Abstract
Introduction
HIV prevalence among pregnant women in Kenya is high. Furthermore, there is a high risk of maternal mortality, as many women do not give birth with a skilled healthcare provider. Previous research suggests that fears of HIV testing and unwanted disclosure of HIV status may be important barriers to utilizing maternity services. We explored relationships between women’s perceptions of HIV-related stigma and their attitudes and intentions regarding facility-based childbirth.
Methods
1,777 pregnant women were interviewed at their first antenatal care visit. We included socio-demographic characteristics, stigma scales, HIV knowledge measures, and an 11-item scale measuring health facility birth attitudes (HFBA). HFBA includes items on cost, transport, comfort, interpersonal relations, and services during delivery at a health facility versus at home. A higher mean HFBA score indicates a more positive attitude towards facility-based childbirth. The mean HFBA score was dichotomized at the median and analyses were conducted with this dichotomized HFBA score using mixed effects logit models.
Results
Women who anticipated HIV-related stigma from their male partner had lower adjusted odds of having positive attitudes about giving birth at the health facility (adjusted OR = .63, 95% CI 0.50–0.78) and less positive attitudes about health facility birth were strongly related to women’s intention to give birth outside a health facility (adjusted OR = 5.56, 95% CI 2.69–11.51).
Conclusions
In this sample of pregnant women in rural Kenya, those who anticipated HIV-related stigma were less likely to have positive attitudes towards facility-based childbirth. Furthermore, negative attitudes about facility-based childbirth were associated with the intention to deliver outside a health facility. Thus, HIV-related stigma reduction efforts might result in more positive attitudes towards facility-based childbirth, and thereby lead to an increased level of skilled birth attendance, and reductions in maternal and infant mortality.
Introduction
There is evidence that HIV and maternal mortality are not separate, but rather two intersecting epidemics in sub-Saharan Africa, as HIV is an increasing contributor to direct and indirect causes of maternal death [1]. Childbirth with a skilled healthcare provider is one of the key strategies recommended for prevention of maternal mortality and morbidity and has also been identified as important for enhancing prevention of mother-to-child transmission (PMTCT) of HIV [2]. In Kenya, only 43% of women give birth in a health facility with a skilled healthcare provider [3] and the lifetime risk of maternal mortality is 1 in 38 [4]. Many Kenyan women deliver outside the health facility with the assistance of an untrained traditional birth attendant (TBA).
A significant body of research has focused on the identification of factors that might explain why many women deliver outside the health facility globally. Investigators have found the place of delivery to be associated with socio-demographic factors; including age, education, religion, parity, and income[3], [5]–[15]. Barriers for delivering at a health facility include lack of transport, long travel times, and lack of money or mandatory supplies[6], [7], [16]–[18]. Furthermore, home birth is highly valued in many African cultures and delivering outside the homestead may be a cultural taboo [11], [15].
Another potentially important factor in decision-making about the type of assistance during childbirth may be the perceived quality of maternity care [8]. In fact, researchers in Ethiopia found that perceived quality of care was more important than distance and cost in decision-making for the place of delivery [19].
One factor potentially affecting women’s perceptions of maternity services that has not been examined in previous research is HIV-related stigma. Fears of stigma, discrimination, and lack of confidentiality in health facilities have been shown to discourage people from accepting HIV testing and linking to HIV care after receiving an HIV-positive test result in multiple settings around the world [20]. Our previous qualitative research in Kenya also identified fear of HIV testing as a reason that some women may avoid childbirth in health facilities, as they fear unwanted disclosure of their HIV testing and HIV status to their spouse or family at the health facility, and subsequent stigma and discrimination [21]. In-depth interviews with healthcare workers also revealed that some pregnant women experience stigma and discrimination from maternity workers [22]. Other literature from Kenya also reveals that women may perceive that they will be forced to test for HIV when visiting maternity services [23], as well as having concerns about the confidentiality of their HIV status at health facilities [24].
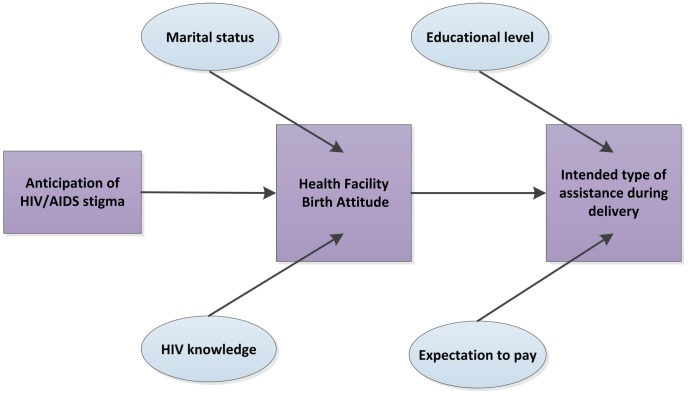
We investigated the relationships between pregnant women’s perceptions of HIV-related stigma, their attitudes towards giving birth at the health facility, and their intended type of assistance during birth. We hypothesized that anticipation of HIV-related stigma would lead to less positive attitudes towards delivery at the health facility and thereby would lead to an intention to deliver outside the health facility.
