Abstract
Background
In infants and children with fractures from an unclear cause, Osteogenesis Imperfecta (OI) is often included as a potential etiology. In infants and children with OI there exists a gap in the published literature regarding the fracture pattern seen at the time of diagnosis. As an additional aid to the diagnosis of OI, we sought to characterize the fracture patterns in infants and children at the time of their diagnosis.
Methods
We performed a retrospective chart review of a series of infants and children under 18 years of age who have the diagnosis of OI (any type) from a single institution.
Results
We identified 68 infants and children with OI: 23 (34%) type 1, 1(2%) type 2, 17(25%) type 3, 24(35%) type 4 and 3(4%) unknown type. A family history of OI is present in 46% of children. Forty-nine (72.0%) patients were diagnosed solely on clinical characteristics, without genetic or fibroblast confirmation. Rib fractures were noted in 21% of the subjects with none being identified during infancy. The number of fractures identified at diagnosis ranged from 1 to >37 with 7 (10%) having more than 2 fractures. All subjects with more than 2 fractures were diagnosed prenatally or in the immediate newborn period. Seventeen (25%) infants were diagnosed after 1 week of age but prior to 12 months of age. None of these infants had either rib fractures or more than 1 fracture at the time of diagnosis.
Conclusion
The majority of children diagnosed with OI are diagnosed by clinical features alone. The fracture pattern at the time of diagnosis in OI is variable with 10% having more than 2 fractures. The diagnosis of OI was made in utero or at delivery in 43% of children. Multiple rib fractures in an infant would be an unexpected finding in OI.
Level Of Evidence
Level III
Keywords: Osteogenesis Imperfecta, Child Abuse, Fractures, Infant, Prenatal Diagnosis
Introduction
In infants or children who present with unexplained or multiple fractures, the differential diagnosis includes the infant or child having an inherent predisposition to skeletal fractures,1,2 the most common of which is Osteogenesis Imperfecta (OI)3.
Osteogenesis Imperfecta is an inherited disorder of type 1 collagen that results in varying degrees of bone fragility, osteoporosis and predisposition to fractures.4 The incidence of OI is between 1/15,000 and 1/60,000 births. There is considerable clinical heterogeneity between the four major types of OI5,6,7: Types 1 and 4 are autosomal dominant and have a variable osseous fragility pattern ranging from mild to moderate and may or may not have secondary characteristics such as blue sclera, dentogenesis imperfecta or presenile hearing loss. Type 2 is routinely fatal in the perinatal period. Type 3 is either autosomal dominant or autosomal recessive and has a marked pattern of osseous fragility with associated growth retardation and progressive bone deformation.
Skeletal injuries are seen in up to one-third of all children by the age of 16 years.8,9 Child abuse victims tend to be younger than children with accidental traumatic fractures.10,11 A recent review of children evaluated at a level I pediatric trauma center reported rib fractures having an adjusted Odds Ratio of 14.4 for child abuse when compared with non-accidental trauma; 23.7 when restricted to children younger than 18 months.10 Additionally, a systematic review of the skeletal findings associated with child abuse demonstrated the presence of multiple fractures being “more common after physical abuse than after non-abusive traumatic injury.”11 Rib fractures have a particularly high association with child physical abuse (CPA).11
OI is often proposed as a cause of fractures in children who present with no clear history to explain the injury3, 12, 13 and may be invoked as an alternate cause of fractures in patients with CPA. Published literature supports that the clinical features of OI are readily distinguishable from CPA.5, 14, 15 Recently some authors have suggested that children with OI are often mistaken for having been victims of CPA.13 Our hypothesis was that the fracture patterns, age at diagnosis and numbers of fractures seen in children at the time of their diagnosis with OI differ from those seen in CPA.
In our study, we were most interested in clinical characteristics when OI was first considered and ultimately confirmed. The purpose of this study is to characterize the fracture patterns and clinical information relied upon by clinicians at the time of diagnosis in a sample of infants and children with OI. We anticipated that the clinical features and number of fractures observed in infants and children at the time of their diagnosis OI would aid the orthopaedist in distinguishing it from CPA.
