Abstract
Purpose
Compare speech perception and localization in subjects who wear one cochlear implant (unilateral CI) or one cochlear implant and hearing aid (CI+HA) and then receive a second cochlear implant (bilateral CI); and to evaluate the importance of the duration between implant surgeries and duration of deafness.
Method
Nine subjects were tested on speech perception in quiet and 13 subjects were tested on speech perception and localization in noise using an array of eight-loudspeakers. All subjects were tested with unilateral CI prior to bilateral implantation and then again with bilateral CI after at least 3 months of bilateral experience.
Results
No significant difference was found between bilateral CI and unilateral CI on averaged speech perception in quiet performance. A significant benefit was found for bilateral CI on averaged speech perception in noise and on localization. Non-significant correlations were found for duration between surgeries, duration of deafness, and duration of bilateral use.
Conclusions
Improvements for speech perception and localization played in background noise were indicated for most subjects after they received their second implant. The correlations should be re-assessed with a larger number of subjects to appropriately evaluate the effects of duration between surgeries, duration of deafness, and duration of bilateral use.
Keywords: adult, sequential bilateral cochlear implants, localization, speech perception
Introduction
The number of profoundly deafened individuals receiving bilateral cochlear implants and the literature studying the benefits of bilateral cochlear implants continues to grow (e.g. Buss et al., 2008; Firstz, Reeder, & Skinner, 2008; Litovsky, Parkinson, Arcaroli, & Sammeth, 2006; Laszig et al., 2004; Tyler, Noble, Dunn, & Witt, 2006; Tyler Perreau & Ji, 2009; Noble, Tyler, Dunn & Bhullar, 2008 a, b). According to the Food and Drug Administration, there are over 219,000 adults and children worldwide with cochlear implants (NIDCD, 2010). Of the individuals with unilateral devices, many are being evaluated to determine candidacy for a second cochlear implant in the opposite ear.
One question often asked by patients and researchers alike is whether a CI user who is accustomed to processing sound unilaterally for many years can integrate stimulation from the opposite ear once they receive a second cochlear implant. This question is critical because of the large population of unilateral patients and the growing interest in sequential bilateral implantation. Additionally, many of these users will have several years duration between receiving their first and second implants and, as a result, might have different internal arrays, number of channels, rate, and signal processing strategies between devices. These mismatches between device processing could produce different representations of the signal, resulting in poor bilateral benefits. Dorman and Dahlstrom (2004) studied performance for two subjects using a Med El CIS-Link processor in one ear and an Advanced Bionics Hi-Focus electrode in the other ear with duration between implants of 10 and 16 years. Performance was measured on words in quiet and sentences in noise. Both subjects showed a binaural advantage on speech perception scores in noise and one showed an advantage in quiet. Tyler, Noble, Dunn, and Witt (2007) observed similar results in a study of seven subjects with a range of time between sequential implant surgeries of 6 to 17 years. Three of seven subjects had devices manufactured by two different companies. Only two subjects had an equal number of frequency channels across ears, and only one subject had an equal stimulation rate. Performance was evaluated on three tasks: words in quiet, sentences in noise (noise facing front, right, and left), and localization. They found that all subjects received a bilateral advantage on at least one of the speech perception tests and five subjects scored better than chance performance on localization. In addition, nearly all subjects showed individual ear differences on speech perception tests with the ear implanted first performing better. Analogous results from a multi-center trial that included 30 sequentially-implanted subjects (range of time between sequential implant surgeries of 1 to 7 years) showed a significant binaural advantage on sentences in noise when adding the second ear with noise emanating from the front versus when the noise was ipsilateral to the first cochlear implant (Ramsden et al., 2005). Subjects were implanted with the same devices between the two ears. When tested with one implant alone, performance was significantly worse using the second cochlear implant compared to the first cochlear implant. These results indicate that subjects can benefit from receiving a second cochlear implant even when different devices are used on each ear and with long durations between implant surgeries.
Additional results evaluating the benefits of sequential bilateral implants are reported in the literature, but are combined with data from simultaneously implanted users. Research from these studies also shows that many subjects are capable of taking advantage of many bilateral benefits, such as the binaural summation effect, and to a lesser degree, the binaural squelch effect. In addition, most are able to more easily take advantage of the physical effect of the head shadow. Schleich, Nopp, and D’Haese (2004) studied bilateral benefits in 21 subjects, among which 18 were sequentially implanted. Averaged results indicated that the subjects gained a 6.8 dB significant improvement in sentence perception in noise due to the head shadow effect, while a non-significant change was measured due to the binaural squelch and binaural summation effects. Laszig et al. (2004) reported similar results after studying 37 subjects (15 were sequentially implanted). They found that all 15 subjects with sequential bilateral CIs benefited from the head shadow effect, producing a 10 to 11.4 dB advantage and half of those benefitted from the binaural squelch effect. Additionally, Schön, Müller, and Helms (2002) reported binaural improvements for six sequentially-implanted subjects and three simultaneously-implanted subjects, showing an average of approximately four dB improvement in signal-to-noise ratio on sentence perception. Thus, while results are not parsed out for those sequentially and simultaneously implanted, in general, the results indicate that users with bilateral cochlear implants benefit from two devices. These results are also consistent in children implanted bilaterally with sequential devices (e.g. Peters, Litovsky, Parkinson, & Lake, 2007).
A potential bias of these studies is that benefits from bilateral devices were determined by comparing the bilateral condition to a unilateral condition where one device is removed. It has been suggested that removing a single CI puts the unilateral condition at an unfair disadvantage because of the lack of everyday unilateral experience (Dunn, Tyler, Oakley, Gantz, & Noble, 2008). Nonetheless, very few studies have reported on the performance differences of sequential bilateral cochlear implant users by comparing performance with only one implant to that after they have received a second cochlear implant in a sequential surgical procedure. Zeitler, Kessler, Terushkin et al. (2008) examined the impact of length of deafness and duration between surgeries on speech perception performance preoperatively before the second implantation and at 3 months postoperatively on 43 children and 22 adults implanted sequentially. Group results showed significant improvements in speech perception with the second implanted ear used alone and in the bilateral condition. There was no effect of length of deafness or duration between surgeries.
