Abstract
The Coordinated-Transitional Care (C-TraC) Program was designed to improve care coordination and outcomes among veterans with high-risk conditions discharged to community settings from the William S. Middleton Memorial Veterans Hospital, in Madison, Wisconsin. Under the program, patients work with nurse case managers on care and health issues, including medication reconciliation, before and after hospital discharge, with all contacts made by phone once the patient is at home. Patients who received the C-TraC protocol experienced one-third fewer rehospitalizations than those in a baseline comparison group, producing an estimated savings of $1,225 per patient net of programmatic costs. This model requires a relatively low amount of resources to operate and may represent a viable alternative for hospitals seeking to offer improved transitional care as encouraged by the Affordable Care Act. In particular, the model may be attractive for providers in rural areas or other care settings challenged by wide geographic dispersion of patients or by constrained resources.
The transition from hospital to home can be treacherous for vulnerable patients. Poor quality transitions can result in medication errors, discontinuity in care plans, and confusion or dissatisfaction for patients.(1–5) Poor transitions probably contribute to the rehospitalization of nearly one in five patients within thirty days of discharge.(6) Yet many of these transitional care problems can be prevented.(7–8)
Rigorous studies in hospital settings that are not part of the Department of Veterans Affairs (VA) health care system have demonstrated that transitional care programs, such as those that provide in-home visits to give focused support to the patient and caregivers during the early posthospital period, can improve patient safety and posthospital outcomes, including fewer rehospitalizations.(7–9) The Affordable Care Act has increased the national focus on care transitions and rehospitalizations through efforts such as Medicare’s Community-Based Care Transitions Program, which enables community-based organizations to apply for federal funding to adopt evidence-based transitional care models.(10)
However, none of these traditional transitional care programs target patients who live in relatively remote areas, beyond the reach of a home visit, nor have any of them been tested in VA or other settings with a wide geographic dispersion of patients.(11–15) Without a program to fit their particular needs, health systems within these types of settings may have difficulty achieving transitional care improvements or accessing Community-Based Care Transitions Program funding for their many patients who live beyond the reach of a home visit.
The VA has recently undergone substantial restructuring of its primary care delivery system to create Patient Aligned Care Teams.(16) These VA teams are based on a patient-centered medical home structure and emphasize care integration, coordination, and management. Each team has a nurse case manager to help achieve these goals, but performing home visits for recently hospitalized patients is typically not compatible with the team’s daily workflow. Therefore, no tested model of transitional care has been utilized routinely in these VA teams.
Existing home-visit based transitional care models are not appropriate for the William S. Middleton Memorial Veterans Hospital, in Madison, Wisconsin—a facility serving a large geographic region of the upper Midwest, in which 75 percent of patients reside beyond the reach of a home visit. Yet, because of the infrastructure existing within the VA Patient Aligned Care Team model, this hospital has a well-developed resource of nurse case managers who could potentially be utilized within a novel, phone-based transitional care program.
To address this geographic challenge and to best utilize these nurse case manager resources, transitional care researchers, nurses, geriatricians, and leadership at the Madison VA Hospital developed the Madison VA Coordinated-Transitional Care (C-TraC) Program as a Geriatric Research Education and Clinical Center(18) clinical quality improvement program.
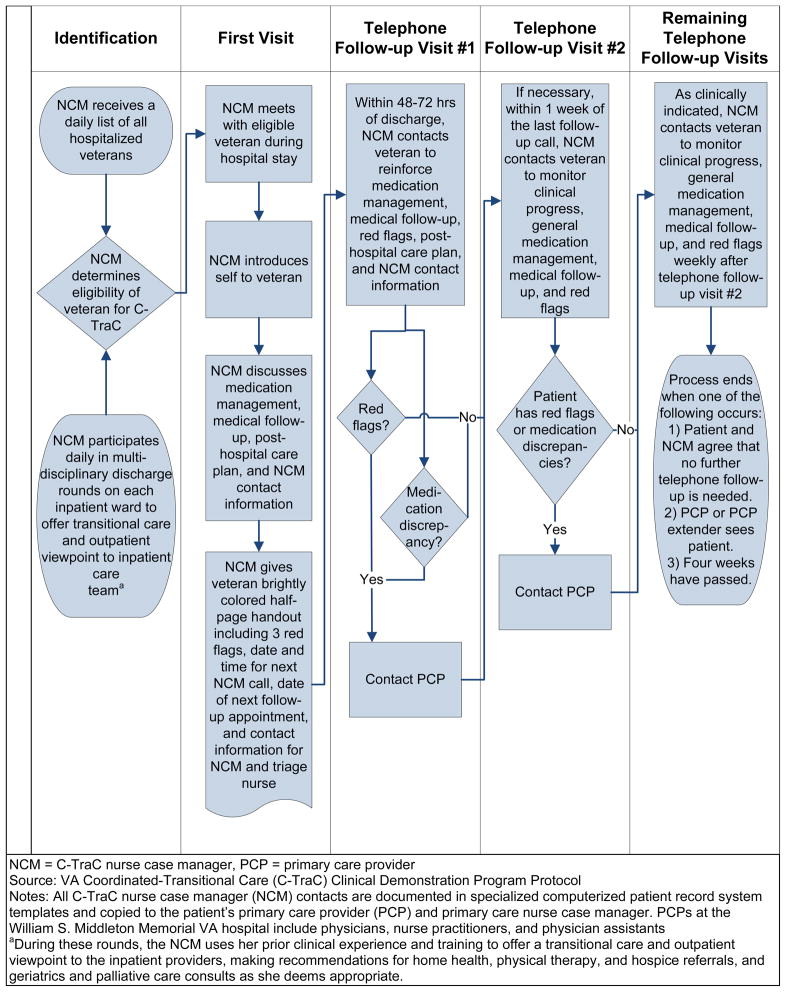
