Abstract
Purpose
To report normal interpupillary distance (IPD) values in different age groups of an Iranian population.
Methods
This study was performed on 1,500 randomly selected subjects from 3,260 consecutive out-patients with refractive errors referred to Farabi Eye Hospital, Isfahan, Iran over a period of two years (2008 to 2010). Measurement of refractive errors and IPD for far distance were performed using an autorefractometer (RMA-3000 autorefractometer, Topcon, Tokyo, Japan).
Results
Mean IPD in adult subjects was 61.1±3.5 mm in women and 63.6±3.9 mm in men (p<0.001). Mean IPD increased 4.8 mm during the second decade, 1.7 mm during the third decade, and 0.6 mm during the fourth and fifth decades of life.
Conclusion
The observed increase in IPD after the age of 30 years indicates that factors other than skeletal growth may affect this parameter.
Keywords: Interpupillary Distance, Refractive Error, Age, Iran
INTRODUCTION
Interpupillary distance (IPD) is the distance between the center of the pupils. It determines the degree of retinal image disparity in fellow eyes which are combined in the brain to produce stereo perception. Knowledge of a given population’s mean IPD is important in the design of stereoscopic displaying devices and the production of stereoscopic content. Awareness of variations and extremes of IPD among the population is also of great importance in this regard. It has proven remarkably difficult to obtain scientific evidence on variations in IPD.1 Familiarity with normal IPD values in population subgroups can help studies on orbitocranial growth patterns, diagnosis of syndromes, surgical management of craniofacial deformities and trauma, and manufacturing of spectacles.2,3 There are several studies on IPD values in different racial groups,1-4 however no study has been reported from Iran. The aim of this study was to define normal IPD values in different age groups of an Iranian population.
METHODS
This cross-sectional study was performed on 3,260 consecutive out-patients with refractive errors who had been referred to Farabi Eye Hospital (Isfahan, Iran) over a period of two years from 2008 to 2010. Two-hundred and sixty cases were excluded from the study as a result of ophthalmologic problems. The remaining 3,000 patients were repeatedly labeled as A and B in the same order as their referral. The A-code group (1,500 patients) was enrolled in the analysis.
All subjects underwent measurement of refractive errors and distance IPD using an objective autorefractometer (RMA-3000 autorefractometer, Topcon, Tokyo, Japan). Two-hundred and sixty patients were excluded because of media opacity, history of ocular trauma or surgery, congenital craniofacial maldevelopment, poor cooperation or problems in autorefractometery. Data collection and statistical analysis was performed on 1,500 cases who were randomly selected from the study population.
Distance IPD and refraction for both eyes were measured using the autorefractometer while the subject was seated comfortably, and his/her forehead and chin were positioned correctly in the instrument. The measurement was repeated if the patient moved his/her head or eyes.
SPSS software (version 16) was used for statistical analyses. Differences between mean values were tested using the t-test with significance level set at P<0.05.
RESULTS
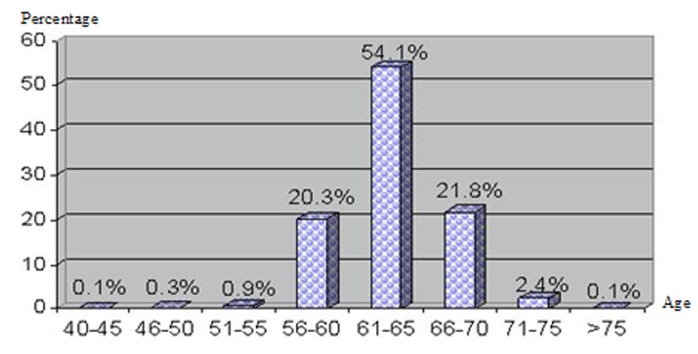
Out of 1,500 studied individuals, 910 (60.7%) subjects were female and 590 (39.3%) were male with mean age of 48.3 years (range, 5-80); 947 subjects (63.1%) were adults over 19 years of age. Mean IPD in adults was 62.1±3.7 (range, 42-75) mm overall; 61.1±3.5 mm in women and 63.6±3.9 mm in men (P<0.001, Fig. 1). IPD showed an increase with age (Table 1) such that mean IPD was 4.8 mm larger in the second decade (P<0.001), 1.7 mm higher in the third decade (P<0.001), and 0.6 mm larger in the fourth and fifth decades of life (P<0.03). In addition, mean IPD was 1 mm higher after the age of 50 years as compared to the 30-50 year age group (P<0.001). IPD ranged from 42 to 75 mm in adults; IPD of 60 to 62 mm included 37.8%, and IPD of 60 to 65 mm included 54.1% of adult subjects.