The aim of this study was to determine if there are benefits of sequential implantation on speech perception in quiet, speech perception in spatially separated noise using an array of loudspeakers, and on localization performance. Data were collected on subjects before and after they received their second implant contralateral to the first implant. A secondary aim was to evaluate the effects of duration between implantation and duration of deafness on speech perception and on localization.
Methods
Subjects
Thirteen post-lingually deafened adults who received sequential bilateral cochlear implants participated in this study. Prior to sequential implantation, three subjects wore a hearing aid on their non-implanted ear (CI+HA) and 10 wore a cochlear implant only (unilateral CI). Subjects were tested prior to receiving their second cochlear implant (unilateral CI or CI+HA; average of 80 months unilateral experience) and then tested again after receiving the second cochlear implant (bilateral CI; average of 6.5 months bilateral experience). For the subjects who wore CI+HA, we chose to allow them to use the hearing aid in our studies as we felt that this would be the most natural listening situation for them. Those subjects have been indicated in Table. From here forward, we refer to ‘unilateral CI’ to indicate both CI+HA subjects and subjects using only one CI prior to sequential surgeries. In the discussion, we will discuss any potential differences in performance due to the CI+HA configuration.
The average time between the first and second cochlear implant surgeries was 74 months (SD=34.9). Three subjects were implanted with Clarion devices (Advanced Bionics Corporation, Sylmar, CA, USA); four were implanted with Nucleus devices (Cochlear Corporation, Lane Cove NSW, Australia); and six were implanted with Med-El devices (Med-El, Innsbruck, Austria). The subjects with Nucleus and Clarion devices received their audiological care at our center and the subjects with Med-EL devices received their audiological care at other facilities and traveled to our center for testing purposes. The average duration of deafness (time between age at becoming profoundly deaf and age at first implantation) for all 13 subjects was 11 years (SD=13.8). The cochlear implant type and programming parameters are presented in Table 1. Demographic information for these individuals is presented in Table 2.
Table 1.
Cochlear implant processor and programming parameters for each visit on the specific ear.
| Subject ID | Test Condition | Processor | Strategy; # of Channels |
Rate (pps) | Ear |
|---|---|---|---|---|---|
| Visit 1: CI-ONLY | Cochlear Freedom | ACE; 24 | 900 Hz | Right | |
| C53B | Visit 2: (1st implant) | Cochlear Freedom | ACE; 24 | 900 Hz | Right |
| Visit 2: (2nd implant) | Cochlear Freedom | ACE; 24 | 900 Hz | Left | |
| Visit 1: CI-ONLY | Cochlear Freedom | ACE; 24 | 900 Hz | Right | |
| C41B | Visit 2: (1st implant) | Cochlear Freedom | ACE; 24 | 900 Hz | Right |
| Visit 2: (2nd implant) | Cochlear Freedom | ACE; 24 | 900 Hz | Left | |
| Visit 1: CI-ONLY | Med-EL Tempo+ | CIS+; 9 | 1993 Hz | Right | |
| M55B | Visit 2: (1st implant) | Med-EL Tempo+ | CIS+; 9 | 1993 Hz | Right |
| Visit 2: (2nd implant) | Med-EL Opus II | CIS+; 11 | 580 Hz | Left | |
| Visit 1: CI-ONLY | AB Auria | Hi Resolution-Sequential; 11 | 2109 Hz | Left | |
| A66B | Visit 2: (1st implant) | AB Harmony | Hi Resolution-Sequential; 11 | 2109 Hz | Left |
| Visit 2: (2nd implant) | AB Harmony | Hi Resolution-Sequential; 11 | 2109 Hz | Right | |
| Visit 1: CI-ONLY | Med-EL Tempo+ | CIS+; 9 | 1212 Hz | Left | |
| M13B | Visit 2: (1st implant) | Med-EL Tempo+ | CIS+; 9 | 1212 Hz | Left |
| Visit 2: (2nd implant) | Med-EL Opus II | CIS+; 11 | 565 Hz | Right | |
| Visit 1: CI-ONLY | Med-EL Opus II | CIS+; 8 | 2000 Hz | Right | |
| M76B | Visit 2: (1st implant) | Med-EL Opus II | CIS+; 8 | 2000 Hz | Right |
| Visit 2: (2nd implant) | Med-EL Opus II | CIS+; 12 | 1613 Hz | Left | |
| Visit 1: CI-ONLY | Med-EL Tempo+ | CIS+; 12 | 1081 Hz | Left | |
| M83B | Visit 2: (1st implant) | Med-EL Tempo+ | CIS+; 12 | 819 Hz | Left |
| Visit 2: (2nd implant) | Med-EL Opus II | CIS+; 9 | 673 Hz | Right | |
| Visit 1: CI+HA | Nucleus 3G | ACE; 20 | 900 Hz | Right | |
| C34B | Visit 2: (1st implant) | Cochlear Freedom | ACE; 20 | 900 Hz | Right |
| Visit 2: (2nd implant) | Cochlear Freedom | ACE; 20 | 900 Hz | Left | |
| Visit 1: CI+HA | AB Harmony | Fidelity; 9 | 1904 Hz | Right | |
| A69B | Visit 2: (1st implant) | AB Harmony | Fidelity; 9 | 1904 Hz | Right |
| Visit 2: (2nd implant) | AB Harmony | Fidelity; 13 | 3712 Hz | Left | |
| Visit 1: CI-ONLY | Nucleus 3G | ACE; 22 | 1200 Hz | Right | |
| C10B | Visit 2: (1st implant) | Cochlear Freedom | ACE; 22 | 1200 Hz | Right |
| Visit 2: (2nd implant) | Cochlear Freedom | ACE; 22 | 900 Hz | Left | |
| Visit 1: CI+HA | Med-EL Tempo+ | CIS+; 12 | 1363 Hz | Right | |
| M53B | Visit 2: (1st implant) | Med-EL Tempo+ | CIS+; 12 | 1363 Hz | Right |
| Visit 2: (2nd implant) | Med-EL Opus II | FSP; 12 | 997 Hz | Left | |
| Visit 1: CI-ONLY | Med-EL Opus II | FSP; 12 | 1818 Hz | Left | |
| M68B | Visit 2: (1st implant) | Med-EL Opus II | FSP; 12 | 1818 Hz | Left |
| Visit 2: (2nd implant) | Med-EL Opus II | FSP; 12 | 1961 Hz | Right | |
| Visit 1: CI-ONLY | Clarion PSP | CIS; 8 | 812 Hz | Right | |
| A32B | Visit 2: (1st implant) | Clarion PSP | CIS; 8 | 812 Hz | Right |
| Visit 2: (2nd implant) | AB Harmony | Fidelity; 15 | 3712 Hz | Left | |
Visit 1=testing with CI-ONLY or CI+HA. Visit 2=testing with CI+CI.