Methods
Ethical Statement
This study received ethical approval from the Kenya Medical Research Institute (KEMRI) Ethical Review Committee and the Committee on Human Research of the University of California, San Francisco.
Setting and Participants
The Maternity in Migori and AIDS Stigma (MAMAS) Study was conducted at sites supported by Family AIDS Care and Education Services (FACES), an HIV prevention, care, and treatment program operating in Nyanza Province Kenya. HIV prevalence among women of reproductive age in Nyanza Province is estimated at 16% [3]. Women at least 18 years old in their first seven months of pregnancy, who were visiting the antenatal care clinic (ANC) for the first time in their pregnancy and did not know their current HIV status (never tested or tested negative more than 3 months ago) were recruited at nine governmental health facilities. After obtaining signed informed consent, participants were interviewed in their preferred language (Dholuo, Kiswahili, or English) by a trained interviewer. Subsequently all women were offered voluntary HIV counselling and testing during the ANC visit, followed by post-test counseling and antiretroviral drugs for PMTCT for those who tested HIV-positive, as per Kenyan national guidelines [25]. Information on their acceptance of HIV testing and their test result were subsequently obtained from the women’s medical charts. Recruitment, baseline interviews and HIV testing took place between November 2007 and April 2009.
Measures
Stigma measures
To measure perceptions of HIV-related stigma at baseline, two stigma scales developed in sub-Saharan Africa were included in the survey. Anticipated stigma is the anticipation that one will personally experience specific types of stigma or discrimination if one is found to be HIV-positive and others learn of one’s HIV status. This type of stigma was measured by a nine-item scale originally developed in Botswana that also captures from whom they expected this stigma: male partner (break-up of relationship, physical abuse), family members (neglect, denial of care), or others (treatment as outcast, bad treatment at school or work, bad treatment by health workers, loss of friends, loss of job) [26]. Researchers in Botswana found this scale to have high internal reliability consistency (Cronbach’s alpha = 0.77) [26]. In the current study, a total anticipated stigma score was calculated by taking the mean of all responses for women who provided responses to at least 6 of the 9 scale items, and women who provided 5 or fewer responses were coded as missing. We furthermore created dichotomous measures of anticipated stigma for the different ‘sources’ of stigma. Given our previous analyses showing the importance of male partner stigma, as compared to other dimensions of stigma, as a predictor of HIV test refusal in this population [27], we chose this as our primary anticipated stigma variable. Analyses were conducted using all of the different anticipated stigma measures, but we chose to construct a more parsimonious model including the anticipated male stigma variable, which had the strongest relationship with the outcome.
To measure general attitudes and perceptions about persons living with HIV (PLWH) and how they are treated in their community, referred to as perceived community stigma in this paper [27], [28], we used a 22-item scale developed by Genberg et al. [29], [30] with items like ‘People living with HIV/AIDS deserve to be punished’ and ‘People living with HIV/AIDS in this community face rejection from their peers’. This scale was found to have high internal consistency validity and good divergent validity in both Thailand and Zimbabwe [30]. As reported elsewhere [27], internal-consistency reliability of these scales in our sample of pregnant women in Kenya was high (Cronbach’s alpha.86 for the anticipated stigma scale and.85 for the perceived community stigma scale).
Health facility birth attitude (HFBA) measure
To measure women’s perceived quality of care and attitudes towards giving birth at the health facility, we developed an 11-item scale derived from our previous qualitative research in Nyanza Province. In that study, we identified common beliefs and attitudes towards giving birth at the health facility assisted by a skilled healthcare provider versus giving birth at home assisted by a TBA, based on in-depth interviews with postpartum women, male partners, TBAs, and health workers [31]. This resulted in 11 statements with which women were asked to agree or disagree (coded 1 or 0). A total HFBA score was calculated by taking the mean score for women who provided responses to 8 or more scale items, and women who provided 7 or fewer responses were coded as missing, with a higher mean score indicating a more positive attitude towards giving birth at a health facility. The internal-consistency reliability of this score in this sample was found to be moderate (Cronbach’s α = .60), but acceptable for research in the early stages [32].
Other variables
The survey also included questions on socio-demographic characteristics. Questions that assessed knowledge regarding HIV transmission and prevention (for example, can a person get HIV by sharing a meal with someone who is infected?) were included and were used to construct a HIV knowledge index based on the number of items that were answered correctly. The primary outcome variables for our analyses of women’s intentions regarding childbirth were based on questions in which participants were asked where they intended to give birth and with what type of assistance. Participants were also asked about expected costs related to their delivery (transportation, supplies, medicines, fees). We considered giving birth in a health facility to be equivalent to giving birth with a skilled health care provider (although recognizing that the quality of birth attendance provided in health facilities may not be optimal) [33].