Figure 1.
Frequency distribution of patients above 40 years of age.
Table 1.
Interpupillary distance (mm) values in various age groups
| Age (yr) | Female | Male | Total | Range |
|---|---|---|---|---|
| 5-9 | 55.08±4.6 | 54.76±2.8 | 54.94±3.9 | 44-74 |
| 10-19 | 59.42±3.6 | 60.30±3.8 | 59.75±3.7 | 38-73 |
| 20-29 | 60.65±3.5 | 63.15±3.3 | 61.48±3.6 | 42-72 |
| 30-50 | 61.16±3.2 | 63.46±3.3 | 62.07±3.5 | 52-75 |
| >50 | 62.04±4.1 | 64.18±4.6 | 63.10±4.4 | 46-74 |
| >19 (Adult) | 61.13±3.5 | 63.58±3.9 | 62.10±3.7 | 42-75 |
| Total | 60.17±4.0 | 61.83±4.6 | 60.82±4.3 | 38-75 |
DISCUSSION
Knowledge of normal IPD values is important in the diagnosis and treatment of congenital orbital or craniofacial anomalies and post-traumatic deformities as well as for proper mounting of spectacle lenses in order to eliminate unwanted prismatic effects. Our sample can be a fair representation of the normal Iranian population because of the large number of cases and that IPD has no correlation with refractive errors.3-6
IPD is known to be dependent on factors such as age, sex and race/ethnicity.2,3 Mean and median IPD values for adult humans are around 63 mm. With regard to extremes, the vast majority of adults have an IPD ranging from 50 to 75 mm.5-7 IPD may be as small as 40 mm in 5 year-old children and even 30 mm among newborn babies.5-7 In the present study, IPD measurements were larger in men as compared to women which is similar to other studies2,7-10, however Gupta11 reported that gender did not influence IPD values in a normal Indian population. As compared to women, all skeletal measurements are larger in men, therefore, larger IPD values in men is probably due to a larger craniofacial skeleton.
Mean adult IPD values in our study was 62.1 mm which is lower than those observed in other races: 63.7mm in black Americans, 64 mm in white Americans, and 63 mm in mixed Europeans.2 IPD of 63.5 mm has been reported as an “international standard” by Waack.12 However, this author did not state any reference for this statement.
Hofstetter13 studied white male adults in the USA and found that mean IPD is 65 to 66 mm, 90% of subjects lie between 60 and 70 mm, and 99.8% lie between 55 and 75 mm; these findings are relatively consistent with our findings which revealed that 91.5% of subjects have IPD from 55 to 70 mm and 93% of individuals have IPD of 60 to 65 mm. With regard to changes in IPD with age, Aslin14 showed that mean IPD increases by 60% from 40 mm in newborns to about 65 mm in adults. It has been reported that most of this change occurs in the first year of life continuing to the age of 17 and probably to the age 30.4,15
As expected, the results of this study are similar to a preliminary study on a portion of the present dataset, and also very similar to data from another study of comparable racial composition using a different measurement method.16 The normal values and standard deviation for IPD determined in this study have important clinical implications as well as applications in the optical industry. While confusion over the mean is one problem, we are also interested in acquiring accurate data on the distribution and extremes of human eye separation. It is clear that human eye separation does not follow a normal distribution with infinitely long tails, and that there must be some extremes outside of which there will be no examples in the human population. Manufacturers of binoculars and stereo-microscopes have had to deal with these extremes for several decades. It is useful to consider the range of adjustments quoted for stereo-microscopes.12
Previous studies provide only limited data on the change in IPD with age, notably that 40-year-old white females are significantly different from white females in their early twenties.11 Evereklioglu et al9 showed that IPD increases markedly up to the age of 19 years in male subjects and up to the age of 14 years in females, reflecting earlier maturation of the latter gender. They refer to evidence in the literature indicating that IPD continues to increase slightly up to the age of 30 years and that IPD continues to increase into early adulthood. Our study revealed a significant difference between IPD of subjects before and after the age of 50 years such that mean IPD was at least 1 mm larger in subjects older than 50 years as compared to the 30-50 year age group (P<0.001).
The most dramatic increase in IPD occurs in the first year of life.4 Pryor16 measured the increase in IPD in 6 to 15-year-old subjects from California and Mexico, and showed that IPD continues to increase from early childhood into late teens.
