Abstract
Background
Little or no longitudinal data have been available to date on the utilization of primary care physicians’ services, particularly by chronically ill and multimorbid patients and by those who see their primary care physician often (“frequent attenders”).
Methods
We collected anonymous data on 305 896 patients from 155 primary care practices over the period 1996–2006 and analyzed them with descriptive statistics, correlations, and multiple logistic regression.
Results
Over the period of the study, patients visited their primary care physicians about 7 times per year on average. Frequent attendance, defined as 24 or more contacts per year, was not strongly associated with chronic illness or multimorbidity (r=0.19 and r=0.24, respectively) but was found to be linked to time-consuming medical services, such as detailed counseling (adjusted odds ratio [OR], 5.8) and house calls (OR, 3.5). Chronically ill patients utilized their primary care physicians’ services less than we had expected. Chronic illness and multimorbidity were more common with increasing age; also correlated with age were the utilization of medical services, the number of visits to the primary care physician, and the number of visits to the primary care physician among frequent attenders.
Discussion
Although in Germany visits to physicians of all types (both primary care physicians and specialists) in private practice became more frequent in total over the period of this study, visits to primary care physicians alone did not. Frequent attenders do not necessarily have chronic illness or multimorbidity but seem to constitute a particularly problematic group. Chronic illness is not a predictor for greater utilization of primary care physicians’ services.
Patients in Germany are consulting practicing physicians increasingly frequently (1, 2). Current talk is of “18 doctor’s appointments per year” (3). An average of 6.8 doctor’s appointments per inhabitant (2007) is reported for the 27 countries of the OECD (Organisation for Economic Co-operation and Development) (1). Information on the following is lacking:
Whether outpatient use of primary care alone is rising
Whether age plays a role
Whether frequent and even increasing contact with physicians is a general phenomenon or is observed in certain special patient groups in particular.
This may be due to insufficient consensus on the distinctions between patients with chronic illnesses, patients with multiple illnesses, frequent attenders of outpatient care, and the older and very elderly. However, it may also be because it is complex to obtain original primary care data and process them for analysis.
A sample of treatment and billing data from medical practice information systems was examined for the following from 1996 to 2006:
Frequency of doctor–patient contacts
Patient characteristics and special patient groups
Primary care services required.
Methods
The retrospective study examined annual cross-sectional results over a period of 11 years. The raw data were anonymized routine data gathered from 155 primary care practices and a total of 472 775 patients in Lower Saxony, Bremen, and Baden-Württemberg. The practices participated voluntarily and included academic teaching practices at the University of Göttingen, the Hannover Medical School, and one practice network in Freiburg.
Raw data on primary care were extracted on single occasion from each practice’s electronic medical practice information system via the compulsory treatment data transfer interface. At the same time, they were assigned code names on site for privacy protection and transferred to the institute that held the data. The way in which data were obtained and an outline of data processing have already been stated elsewhere (4– 6). Internal data validation was performed according to the guideline ”Gute Praxis Sekundärdatenanalyse” (GPS, Good Secondary Data Analysis Practice) (7). The period examined ran from January 1, 1996 (the date the 1996 Uniform Value Scale was introduced) to December 31, 2006 (the last time sample data were gathered for a whole year).
A doctor–patient contact (DPC) on a specific date was considered to have occurred when at least one billing item was found that required personal contact between doctor and patient. This took account of items from the official medical fee schedule, the Uniform Value Scale (Einheitlicher Bewertungsmaßstab, EBM) from 1996 onwards for patients covered by statutory health insurance, and from April 1, 2005 the EBM 2000plus. An ICD diagnosis for a patient was identified as “serious” if it denoted one of the 80 illnesses in the risk adjustment scheme (year for comparison 2009).
Special patient groups
Two definitions were used to determine the status “patient with chronic illness” for a year:
“G-BA patient with chronic illness” was used for any patient who had at least one diagnosis for a quarter that was identical in the index quarter and the three preceding quarters and was one of the illnesses in the risk adjustment scheme, i.e. was “serious.” This use was in accordance with the Guidelines on Chronically Ill Patients of Germany’s Federal Joint Committee (G-BA, Gemeinsamer Bundesausschuss).