1st implant=ear implanted first. 2nd implant=ear implanted second.
Table 2.
Subject gender, age at first implantation, etiology, duration between surgeries, duration of bilateral use, and duration of deafness demographic information.
| Subject ID | Gender (M=Male; F=Female) |
Age at 1st Implantation (years) |
Etiology (R=Right; L=Left) |
Duration between 1st and 2nd CI (years) |
Duration of bilateral use (years) |
Duration of deafness (years) |
|---|---|---|---|---|---|---|
| C53B | F | 45 | UNK | 1.9 | 0.5 | 0.2 |
| C41B | M | 44 | UNK | 2.6 | 0.3 | 4 |
| M55B | M | 69 | UNK | 4.0 | 0.8 | 44 |
| A66B | F | 42 | UNK | 5.3 | 0.5 | 3 |
| M13B | M | 53 | UNK | 5.6 | 0.6 | 1 |
| M76B | F | 69 | UNK | 6.0 | 0.7 | 1 |
| M83B | F | 35 | UNK | 6.2 | 0.9 | 29 |
| C34B | F | 48 | R-infection L-head trauma | 6.3 | 0.3 | UNK |
| A69B | F | 58 | UNK | 6.3 | 0.5 | 2 |
| C10B | M | 34 | Hereditary-other | 6.9 | 1.3 | 1 |
| M53B | M | 28 | UNK | 7.3 | 0.8 | 24 |
| M68B | M | 53 | UNK | 8.7 | 0.3 | 5 |
| A32B | M | 48 | UNK | 13.7 | 0.3 | 19 |
UNK=Unknown.
Procedures
All subjects signed institutional review board approved consent forms to participate in our studies. Each subject participated in tests of speech perception and localization. However, only 9 of 13 subjects participated in the word recognition test due to time constraints during the testing. All speech perception and localization tests were presented in the sound field, in a 10’× 9.3’× 6.5’ sound-treated booth with a reverberation time (RT60) at 1000 Hz of .079 seconds. Order of tests and test conditions were randomized among the subjects.
CNC Words in Quiet
Speech perception in quiet was measured using recorded Consonant-Nucleus-Consonant monosyllabic words (CNC) (Tillman & Carhart, 1966) presented from a front-facing loudspeaker (0°) at 1 m distance. Two lists of 50 CNC words were administered in the unilateral CI condition (1st visit) and in the bilateral CI condition (2nd visit) and scored based on percent-correct (%) performance at both the word and the phoneme levels. All lists were randomized between subjects and no subject received two of the same lists during this study. Speech materials were presented at 70 dB(C).
Cueing-the-Listener
Speech perception in noise was measured using a test we will refer to in this paper as “Cueing-the-Listener” (Tyler, et al 2006). During this test an auditory cue (either “hey I’m over here” or “she saw the”) was presented in order to orient the listener to the location of the loudspeaker that one of the closed-set of 12 randomly selected spondee words would be played from (Tyler, et al 2006). The spondee words were spoken by a female speaker. The listener used a touch screen to select which spondee word was heard amongst the background noise. One of eight randomly selected loudspeakers spanning a horizontal arc of 108° was used to play the target signal. Loudspeaker one and loudspeaker eight were placed 54° to the left and to the right (0°) position. A competing background noise (Turner, Gantz, Vidal, Behrens, & Henry, 2004) was also played from one of the eight loudspeakers. The background noise was a male and a female each repeating a different sentence. The female speaker used in the background noise was not the same speaker saying the spondee words. The location of the background noise was located either four loudspeakers to the right or left of the loudspeaker that played the target signal (e.g. if the target was played from loudspeaker 2, the background noise was played from loudspeaker 6). The level of the background noise was varied adaptively with the level of the spondee word remaining constant. The initial step-size was 8 dB and the minimum step-size was 2 dB. Following each up and down reversal, the step size was halved. The signal-to-noise ratio (SNR) yielding 50% correct was obtained using a 1-up and 1-down adaptive rule with a total of 14 reversals. The average of the last 10 reversals was used to calculate the SNR for that trial set. The SNR was calculated based on the average threshold of the last three of five trial sets. The initial starting level for the background noise and the spondee varied between subjects so that a ceiling performance on the test would be avoided. The maximum loudness that the background noise could be played was 90 dB A. The minimum level of the spondee that the spondee was played was 60 dB A. Thus, ceiling performance would have been a −30 dB S/N ratio for these loudness settings. The auditory cue was played in quiet; one-second later the background noise was begun, and the target was played 0.8 seconds following the start of the background noise. The duration of the background noise was 2 seconds and the maximum duration of the spondee words was 1.05 seconds.