C-TraC is a phone-based, protocol-driven program designed to reduce thirty-day rehospitalizations and to improve care transitions during the early posthospitalization period. The program uses a registered nurse case manager to coordinate the veteran’s transitional care through active participation in inpatient multidisciplinary discharge rounds, a single brief protocol-driven inpatient encounter, and one to four protocol-driven posthospital telephone calls with the veteran and, if available, the veteran’s caregiver.
This article provides a detailed outline of the program’s clinical protocols and feasibility and an assessment of its impact on thirty-day rehospitalization. It provides evidence that C-TraC may be a practical and effective transitional care option for VA, rural, or other care settings challenged by wide geographic dispersion of patient populations or by constrained resources.
The C-TraC Program
Veteran Eligibility
The C-TraC Program was launched April 1, 2010, as a Geriatric Research Education and Clinical Center(17) clinical quality improvement project at the Madison VA Hospital. The facility is an eighty-seven-bed general VA hospital, with approximately 4,400 admissions annually. It provides inpatient medical and surgical services to eligible veterans throughout Wisconsin, northern Michigan, and northern Illinois. Of the veterans who receive care at the hospital, 75 percent reside beyond the reach of a home visit.
C-TraC targeted community-dwelling veterans at high risk of poor posthospital outcomes. Veterans hospitalized on medical or surgical wards and discharged to noninstitutional community settings, including home or assisted living facilities, were eligible, provided that they had a working telephone. Eligible veterans also required medical documentation of dementia, delirium, or other cognitive impairment or, alternatively, had to be at least sixty-five years old and either living alone or previously hospitalized during the preceding year. Veterans were excluded if they were discharged as twenty-four-hour observation patients or if their primary diagnosis was alcohol withdrawal.
The program was deemed not to be research by the University of Wisconsin Institutional Review Board and by the Madison VA Research and Development Committee. Therefore, no research-level written consent was obtained. Veterans were verbally asked if they wanted to participate, and, as with any clinical program, they had the right to refuse services.
Goals Of C-TraC
For eligible veterans, the C-TraC nurse case manager, who was a senior registered nurse with extensive geriatrics and case management experience, used standardized protocols to achieve the following four goals, adapted from Coleman’s Four Pillars of transitional care.(7) These pillars are as follows: First, educate and empower the veteran and the veteran’s caregiver in medication management. Second, ensure that the veteran has medical follow-up in place and is ready to participate in that follow-up. Third, educate the veteran and the veteran’s caregiver regarding the signs of a worsening medical condition, called “red flags,” and how to respond. Fourth, ensure that the veteran and the veteran’s caregiver know whom to contact if concerns arise after hospital discharge but before the first outpatient follow-up.
In contrast to Coleman’s Four Pillars approach, C-TraC veterans did not create a personal health record with the nurse case manager. This step was omitted because the day of discharge was already full of hours of education that could overwhelm a vulnerable patient; because performing this step over the phone would have been problematic; and because having a patient handwrite his or her own health record would be difficult, frustrating, and possibly ineffective for those with cognitive impairments or other vulnerabilities.
The Protocol
The nurse case manager identified eligible veterans and participated in daily multidisciplinary discharge rounds on each specified inpatient ward. During these rounds, she offered geriatric and transitional care advice to the inpatient providers, making recommendations for home health, therapy, and hospice referrals and geriatrics and palliative care consults as appropriate. Also, from her prior contacts, she often had in-depth knowledge about frequently hospitalized veterans and could provide important information to the inpatient care teams who knew the veteran less well. The nurse case manager performed these tasks even if the veteran was not interested in C-TraC participation.