“M2Q patient with chronic illness” was used for any patient with at least one identical ICD diagnosis in at least two quarters of a calendar year. This corresponds to the M2Q criterion in the morbidity-oriented risk adjustment scheme (9, 10).
A patient was considered to have “multiple illnesses” if ICD diagnoses from at least five different chapters of the ICD were found within one year. This definition leads to a similar percentage of the sample as a whole to the other definitions of special patient groups.
“Frequent attenders” were those with at least 24 DPCs in one year, approximately 5% of all patients (95th percentile).
The chance of a patient belonging to one of these four special patient groups (two definitions of patients with chronic illnesses, patients with multiple illnesses, or frequent attenders) was determined from the variables patient sex and patient age together, using multivariate logistic regression. The possibility that patients might belong simultaneously to two of the four patient groups was examined by determining correlation, both parametrically and nonparametrically.
A primary care physician’s personal services were identified on the basis of billing items divided into the following four groups of services:
Detailed consultation
Full examination
Home visit
Emergency care.
If at least one relevant billing item was found for the patient in a year, the group of services was taken to have been used. The chances of using services from one of these four groups of services was calculated using multivariate logistic regression on the basis of patient sex and age, and using bivariate analysis for each one of the four patient groups.
This calculation yielded six patient characteristics (sex and five age groups), four patient groups, and four groups of services, i.e. 14 dichotomous variables. The relations between these were examined using logistic regression. Odds ratios were calculated and shown both directly and adjusted for the influence of other variables.
Pearson’s and nonparametric (Kendall’s tau-b) correlations and odds ratios were calculated using a bilateral 99% confidence interval. All calculations were performed using SPSS 19 or STATA 12.1.
The University of Göttingen’s and Hannover Medical School’s ethics approval of this research into routine primary care data has been granted.
Results
The data obtained from 548 812 patient years, 305 896 patients, and a total of more than 3.9 million doctor– patient contacts at 118 primary care practices met the methodical requirements for secondary data analysis from 1996 to 2006.
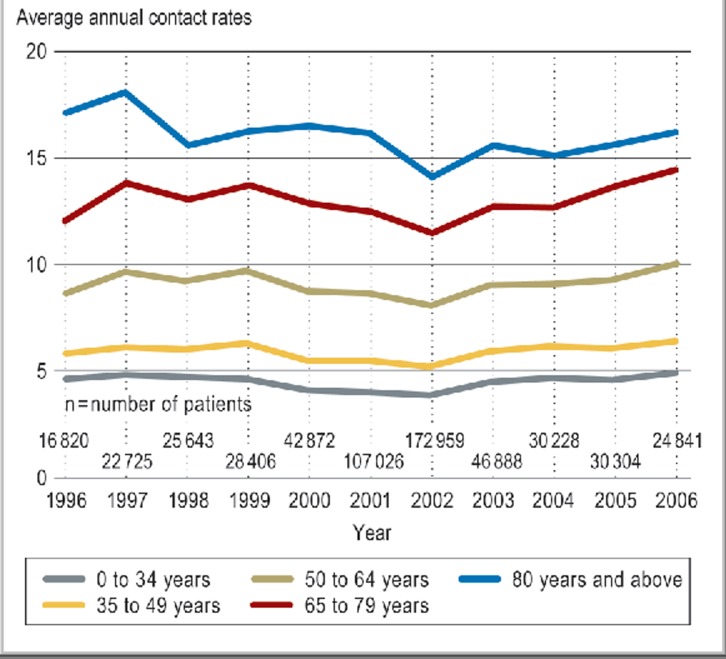
The relative number of doctor–patient contacts (DPCs), calculated on the basis of the number of DPCs using the number of patients per year of services, increased substantially with age (Figure 1).
Figure 1.