Statistical Analysis
Initial analyses were conducted using SPSS 16.0. [34]. With HFBA as the dependent variable, initial tests of bivariable associations were conducted using the Pearson’s Chi-square for nominal or ordinal variables, student T-test and ANOVA for continuous variables, and Kruskal-Wallis-test or the Mann-Whitney U-test for continuous variables with non-normal distributions. Following these initial analyses, HFBA was dichotomized into high and low, with the median (.73) chosen as a cut-off point. After conducting unadjusted logistic regression analyses to identify significant associations, we ran a mixed-effects logit model [35] using Stata 11 [36]. This multivariable model accounted for clustering by site and included variables that were significantly associated with the HFBA score in bivariable analyses (p<.05), as well as other variables that have been shown to be important for childbirth decision-making in the literature. Specifically, we included socio-economic factors including age, educational level, and occupation, as these factors related to women’s empowerment have been shown to be important factors in decision-making regarding childbirth in Kenya and similar countries [3], [37]. These analyses were repeated with a continuous version of the HFBA variable (normally transformed) to examine the potential impact of dichotomization on our results. Similar analytic methods were used to examine the predictors of intended type of assistance during delivery, in that variables found to have statistically significant relationships with the outcome in bivariable analyses (p<.05) were included in the multivariable model (education, occupation, being in a polygamous relationship, HFBA, expectations to pay for transport or supplies, and anticipated stigma), as well as household television ownership as a measure of wealth and access to mass media [38]. Binomial regression was used to obtain estimates of risk ratios for the multivariable analyses, with adjustment for clustering by site.
Finally, we conducted exploratory mediation analyses to examine if the effects of anticipated male partner HIV-related stigma on intended type of delivery might potentially operate through effects on HFBA. The conditions for mediation were met [39] as: 1) anticipated male partner stigma is significantly associated with HFBA, 2) HFBA independently predicts intended type of delivery assistance, and 3) the association of anticipated male partner stigma with intended type of birth assistance is reduced after adjustment for HFBA.
Results
Study Sample
Baseline interview data were available for 1,777 women (Table 1). Per Kenyan National Guidelines all women should have been offered HIV testing; however, no testing services were available for 203 (12%) of participants. During the study period, HIV testing services were sometimes unavailable at the study sites due to lack of HIV test kits, health worker absence, or other health system failures. Of the women for whom testing was available, 1,431 (94%) agreed to be tested, and 259 (18% of those tested) tested HIV-positive. Indicators of the women’s anticipations of stigma if they were to test positive for HIV are also presented in Table 1.
Table 1. Socio-demographic and HIV-related characteristics of MAMAS study participants (N = 1777).
| Variable | Mean (median, range) or N (%) |
| Mean age (median, range) | 23.58 (22, 18–49) |
| Mean number of pregnancies (median, range) | 3.22 (3, 1–16) |
| Education, n (%) | |
| Primary school (elementary) or less | 1483 (83.5) |
| Secondary school (high school) or more | 294 (16.5) |
| Religion, n (%) | |
| Roman Catholic | 331 (18.6) |
| Seventh Day Adventist | 582 (32.8) |
| Other | 862 (48.5) |
| Luo Ethnicity, n (%) | 1641 (92.3) |
| Currently married, n (%) | 1554 (87.5) |
| Currently living with male partner, n (%) | 1546 (87.0) |
| Male partner has other wives, n (%) (n = 1546) | 439 (28.4) |
| Occupation, n (%) | |
| Housework | 402 (22.7) |
| Selling things/fish monger | 355 (20.0) |
| Farming/agricultural work/manual labor | 742 (41.8) |
| Male partner’s occupation, n (%) (n = 1545) | |
| Selling things | 172 (11.1) |
| Farming/agricultural work | 586 (37.9) |
| Fishing | 188 (12.2) |
| Manual labor | 243 (15.7) |
| Household goods, n (%) | |
| Television | 187 (10.5) |
| Mobile phone | 839 (47.2) |
| Radio | 1330 (74.0) |
| HIV status1, n (%) | |
| Positive | 259 (14.7) |
| Negative | 1205 (68.2) |
| Refused testing | 99 (5.6) |
| Service not available | 203 (11.5) |
| Anticipated male partner stigma related to HIV | 627 (35.3) |
| Anticipated family stigma related to HIV | 621 (34.9) |
| Anticipated stigma from others related to HIV | 1051 (59.1) |
obtained from medical chart after the interview, based on offer of HIV testing during the first ANC visit.
Health Facility Birth Attitudes
Almost all participants agreed that giving birth at the health facility is safer than at home (97.9%), but there was more variability on items having to do with costs, interpersonal relations, and comfort (Table 2). Of note, 20% of women agreed that women who give birth at health facilities can be tested for diseases without their consent.
Table 2. Agreement on the 11 Health Facility Birth Attitude (HFBA) items (N = 1777).