The nurse case manager met with each eligible veteran and his or her caregiver, if that person was present, prior to hospital discharge. At that time, she introduced herself and the program’s goals and verbally inquired whether the veteran wished to participate in the program. If so, she proceeded to schedule a phone call within 48–72 hours of discharge, and to ensure that an active plan for posthospital medical follow-up was in place.
The nurse case manager gave the veteran a brightly colored half-page handout documenting the veteran’s red flags, the dates and times for the follow-up call and the posthospital medical follow-up appointment, and contact information for herself and triage, with instructions to call if red flags or other concerns arose. Red flags were identified by the nurse case manager and limited to three in number to optimally conform with principles of adult learning.(18)
Additionally, as the standard of care, all veterans discharged from Madison VA Hospital received complete medication reconciliation and discharge counseling by a pharmacist, and routine educational materials and discharge teaching by medical and nursing personnel. Medication reconciliation is a process by which medication discrepancies between different sites of care are identified through review of a patient’s current and previous medication regimens as a way to improve patient safety.(19)
The veteran and the veteran’s caregiver, if present, were phoned at the prearranged time within 48–72 hours after discharge to reinforce the four transitional care goals. In this initial phone call, veterans were asked to have all of their pill bottles in front of them. They were then asked, “Tell me how you take your medications,” to facilitate a patient-led medication reconciliation. The hospital discharge medication list was used as the “gold standard” for this process.
Red flags, plans for medical follow-up, and contact information were again reviewed. These calls lasted thirty-six minutes each, on average, with the majority of time spent in medication reconciliation. Each veteran received 1.5 calls, on average.
Calls continued on a weekly basis until the primary care provider or appropriate specialty provider saw the veteran in follow-up, or the veteran and nurse case manager agreed that no additional calls were necessary, or four weeks passed. If red flags or medication discrepancies were identified, the nurse case manager contacted the primary care provider. If these issues merited immediate attention, the nurse case manager would arrange an urgent care appointment for the veteran or recommend that the veteran be seen in the emergency department.
If a home visit for in-person assessment or clinical care was deemed necessary by the nurse case manager, she would arrange a nursing visit through an available home health agency in the veteran’s area. For cognitively impaired veterans without a caregiver, the nurse case manager worked to activate potential caregivers and community supports.
All contacts were documented using specially designed electronic health record templates and copied to the primary care provider and outpatient nurse case manager. The nurse case manager was available Monday through Friday, 8 a.m. to 5 p.m. Patient calls that arose outside of these hours were fielded by the VA triage service.
The full role of the nurse case manager can be seen in Exhibit 1. Additional programmatic implementation details and metrics can be found in the expanded methods section within the technical Appendix. The C-TraC protocols, phone scripts, and other materials are available through the University of Wisconsin Health Innovation Program.(20)
Exhibit 1.
Role of a C-TraC Nurse Case Manager
Study Data And Methods
Program Evaluation: Data Collection And Analysis
Sociodemographics, comorbidities, functional measures, C-TraC process measures, and outcomes were abstracted from each veteran’s medical record by a team of three trained medical abstractors using a standardized manual and form.(21) Outcomes data included medication discrepancies discovered and rectified during the phone call 48–72 hours after discharge and the presence of a thirty-day rehospitalization back to the VA.
Twenty-four months worth of data were analyzed to determine changes in program effectiveness, program maturation, and sustainability of effect. The first six months of the program, April–September 2010, constituted a baseline or establishment period, during which full data collection commenced but draft intervention protocols were implemented in only a partial, trial fashion with a limited number of participants. The large majority of individuals in the baseline period did not receive the bulk of the intervention.
The subsequent eighteen months of the program, October 2010 through March 2012, constituted the intervention period. During the intervention period the C-TraC program used finalized protocols and fully trained staff, and enrollment was maximized to capacity.
Basic frequencies were calculated for C-TraC process measures, outcomes, and veteran characteristics. Multivariate logistic regression with robust estimates of the variance to account for clustering were used to produce adjusted odds ratios and 95 percent confidence intervals examining the relationship between thirty-day rehospitalization and enrollment within the C-TraC intervention period versus the baseline period, adjusting for all sociodemographics, Charlson comorbidity score, and functional measures listed in the technical Appendix.(27–28) All confidence intervals and p values were tested for significance at 0.05. Full data abstraction and analysis details can be found in the expanded methods section within the technical Appendix.
Limitations
The results presented here should be considered in light of a number of limitations. The data were collected from patients within a single midwestern VA hospital. Madison VA patients have ready access to primary care, nurse case managers, urgent care, and a twenty-four-hour triage nursing line, all staffed by providers who use the same electronic health record. These characteristics may have made C-TraC more effective, but they are also available in many other non-VA health systems and primary care medical homes.
Future studies are needed to determine if C-TraC’s effects on rehospitalization persist in larger patient samples and in other sites. This initial study supports the feasibility of testing the program in larger, multisite trials.