Average annual contact rates by age group
Yearly contact rates in the sample as a whole ranged from 6.8 to 7.8 DPCs over the 11 years examined. The average for the sample was 7.3 DPCs per year per patient. Linear regression of these annual contact rates from 1996 to 2006 yielded a negative beta coefficient (increase), indicating a decrease in contact rates during the observed period.
Older (65 to 79 years) and very elderly (80 years and older) patients accounted for 14.4% and 6.6% respectively of all patients in the sample. Annually, the percentage of G-BA patients with chronic illness varied between 2.2% and 8.6%, the percentage of M2Q patients with chronic illness between 23.0% and 32.0%, and the percentage of patients with multiple illnesses between 13.2% and 16.7%. The percentage of frequent attenders varied only slightly from 1996 to 2006, between 5.0% and 7.7% of all attenders of the practices.
Older age is associated with higher proportions of the four special groups of users for all patients, as shown in the global model using multivariate logistic regression on the basis of sex and age group (Table 1). This was particularly true of G-BA patients with chronic illnesses and frequent attenders, less so for patients with multiple illnesses, and barely true at all for M2Q patients with chronic illnesses. Where the result was insignificant according to the 99% confidence interval, the magnitudes of effect have been identified accordingly, both here and in the data presentations below.
Table 1. Regression of patient groups by sex and age group.
| Dependent variable | Independent variable | Multivariate odds ratio | Adjusted odds ratio |
| G-BA patients with chronic illnesses | Female | 1.0* | 0.8 |
| 35 to 49 years | 3.5 | 2.9 | |
| 50 to 64 years | 11.1 | 6.9 | |
| 65 to 79 years | 20.4 | 11.7 | |
| 80 years and above | 24.5 | 16.0 | |
| M2Q patients with chronic illnesses | Female | 1.2 | 1.1 |
| 35 to 49 years | 1.3 | 1.1 | |
| 50 to 64 years | 1.9 | 1.2 | |
| 65 to 79 years | 2.2 | 1.0 | |
| 80 years and above | 1.9 | 0.7 | |
| Patients with multiple illnesses | Female | 1.3 | 1.3 |
| 35 to 49 years | 1.5 | 1.2 | |
| 50 to 64 years | 2.5 | 1.5 | |
| 65 to 79 years | 3.3 | 1.5 | |
| 80 years and above | 3.3 | 1.4 | |
| Frequent attenders | Female | 1.1 | 1.0 |
| 35 to 49 years | 2.7 | 2.4 | |
| 50 to 64 years | 8.0 | 5.1 | |
| 65 to 79 years | 18.5 | 8.7 | |
| 80 years and above | 32.6 | 10.0 |
*Insignificant according to the 99% confidence interval
There was only slight to moderate pairwise correlation between membership in the four special patient groups (Table 2). The user groups are therefore sufficiently well differentiated from each other. Nonparametric correlations (Kendall’s tau-b), calculated on the basis of 109 262 (20%) randomly selected datasets from the sample, did not differ from the corresponding values in Table 2. All values fell within the 99% confidence interval.
Table 2. Correlations between membership in patient groups (Pearson’s correlation coefficients).
| G-BA patients with chronic illnesses | M2Q patients with chronic illnesses | Patients with multiple illnesses | Frequent attenders | |
| G-BA patients with chronic illnesses | 1 | |||
| M2Q patients with chronic illnesses | 0.36 | 1 | ||
| Patients with multiple illnesses | 0.34 | 0.42 | 1 | |
| Frequent attenders | 0.19 | 0.18 | 0.24 | 1 |
All results significant according to the 99% confidence interval
Health service use
Patients’ use of health services was affected only a little by sex but substantially by age. This is shown in the global model using multivariate logistic regression (Table 3).