Localization-in-Background noise
Localization was measured using an eight-loudspeaker everyday sounds localization in noise test. This is the same test as described in Dunn, Tyler, & Witt (2005) with the exception of the addition of noise used in this study. Sixteen everyday sounds (Kramer, 1998) presented at 60 dB(C) were repeated six times and presented randomly from one of the eight loudspeakers. A competing background noise consisting of a male and a female voice repeating sentences (Turner et al., 2004) was also played from one of the eight loudspeakers at 50 dB(C). The loudspeaker location for the background noise was different from that of the target everyday sound and was also randomly selected.
Participants were instructed to identify the loudspeaker location from which the target everyday sound originated by pressing a number button corresponding to the loudspeaker on a touch screen which was placed in front of them. The touch screen had a visual display of the eight loudspeaker array and provided instructions for performing the test. When the test was initiated, the background noise started playing from a randomly selected loudspeaker. The subject was then instructed to push “play” whenever they were ready to hear a target everyday sound. Upon completion of the everyday sound the background noise stopped playing immediately and the subject was instructed to respond. Once the subject responded another trial began. A total of 96 trials were presented and localization performance was determined by calculating the average Root Mean Square (RMS)-error in degrees. For a detailed description of this scoring, see Dunn et al., 2005.
Results
CNC Words in Quiet
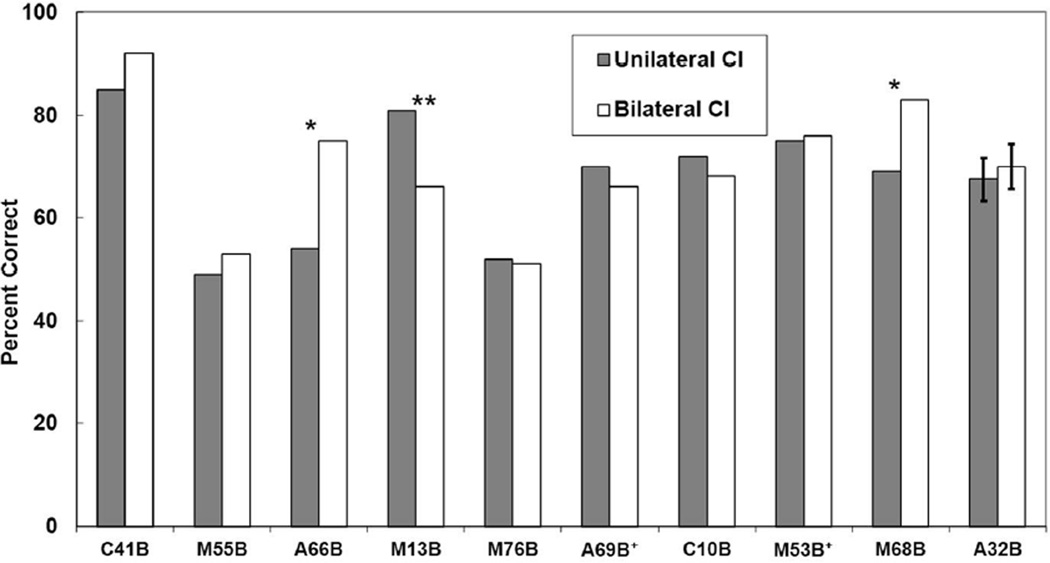
Figure 1 shows individual results for CNC words presented in quiet with unilateral CI and with bilateral CI. Average results for the 9 subjects were 67% with unilateral CI and 70% with bilateral CI. Individual results showed that 2 subjects (A66B and A32B) performed significantly better (using the binomial model [Thornton & Raffin, 1978]) with bilateral CI when compared to unilateral CI. One subject (M13B) performed significantly worse with bilateral CI than with unilateral CI. All other subjects showed no difference between scores. Averaged group results for the unilateral CI was 67% and 70% for the bilateral CI listening condition. A paired t-test on group results showed no significant difference between these two listening conditions. Additionally, the Pearson product-moment correlation coefficient was used to analyze relationships between the difference score for the unilateral CI and bilateral CI listening conditions and the duration between the first and second CI surgeries and between the difference score for the unilateral CI and bilateral CI listening conditions and the duration of deafness. Non-significant correlations were found between the difference score for the unilateral CI and bilateral CI listening conditions to the duration between the first and second CI surgeries (r =.16, p > .05), to the duration of deafness (r =.05, p > .05) and to the duration of bilateral use (r = −.44, p > .05).
Figure 1.
Nine individual and group average CNC word in quiet scores for unilateral CI and bilateral CI (a “+” next to the subject name denotes those who used a CI+HA). The single asterisk indicates a significant improvement in performance between unilateral CI and bilateral CI test conditions whereas the double asterisk indicates a significant decrement in performance between these two conditions.