The nurse case manager was not available on weekends or holidays. Some veterans who may have qualified for enrollment and who were hospitalized during weekends and holidays may have been missed. Additionally, since the program enrolled only veterans discharged to the community, these results do not apply to veterans discharged to other settings, such as nursing homes. Veterans discharged to settings other than the community may require alternative approaches to their transitional care. Also, only rehospitalizations to the VA were measured. Rehospitalizations to non-VA hospitals were not assessed.
Changes in rehospitalization were assessed using a pre-post design. Such designs are inherently limited because the baseline and comparison groups may differ in important ways. To address this limitation, statistical modeling was used to adjust for measurable between-group differences. Furthermore, thirty-day rehospitalizations during the intervention period were measured over eighteen months to assess C-TraC’s sustainability in the event of effect weakening.
It is possible that this pre-post design may have underestimated the program’s effect, because the baseline was established during the intervention ramp-up phase when some things may have already been in the process of changing. Future testing of C-TraC in a multisite randomized trial would provide a more rigorous assessment.
Study Results
Serving High-Risk Veterans
Seven hundred and thirteen veterans were identified as eligible and approached for enrollment in C-TraC from the April 1, 2010, program launch through March 31, 2012, using the criteria and procedures listed above. Five veterans refused enrollment and were excluded, producing a final sample size of 708. All veterans enrolled in the program were included in the analysis, regardless of whether they completed the full protocol.
C-TraC-enrolled veterans reflected the typical population of high-risk and cognitively impaired veterans served at Madison VA Hospital (Exhibit 2). The majority of these veterans were older than seventy years, male, and white. Thirty-nine percent lived alone; 26 percent had no high school diploma or equivalent. They had high rates of previous hospitalizations, cognitive impairment, and other comorbidities (Appendix table 1).
Exhibit 2.
Characteristics Of Veterans In The VA Coordinated-Transitional Care (C-TraC) Program
| Characteristic | Total (N = 708) | Baseline period (n = 103) | Intervention period (n = 605) |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Average age (years) | 75a | 74b | 75c |
| White | 97% | 99% | 97% |
| Male | 97 | 98 | 97 |
| Lives alone | 39 | 41 | 39 |
| Medicaid | 2 | 2 | 2 |
| Education level | |||
| <8 years | 10 | 10 | 11 |
| Some high school | 16 | 19 | 15 |
| High school diplomad | 39 | 39 | 40 |
| Some college | 24 | 25 | 24 |
| College degree | 10 | 8 | 11 |
| Comorbidities and disease severity | |||
| Previous hospitalization in past 12 months | 69** | 79** | 68** |
| Average Charlson comorbidity Score | 6.2e | 6.5e | 6.1e |
| Functional measures, 2 weeks prior to hospitalization | |||
| Additional help neededf | 27% | 22% | 28% |
| Increased difficulty standing or walking | 44 | 46 | 43 |
| Manages own medications | 67 | 64 | 67 |
Source: Authors’ analysis.
Notes: Baseline period was April–September 2010. Intervention period was October 2010–March 2012. Charlson comorbidity score calculated as described in Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51. Charlson M, Pompei P, Ales KL, MacKenzie CR. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J Chronic Dis. 1987;40(5):373–383.See Appendix Table 1 for additional details (see Note 21 in text).
Standard deviation: 8.4.
Standard deviation: 7.3
Standard deviation: 8.6.
Or graduate equivalency degree (GED).
Standard deviation: 3.9.
With one or more of the following activities: bathing, dressing, transferring to or from bed or toilet.
p < 0.05
Sixty-seven percent reported managing their own medications, but 27 percent reported needing more help with some basic activities of daily living, and 44 percent noted a decline in their ability to stand or walk during the two weeks prior to the hospitalization. Baseline period veterans had slightly higher rates of previous hospitalization than intervention period veterans. However, no other major between-group differences were noted.
Outcomes: Medication Discrepancies, Rehospitalizations
During the phone call performed by the C-TraC nurse case manager 48–72 hours after discharge, 47 percent of all veterans had a medication discrepancy identified and corrected (Exhibit 3). The average number of medication discrepancies per veteran, for those with any discrepancy, was 2 (range 1–10). The most common classes of medications with discrepancies can be seen in Exhibit 3.
Exhibit 3.