It is unlikely to find many fully-grown adults with an IPD outside the range of 55-70 mm. Therefore, it is expected that this relatively narrow range will include the vast majority of adults, as stereomicroscope manufactures have already explicitly assumed in the adjustment ranges of their devices. Designing with a narrower range in mind may exclude some of the adult population.17
In the current study, we found that mean IPD increased with age. Although this enlargement was more significant in the first three decades of life, it continued after 30 years of age, even after the age of 50. IPD enlargement after the age of 30 indicates that factors other than skeletal growth may affect this parameter.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Jonasson F, Thordarson K. Refraction and interpupillary distance measurements of adult Icelanders with special references to presbyopes possible use of supermarket standard spectacles. Acta Ophthalmol Suppl. 1987;182:44–47. doi: 10.1111/j.1755-3768.1987.tb02588.x. [DOI] [PubMed] [Google Scholar]
- 2.Murphy WK, Laskin DM. Intercanthal and interpupillary distance in the black population. Oral Surg Oral Med Oral Pathol. 1990;69:678–680. doi: 10.1016/0030-4220(90)90346-t. [DOI] [PubMed] [Google Scholar]
- 3.Bogren HG, Franti CE, Wilmarth SS. Normal variations of the position of the eye in the orbit. Ophthalmology. 1986;93:1072–1077. doi: 10.1016/s0161-6420(86)33618-2. [DOI] [PubMed] [Google Scholar]
- 4.Millidot M. Dictionary of Optometry and Visual Science. 5th. Boston: Butterworth-Heinemann; 2000. [Google Scholar]
- 5.Dodgson NA. Variation and extrema of human interpupillary distance. In: Woods AJ, Merritt JO, Benton SA, Bolas MT, editors. Proceedings of SPIE: Stereoscopic Displays and Virtual Reality Systems XI. San Jose, CA, USA; 2004. [Google Scholar]
- 6.Wang Y, Zhao Y, Ai Y. Survey on the growth of interpupillary distance of Chinese children aged 5 to 17 years. Zhonghua Yan Ke Za Zhi. 2001;37:63–65. [PubMed] [Google Scholar]
- 7.MacLachlan C, Howland HC. Normal values and standard deviations for pupil diameter and interpupillary distance in subjects aged 1 month to 19 years. Ophthalmic Physiol Opt . 2002;22:175–182. doi: 10.1046/j.1475-1313.2002.00023.x. [DOI] [PubMed] [Google Scholar]
- 8.Zhang M, Hong R, Fu Z, Ye M, Yang H. The measurement of normal values of exophthalmos, interpupillary distance, and interorbital distance of children and adolescence in Xiamen and the rule of their development. Zhonghua Yan Ke Za Zhi . 2000;36:462–466. [PubMed] [Google Scholar]
- 9.Evereklioglu C, Doganay S, Er H, Tercan M, Gunduz A, Balat A, et al. Interpupillary index: a new parameter for hypo-hypertelorism. J Craniomaxillofac Surg . 2001;29:191–194. doi: 10.1054/jcms.2001.0230. [DOI] [PubMed] [Google Scholar]
- 10.Pivnick EK, Rivas ML, Tolley EA, Smith SD, Presbury GJ. Interpupillary distance in a normal black population. Clin Genet. 1999;55:182–192. doi: 10.1034/j.1399-0004.1999.550306.x. [DOI] [PubMed] [Google Scholar]
- 11.Gupta VP, Sodhi PK, Pandey RM. Normal values for inner intercanthal, interpupillary, and outer intercanthal distances in the Indian population. Int J Clin Pract . 2003;57:25–29. [PubMed] [Google Scholar]
- 12.Waack FG. Stereo Photography. [15 March 2011]. (English translation of German book published by the German Stereoscopic Society). http:// www.stereoscopy.com/library/waack-ch-3.html.
- 13.Hofstetter HW. History of optometery. J Am Optometric Assoc. 1972;43:1151–1155. [Google Scholar]
- 14.Aslin RN, Jackson RW. Accommodative-convergence in young infants: development of a synergistic sensory-motor system. Can J Psychol. 1979;33:222–231. doi: 10.1037/h0081722. [DOI] [PubMed] [Google Scholar]
- 15.Fledelius HC, Stubgaard M. Changes in eye position during growth and adult life as based on exophthalmometry, interpupillary distance and orbital distance measurements. Acta Ophthalmol (Copenh) 1986;64:481–486. doi: 10.1111/j.1755-3768.1986.tb06958.x. [DOI] [PubMed] [Google Scholar]
- 16.Pryor HB. Objective measurement of interpupillary distance. Pediatrics. 1969;44:973–977. [PubMed] [Google Scholar]
- 17.Kaimbo WA, Ngiyulu Makuala R, Tshilolo Mwepu L, Missotten L. Outer orbital distance, inner canthal distance and interpupillary distance, proptosis in children with homozygous sickle cell disease. Bull Soc Belge Ophtalmol. 2000;275:33–37. [PubMed] [Google Scholar]