| Variable | Agree, n (%) |
| Giving birth at a health facility is expensive. | 823 (48.3) |
| It is safer for a woman to give birth at a facility than at home. | 1738 (97.9) |
| During a birth, a TBA provides more comfort to a woman than a health worker (doctor or nurse) does. | 353 (20.3) |
| It is difficult to travel to a health facility if a woman goes into labor at night. | 825 (46.7) |
| Women who give birth at health facilities are often treated harshly by health workers | 287 (16.7) |
| A doctor or a nurse is better able to deal with problems that arise during childbirth than a TBA | 1719 (97.0) |
| It is acceptable for a woman to be assisted by a male doctor or nurse during childbirth | 1566 (88.6) |
| TBAs have more flexible arrangements for payment than do health facilities. | 558 (32.0) |
| Women who give birth at health facilities undergo a lot of procedures such as injections, stitches and surgery. | 1489 (84.6) |
| Women who give birth at health facilities may be tested for diseases without their consent. | 357 (20.2) |
| Childbirth goes faster with a TBA | 149 (8.6) |
After conducting unadjusted analyses to identify significant associations (Table 3), we ran a multivariable model, accounting for clustering by site including items that were significantly associated with the HFBA score, as well as other variables that have been shown to be important for childbirth decision-making in the literature. In these adjusted analyses, women who were married were more likely to have a high HFBA score, as were women with a high score on the HIV knowledge index (Table 4). Women who anticipated HIV-related stigma from their male partner had lower adjusted odds of having positive attitudes about giving birth at the health facility than women who did not anticipate such stigma. Repeating these analyses with a continuous (normally transformed) HFBA variable produced similar results, with anticipated male partner stigma, marital status, and the HIV knowledge index having strong significant adjusted relationships with HFBA, but with occupation and television ownership also retaining significance in the adjusted model (data not shown).
Table 3. Unadjusted logistic regression of predictors of health facility birth attitude (n = 1759).
| Variable | Low HFBA Score (N = 919) | High HFBA Score (N = 840) | OR (95%CI) for a high HFBA score |
| Mean age (median, range) | 23.64 (22, 18–43) | 23.58 (22, 18–49) | 0.998 (0.981–1.015) |
| Mean parity (median, range) | 3.27 (3, 1–16) | 3.21 (3, 1–12) | 0.986 (0.942–1.032) |
| Education : primary or less vs. (more than) secondary | 762 (82.9) | 709 (84.4) | 1.115 (0.865–1.437) |
| Religion: 7th Day Adventist vs. other | 307(33.4) | 266 (31.7) | 0.925 (0.758–1.130) |
| Ethnicity: Luo vs other ethnicities | 845 (91.9) | 778 (92.6) | 1.099(0.773–1.561) |
| Marital status : currently married vs. notcurrently married | 790 (86.1) | 753 (89.6) | 1.402 (1.049–1.874)* |
| Currently living with male partner | 795 (86.6) | 741 (88.2) | 0.864 (0.651–1.146) |
| In a polygamous relation | 237 (25.8) | 199 (23.7) | 0.892 (0.718–1.108) |
| Occupation: farming vs other occupation | 439 (47.9) | 376 (44.8) | 0.882 (0.731–1.065) |
| Male occupation (n = 1535): farming vs other occupation | 294 (37.0) | 288 (38.9) | 1.081 (0.880–1.329) |
| Household utilities: | |||
| Radio | 678 (73.8) | 640 (76.2) | 1.446 (0.868–2.411) |
| Television | 113 (12.3) | 73 (8.7) | 1.473 (1.080–1.009)* |
| Cell phone | 447 (48.6) | 385 (45.8) | 1.119 (0.928–1.350) |
| Mean HIV knowledge index score (n = 1715)(median, range) | 0.87 (0.91, 0.27–1) | 0.90 (0.91, 0.45–1) | 7.917 (3.285–19.080)** |
| Mean anticipated stigma score (n = 1697)(median, range) | 0.32(0.22, 0–1) | 0.22 (0.11, 0–1) | 0.309 (0.221–0.432)** |
| Anticipated stigma from male partner1 | 375 (40.8) | 245 (29.2) | 0.591 (0.483–0.724)** |
| Anticipated stigma from family2 | 390 (42.4) | 228 (27.1) | 0.491 (0.400–0.601) ** |
| Anticipated stigma from others3 | 598 (65.1) | 444 (52.9) | 0.598 (0.490–0.729)** |
| Mean perceived community stigma score (n = 1690)(median, range) | 0.88 (0.89, 0–2.35) | 0.79 (0.83, 0–2.39) | 0.540 (0.415–0.703) ** |
120 participants refused to answer.
87 participants refused to answer.
78 participants refused to answer.
p<.05.
p<.01.
Table 4. Predictors of a Positive Attitude towards Delivery in a Health Facility (high HFBA score) (n = 1636) – multivariate model accounting for clustering by sitea,b.
| Variable | Number of women in the category (n) | Adjusted Odds Ratio (OR) for morepositive attitude towards the HF (95% CI)a | Adjusted Risk Ratio (RR) for more positive attitude towards the HF (95% CI)b |
| Age (years) | 1636 | 0.988 (0.969–1.007) | 0.997 (0.989–1.006) |
| Primary or less education | 1365 | 0.889 (0.660–1.198) | 1.024 (0.873–1.201) |
| Farmer vs. other occupation | 787 | 0.806 (0.642–1.011) | 0.930 (0.783–1.106) |
| Currently married | 1434 | 1.658 (1.20–2.289)** | 1.17 (0.985–1.401) |
| Having a television | 175 | 0.757 (0.533–1.076) | 0.806 (0.756–0.860)** |
| HIV knowledge index score | 1636 | 10.775 (4.098–28.331)** | 3.51 (1.708–7.232)** |
| Anticipated male partner stigma | 618 | 0.627 (0.505–0.779)** | 0.788 (0.704–0.882)** |
p<.05.
p<.01.