Medication Discrepancies Identified And Rectified By The VA Coordinated-Transition Care (C-TraC) Program
| Medication discrepancy characteristic | N/% |
|---|---|
| Prevalence of medication discrepancies | |
| Average medications per veteran | 17a |
| Total medication discrepancies | 639 |
| Veterans with medication discrepancies rectified by C-TraC | 47% |
| Average medication discrepancies per veteranb rectified by C-TraC | 2c |
| Most common medication classes with discrepancies (% of all discrepancies) | |
| Gastrointestinal agents | 21 |
| Vitamins/supplements | 21 |
| Pain control (analgesics, nonsteroidal anti-inflammatory drugs) | 17 |
| Cardiovascular (antihypertensives, diuretics, nitrates) | 16 |
| Steroidal anti-inflammatory drugs (corticosteroids) | 7 |
| Bronchodilators | 8 |
| Most common medications with discrepancies (% of all discrepancies) | |
| Albuterol (asthma/emphysema medication) | 6 |
| Omeprazole (stomach acid blocker) | 6 |
| Aspirin (pain reliever/fever reducer/blood thinner) | 5 |
| Docusate (laxative) | 5 |
| Furosemide (diuretic) | 4 |
Source: Authors’ analysis.
Notes: During the follow-up phone call performed by the nurse case manager 48–72 hours after discharge, 547 medication discrepancies were identified and rectified by C-TraC. Prior to the first follow-up phone call, 58 veterans who were enrolled in the C-TraC program met program discharge criteria. Data shown are for veterans who received the follow-up phone call.
Range: 0–43.
For veterans with any discrepancy.
Range: 1–10.
C-TraC intervention period enrollees experienced lower rates of thirty-day rehospitalization as compared to the baseline group, with 34 percent of the baseline group and 23 percent of the intervention group experiencing a thirty-day rehospitalization (p = 0.013; Appendix figure 1). After adjusting for sociodemographics, comorbidity, and functional status using multivariate logistic regression models, C-TraC intervention enrollees were less likely to be rehospitalized than the baseline group (odds ratio: 0.55; 95% confidence interval: 0.33, 0.90; p = 0.018; Appendix table 2).
The 605 intervention period enrollees had an average rehospitalization length-of-stay of 6.1 days and average direct daily costs for acute medical and surgical care of $2,364 per day. The eleven-percentage-point decrease in rehospitalizations corresponded to 408.7 prevented hospital days at a gross direct cost avoidance of $966,167 over eighteen months. After accounting for all programmatic costs, the net cost avoidance for the C-TraC program over the eighteen-month intervention period was $1,225 per veteran enrolled.
Sustained Results
Appendix figure 1 shows thirty-day rehospitalization by three-month quarters. These data support that the decrease in rehospitalizations observed for C-TraC enrollees was sustained throughout the eighteen-month intervention period with rehospitalization rates ranging from 22 percent to 25 percent. Given these results, the C-TraC program is now sustainably funded by Madison VA Hospital and continues in operation to this day. Rehospitalization effects continue to be monitored.
Discussion
Overview
The Madison VA C-TraC Program is a feasible, protocol-driven program that is associated with lower thirty-day rehospitalization rates and an overall net cost avoidance within the Madison VA Hospital. This suggests that C-TraC improves care transitions while simultaneously freeing up inpatient beds, enabling the hospital to provide inpatient care to more veterans in need.
Additionally, C-TraC makes use of preexisting nursing resources available in most patient-centered medical homes, including the VA’s Patient Aligned Care Teams.(16) Operating C-TraC can be done at comparatively low cost in a transitional care field in which few low-resource options currently exist. This is especially important given the increased national attention on rehospitalization triggered by the Affordable Care Act, motivating all hospitals to address transitional care, regardless of resources or location.
Utility In Other Settings
Simple, protocol-driven, telephone-based programs like C-TraC may be able to reach larger patient populations, including patients living a greater distance from hospitals, and could potentially be used in a wider variety of care settings than traditional in-home transitional care programs.(7–8) It may not be possible for hospitals with constrained resources, such as safety-net organizations, or those with patient populations dispersed over large areas, such as critical access and rural hospitals, to launch more traditional home-visit-based transitional care programs.
Health systems that were previously unable to support a transitional care option because of constrained resources or a wide geographic dispersion of patients could use a program like C-TraC to improve their transitional care services or to qualify for funding currently available through Medicare’s Community-Based Care Transitions Program.(10) The Community-Based Care Transitions Program, created by Section 3026 of the Affordable Care Act, enables community-based organizations or hospitals partnered with community-based organizations to apply for federal funding to enact evidence-based interventions to improve care transitions and reduce rehospitalizations for high-risk Medicare beneficiaries.(22)
However, it is important to note that C-TraC was piloted in a VA hospital, and that VA hospitals may differ from non-VA hospitals in important ways. VA hospitals utilize a single electronic health record system that is shared among all VA-affiliated inpatient and outpatient providers, allowing for more streamlined communication. Although some non-VA hospitals also have shared electronic health record systems, many do not.
Inpatient and outpatient medical staff are typically employed directly by the VA. Similar direct physician employment occurs in some, but not all, non-VA hospitals and health systems. Additionally, VA staff are bound by a shared goal of bettering the health of all veterans.