Materials and Methods
Design and Population
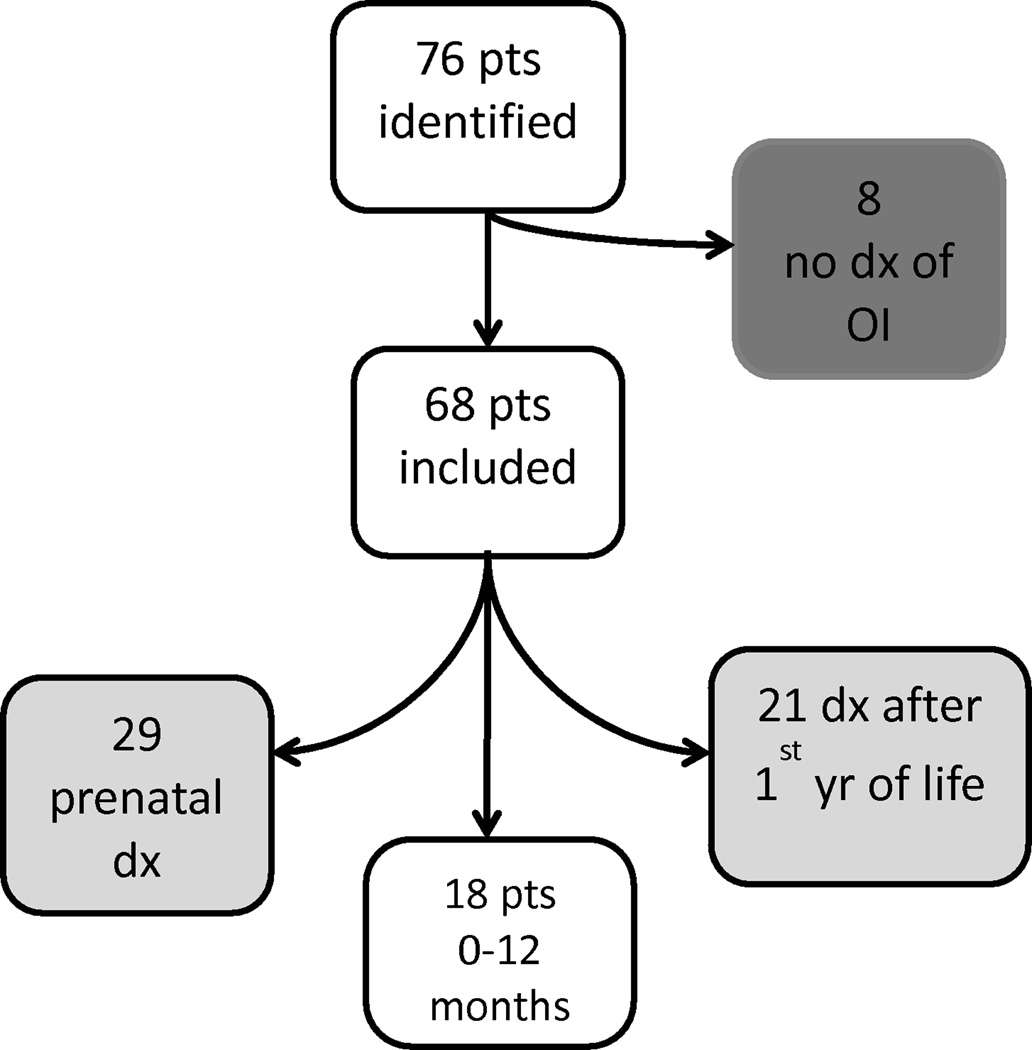
We performed a retrospective chart review of all children (under 18 years) with the diagnosis of OI of any type who had active records at The Shriner’s Hospital for Children in Houston, TX as January 2011. The Shriners Hospital for Children—Houston is not-for-profit children’s orthopedic hospital with over 13,000 outpatient visits per year. Eligible patients were identified by a query of the hospital Electronic Health Records for all current patients with the diagnosis of OI of any type. The initial query of the electronic health record resulted in 76 potential subjects; eight were ineligible as they did not ultimately carry the diagnosis of OI. The remaining 68 patients formed the study subjects. Figure 1 represents how the subjects were assembled.
Figure 1.
Assembly of subjects
Data Abstraction
Each subject’s complete medical records were abstracted for demographics, past history, diagnostic criteria, radiographic findings, genetic testing and social history, including involvement by any state Child Protection Services (CPS). Our query was limited to the findings present at diagnosis and was not intended to represent the natural course of children with OI. Extremity fractures were often noted in the records by body location and not by actual bone. To maintain consistency we coded any extremity bones noted as body location. Fractures of the radius, ulna or humerus were coded as “arm”. Fractures of the femur, tibia or fibula were coded as “leg”.