Odds ratios (ORs) were calculated using mixed effects logistic regression adjusted for clustering by site.
Risk ratios (RRs) were calculated using binomial regression adjusted for clustering by site.
Intended Type of Assistance during Delivery
Women with a low HFBA score had five times the odds of saying that they intended to deliver at home than women with a high HFBA score, as compared to women with a high HFBA score (OR 5.15, 95% CI 2.70–9.84). Examination of the individual anticipated stigma items revealed that women who feared bad treatment by health workers if they tested HIV-positive had two times higher odds of intending to deliver at home (OR 2.02, 95%CI 1.09–3.76) and those who anticipated male partner stigma had 1.6 times higher odds (OR 1.69, 95%CI 1.01–2.59). In a multivariable model for intended type of assistance during delivery (Table 5), women who expected to pay for transport or supplies had lower adjusted odds of intending to deliver at home. In contrast, women who had a low HFBA score or a low level of education had significantly higher adjusted odds of intending to have a home delivery.
Table 5. Predictors of the Intention to Deliver with a Traditional Birth Attendant (TBA) vs. a Skilled healthcare provider (n = 1562) - multivariate model accounting for clustering by sitea,b,c.
| Variable | Number of women in the category (n) | Adjusted Odds Ratio (OR) for theintention to deliver with a TBA (95% CI)a | Adjusted Risk Ratio (RR) for the intention to deliver with a TBA (95% CI)b |
| Primary or less education | 1301 | 4.944 (1.116–21.903)* | 4.104 (1.503–11.201)** |
| Farmer vs. other occupation | 742 | 1.359 (0.726–2.543) | 1.290 (0.594–2.800) |
| Polygamous relationship | 390 | 1.073 (0.593–1.943) | 1.001 (0.788–1.274) |
| Having a television | 169 | 0.675 (0.182–2.51) | 0.733 (0.283–1.902) |
| Expects to pay for transport | 672 | 0.203 (0.080–0.512)** | 0.247 (0.090–0.680)** |
| Expects to pay for supplies | 1091 | 0.087 (0.043–0.174)** | 0.140 (0.056–0.350)** |
| Low HFBA score | 820 | 5.559 (2.686–11.506)** | 6.001 (3.847–9.361)** |
| Anticipated male partner stigma | 591 | 1.205 (0.683–2.125) | 1.330 (1.157–1.529)** |
p<.05.
p<.01.
Odds ratios (ORs) were calculated using mixed effects logistic regression adjusted for clustering by site.
Risk ratios (RRs) were calculated using binomial regression adjusted for clustering by site.
Analysis includes women who expressed an intention to deliver with a TBA or a skilled healthcare provider.
We also examined responses to another variable in our dataset, “HIV-positive women who give birth at health facilities are likely to have their HIV status revealed to their husband/partner or others in the community” (agree or disagree). Overall, 57% of women agreed with this item. This variable was significantly associated with intention for home birth (p = .001), with those women agreeing with this statement being more likely to intend a home birth. In stratified analyses we found that for those women who anticipated male partner stigma, this variable was significantly associated with intention for home birth (p = .001), whereas for those who did not anticipate male partner stigma, there was not a significant association (p = .448).
Mediation Analyses
We conducted exploratory mediation analyses to examine if the effects of anticipated male partner HIV-related stigma on intended type of delivery might potentially operate through effects on health facility birth attitudes. In unadjusted analysis, anticipating stigma from a partner had an odds ratio of 1.62 (p = .045) for intending to deliver with a TBA. After adjusting for HFBA, the odds ratio decreased to 1.35 and became non-significant (p = .22). This suggests that HIV-related stigma may not directly influence the intended type of assistance during delivery, but operates indirectly as an important factor shaping attitudes toward giving birth at the health facility (Figure 1).
Figure 1. Relationships among HIV-related stigma, HFBA and intended type of assistance during delivery.
Discussion
Both women’s attitudes about giving birth in a health facility and their anticipations of HIV-related stigma may be key factors in decision-making for the type of assistance for delivery in high HIV prevalence settings. We found that among pregnant women in rural Kenya, anticipations of HIV-related stigma were associated with a less positive attitude towards giving birth at the health facility. Data from this study, as well as from other studies in East Africa, support the idea that this is linked to women’s perception of the lack of confidentiality at the health facility, resulting in fears that their male partner, family, and community members will learn about their HIV testing and serostatus; potentially resulting in stigma, discrimination, and even violence[40]–[42].
Furthermore, our analyses showed that women’s attitude towards giving birth at a health facility (as measured by the HFBA) was strongly associated with the woman’s intended place of childbirth. Although we cannot make causal inferences based on these cross-sectional data, our analyses suggest that that HIV-related stigma may be an important factor influencing women’s feelings about giving birth at the health facility. As we show that women’s attitudes towards the health facility strongly influence their intentions regarding where they will give birth, reducing HIV-related stigma might tilt the balance in favor of more positive attitudes towards facility-based childbirth.