Although these cultural and organizational aspects of the VA may contribute to C-TraC’s success, whether they do so or not is not certain. It will be important to test the program in a wide variety of non-VA health systems to determine if C-TraC is effective in a spectrum of settings.
Integration Into The Patient-Centered Medical Home
By encouraging nurse case managers to maximize their scope of practice, programs like C-TraC allow for more efficient use of resources already embedded within many health systems, patient-centered medical homes, and VA Patient Aligned Care Teams.(16) C-TraC combines more traditional elements of case management with coaching protocols used in transitional care to formalize the role of a nurse case manager as the coordination hub of the system, allowing this person to more proactively bridge the gap between hospital care teams and primary care. Hospital-based C-TraC nurse case managers could be incorporated into patient-centered medical homes as a way to more effectively bridge hospitals and outpatient systems, while also supporting high-risk patients during posthospital transitions.
Program Acceptability
C-TraC refusal rates were low. In contrast, home-visit-based transitional care programs can have very high patient refusal rates, up to 86 percent in some studies.(23–24) C-TraC’s posthospital phone-based approach was well received by veterans, with only five in-hospital refusals of enrollment offers during the first twenty-four months of program operation. Ninety percent of enrollees were successfully reached for the follow-up phone call 48–72 hours after discharge. This reach rate compares favorably to other phone outreach programs.(25)
Although this study was not designed to determine why the refusal rates for participation in C-TraC were so low, some hypotheses can be considered. First, it is possible that phone-based transitional care programs are fundamentally more acceptable to a larger proportion of the population than in-home programs.
Second, this is the first transitional care intervention published for a VA hospital setting. VA patients are different than non-VA patients in many important ways and may be more accepting of VA programs, like C-TraC.
Third, the nurse case manager was tightly integrated with both the inpatient and outpatient teams. As a result, the nurse case manager may have been seen by veterans as a natural extension of hospital and outpatient care.
Fourth and finally, although most enrolled veterans had no prior relationship with the nurse case manager, some of the frequently rehospitalized veterans did encounter her more than once. These repeat encounters may have allowed for additional rapport building. Nevertheless, this low refusal rate merits further study to determine how C-TraC’s success in this regard could be replicated in other programs, and it suggests that C-TraC may provide an alternative transitional care option for patients who are unwilling to allow a home visit.
Importance Of Medication Reconciliation After Discharge
Nearly half of all C-TraC subjects had medication discrepancies noted within two or three days of hospital discharge. All of these veterans had medication reconciliation and discharge counseling in the hospital, yet C-TraC reinforcement teachings after discharge were needed to support the veterans optimally as they struggled to manage complicated medication regimens at home. This reality suggests that current Joint Commission mandates for medication reconciliation(26) should be broadened to encourage additional or alternative approaches to support medication management even after hospital discharge.
Conclusion
This study suggests that C-TraC is a feasible transitional care program that decreases rehospitalizations in Madison VA Hospital veterans with high-risk conditions. C-TraC operates on a relatively low cost and resource base, and may represent a viable alternative for transitional care in VA, rural, or other settings challenged by geographic distance, constrained resources, or patients who refuse in-home transitional care visits. C-TraC’s phone-based design is well suited for implementation within patient-centered medical home–type care models, including the VA’s Patient Aligned Care Teams.
Future multisite research studies are needed to evaluate C-TraC’s effectiveness in decreasing rehospitalizations in other health systems and settings.
Supplementary Material
Acknowledgments
Some of the information in this article was presented as a poster at the annual meeting of the American Geriatrics Society, Seattle, Washington May 3rd 2012. The design, implementation and assessment of the C-TraC program and the writing of this article was supported by a VA Transformation-21 Grant, “Patient-Centric Alternatives to Institutional Extended Care”; the Madison VA Geriatrics Research, Education, and Clinical Center (GRECC-Manuscript #2012-08); and funded through the National Institute on Aging Paul B. Beeson Patient-Oriented Research Career Development Award (K23AG034551 [PI Kind], National Institute on Aging, in partnership with The American Federation for Aging Research, The John A. Hartford Foundation, The Atlantic Philanthropies and The Starr Foundation). Additional support was provided by the University of Wisconsin School of Medicine and Public Health’s Health Innovation Program; the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research; and the Clinical and Translational Science Award program of the National Center for Research Resources, National Institutes of Health (Grant 1UL1RR025011). No funding source had a role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The authors acknowledge Ken Shay, Barbara Hyduke, and Karen Massey in the VA Office of Geriatrics and Extended Care in VA Central Office and the leadership of both the Veterans Integrated Service Network 12 and the William S. Middleton VA Hospital for their support of the C-TraC program; Peggy Munson for Institutional Review Board assistance; Sheila Kelly and Megan Carey for data abstraction; and Colleen Brown, Andrea Gilmore, Melissa Hovanes, Brock Polnaszek, and Joanna Wong for manuscript formatting and graphics.