Table 3. Regression of service groups by sex and age group.
| Dependent variable | Independent variable | Multivariate odds ratio | Adjusted odds ratio |
| Detailed consultation*2 | Female | 1.1 | 1.1 |
| 35 to 49 years | 1.4 | 1.3 | |
| 50 to 64 years | 2.0 | 1.6 | |
| 65 to 79 years | 2.6 | 1.8 | |
| 80 years and above | 2.3 | 1.4 | |
| Full examination*2 | Female | 1.0 | 0.9 |
| 35 to 49 years | 0.9 | 0.9 | |
| 50 to 64 years | 1.0 | 0.9 | |
| 65 to 79 years | 1.2 | 0.9 | |
| 80 years and above | 1.4 | 1.0 | |
| Home visit | Female | 1.2 | 1.2 |
| 35 to 49 years | 1.1 | 1.0 | |
| 50 to 64 years | 2.1 | 1.8 | |
| 65 to 79 years | 6.3 | 5.0 | |
| 80 years and above | 31.1 | 26.2 | |
| Emergency care | Female | 1.0 *1 | 0.9 |
| 35 to 49 years | 1.0 *1 | 1.0 *1 | |
| 50 to 64 years | 1.4 | 1.0 | |
| 65 to 79 years | 3.2 | 0.9 | |
| 80 years and above | 8.9 | 0.9 |
*1Insignificant according to the 99% confidence interval;
*2Excluding the EBM 2000plus
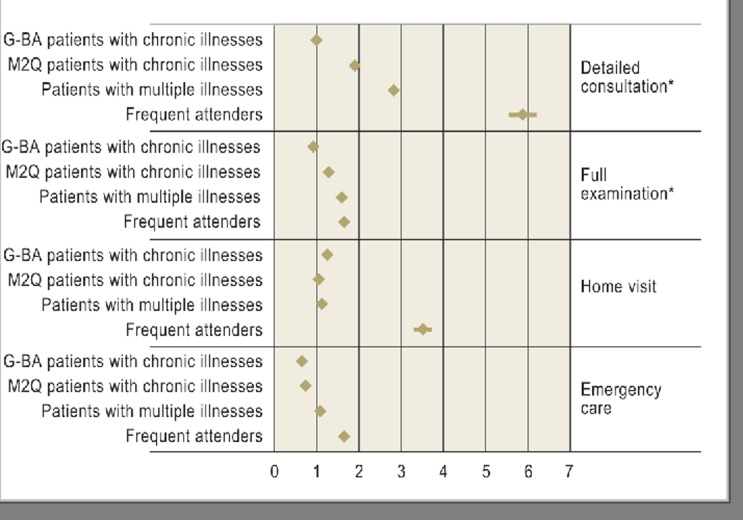
Membership in each special patient group (patients with chronic illnesses according to two definitions, patients with multiple illnesses, and frequent attenders) had a different weighting. This is shown both for bivariate analysis and following adjustment (Table 4).
Table 4. Regression of service groups by patient group.
| Dependent variable | Independent variable | Bivariate odds ratio | Adjusted odds ratio |
| Detailed consultation*2 | G-BA patients with chronic illnesses | 3.9 | 1.0 *1 |
| M2Q patients with chronic illnesses | 3.1 | 1.9 | |
| Patients with multiple illnesses | 5.3 | 2.8 | |
| Frequent attenders | 11.6 | 5.8 | |
| Full examination*2 | G-BA patients with chronic illnesses | 1.8 | 0.9 |
| M2Q patients with chronic illnesses | 1.9 | 1.3 | |
| Patients with multiple illnesses | 2.4 | 1.6 | |
| Frequent attenders | 3.0 | 1.6 | |
| Home visit | G-BA patients with chronic illnesses | 3.1 | 1.2 |
| M2Q patients with chronic illnesses | 1.5 | 1.0 | |
| Patients with multiple illnesses | 2.2 | 1.1 | |
| Frequent attenders | 9.5 | 3.5 | |
| Emergency care | G-BA patients with chronic illnesses | 1.5 | 0.6 |
| M2Q patients with chronic illnesses | 1.0 *1 | 0.7 | |
| Patients with multiple illnesses | 1.4 | 1.1 | |
| Frequent attenders | 5.3 | 1.6 |
*1Insignificant according to the 99% confidence interval;
*2Excluding the EBM 2000plus
The extent to which demand for primary care is correlated with membership in a special patient group is also shown by the graphic representation of the adjusted odds ratios from Table 4 (Figure 2).