Cueing-the-Listener
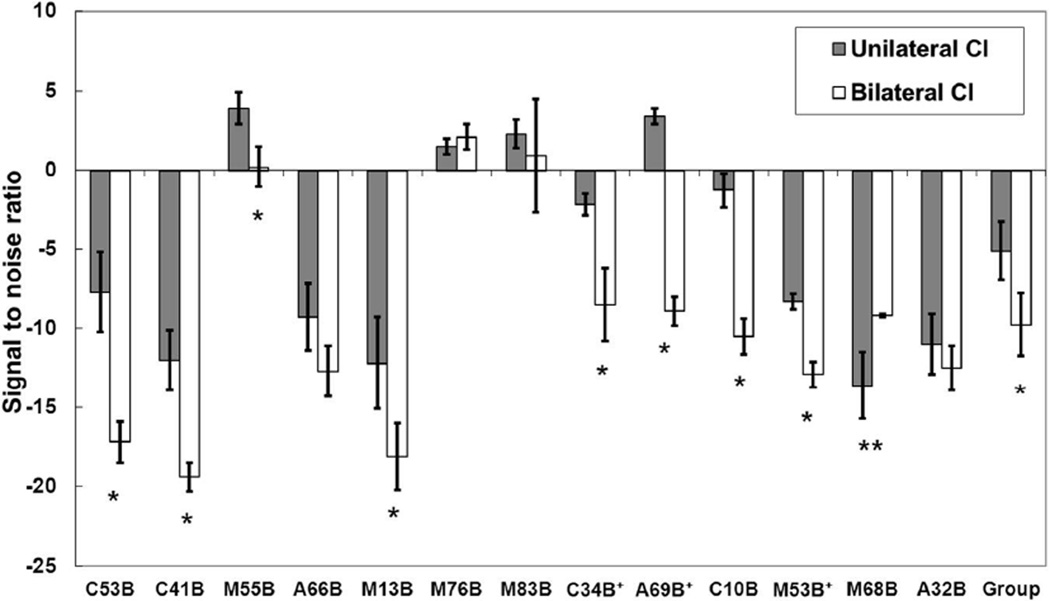
In Figure 2, individual results from the Cueing-the-Listener test are displayed for the unilateral CI and bilateral CI listening conditions. Individual results showed that 8 out of 13 subjects showed a significant benefit (using standard mean error bars calculated from the last three of the five trial sets) of listening with bilateral CI and 1 subject scored significantly worse with bilateral CI. All other subjects showed no difference in performance between the unilateral CI and bilateral CI listening conditions. Averaged group results for the unilateral CI was −5.1 dB SNR and −9.7 dB SNR for the bilateral CI listening condition. To obtain the same performance level, the group results showed that when bilateral CI, subjects were able to listen to significantly higher levels of noise than when unilateral CI subjects (t(12) = 2.69, p < .05). Additionally, non-significant correlations were found when comparing the difference score for the unilateral CI and bilateral CI listening conditions to the duration between the first and second CI surgeries (r =.43, p > .05), to the duration of profound deafness (r =.39, p > .05) and to the duration of bilateral use (r = −.19, p > .05).
Figure 2.
Thirteen individual and group average Cueing-the-Listener signal-to-noise ratio for unilateral CI and bilateral CI (a “+” next to the subject name denotes those who used a CI+HA). Average scores are shown with standard error bars. The single asterisk indicates a significant improvement in performance between unilateral CI and bilateral CI test conditions whereas the double asterisk indicates a significant decrement in performance between these two conditions.
Localization-in-Background noise
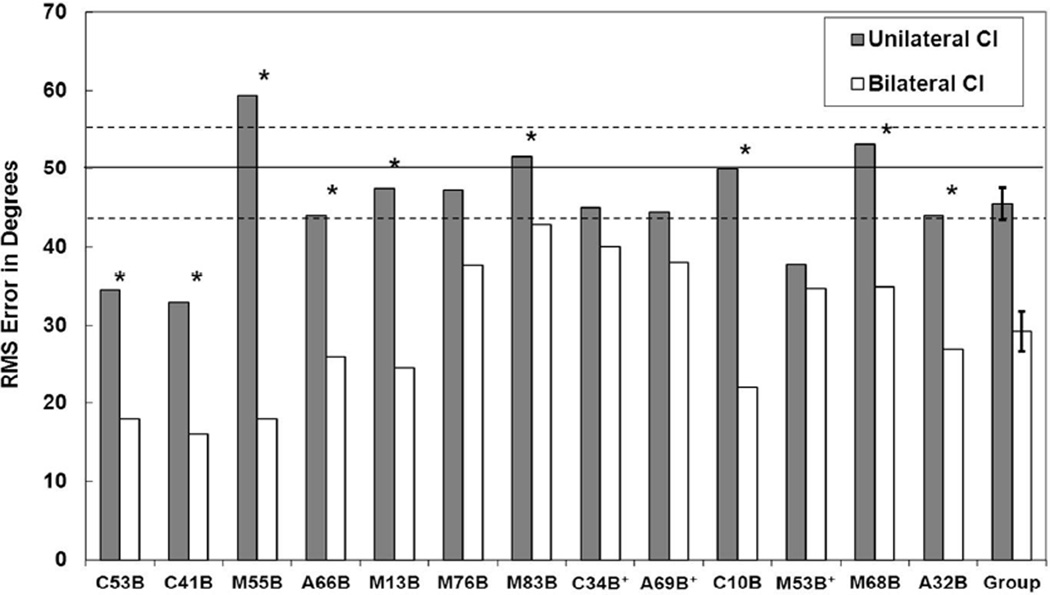
Figure 3 shows localization performance in the unilateral CI and bilateral CI listening conditions. Analysis of individual performance showed that 9 subjects had significant improvement when comparing the performance in the unilateral CI and bilateral CI listening conditions (improvement ranging from 17° to 41°) by paired t-tests. Four subjects showed no significant difference on localization abilities between the unilateral CI and bilateral CI listening conditions. Ten subjects out of the 13 did not score better than chance with unilateral CI, whereas all 13 subjects performed better than chance with bilateral CI. Chance performance on this test was calculated by simulating chance observations of 96 total sounds where 12 sounds come from each of 8 loudspeakers. The response value was drawn from a uniform distribution of choosing loudspeakers 1 through 8 twelve times. RMS-error was computed for each of 10,000 simulated draws. The mean RMS value of the simulated draws was 3.237 with a 95% confidence interval of 2.874 to 3.582. This number was then multiplied by 15.5 to gain the azimuth between loudspeakers and obtain the RMS-error in degrees. In this case, the mean chance performance was 50.18° with a 95% confidence interval 44.55° to 55.53°.