Biographies
Kind is director of the Veterans Affairs (VA) Coordinated-Transitional Care (C-TraC) Demonstration Program, within the Geriatrics Research, Education, and Clinical Center (GRECC) at the William S. Middleton VA Hospital, Madison, Wisconsin. She also serves as codirector of and attending physician in GRECC’s Memory Assessment Clinic, and she is an assistant professor in the Division of Geriatrics and Gerontology, University of Wisconsin School of Medicine and Public Health.
Kind’s research focuses on improving care transitions for vulnerable populations. She is board certified in geriatrics and internal medicine and received both a medical degree and a doctorate in population health sciences, with a focus on health services research, from the University of Wisconsin.
Laury Jensen is a registered nurse and C-TraC’s nurse case manager. To this position, she brings an extensive background in nursing case management and care coordination in the inpatient, outpatient, and home health settings.
Twice the recipient of the William S. Middleton VA Hospital’s Team Innovation Award, Jensen obtained her bachelor’s degree in nursing from Edgewood College, Madison, Wisconsin.
Steve Barczi, director of education and evaluation for GRECC, is an associate professor of medicine in the Department of Medicine, Division of Geriatrics and Gerontology, University of Wisconsin School of Medicine and Public Health. His additional appointments with the University of Wisconsin include director of the Geriatric Medicine Fellowship Program and codirector of the Advanced Research Fellowship in Geriatrics, both at GRECC.
Board certified in internal medicine, geriatrics, and sleep medicine, Barczi holds a medical degree from the University of Illinois.
Alan Bridges is chief of staff of the William S. Middleton VA Hospital. In addition, he holds multiple appointments with the University of Wisconsin, including senior vice chair of its Department of Medicine and professor of medicine in its School of Medicine and Public Health.
Board certified in internal medicine and rheumatology, Bridges received a medical degree from the University of Illinois College of Medicine, Peoria.
Rebecca Kordahl is the nurse executive and associate director of patient care services at the William S. Middleton VA Hospital. She is responsible for the overall management of nursing practice, nursing education and professional development, nursing research, and numerous administrative functions.
The recipient of a diploma in nursing from Lutheran Deaconess School of Nursing, Minneapolis, Minnesota, Kordahl holds an MBA from St. Thomas University, Saint Paul, Minnesota, and is board certified in advanced nursing administration.
Maureen Smith is a physician, health services researcher, and associate professor at the University of Wisconsin School of Medicine and Public Health. Her leadership roles include faculty director of the Health Innovation Program and director of the community-academic partnerships core of the Institute for Clinical and Translational Research.
Smith holds both a master’s degree in public health and a medical degree from Yale University and a doctorate in health services research, policy, and administration from the University of Minnesota.
Sanjay Asthana is the Duncan G. and Lottie H. Ballantine Endowed Chair in Geriatrics in the Department of Medicine, University of Wisconsin School of Medicine and Public Health, as well as director of GRECC at the Madison VA Hospital. His numerous concurrent academic appointments include professor of medicine and division head of Geriatrics and Gerontology, also at the University of Wisconsin School of Medicine and Public Health.
A former practicing physician in Canada and India as well as in the United States, Asthana received a medical degree from the University College of Medical Sciences, University of Delhi, India.
Footnotes
ABOUT THE AUTHORS: AMY J.H. KIND, LAURY JENSEN, STEVE BARCZI, ALAN BRIDGES, REBECCA KORDAHL, MAUREEN A. SMITH & SANJAY ASTHANA
In this month’s Health Affairs, Amy Kind and coauthors report on their analysis of the Coordinated-Transitional Care program, or C-TraC, employed at the William S. Middleton Memorial Veterans Hospital, in Madison, Wisconsin. Under the program, nurse case managers consult with patients, including by telephone after they are discharged, on such issues as medication reconciliation. Those who received the full protocol experienced one-third fewer rehospitalizations than those in a baseline comparison group, yielding an estimated savings of $1,225 per patient net of programmatic costs. The authors suggest that this relatively low-cost model may be attractive to providers in rural areas or to others with similarly constrained resources.