Figure 2.
Regression of service groups by patient group
*excluding the EBM 2000plus
The chance of at least one use of detailed consultation, home visit, or emergency care per year was substantially higher for frequent attenders than for patients with chronic or multiple illnesses.
Overall, it is clear that “patient with chronic illnesses” status led to almost no increase in use of home visits or full examinations. In fact, patients with chronic illnesses actually used emergency care substantially less frequently than those without chronic illnesses. Both definitions of chronic illness (G-BA and M2Q) affected the model only slightly and also differed from each other only slightly in terms of foreseeable service use (Figure 2). In contrast, frequent attenders not only used primary care practices for a particularly long time according to the definition, but generally also showed a very high use of primary care physicians’ personal services. Finally, high patient age is associated with time-consuming home visits and emergency care that cannot be planned, including outside practices’ regular hours.
Discussion
The number of personal doctor–patient contacts per year, extracted from routine primary care data, remained almost unchanged between 1996 and 2006. The average number of contacts per patient year for this German sample was 7.3. However, doctor–patient contact rates differed widely between age groups: They increased substantially with age, an effect that did not change over 11 years.
The number of frequent attenders as a percentage of all patients remained almost constant over the 11 observed years. The number of frequent attenders as a percentage of all patients increased substantially with age for all patients within a single age group. Frequent attenders used far more primary care services than, for example, patients with chronic or multiple illnesses.
Only isolated examples of systematically gathered and longitudinal data on the average number of outpatient doctor’s appointments per year are available for Germany.
Research by the Institute for Social Medicine, Epidemiology, and Health-Care System Research (ISEG, Institut für Sozialmedizin, Epidemiologie und Gesundheitssystemforschung), which is published annually as the BARMER GEK Doctors’ Report (BARMER-GEK-Arztreport) (3), uses the simpler term “doctor contact” to denote a use of medical services. This covered persons insured by a single statutory health insurer in “2008, including approximately 2% of the population of the German Federation,” thereby excluding, in particular, those with private insurance. In addition, primary care was not separated from specialized outpatient care. According to the report, the annual per capita average of all outpatient doctor contacts rose from 16.4 (2004) to 17.7 (2007) and is estimated at 18.1 doctor contacts for 2008.
For primary care alone, this research reported an annual average of 7.3 doctor contacts per practice user, with no reliable trend or recognizable increase. The number of doctor contacts between 1996 and 2006 ranged from 6.8 to 7.8. These two estimates—that of the BARMER GEK Doctors’ Report and that of this article—together lead us to suspect that approximately half of all outpatient doctor contacts were with primary care physicians. Differences between trends—an increase in the contact rate for all practicing physicians, an unchanging annual number of contacts for primary care physicians only—allow us to assume that an increase in outpatient doctor contacts was caused primarily by an increase in demand for specialized practicing physicians, provided they were not caused by systematic differences in sample selection.
The authors of this article also found a marked increase in annual numbers of doctor contacts with increasing age, particularly for very elderly patients. Women attended appointments with primary care physicians more frequently than men, but sex made only a small difference, unlike in the results of Grobe et al. (3).
In international terms, Germany’s proportion of all outpatient doctor contacts and the primary care physician contact rate per year are very high. The OECD’s comparative figures for 2007 (1) for Germany were systematically incorrect and too low, as the BARMER GEK Doctors’ Report (3) also correctly established. In the USA, the annual number of contacts with outpatient primary care providers, i.e. medical practices, hospital ambulances, and emergency rooms, are substantially lower overall: 3.8 contacts per patient in 2006 and 4.1 in 2007 (11).