Figure 3.
Thirteen individual and group average localization RMS-error in degree scores for unilateral CI and bilateral CI (a “+” next to the subject name denotes those who used a CI+HA). The solid line at 50 degrees indicates chance score and the two dashed lines indicate the 95% confidence interval for this chance score. The single asterisk indicates a significant improvement in performance between unilateral CI and bilateral CI test conditions.
The three subjects who wore a cochlear implant and a hearing aid on opposite ears (CI+HA) prior to getting his or her second cochlear implant performed similarly to the subjects who wore one cochlear implant. After receiving their second cochlear implant, these three subjects did not show significant improvements in their localization abilities. However, two subjects who scored above chance with CI+HA were now scoring better than chance (A69B and C34B). Averaged group results for the unilateral CI were 46° RMS-error and 29° RMS-error for the bilateral CI listening condition. The average RMS for normal hearing listeners on this same test is 0° RMS-error. Group results showed a significant benefit for bilateral CI (t(12) = 5.6, p < .001) with an average 17° lower RMS-error than unilateral CI. Additionally, non-significant correlations were found when comparing the difference score for the unilateral CI and bilateral CI listening conditions to the duration between the first and second CI surgeries (r =.17, p > .05), to the duration of profound deafness (r = −.15, p > .05), and to the duration of bilateral use (r = −.21, p > .05).
Discussion
A number of patients who currently have one cochlear implant are interested in obtaining a second cochlear implant in the opposite ear. One research question has been concerned with whether or not sequentially-implanted CI users would benefit from a second device after a number of years between implant surgeries. To our knowledge, only one study (Zeitler, Kessler, Terushkin et al., 2008) has observed the actual benefits that sequential patients receive when they are tested prior to getting their second cochlear implant and then tested again on the same tests after getting their second cochlear implant.
We evaluated the benefit of sequential bilateral implantation by comparing unilateral CI and bilateral CI on speech perception in quiet and in noise and on localization. In this study, the averaged group results for both speech perception in noise and localization in noise were significantly better after subjects received their second cochlear implant. No significant correlation was found between performance for the speech-in-noise and the localization-in-noise. The average amount of improvement on speech perception in noise was 4.6 dB (SD=4.5) and 16.2° (SD=10.2) on localization with background noise. Individual results showed that 62% of the subjects showed statistically significant benefits on the Cueing-the-Listener task whereas 69% of the subjects showed statistically significant benefits on the localization task. These results support the notion that those listeners who showed a benefit with two cochlear implants are presumably better able to quickly identify where a sound is coming from in comparison to a listener with only one implant. This could be due to a greater ability to take advantage of head shadow and binaural squelch effects. Although, squelch effects, when measured in other publications, are often very small.
There were three subjects who utilized a hearing aid on the opposite ear prior to receiving their second cochlear implant. These subjects had average or above average improvements on speech perception in noise after receiving their second implant. In contrast, however, these three subjects had below average improvements on localization. These subjects had, on average, 6 months of bilateral CI experience at the time of testing. This might indicate that it takes more time for the brain to transition from hearing with CI+HA to bilateral CI for localization than it does for speech perception. Chang et al. (2010) showed that localization performance continually improves up to 1 year post-implantation in some simultaneously implanted bilateral adults. However, it was determined that most of the benefits occur within the first three months after implantation.
The average speech perception in noise and localization results are consistent with the previously mentioned studies involving sequential bilateral cochlear implant listeners. These results are also consistent with the research by Dunn et al. (2009) where the same speech perception in noise test and similar localization test were used. The localization task in the present study introduced a noise component in the background versus no background noise was used in the previous manuscript (Dunn et al., 2009). Dunn et al. (2009) evaluated the differences in performance between a group of unilaterally-implanted subjects who were matched by age at implantation, duration of deafness, and pre-implant residual hearing to a group of simultaneous bilateral subjects. They showed a significant benefit for bilateral cochlear implantation on Cueing-the-Listener and localization in quiet supporting the hypothesis that bilateral cochlear implants might be more beneficial over single cochlear implants.
No difference in performance was shown between the unilateral CI and bilateral CI listening conditions for CNC words in quiet. One reason for this finding might be due to the small number of subjects tested in this study. In addition, it is well known that one of the benefits of bilateral cochlear implantation is listening in noise, particularly for spatially separate speech and noise. This enables listeners to use the binaural squelch and binaural summation effects and more easily take advantage of the head shadow effect. Individually, only two subjects showed a significant improvement in the bilateral CI listening condition over the unilateral CI condition. This indicates that the use of binaural summation in quiet may not be that beneficial. Additionally, one subject showed a decrement in performance when using bilateral CIs compared to when using one CI. However, because most of the subjects had, on average, just a little over 6 months of experience, more bilateral experience might be needed to quantify the asymptotic benefit they will receive from their second cochlear implant. According to Chang et al. (2010), who followed 17 simultaneously implanted bilateral subjects between 6 months and 48+ months, word recognition scores in quiet were significantly different from 12 months to 48+ months. This indicates that while the greatest benefits might occur within the first year after implantation (Chang et al., 2009; Gantz et al., 2000; Hamzavi, Baumgartner, Pok, Franz, & Gstoettner., 2003; Manrique et al., 1998; Oh et al., 2003; Ruffin et al., 2006; Waltzman, Cohen, Green, & Roland, 2002), improvement in speech perception can continue over time as well.