In addition to the role of HIV-related stigma, we found that women who were currently married had a more positive attitude towards facility-based childbirth than women who were not. Unmarried pregnant women may have a negative attitude towards facility-based childbirth if they perceive that healthcare providers have negative attitudes toward sexual activity and childbearing among single women [43]. It is notable that women who expected to pay for transport and/or supplies related to childbirth had lower adjusted odds of intending to deliver at home, in a setting where lack of money is often mentioned as a barrier for delivering at the health facility. This expectation is therefore most likely not a measure of the ability to pay these costs, but of how well-informed women are about the expenses related to delivering at a health facility.
While at least one ANC visit is the norm for most women in sub-Saharan Africa and acceptance of HIV testing in ANC has increased greatly in many settings due to health worker training and opt-out approaches to HIV testing [23], [44], childbirth in a health facility is still relatively uncommon in rural Kenya. In a similar setting in Tanzania, researchers found that health workers’ emphasis on PMTCT during ANC visits resulted in neglecting to communicate the importance of delivering at the health facility for both HIV negative and positive women [45]. In our qualitative data from this rural Kenyan setting, we learned that many people view giving birth in a health facility as only necessary for women who have serious complications (like HIV) and thus those who give birth in health facilities may run the risk of being assumed to be HIV-positive and suffering from HIV-related stigma [46]. Another effect of emphasizing HIV during ANC visits may be that it increases awareness among women and thereby increases fears of disclosure and stigma.
The current study has several limitations. We only interviewed women who visited the ANC by their seventh month of pregnancy. It is possible that women who do not visit the health facility at all or visit only very late in pregnancy have more negative attitudes towards giving birth at the health facility. However, it would not have been feasible to locate and conduct this research with a community-based sample of pregnant women. Given that 92% of all pregnant women have at least one ANC visit during pregnancy in rural Nyanza [3], our sample is relatively representative. Additionally, we were only able to show a relationship between HIV-related stigma, health facility birth attitudes and the intended type of assistance during delivery with these data, but not with the actual type of assistance. It might well be that factors such as lack of decision-making autonomy, lack of money, or the difficulty of transport are more important barriers, and that intentions are not related to actual behavior. However, in longitudinal follow-up of a sub-sample of these women, of those who intended to deliver at home 83% actually did deliver at home, compared to 64% of those who did not intend to deliver at home (p = .055) [47]. Thus women who specifically state that they intend to give birth at home are in fact highly likely to do so. Another limitation is the moderate level of the internal-consistency reliability of the new 11-item HFBA score in this sample. However, this disadvantage is balanced by the strong grounding of the scale items in the cultural context based on qualitative data, as well as the predictive power of this scale vis-a-vis the outcome variables we examined. Although we chose to dichotomize this variable at the median for our primary analyses for ease of interpretation, we recognize that this resulted in loss of information and reduced statistical power. Futhermore, although we adjusted for many important factors in our analyses, there is still the possibility that some other unmeasured confounding variable is responsible for the significant associations we found. Finally our mediation analyses were only exploratory, as they were based on cross-sectional data and we did not adjust for potential confounders between the mediator and the outcome.
Conclusions
Our study supports the combination of strategies to reduce HIV transmission and prevent maternal and infant mortality [1]. In particular, our findings suggest that working with maternity care providers to increase confidentiality and reduce HIV-related stigma and discrimination, as well as involvement of male partners, could have beneficial effects on women’s utilization of facility-based childbirth services. Interventions for HIV-related stigma reduction might not only reduce stigma but may also result in more women choosing to deliver with a skilled healthcare provider in a health facility. This in turn could contribute to reducing the level of unsafe births and maternal/infant mortality, as well as providing more opportunities for PMTCT. We suggest that future research should further investigate the important role of HIV-related stigma in decision-making around place of delivery in rural settings in Sub-Saharan Africa.
Acknowledgments
We thank the Kenyan women who participated in the study and shared their experiences with us. We acknowledge the important logistical support of the KEMRI-UCSF Collaborative.
Group and especially Family AIDS Care and Education Services (FACES). We thank the FACES Community Clinic Health Assistants (CCHAs) in Migori and Rongo for their diligent work in collecting the data. We gratefully acknowledge the Director of KEMRI and the Director of KEMRI’s Centre for Microbiology for their support in conducting this research and for permission to publish this manuscript.
Funding Statement
The authors thank the Marco Polo Fonds, the Groninger Universiteitsfonds, the J.K. de Cock Stichting (www.decockstichting.nl) and the Hendrik Muller Vaderlandsch Fonds (www.mullerfonds.nl) for supporting the work of José Medema-Wijnveen. The project described was supported by Award Number K01MH081777 from the National Institute of Mental Health (NIMH), National Institutes of Health (NIH). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Abdool-Karim Q, Abouzahr C, Dehne K, Mangiaterra V, Moodley J, et al. (2010) HIV and maternal mortality: Turning the tide Lancet. 375: 1948–1949. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (1999) Reducing maternal mortality. A joint statement by WHO/UNFPA/UNICEF/World Bank. Available at: http://www.unfpa.org/upload/lib_pub_file/236_filename_e_rmm.pdf. Accessed October 5th, 2012.