The protocol was approved by the IRBs of both the University of Texas Health Science Center at Houston and the Baylor College of Medicine.
Results
Table 1 shows distribution of the four major types of OI and the timing of when the diagnosis was made. The most common type of OI was type 4 (35%). Prenatal diagnosis was most common in OI types 3 and 4. Twenty-nine (43%) of the children were diagnosed either prenatally or at birth, and 14 (21%) were diagnosed after the 4 years of age. A positive family history of OI was reported in 46%. A family history of OI was least common in OI type 3; present only in 1 of 17 (6%).
Table 1.
Clinical Features at Diagnosis by OI type
| OI Type 1 n = 23(%) |
OI Type 2 n = 1(%) |
OI Type 3 n = 17(%) |
OI Type 4 n = 24(%) |
OI Type Unknown n = 3(%) |
Total n = 68(%) |
|
|---|---|---|---|---|---|---|
| FH of OI | 17(73.9) | 0 | 1(5.9) | 10(41.7) | 3(100) | 31(45.6) |
| Age at DX | ||||||
| Prenatal | 2(8.7) | 1(100) | 2(11.8) | 4(16.7) | 0 | 9(13.2) |
| Birth | 3(13.0) | 0 | 13(76.5) | 5(20.8) | 0 | 21(30.9) |
| 0–12 mo | 10(43.5) | 0 | 2(11.8) | 3(12.5) | 2(66.7) | 17(25.0) |
| 1–4 years | 4(17.4) | 0 | 0 | 3(12.5) | 0 | 7(10.3) |
| >4 years | 4(17.4) | 0 | 0 | 9(37.5) | 1(33.3) | 14(20.6) |
The most common fractures noted at diagnosis were extremity fractures. Twenty-two (32%) subjects had extremity fractures. There were 17 arm fractures and 36 leg fractures. Rib fractures were noted in 15 (22%) subjects. Of these 15, 13 (87%) were diagnosed prenatally or immediately after birth, 12 (80%) were noted to have blue sclera, 10 (67%) were noted to have osteopenia on x-ray, and 5 (33%) had a family history of OI. The two (13%) infants with rib fractures who were not diagnosed prenatally or at birth were diagnosed at 14 months and 43 months. They both were diagnosed with OI type 1, had a family history of OI and blue sclera.
The number of fractures noted at the time of diagnosis is represented in Table 2. Twenty-six (38%) subjects had no fractures at diagnosis and 7 (10%) had 3 or more. These 7 subjects were diagnosed either prenatally (2) or immediately after birth (5); none had a family history, and all were diagnosed clinically without genetic or fibroblast testing.
Table 2.
Fracture Number at Diagnosis by OI type
| Number of Fractures |
OI Type 1 |
OI Type 2 |
OI Type 3 |
OI Type 4 |
OI Type Unknown* |
Total |
|---|---|---|---|---|---|---|
| Unknown* | 1 | 0 | 4 | 6 | 1 | 12 |
| 0 | 10 | 0 | 3 | 11 | 2 | 26 |
| 1 | 10 | 0 | 4 | 1 | 0 | 15 |
| 2 | 1 | 0 | 3 | 4 | 0 | 8 |
| 3 | 0 | 0 | 0 | 1 | 0 | 1 |
| 4 | 0 | 0 | 1 | 1 | 0 | 2 |
| >4 | 1 | 1 | 2 | 0 | 0 | 4 |
| 23 | 1 | 17 | 24 | 3 | 68 | |
Unknown = actual number of fractures not recorded in the medical record (i.e. reported as “multiple fractures” alone)
There were 17 children who were diagnosed after birth (after the first week of life) through their 12th month (Table 3). Of these infants, most (59%) had OI type I, 94% were diagnosed on clinical features alone without genetic or fibroblast testing, and 53% had a family history. No subject had more than two fractures at the time of diagnosis, although in two the number of fractures was not reported in the records. The first was diagnosed with OI type 4 at 2 months of age but was noted in utero to have bilateral femoral fractures. The second was diagnosed with an undetermined type of OI at 12 months of age, but had a sibling with a prior diagnosis of OI. Six of 17 (35%) subjects had no fractures at the time of diagnosis; all of these had a family history of OI, and 5 had a physical finding of blue sclerae. No subjects diagnosed in the first year of life were reported to have rib fractures at initial presentation.
