.5 to 25.1 | <0.001 |
| Color Vision | 99.9±0 | 98.3±7.1 | 1.6 | -0.2 to -0.3 | >0.99 |
| Peripheral Vision | 99.6±3.3 | 89.4±16.9 | 10.1 | 6.8 to 13.5 | <0.001 |
| Total Score | 97±4.4 | 86.1±10.7 | 11 | 8.7 to 13.2 | <0.001 |
SD, standard deviation; PRK, photorefractive keratectomy; Specs/CL, spectacles and contact lenses; CI, confidence interval
Figure 1.
Comparison of quality of life subscales among the study groups. Specs/CL, spectacles and contact lens; PRK, photorefractive keratectomy
The internal consistency of the VFQ-25 questionnaire was calculated for each subscale (Table 3) and an acceptable Cronbach's alpha value was achieved for most subscales.
Table 3.
Internal consistency of the Persian VFQ-25 questionnaire in myopic patients
| Item | Number of Item | Cronbach Alpha % |
|---|---|---|
| General Health | 1 | - |
| General Vision | 1 | - |
| Ocular Pain | 2 | 72.1 |
| Near Activities | 3 | 65.9 |
| Distance Activities | 3 | 58.0 |
| Social Function | 2 | 80.4 |
| Mental Health | 4 | 74.2 |
| Role Difficulties | 2 | 83.6 |
| Dependency | 3 | 82.9 |
| Driving | 3 | 85.3 |
| Color Vision | 1 | - |
| Peripheral Vision | 1 | - |
| Total Score | 25 | 89.3 |
Using a general linear model adjusted for demographic variables and baseline visual status (Table 4), we found that the PRK group enjoyed a 11.2 point higher total QOL score (95% confidence interval, 8.1-14.3; P<0.001). As shown in table 4, demographic data had no correlation with total QOL score in univariate and adjusted multivariate analysis except for the level of education such that QOL was 3.3 scores higher in patients who had academic education, but there was no significant difference between patients with academic and non-academic educational levels after adjusting for other characteristics.
Table 4.
Relationship between demographic variables and total quality of life scores
| Univariate | Multiple Regression | |||||
|---|---|---|---|---|---|---|
| B | 95% CI | P | B | 95% CI | P | |
| Group | ||||||
| PRK | Ref | Ref | ||||
| Specs/CL | -11.0 | -13.2 to -8.7 | <0.001 | -11.2 | -14.3 to -8.1 | < 0.001 |
| Age | ||||||
| 10 years | -0.6 | -2.4 to 1.2 | 0.493 | -0.1 | -0.4 to 0.2 | 0.54 |
| Sex | ||||||
| M | Ref | Ref | ||||
| F | 1.0 | -1.9 to 3.8 | 0.5 | -1.0 | -4.1 to 2.1 | 0.52 |
| Education | ||||||
| Non-academic | Ref | Ref | ||||
| Academic | 3.3 | 0.6 to 6 | 0.018 | 1.7 | -1.4 to 4.8 | 0.28 |
| Marital status | ||||||
| Single | Ref | Ref | ||||
| Married | 0.4 | 0.1 to 1 | 0.796 | -0.3 | -4 to 3.3 | 0.85 |
| Divorced | 3.2 | 1 to 1 | 0.311 | 2.7 | -5.2 to 10.6 | 0.50 |
| SE in better eye | 0.0 | -0.9 to 1 | 0.922 | 1.3 | 0.4 to 2.2 | 0.006 |
| VA in better eye | -4.3 | -8.3 to -0.4 | 0.033 | -2.0 | -2.9 to -1.1 | 0.041 |
PRK, photorefractive keratectomy; Specs/CL, spectacles and contact lenses; M, male; F, female; P, P-value; SE, spherical equivalent; VA, visual acuity; B, regression coefficient; Ref, reference group or the group against which the comparison is being made; CI, confidence interval
We also compared baseline UCVA and SE in the better eye of all patients in this adjusted general linear model; total QOL score was improved by 2 units for each 1 line increase in VA, and 1.3 units for each 1 diopter decrease in SE.
DISCUSSION
Refractive surgery decreases dependence on glasses and contact lenses; it is a successful method due to the comfort and good UCVA achieved after surgery, and the low rate of side effects.3In this study, mean total QOL was 11 scores higher in patients who had undergone PRK as compared to spectacle or contact lens wearers (P<0.001). Furthermore, the Persian version of the VFQ-25 had acceptable internal consistency as observed in this study.
In previous studies, improvement in vision related QOL after refractive surgery was mostly attributed to psychological and social aspects rather than visual function.4-6Awwad et al4showed a significant improvement in psychological well-being and social role three months after wave front-guided LASIK surgery for myopia whereas visual function remained unchanged. In another prospective study, visual function scores remained almost unchanged after conventional LASIK, while QOL subscales related to cost, safety, appearance and convenience showed considerable improvement.5Nevertheless, sample size in these two studies (30 and 66 patients, respectively) may be insufficient to reveal changes in visual function. After three months of follow-up in 204 patients (and 171 patients for 6 months) who underwent LASIK, Lee et al6reported a significant improvement in visual function and symptoms as well as social and psychological aspects. In the current study, higher scores were achieved in PRK groups in all QOL subscales except for ocular pain and color vision. We detected larger differences between the two groups in general vision and health, driving, role difficulties, mental health and distance activities (Table 2).