- 3.Kenya National Bureau of Statistics (KNBS), ICF Macro (2010) Demographic and health survey 2008–2009 Kenya. Available at: http://www.measuredhs.com/pubs/pdf/fr229/fr229.pdf. Accessed October 5th, 2012.
- 4.World Health Organization (2010) Trends in maternal mortality: 1990 to 2008. Available at: http://whqlibdoc.who.int/publications/2010/9789241500265_eng.pdf. Accessed October 5th, 2012.
- 5. Amooti-Kaguna B, Nuwaha F (2000) Factors influencing choice of delivery sites in rakai district of uganda Social Science & Medicine (1982). 50: 203–213. [DOI] [PubMed] [Google Scholar]
- 6. Bazzano AN, Kirkwood B, Tawiah-Agyemang C, Owusu-Agyei S, Adongo P (2008) Social costs of skilled attendance at birth in rural Ghana International Journal of Gynaecology and Obstetrics. 102: 91–94. [DOI] [PubMed] [Google Scholar]
- 7.Family Care International Kenya (2007) Testing approaches for increasing skilled care during childbirth: Key findings from Homabay and Migori districts, Kenya. Available at: http://www.familycareintl.org/UserFiles/File/SCI%20Kenya%20Summary%20Report%20-%2030Oct07.pdf. Accessed October 5th, 2012.
- 8. Gabrysch S, Campbell OM (2009) Still too far to walk: Literature review of the determinants of delivery service use BMC Pregnancy and Childbirth. 9: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gage AJ (2007) Barriers to the utilization of maternal health care in rural Mali Social Science & Medicine (1982). 65: 1666–1682. [DOI] [PubMed] [Google Scholar]
- 10. Gyimah SO, Takyi BK, Addai I (2006) Challenges to the reproductive-health needs of african women: On religion and maternal health utilization in Ghana Social Science & Medicine (1982). 62: 2930–2944. [DOI] [PubMed] [Google Scholar]
- 11. Nangendo SM (2006) Factors affecting the use of modern prenatal and maternity services in got agulu sub-location western kenya African Study Monographs. 27: 145–156. [Google Scholar]
- 12. Stanton C, Blanc AK, Croft T, Choi Y (2007) Skilled care at birth in the developing world: Progress to date and strategies for expanding coverage Journal of Biosocial Science. 39: 109–120. [DOI] [PubMed] [Google Scholar]
- 13. Stephenson R, Baschieri A, Clements S, Hennink M, Madise N (2006) Contextual influences on the use of health facilities for childbirth in africa American Journal of Public Health. 96: 84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van Eijk AM, Bles HM, Odhiambo F, Ayisi JG, Blokland IE, et al. (2006) Use of antenatal services and delivery care among women in rural western Kenya: A community based survey Reproductive Health. 3: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wild K, Barclay L, Kelly P, Martins N (2010) Birth choices in Timor-Leste: A framework for understanding the use of maternal health services in low resource settings Social Science & Medicine (1982). 71: 2038–2045. [DOI] [PubMed] [Google Scholar]
- 16. Kasenga F, Hurtig AK, Emmelin M (2010) HIV-positive women’s experiences of a PMTCT programme in rural malawi Midwifery. 26: 27–37. [DOI] [PubMed] [Google Scholar]
- 17. Mbaruku G, Msambichaka B, Galea S, Rockers PC, Kruk ME (2009) Dissatisfaction with traditional birth attendants in rural Tanzania International Journal of Gynaecology and Obstetrics. 107: 8–11. [DOI] [PubMed] [Google Scholar]
- 18. Danforth EJ, Krukz ME, Rockers PC, Mbaruku G, Galea S (2009) Household decision-making about delivery in health facilities: Evidence from tanzania Journal of Health, Population, and Nutrition. 27: 696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kruk ME, Paczkowski MM, Tegegn A, Tessema F, Hadley C, et al. (2010) Women’s preferences for obstetric care in rural ethiopia: A population-based discrete choice experiment in a region with low rates of facility delivery Journal of Epidemiology and Community Health. 64: 984–988. [DOI] [PubMed] [Google Scholar]
- 20. Nyblade L, Stangl A, Weiss E, Ashburn K (2009) Combating HIV stigma in health care settings: What works? Journal of the International AIDS Society 12: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Turan JM, Miller S, Bukusi EA, Sande J, Cohen CR (2008) HIV/AIDS and maternity care in kenya: How fears of stigma and discrimination affect uptake and provision of labor and delivery services AIDS Care. 20: 938–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Turan JM, Bukusi EA, Cohen CR, Sande J, Miller S (2008) Effects of HIV/AIDS on maternity care providers in Kenya Journal of Obstetric, Gynecologic, and Neonatal Nursing. 37: 588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ujiji OA, Rubenson B, Ilako F, Marrone G, Wamalwa D, et al. (2011) Is ‘opt-out HIV testing’ a real option among pregnant women in rural districts in Kenya? BMC Public Health 11: 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Otieno PA, Kohler PK, Bosire RK, Brown ER, Macharia SW, et al. (2010) Determinants of failure to access care in mothers referred to HIV treatment programs in Nairobi, Kenya AIDS Care. 22: 729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.NASCOP (2002) National guidelines: Prevention of mother-to-child HIV/AIDS transmission (PMCT), 2nd edition. Avalaible at: http://nascop.or.ke/library/pmtct/PMTCT%20Guideline-March%202010.pdf. Accessed: October 5th, 2012.