Table 3.
Clinical Features in Infants Diagnosed after birth and by 12 months by OI type
| Feature | Type 1 | Type 2 | Type 3 | Type 4 | Type Unknown |
Total N=17 |
|---|---|---|---|---|---|---|
| FHx of OI | 7 | 0 | 0 | 2 | 0 | 9 |
| Blue Sclerae | 9 | 0 | 3 | 1 | 0 | 13 |
| Osteopenia | 3 | 0 | 1 | 2* | 0 | 6 |
| Number of Fractures |
||||||
| unknown | 0 | 0 | 0 | 1 | 1 | 2 |
| 0 | 3 | 0 | 0 | 2 | 1 | 6 |
| 1 | 6 | 0 | 2 | 0 | 0 | 8 |
| 2 | 1 | 0 | 0 | 0 | 0 | 1 |
| 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| 4 | 0 | 0 | 0 | 0 | 0 | 0 |
| >4 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10 | 0 | 2 | 3 | 2 | 17 | |
The clinical feature of OI present in our subjects at diagnosis are represented in Table 4. The most common feature identified was blue sclerae; seen in 51 (75%). Hearing loss was the least common diagnostic finding, present in only 4 subjects. Dentinogenesis imperfecta reported in only 11 subjects at the time of diagnosis. This low number is likely due to 47 (69%) infants were diagnosed before their first birthday, prior to when meaningful tooth eruption could be expected to occur. Forty-nine (72%) of the children were diagnosed strictly on clinical features with no additional confirmatory testing. In our study 3 (4%) subjects with the diagnosis of OI did not have either a family history, osteopenia reported on radiograph, or blue sclera. All 3 had OI type 4 confirmed with either genetic fibroblast testing. They were diagnosed at birth, 23 months and 13 years and none had rib fractures at the time of diagnosis. The subject diagnosed in the newborn period was noted to have Wormian bones on radiograph.
Table 4.
Diagnostic Features Present at Diagnosis by OI Type
| Diagnostic Feature |
OI Type 1 | Type 2 | Type 3 | Type 4 |
unknown | Total N=68 |
|---|---|---|---|---|---|---|
| FHx | 17 | 0 | 1 | 10 | 2 | 30 (44.1%) |
| Osteopenia | 7 | 1 | 12 | 14 | 0 | 34 (50.0%) |
| Dent Imp | 1 | 0 | 2 | 8 | 0 | 11 (16.2%) |
| Hearing Loss | 1 | 0 | 3 | 0 | 0 | 4 (5.9%) |
| Blue Sclerae | 22 | 1 | 14 | 11 | 3 | 51 (75.0%) |
| Genetic Studies | 3 | 0 | 4 | 7 | 0 | 14 (20.6%) |
| Fibroblast | 4 | 1 | 1 | 4 | 0 | 10 (14.7%) |
Two (3%) subjects were reported to CPS, but neither had a police investigation. One infant who was reported to CPS at 7 months of age was removed from the mother’s custody due to neglect. The infant’s predisposition to fractures, diagnosed prenatally, was not a factor. The other subject was diagnosed with OI at 6 months of age, had a family history of OI and had osteopenia noted on x-ray. The infant was not removed from parental custody. The cause for CPS referral was not recorded.
Discussion
This is the largest study to review the presenting clinical characteristics of children who were diagnosed with OI we are aware of. Other published reports have profiled childhood fractures in children with OI16 or the phenotypic and genetic heterogeneity of children with OI6, but none have described the fracture pattern and clinical features at the time of diagnosis. From our sample, we can draw three important findings about fractures at the time of diagnosis in infants and children diagnosed with OI.