A secondary goal of this paper was to evaluate whether the duration between the first and second cochlear implant surgeries and the duration of deafness can be associated with bilateral benefits. Ramsden et al. (2005) concluded that sequential implantation with long delays between ears limited the amount of bilateral benefit sequentially implanted subjects might receive. We did not find trends in our data that indicate a negative impact on performance due to longer durations between surgeries or deafness. However, we feel that an analysis with a larger number of subjects are needed before it is determined whether duration of deafness or years between surgeries should be considered before sequential surgeries.
It is unknown if, and by how much, binaural performance could be improved with similar devices, number of channels, signal processing across ears (e.g. Tyler, Witt, Dunn et al., 2010) or by training (Tyler, Witt, Dunn and Wang, 2010) Two of the subjects (M83B and A32B) with different devices, signal processing, and number of channels across ears did not show a benefit with our speech perception in noise test and only one (M83B) of those subjects did not show a benefit with localization. In addition, the one subject (M76B) with a different number of channels, but with the same devices and signal processing across ears did not show a benefit with speech perception in noise. It could be that these subjects may benefit from programming that would enable more similar processing across ears. Because of device and programming limitations, whether due to the type of internal device or possibly due to electrode stimulation issues (e.g. open or shorted electrodes), it is not always possible to obtain this goal. Regardless of this fact, we find it remarkable that the majority of the subjects with different configurations across ears are able to obtain binaural benefits.
Conclusion
The results in this study showed significantly greater benefit when subjects had bilateral cochlear implants compared to only one implant on speech perception in noise and on localization. Furthermore, only a weak correlation was found indicating an effect for duration between surgeries, duration of deafness, and duration of bilateral use. However, a larger number of subjects are needed to evaluate the effect of these variables. Additionally, more bilateral experience could be needed to determine the full extent of the bilateral benefit with sequential implants.
Acknowledgement
This research was supported in part by research grant 2 P50 DC00242 from the National Institutes on Deafness and Other Communication Disorders, National Institutes of Health; grant RR00059 from the General Clinical Research Centers Program, Division of Research Resources, National Institutes of Health; the Lions Clubs International Foundation; and the Iowa Lions Foundation. We would also like to thank MED-EL Corporation for their support in acquiring subjects for this study and Ann Perreau and Stephanie Gogel for helping us to collect data.
References
- Buss E, Pillsbury HC, Buchman CA, Pillsbury CH, Clark MS, et al. Multi-center U.S. bilateral MED-EL cochlear implantation study: speech perception over the first year of use. Ear and Hearing. 2008;29:20–32. doi: 10.1097/AUD.0b013e31815d7467. [DOI] [PubMed] [Google Scholar]
- Chang S, Tyler R, Dunn C, Ji H, Witt S, et al. Performance over time on adults with simultaneous bilateral cochlear implants. Journal of the American Academy of Audiology. 2010;21:35–43. doi: 10.3766/jaaa.21.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorman MF, Dahlstrom L. Speech understanding by cochlear-implant patients with different left- and right-ear electrode arrays. Ear and Hearing. 2004;25:191–194. doi: 10.1097/01.aud.0000120367.70123.9a. [DOI] [PubMed] [Google Scholar]
- Dunn CC, Tyler RS, Witt SA. Benefit of wearing a hearing aid on the unimplanted ear in adult users of a cochlear implant. Journal of Speech, Language, and Hearing Research. 2005;48(3):668–680. doi: 10.1044/1092-4388(2005/046). [DOI] [PubMed] [Google Scholar]
- Dunn CC, Tyler RS, Oakley SA, Gantz BJ, Noble W. Comparison of speech recognition and localization performance in bilateral and unilateral cochlear implant users matched on duration of deafness and age at implantation. Ear and Hearing. 2008;29:352–359. doi: 10.1097/AUD.0b013e318167b870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn CC, Noble W, Tyler RS, Kordus M, Gantz BJ, et al. Bilateral and unilateral cochlear implant users compared on standard and newly developed speech tests and on sound localization. Ear and Hearing. 2009;31:1–3. [Google Scholar]
- Firszt JB, Reeder RM, Skinner MW. Restoring hearing symmetry with two cochlear implants or one cochlear implant and a contralateral hearing aid. Journal of Rehabilitation Research and Development. 2008;45(5):749–768. doi: 10.1682/jrrd.2007.08.0120. [DOI] [PubMed] [Google Scholar]
- Gantz BJ, Rubinstein JT, Tyler RS, Teagle HF, Cohen NL, et al. Long-term results of cochlear implants in children with residual hearing. Annals Otology, Rhinology, and Laryngology. 2000;185(Suppl):33–36. doi: 10.1177/0003489400109s1214. [DOI] [PubMed] [Google Scholar]
- Hamzavi J, Baumgartner WD, Pok SM, Franz P, Gstoettner W. Variables affecting speech perception in postlingually deaf adults following cochlear implantation. Acta Otolaryngology. 2003;123:493–498. doi: 10.1080/0036554021000028120. [DOI] [PubMed] [Google Scholar]
- Kramer SE. Assessment of hearing disability and handicap: A multidimensional approach. Amersfoort, The Netherlands: 1998. Print Partner Ipskamp. [Google Scholar]
- Laszig R, Aschendorff A, Stecker M, Muller-Deile J, Maune S, et al. Benefits of bilateral electrical stimulation with the nucleus cochlear implant in adults: 6-month postoperative results. Otology & Neurotology. 2004;25:958–968. doi: 10.1097/00129492-200411000-00016. [DOI] [PubMed] [Google Scholar]
- Litovsky R, Parkinson A, Arcaroli J, Sammeth C. Simultaneous bilateral cochlear implantation in adults: a multicenter clinical study. Ear and Hearing. 2006;27:714–731. doi: 10.1097/01.aud.0000246816.50820.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manrique MJ, Espinosa JM, Huarte A, Molina M, Garcia-Tapia R, et al. Cochlear implants in post-lingual persons: results during the first five years of the clinical course. Acta Otorrinolaringol Espaniel. 1998;49:19–24. [PubMed] [Google Scholar]
- NIDCD. [Retrieved May, 14, 2012];2010 from http://www.nidcd.nih.gov/health/hearing/coch.htm.