Frequent attenders
Use of the term “frequent attender” to denote users of outpatient health care varies (12–15), among other reasons because the members of this subgroup of patients are heterogeneous. The definition of a “frequent attender” used in this research, i.e. a patient with at least 24 contacts with his/her primary care physician in one year, was established pragmatically using the 95th percentile of all annual contact numbers in the examined sample. It is useful to identify frequent attenders and deal with them separately, because of their well-known extensive use of primary care services and their particular demand for practice employees’ time (12, 16, 17). In this research, they differ substantially from other patients with respect to their frequent diagnoses and reasons for consultation (not shown here). This difference has not been found in other studies (17). The multiple complaints and illnesses identified for these patients may be, on the one hand, a sign of how difficult it is to allocate frequent attenders to standard categories and medical diagnoses, and on the other hand a cause of increased demand for services.
Longitudinally, the frequent attender patient group was comparable to other sections of the same sample, e.g. patients with chronic or multiple illnesses, to only a limited extent. This is another reason of frequent attenders’ high use of health services, particularly detailed consultations, home visits, emergency care, and (not shown here) hi-tech diagnostics, requires a specific primary care procedure to address it appropriately.
Programs targeting frequent attenders and aiming to reduce their health service use have seen little success at the patient level, particularly those that have been short-term (18). Programs of this kind are more promising at the level of the physician (19). It might be a sign of greater professionalism if all employees of primary care practices reduced the use of inappropriate services for frequent attenders. This is also in line with the recommendations of the US Good Stewardship Working Group and its conclusion that “less is more” (20) to achieve professionalism among physicians as the essential basis for medicine in our society (21).
Other patient groups
Patients with chronic illnesses in this sample required less emergency care per year than other patients. The percentages of patients classified as chronically ill in routine primary care data varied substantially, as was expected, because various definitions of chronic illness were used, in this case those of the Guidelines on Chronically Ill Patients of Germany’s Federal Joint Committee and the M2Q Criterion in the morbidity-oriented risk adjustment scheme. However, these differences between definitions had only marginal effects on services used, in other words the resources used in primary care. With these definitions, particularly high consumption of resources by chronically ill patients was not demonstrated, at least for primary care. Definitions of chronic illness based on illness diagnoses (22) may be insufficient in scope. Additional dimensions that take into account functions and ability to participate and also include patients’ own appraisal should be found (22, 23).
The use of primary care services by patients with multiple illnesses fell between that of the other patient groups. The majority of patients with multiple illnesses received detailed consultation.
Older, and to a still greater extent very elderly, patients required home visits from primary care physicians much more frequently than other age groups and also received emergency care more frequently. However, no differences between age groups were determined in terms of full patient examinations.
Limitations of the research
The examined sample of primary care practices and their routine data was a voluntary sample with varying annual patient numbers. It may therefore have been prone to selection bias. The completeness of the primary data, which were gathered for a purpose other than health services research, varied between practices. With regard to the results based on bills for services, it was ascertained that the data were complete and that the primary sample data were in accord with billing data of the National Association of Statutory Health Insurance Physicians (KBV, Kassenärztliche Bundesvereinigung) (24).
In the EBM 2000plus, primary care billing items were no longer defined for detailed consultation or full examination. As a result, after April 1, 2005 it was no longer possible to make any statements concerning these two personal services of primary care physicians for those with statutory health insurance.
The age group divisions used here had a pragmatic basis: There were no fundamental differences between adolescents and young adults in terms of the examined issues, so they were placed in the same group. In contrast, the group of patients over 80 years old was small in absolute terms.
Conclusion
There was little evidence of high health service use or consumption of resources at appointments with primary care physicians for patients with chronic or multiple illnesses, but there was evidence of this for frequent attenders and elderly and very elderly patients. Demand for services will continue to increase as a result of demographic change (23, 25). In particular, more time-consuming and difficult-to-plan home visits and emergency care are foreseeable. Efficient, patient-centered, high-quality care should be put in place to address this. The first steps might be home visits using specially trained care professionals and case management models for older patient groups, with sufficient room for “talking medicine” and counseling.
Key Messages.
In this research, German patients had a constant rate of 7.3 annual contacts with their primary care physicians between 1996 and 2006.