First, while rib fractures have been demonstrated as being associated with physical abuse in children11, 17 they were noted in 22.1% of our subjects in whom abuse was not a concern. Our study demonstrates that rib fractures can appear in neonates and children with OI, but importantly not infants. In our study subjects rib fractures occurred in two distinct populations: those with OI diagnosed prenatally or perinatally, and those who began to fracture in the course of an active childhood beyond their infancy. Birth is a traumatic process which clearly exposes the neonate to forces well beyond those seen during routine care seen in infancy. Any predisposition to fractures will be revealed during the birthing process. Thus rib fractures which appear in infancy would not be supported as being from OI. Other reports of rib fractures in children with OI demonstrate similar timing18,19 or exhibit clear stigmata of the disease.20,21
A second important finding from our study is that infants and children with 3 or more fractures at the time of diagnosis represent a small portion of children with OI. Each of the 7 subjects were diagnosed either in utero or immediately at birth and were all diagnosed clinically despite the absence of a family history. Thus, outside of the newborn period, multiple unexplained fractures in infants should continue to raise the suspicion of an alternate diagnosis to bone fragility, such as child physical abuse.11 Multiple fractures were also demonstrate as associated with CPA in a large nationwide hospital discharge database in which 85% of children aged 0–11 months with at least 3 fractures were diagnosed with abuse.22
Third, infants and children with OI can be readily diagnosed without fibroblast or genetic testing. A clear majority of children diagnosed with OI (72%) were diagnosed based solely on clinical grounds. Currently, much of the fibroblast and genetic testing performed on children with multiple fractures occurs in the context of courtroom proceedings. One study of fibroblast testing in the context of suspected OI reported that in “88% of cases the child protection service workers, attorneys, or courts had requested testing.”14 It is apparent that much of the confirmatory testing may be unnecessary.
In our study, patients were rarely involved with CPS (2, 3%) and their involvement was unrelated to the diagnosis of OI. In contrast, Kocher and Dichtel13 described 33 infants and children who had confirmed OI and were reportedly misdiagnosed as child abuse. The authors reviewed anonymous records voluntarily submitted by members of a community group, one-third actively suing CPS, which consisted of incomplete medical records (identifiers redacted by the families) and family narratives. Their study reported 28 out of 33 (85%) children with multiple fractures, with an average of 7 fractures per child, all of whom had some CPS contact. Despite the study’s methodological flaws, the authors of this study agree that the “emphasis should be on the clinical recognition of OI features instead of universal laboratory testing.”13
There are three important limitations to our study to consider. First, our study is subject to the same cautions which are applicable to all other retrospective chart reviews. Because The Shriner’s Children’s Hospital is an international orthopaedic referral center, there were missing data which we were unable to confirm, including number of fractures seen in some of the subjects. Second, we likely have undercounted the number of fractures because as a record review we did not review the radiographs individually and some subjects may have not had complete skeletal assessments at the time of diagnosis. Third, the patients seen and the practice pattern at the Shriners hospital may not be representative of other OI populations or services. Despite these limitations, our study leads to some important next steps. Repeating this study at other clinical sites would demonstrate the generalizability of these data, increase the sample size and would account for different patient populations and practice patterns.
Conclusions
The data from our study of infants and children with OI supports our hypothesis that the number of fractures, age at diagnosis and location of fractures are clinical features which can aid in the diagnosis of OI. Infants or children with more than 2 fractures outside of the newborn period were not seen in our subjects with OI. The presence of rib fractures in an infant remains highly associated with being from CPA and our study would not support OI as an underlying cause. Additionally, our data confirm that in infants and children OI can be diagnosed after a thorough clinical assessment in the absence of any confirmatory testing. In summary, the commonly described clinical scenario of an infant with multiple fractures, including rib fractures, is not likely from undiagnosed OI.
Acknowledgments
Financial Support: Dr. Greeley is supported by Award Number K23HD065872 from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute Of Child Health & Human Development or the National Institutes of Health.