References
- 1.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51(4):549–55. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 2.Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305–11. doi: 10.1001/archinte.167.12.1305. [DOI] [PubMed] [Google Scholar]
- 3.Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18(8):646–51. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snow V, Beck D, Budnitz T, Miller DC, Potter J, Wears RL, et al. Transitions of Care Consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med. 2009;4(6):364–70. doi: 10.1002/jhm.510. [DOI] [PubMed] [Google Scholar]
- 5.Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient’s perspective: the care transitions measure. Med Care. 2005;43(3):246–55. doi: 10.1097/00005650-200503000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 7.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–8. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 8.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–84. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 9.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: the importance of transitional care in achieving health reform. Health Aff (Millwood) 2011;30(4):746–54. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- 10.CMS.gov. Baltimore (MD): Centers for Medicare and Medicaid Services; Community-Based Care Transitions Program [Internet] [updated 2012 Aug 17; cited 2012 Oct 26]. Available from: http://www.cms.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?itemID=CMS1239313. [Google Scholar]
- 11.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252–7. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- 12.Krishnan LL, Petersen NJ, Snow AL, Cully JA, Schulz PE, Graham DP, et al. Prevalence of dementia among Veterans Affairs medical care system users. Dement Geriatr Cogn Disord. 2005;20(4):245–53. doi: 10.1159/000087345. [DOI] [PubMed] [Google Scholar]
- 13.Mooney C, Zwanziger J, Phibbs CS, Schmitt S. Is travel distance a barrier to veterans’ use of VA hospitals for medical surgical care? Soc Sci Med. 2000;50(12):1743–55. doi: 10.1016/s0277-9536(99)00414-1. [DOI] [PubMed] [Google Scholar]
- 14.Yaffe K, Vittinghoff E, Lindquist K, Barnes D, Covinsky KE, Neylan T, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67(6):608–13. doi: 10.1001/archgenpsychiatry.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu CW, Penrod JD, Ross JS, Dellenbaugh C, Sano M. Use of Medicare and Department of Veterans Affairs health care by veterans with dementia: a longitudinal analysis. J Am Geriatr Soc. 2009;57(10):1908–14. doi: 10.1111/j.1532-5415.2009.02405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of Veterans Affairs. Primary Care Program Office: Patient Aligned Care Team (PACT) [Internet] Washington (DC): VA; [updated 2010 Nov 17; cited 2012 Oct 26]. Available from: http://www.va.gov/PrimaryCare/pcmh/ [Google Scholar]
- 17.Department of Veterans Affairs. Geriatric Research Education and Clinical Centers [Internet] Washington (DC): VA; [reviewed/updated 2012 Aug 17; cited 2012 Oct 26]. Available from: http://www.va.gov/GRECC/index.asp. [Google Scholar]
- 18.Cowan N, Morey CC, Chen Z, Gilchrist AL, Saults JS. Theory and measurement of working memory capacity limits. Psychology of Learning and Motivation. 2008;49:49–104. [Google Scholar]
- 19.Agency for Healthcare Research and Quality. Patient safety primers: medication reconciliation [Internet] Rockville (MD): AHRQ; [cited 2012 Oct 26]. Available from: http://www.psnet.ahrq.gov/primer.aspx?primerID=1. [Google Scholar]
- 20.University of Wisconsin Health Innovation Program. HIPxChange [Internet] Madison (WI): HIP; [cited 2012 Oct 26]. Available from: http://www.hipxchange.org/C-Trac. [Google Scholar]
- 21.Reisch LM, Fosse JS, Beverly K, Yu O, Barlow WE, Harris EL, et al. Training, quality assurance, and assessment of medical record abstraction in a multisite study. Am J Epidemiol. 2003;157(6):546–51. doi: 10.1093/aje/kwg016. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Medicare and Medicaid Services. Community-based Care Transitions Program: solicitation for applications. Baltimore (MD): CMS; 2012. [updated 2012 Aug 17; cited 2012 Sep 19]. Available from: http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/downloads/CCTP_Solicitation.pdf. [Google Scholar]
- 23.Stauffer BD, Fullerton C, Fleming N, Ogola G, Herrin J, Stafford PM, et al. Effectiveness and cost of a transitional care program for heart failure: a prospective study with concurrent controls. Arch Intern Med. 2011;171(14):1238–43. doi: 10.1001/archinternmed.2011.274. [DOI] [PubMed] [Google Scholar]
- 24.Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med. 2011;171(14):1232–7. doi: 10.1001/archinternmed.2011.278. [DOI] [PubMed] [Google Scholar]
- 25.Bostrom J, Caldwell J, McGuire K, Everson D. Telephone follow-up after discharge from the hospital: does it make a difference? Appl Nurs Res. 1996;9(2):47–52. doi: 10.1016/s0897-1897(96)80402-2. [DOI] [PubMed] [Google Scholar]
- 26.Joint Commission. National patient safety goals effective January 1, 2012 [Internet] Oakbrook Terrace (IL): Joint Commission; 2012. [cited 2012 Mar 12]. Available from: http://www.jointcommission.org/assets/1/6/NPSG_Chapter_Jan2012_HAP.pdf. [Google Scholar]
- 27.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 28.Charlson M, Pompei P, Ales KL, MacKenzie CR. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.