- 26. Weiser SD, Heisler M, Leiter K, Percy-de Korte F, Tlou S, et al. (2006) Routine HIV testing in Botswana: A population-based study on attitudes, practices, and human rights concerns PLoS Medicine. 3: e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Turan JM, Bukusi EA, Onono M, Holzemer WL, Miller S, et al. (2011) HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: Results from the MAMAS study AIDS and Behavior. 15: 1111–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, et al. (2008) HIV-related stigma: Adapting a theoretical framework for use in india Social Science & Medicine (1982). 67: 1225–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Genberg BL, Hlavka Z, Konda KA, Maman S, Chariyalertsak S, et al. (2009) A comparison of HIV/AIDS-related stigma in four countries: Negative attitudes and perceived acts of discrimination towards people living with HIV/AIDS Social Science & Medicine (1982). 68: 2279–2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Genberg BL, Kawichai S, Chingono A, Sendah M, Chariyalertsak S, et al. (2008) Assessing HIV/AIDS stigma and discrimination in developing countries AIDS and Behavior. 12: 772–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Turan JM, Miller S, Bukusi EA, Sande J, Cohen CR (2008) HIV/AIDS and maternity care in Kenya: How fears of stigma and discrimination affect uptake and provision of labor and delivery services AIDS Care. 20: 938–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Switzer GE, Wisniewski SR, Belle SH, Dew MA, Schultz R (1999) Selecting, developing, and evaluating research instruments Social Psychiatry and Psychiatric Epidemiology. 34: 399–409. [DOI] [PubMed] [Google Scholar]
- 33.Miller S, Cordero M, Coleman AL, Figueroa J, Brito-Anderson S, et al.. (2003) Quality of care in institutionalized deliveries: The paradox of the dominican republic International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics 82: 89–103; discussion 87–8. [DOI] [PubMed]
- 34.SPSS Inc (2008) SPSS for windows release 16.0.2.
- 35.Vittinghof E, Glidden DV, Shiboski SC, McCulloh CE (2005) Repeated measures analysis In: Anonymous Regression methods in biostatistics New York, USA: Springer Science+Business Media, Inc.
- 36.StataCorp (2009) Stata statistical software: Release 11.
- 37. Ahmed S, Creanga AA, Gillespie DG, Tsui AO (2010) Economic status, education and empowerment: Implications for maternal health service utilization in developing countries. PloS One 5: e11190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kenya National Bureau of Statistics (KNBS), ICF Macro (2010) Demographic and health survey 2008–2009 kenya 2011.
- 39. Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations Journal of Personality and Social Psychology. 51: 1173–1182. [DOI] [PubMed] [Google Scholar]
- 40. Awiti Ujiji O, Ekstrom AM, Ilako F, Indalo D, Wamalwa D, et al. (2011) Reasoning and deciding PMTCT-adherence during pregnancy among women living with HIV in kenya Culture, Health & Sexuality. 13: 829–840. [DOI] [PubMed] [Google Scholar]
- 41. Peltzer K, Phaswana-Mafuya N, Treger L (2009) Use of traditional and complementary health practices in prenatal, delivery and postnatal care in the context of HIV transmission from mother to child (PMTCT) in the Eastern cape, South Africa African Journal of Traditional, Complementary, and Alternative Medicines : AJTCAM/African Networks on Ethnomedicines. 6: 155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Thorsen VC, Sundby J, Martinson F (2008) Potential initiators of HIV-related stigmatization: Ethical and programmatic challenges for PMTCT programs Developing World Bioethics. 8: 43–50. [DOI] [PubMed] [Google Scholar]
- 43. Gage AJ (1998) Premarital childbearing, unwanted fertility and maternity care in kenya and namibia Population Studies. 52: 21–34. [Google Scholar]
- 44. Byamugisha R, Tumwine JK, Ndeezi G, Karamagi CA, Tylleskar T (2010) Attitudes to routine HIV counselling and testing, and knowledge about prevention of mother to child transmission of HIV in eastern Uganda: A cross-sectional survey among antenatal attendees Journal of the International AIDS Society. 13: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Magoma M, Requejo J, Campbell OM, Cousens S, Filippi V (2010) High ANC coverage and low skilled attendance in a rural Tanzanian district: A case for implementing a birth plan intervention BMC Pregnancy and Childbirth. 10: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Turan JM, Hatcher AH, Medema-Wijnveen JS, Onono M, Miller S, et al. (2012) The role of HIV-related stigma in utilization of skilled childbirth services in rural kenya: A prospective mixed-methods study. PLoS Med. 9(8): e1001295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Medema-Wijnveen JS, Onono M, Bukusi EA, Miller S, Cohen CR, et al.. (2011) “HIV/AIDS stigma and attitudes towards giving birth at a health facility among pregnant women in rural Kenya” 2011. Paper presented at: The International AIDS Society Conference; 2011 July 17–20; Rome, Italy.