Abbreviations
- OI
Osteogenesis Imperfecta
- CPA
Child Physical Abuse
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nancy D. Kellogg and and the Committee on Child Abuse and Neglect. Evaluation of Suspected Child Physical Abuse. Pediatrics. 2007;119:1232–1241. doi: 10.1542/peds.2007-0883. [DOI] [PubMed] [Google Scholar]
- 2.Jenny C the Committee on Child Abuse and Neglect. Evaluating infants and young children with multiple fractures. Pediatrics. 2006;118:1299–1303. doi: 10.1542/peds.2006-1795. [DOI] [PubMed] [Google Scholar]
- 3.Bishop N, Sprigg A, Dalton A. Unexplained fractures in infancy: looking for fragile bones. Arch Dis Child. 2007;92:251–256. doi: 10.1136/adc.2006.106120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rauch F, Glorieux F. Osteogenesis Imperfecta. The Lancet. 2004;363:1377–1385. doi: 10.1016/S0140-6736(04)16051-0. [DOI] [PubMed] [Google Scholar]
- 5.Sillence DO. Annals of the New York Academy of Sciences. 1. Vol. 543. Third International Conference on Osteogenesis Imperfecta; 1988. Osteogenesis Imperfecta: Nosology and Genetics; pp. 1–16. [DOI] [PubMed] [Google Scholar]
- 6.Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfect. Journal of Medical Genetics. 1979;16:101–116. doi: 10.1136/jmg.16.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Byers P, Krakow D, Nunes M, et al. Genetic Evaluation of Suspected Osteogenesis Imperfecta (OI) Genetics In Medicine. 2006;8(6):383–388. doi: 10.1097/01.gim.0000223557.54670.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lyons RA, Delahunty AM, Kraus D, et al. Children’s Fractures: a population based study. Inj Prev. 1999;5:129–132. doi: 10.1136/ip.5.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rennie l, Court-Brown C, Mok J, et al. The epidemiology of fractures in children. Injury. 2007;38:913–922. doi: 10.1016/j.injury.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 10.Pandya N, Baldwin K, Wolfgruber H, et al. Child Abuse and Orthopaedic Injury Patterns: Analysis at a Level I Pediatric Trauma Center. J Pediatr Orthop. 2009;29:618–625. doi: 10.1097/BPO.0b013e3181b2b3ee. [DOI] [PubMed] [Google Scholar]
- 11.Kemp A, Dunstan F, Harrison S, et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ. 2008;337:a1518. doi: 10.1136/bmj.a1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Onyon C, Rabb L, Debelle G. Non-accidental Injury and Bone Fragility Disorders: The Need for a Multidisciplinary Perspective. Child Abuse Review. 2009;18:346–353. [Google Scholar]
- 13.Kocher M, Dichtel L. Osteogenesis imperfecta misdiagnosed as child abuse. Journal of Pediatric Orthopaedics B. 2011;(6):440–443. doi: 10.1097/BPB.0b013e328347a2e1. [DOI] [PubMed] [Google Scholar]
- 14.Steiner R, Pepin M, Byers Studies of collagen synthesis and structure in the differentiation of child abuse from osteogenesis imperfect. Journal of Pediatrics. 1996;128:542–547. doi: 10.1016/s0022-3476(96)70367-0. [DOI] [PubMed] [Google Scholar]
- 15.Chapman S, Hall C. Non-accidental injury or brittle bones. Pediatric Radiology. 1997;27:106–110. doi: 10.1007/s002470050078. [DOI] [PubMed] [Google Scholar]
- 16.Vetter U, Pontz B, Zauner E, et al. Osteogenesis Imperfecta: A Clinical Study of the First Ten Years of Life. Calcif Tissue Int. 1992;50:36–41. doi: 10.1007/BF00297295. [DOI] [PubMed] [Google Scholar]
- 17.Williams R, Connolly P. In children undergoing chest radiography what is the specificity of rib fractures for non-accidental injury? Arch Dis Child. 2004;89:490–492. doi: 10.1136/adc.2004.051615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bulloch B, Schubert C, Brophy P, et al. Cause and Clinical Characteristics of Rib Fractures in Infants. Pediatrics. 2000;105(4):e48. doi: 10.1542/peds.105.4.e48. [DOI] [PubMed] [Google Scholar]
- 19.Schweich P, Fleisher G. Rib Fractures in Children. Pediatric Emergency Care. 1985;1(4):187–189. doi: 10.1097/00006565-198512000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Gahagan S, Rimsza M. Child Abuse or Osteogenesis Imperfecta: How Can We Tell? Pediatrics. 1991;88(5):987–992. [PubMed] [Google Scholar]
- 21.Ojima K, Matsumoto H, Hayase T, et al. An autopsy case of osteogenesis imperfecta initially suspected as child abuse. Forensic Science International. 1994;65(2):97–104. doi: 10.1016/0379-0738(94)90264-x. [DOI] [PubMed] [Google Scholar]
- 22.Leventhal J, Martin K, Asnes A. Incidence of Fractures Attributable to Abuse in Young Hospitalized Children: Results From Analysis of a United States Database. Pediatrics. 2008;122(3):599–604. doi: 10.1542/peds.2007-1959. [DOI] [PubMed] [Google Scholar]