Frequent attenders’ number of physician contacts and their proportion in total patient number increased markedly with patient age.
Higher patient age was more strongly associated with home visits and emergency care. Patients with multiple illnesses and frequent attenders required more detailed consultations.
Frequent attenders used large amounts of primary care. Patients with chronic illnesses to some extend used less primary care than expected.
Existing definitions of chronic illness are of little use in predicting the use of primary care resources.
Acknowledgments
Translated from the original German by Caroline Devitt, MA.
The authors would like to thank Prof. Wolfgang Himmel, Göttingen for his critical revision of the manuscript of this article.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Health at a Glance 2009. OECD Indicators. English version 2009. www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2009_health_glance-2009-enp.90-91, und http://dx.doi.org/10.1787/718370642522. last accessed on 02.05.2012.
- 2.Koch K, Miksch A, Schürmann C, Joos S, Sawicki PT. The German health care system in international comparison: The primary care physicians’ perspective. Dtsch Arztebl Int. 2011;108(15):255–261. doi: 10.3238/arztebl.2011.0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grobe TG, Dörning H, Schwartz FW. Barmer GEK Arztreport ISEG Institut für Sozialmedizin, Epidemiologie und Gesundheitssystemforschung, Hannover 2010. www.barmer-gek.de/barmer/web/Portale/Presseportal/Subportal/Presseinformationen/Archiv/2010/100119-PK-Arztreport/PDF-Arztreport,property=Data.pdf. last accessed on 02.05.2012. [Google Scholar]
- 4.Himmel W, Hummers-Pradier E, Kochen MM MedViP-Gruppe. Medizinische Versorgung in der hausärztlichen Praxis - Ein neuer Forschungsansatz. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2006;49:151–159. doi: 10.1007/s00103-005-1215-2. [DOI] [PubMed] [Google Scholar]
- 5.Heidenreich R, Himmel W, Boeckmann H, et al. EDV-Erfassung von Routinedaten in hausärztlichen Praxen. Z Ärztl Fortbild Qualitätssich. 2005;99:472–479. [PubMed] [Google Scholar]
- 6.Kersting M, Gierschmann A, Hauswaldt J, et al. Routinedaten aus hausärztlichen Arztinformationssystemen - Export, Analyse und Aufbereitung für die Versorgungsforschung. Gesundheitswesen. 2010;72:323–331. doi: 10.1055/s-0030-1249689. [DOI] [PubMed] [Google Scholar]
- 7.Ihle P, Swart E. GPS - Gute Praxis Sekundärdatenanalyse: Revision nach grundlegender Überarbeitung. Gesundheitswesen. 2008;70:54–60. doi: 10.1055/s-2007-1022529. [DOI] [PubMed] [Google Scholar]
- 8.Bekanntmachung des Gemeinsamen Bundesausschusses. Bundesanzeiger Nr. 18. 2004. Januar. Richtlinie zur Definition schwerwiegender chronischer Krankheiten im Sinne des § 62 des Fünften Buches Sozialgesetzbuch (SGB V) 1343 pp. [Google Scholar]
- 9.Bundesversicherungsamt. So funktioniert der neue Risikostrukturausgleich im Gesundheitsfonds. Stand: 16. September 2008. www.bundesversicherungsamt.de/cln_115/nn_1046746/DE/Risikostrukturausgleich/risikostrukturausgleich__node.html?__nnn=true, last accessed on 02.05.2012.
- 10.Bundesversicherungsamt. Bekanntgabe vom 13.05.2008, erneuert für 2011 am 30.06.2010. www.bundesversicherungsamt.de/cln_115/nn_1440668/DE/Risikostrukturausgleich/Festlegungen/Festlegung__zu__beruecksichtigende__Krankheiten.html. last accessed on 02.05.2012.