- Noble W, Tyler R, Dunn CC, Bhullar N. Hearing handicap ratings among different profiles of adult cochlear implant users. Ear and Hearing. 2008b;29(1):112–120. doi: 10.1097/AUD.0b013e31815d6da8. [DOI] [PubMed] [Google Scholar]
- Noble W, Tyler R, Dunn CC, Buhllar N. Unilateral and bilateral cochlear implants and the implant-plus-hearing-aid profile: Comparing self-assessed and measured abilities. International Journal of Audiology. 2008a;47(8):505–514. doi: 10.1080/14992020802070770. [DOI] [PubMed] [Google Scholar]
- Oh SH, Kim CS, Kang EJ, Lee DS, Lee HJ, Chang SO, et al. Speech perception after cochlear implantation over a 4-year time period. Acta Otolaryngology. 2003;123:148–153. doi: 10.1080/0036554021000028111. [DOI] [PubMed] [Google Scholar]
- Peters BR, Litovsky R, Parkinson A, Lake J. Importance of age and postimplantation experience on speech perception measures in children with sequential bilateral cochlear implants. Otology & Neurotology. 2007;28:649–657. doi: 10.1097/01.mao.0000281807.89938.60. [DOI] [PubMed] [Google Scholar]
- Ramsden R, Greenham P, O-Driscoll M, Mawman D, Proops D, et al. Evaluation of bilaterally implanted adult subjects with nucleus 24 cochlear implant system. Otology & Neurotology. 2005;26:988–998. doi: 10.1097/01.mao.0000185075.58199.22. [DOI] [PubMed] [Google Scholar]
- Ruffin CV, Tyler RS, Witt SA, Dunn CC, Gantz BJ, et al. Long-term performance of clarion 1.0 cochlear implant users. Laryngoscope. 2007;117(7):1183–1190. doi: 10.1097/MLG.0b013e318058191a. [DOI] [PubMed] [Google Scholar]
- Schleich P, Nopp P, D’ Haese P. Head shadow, squelch, and summation effects in bilateral users of the med-el combi 40/40+ cochlear implant. Ear and Hearing. 2004;25(3):197–204. doi: 10.1097/01.aud.0000130792.43315.97. [DOI] [PubMed] [Google Scholar]
- Schön F, Müller J, Helms J. Speech reception thresholds obtained in a symmetrical four-loudspeaker arrangement from bilateral users of MED-EL cochlear implants. Otology & Neurotology. 2002;23:710–714. doi: 10.1097/00129492-200209000-00018. [DOI] [PubMed] [Google Scholar]
- Thornton AR, Raffin MJM. Speech discrimination scores modeled as a binomial variable. Journal of Speech and Hearing Research. 1978;21:497–506. doi: 10.1044/jshr.2103.507. [DOI] [PubMed] [Google Scholar]
- Tillman TW, Carhart R. Texas: USAF School of Aerospace Medicine, Brooks Air Force Base; 1966. An expanded test for speech discrimination utilizing CNC monosyllabic words. Northwestern University Auditory Test No. 6 Technical Report No. SAM-TR-66-55. [DOI] [PubMed] [Google Scholar]
- Turner CW, Gantz BJ, Vidal C, Behrens A, Henry BA. Speech recognition in noise for cochlear implant listeners: benefits of residual acoustic hearing. Journal of the Acoustical Society of America. 2004;115:1729–1735. doi: 10.1121/1.1687425. [DOI] [PubMed] [Google Scholar]
- Tyler RT, Witt SA, Dunn CC, Wang W. Initial development of a spatially separated speech-in-noise and localization training program. Journal of the American Academy of Audiology. 2010;21(6):390–403. doi: 10.3766/jaaa.21.6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler RS, Noble W, Dunn CC, Witt SA. Some benefits and limitations of binaural cochlear implants and our ability to measure them. International Journal of Audiology. 2006;45(Suppl 1):113–119. doi: 10.1080/14992020600783095. [DOI] [PubMed] [Google Scholar]
- Tyler RS, Noble W, Dunn CC, Witt SA. Speech perception and localization with adults with bilateral sequential cochlear implants. Ear and Hearing. 2007;28(2 Suppl):86S–90S. doi: 10.1097/AUD.0b013e31803153e2. [DOI] [PubMed] [Google Scholar]
- Tyler RS, Perreau A, Ji H. Validation of the spatial hearing questionnaire. Ear and Hearing. 2009;30(4):419–430. doi: 10.1097/AUD.0b013e3181a61efe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler RS, Witt SA, Dunn CC, Perreau A, Parkinson AJ, Wilson BS. An attempt to improve bilateral cochlear implants by increasing the distance between electrodes and providing complementary information to the two ears. Journal of the American Academy of Audiology. 2010;21(1):52–66. doi: 10.3766/jaaa.21.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waltzman SB, Cohen NL, Green J, Roland JT., Jr Long-term effects of cochlear implants in children. Otolaryngology - Head and Neck Surgery. 2002;126:505–511. doi: 10.1067/mhn.2002.124472. [DOI] [PubMed] [Google Scholar]
- Zeitler DM, Kessler MA, Terushkin V, Roland TJ, Jr, Svirsky MA, Lalwani AK, Waltzman SB. Speech perception benefits of sequential bilateral cochlear implantation in children and adults: a retrospective analysis. Otology & Neurotology. 2008;29(3):314–325. doi: 10.1097/mao.0b013e3181662cb5. [DOI] [PubMed] [Google Scholar]