Mean age and marital status were comparable between the study groups, however, other demographic variables, baseline visual status and refraction were different (Table 1). For managing these differences, we performed multivariate analysis (Table 4) which allowed us to attribute differences in QOL to the method of myopia correction. The higher number of women in the current study is justified by more demand by women for refractive surgery in our community which is in line with other studies which enrolled consecutive samples of refractive surgery candidates.5-7Nevertheless, in our study, gender had no effect on vision-related QOL and the total QOL score was not different between male and female subjects.
We used the Persian version of the VFQ-259whose psychometric properties have been verified for some other versions.10-12This questionnaire is designed to measure the influence of various eye diseases and interventions on QOL and is sensitive to refractive errors. Although, patient satisfaction and improvement of QOL after LASIK have been discussed in previous studies,3-7few studies have specifically been conducted on the outcomes of PRK which has gained more popularity in recent years.8An acceptable sample of PRK patients and comparison with a matched group of spectacle or contact lens wearers not contemplating refractive surgery differentiates our study from its previous counterparts, especially considering the paucity of data in this field in developing countries.
The effect of refractive surgery on vision related QOL has been measured using a variety of questionnaires and methods.3-7 Some studies reported improvement of QOL only in one group of patients before and after refractive surgery,4-6while others compared the results within a group of patients who also used glasses or contact lenses.5,7As the questionnaire and scoring methods are different, there is limited capacity for direct comparison of the numerical amount of QOL improvement among different studies. Additionally, equal numerical weights are assigned to ranked scores in Likert-scaled questionnaires and the same responses to different questions are assumed to be similar. For instance, if patients report a "little difficulty" for both near vision and driving subscales, these subscales will gain the same numerical value which may not be logically valid5. Such limitations may be important for interpreting the results of our study and similar studies in this field.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86:63–70. doi: 10.2471/BLT.07.041210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Broman AT, Munoz B, Rodriguez J, Sanchez R, Quigley HA, Klein R, et al. The impact of visual impairment and eye disease on vision-related quality of life in a Mexican-American population: proyecto VER. Invest Ophthalmol Vis Sci. 2002;43:3393–3398. [PubMed] [Google Scholar]
- 3.Solomon KD, Fernández de, Sandoval HP, Biber JM, Groat B, Neff KD, et al. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009;116:691–701. doi: 10.1016/j.ophtha.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 4.Awwad ST, Alvarez-Chedzoy N, Bowman RW, Cavanagh HD, McCulley JP. Quality of life changes after myopic wavefront-guided laser in situ keratomileusis. Eye Contact Lens. 2009;35:128–132. doi: 10.1097/ICL.0b013e3181a142e5. [DOI] [PubMed] [Google Scholar]
- 5.Garamendi E, Pesudovs K, Elliott DB. Changes in quality of life after laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2005;31:1537–1543. doi: 10.1016/j.jcrs.2004.12.059. [DOI] [PubMed] [Google Scholar]
- 6.Lee J, Lee J, Park K, Cho W, Kim JY, Kang HY. Assessing the value of laser in situ keratomileusis by patient-reported outcomes using quality of life assessment. J Refract Surg. 2005;21:59–71. doi: 10.3928/1081-597X-20050101-12. [DOI] [PubMed] [Google Scholar]
- 7.Chen CY, Keeffe JE, Garoufalis P, Islam FM, Dirani M, Couper TA, et al. Vision-related quality of life comparison for emmetropes, myopes after refractive surgery, and myopes wearing spectacles or contact lenses. J Refract Surg. 2007;23:752–759. doi: 10.3928/1081-597X-20071001-04. [DOI] [PubMed] [Google Scholar]
- 8.Ghadhfan F, Al-Rajhi A, Wagoner MD. Laser in situ keratomileusis versus surface ablation: visual outcomes and complications. J Cataract Refract Surg. 2007;33:2041–2048. doi: 10.1016/j.jcrs.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 9.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119:1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 10.Suzukamo Y, Oshika T, Yuzawa M, Tokuda Y, Tomidokoro A, Oki K, et al. Psychometric properties of the 25-item National Eye Institute Visual Function Questionnaire (NEI VFQ-25), Japanese version. Health Qual Life Outcomes. 2005;3:65. doi: 10.1186/1477-7525-3-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Toprak AB, Eser E, Guler C, Baser FE, Mayali H. Cross-validation of the Turkish version of the 25-item National Eye Institute Visual Functioning Questionnaire (NEI-VFQ 25). Ophthalmic Epidemiol. 2005;12:259–269. doi: 10.1080/09286580590967763. [DOI] [PubMed] [Google Scholar]
- 12.Baker RS, Bazargan M, Calderón JL, Hays RD. Psychometric performance of the National Eye Institute visual function questionnaire in Latinos and non-Latinos. Ophthalmology. 2006;113:1363–1371. doi: 10.1016/j.ophtha.2006.01.073. [DOI] [PubMed] [Google Scholar]