- 11.Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2007. Vital Health Stat 13. 2011;169:1–38. [PubMed] [Google Scholar]
- 12.Vedstedt P, Christensen MB. Frequent attenders in general practice care: a literature review with special reference to methodological considerations. Public Health. 2005;119:118–137. doi: 10.1016/j.puhe.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 13.Luciano JV, Fernandez A, Pinto-Meza A, Lujan L, Bellon JA, et al. Frequent attendance in primary care: comparison and implications of different definitions. Br J Gen Pract. 2010;60:49–55. doi: 10.3399/bjgp10X483139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koskela TH, Ryynanen OP, Soini EJ. Risk factors for persistent frequent use of the primary health care services among frequent attenders: a Bayesian approach. Scand J Prim Health Care. 2010;28:55–61. doi: 10.3109/02813431003690596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scherer M, Himmel W, Kochen MM, et al. Psychosocial determinants for frequent primary health care utilisation in patients with heart failure. GMS Psychosoc Med. 2008;5 Doc02, 1-7 [PMC free article] [PubMed] [Google Scholar]
- 16.Green I, Israeli V, Vinker S. [„Oh no, not him again“ frequent attenders: the range of the phenomenon and how to cope with it?] Harefuah. 2008;147:910. 3, 939, 938 (Abstract) [PubMed] [Google Scholar]
- 17.Bergh H, Marklund B. Characteristics of frequent attenders in different age and sex groups in primary health care. Scand J Prim Health Care. 2003;21:171–177. doi: 10.1080/02813430310001149. [DOI] [PubMed] [Google Scholar]
- 18.Smits FT, Brouwer HJ, ter Riet G, van Weert HC. Epidemiology of frequent attenders: a 3-year historic cohort study comparing attendance, morbidity and prescriptions of one-year and persistent frequent attenders. BMC Public Health. 2009;9 doi: 10.1186/1471-2458-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bellon JA, Rodriguez-Bayon A, de Dios Luna J, Torres-Gonzalez F. Successful GP intervention with frequent attenders in primary care: randomised controlled trial. Br J Gen Pract. 2008;58:324–330. doi: 10.3399/bjgp08X280182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The „Top 5“ Lists in Primary Care - Meeting the Responsibility of Professionalism. Arch Intern Med. The Good Stewardship Working Group. Published online May 23, 2011. doi: 10.1001/archinternmed. 2011.231, last accessed on 27.07.2011. [DOI] [PubMed] [Google Scholar]
- 21.Medical Professionalism in the New Millenium. A Physician Charter. 2002. www.abimfoundation.org/Professionalism/˜/media/Files/Physician%20Charter.ashx. last accessed on 02.05.2012. [DOI] [PubMed]
- 22.Schmidt S, Thyen U. Was sind chronisch kranke Kinder? Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2008;51:585–591. doi: 10.1007/s00103-008-0534-5. [DOI] [PubMed] [Google Scholar]
- 23.Scheidt-Nave C, Richter S, Fuchs J, Kuhlmey A. Herausforderungen an die Gesundheitsforschung für eine alternde Gesellschaft am Beispiel „Multimorbidität“. Bundesgesundheitsbl. Gesundheitsforschung Gesundheitsschutz. 2010;53:441–450. doi: 10.1007/s00103-010-1052-9. [DOI] [PubMed] [Google Scholar]
- 24.Hauswaldt J, Kersting M, Hummers-Pradier E. Influenza-Impfungen durch Niedersächsische Hausärzte - eine Sekundäranalyse vertragsärztlicher Versorgungsdaten aus 1995/1996, 2002/2003 und 2005/2006. Gesundheitswesen. 2010;72:332–339. doi: 10.1055/s-0030-1249690. [DOI] [PubMed] [Google Scholar]
- 25.Sievert U, Fendrich K, Dobljammer-Reiter G, Scholz RD, Schneff-Werner P, Hoffmann W. Health care consequences of demographic changes in Mecklenburg - West Pomerania: projected case numbers for age-related diseases up to the year 2020, based on the study of health in Pomerania (SHIP) Dtsch Arztebl Int. 2010;107(18):328–334. doi: 10.3238/arztebl.2010.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]