Abstract
Podostroma cornu-damae is a rare fungus that houses a fatal toxin in its fruit body. In this case report, two patients collected and boiled the wild fungus in water, which they drank for one month. One patient died, presenting with desquamation of the palms and soles, pancytopenia, severe sepsis and multiple organ failure. The other patient recovered after one month of conservative care after admission. We found a piece of Podostroma cornu-damae in the remaining clusters of mushrooms. Mushroom poisoning by Podostroma cornu-damae has never been previously reported in Korea.
Keywords: Podostroma cornu-damae, mushroom, poisoning, pancytopenia
INTRODUCTION
Among thousands of species of mushrooms worldwide, about 30 species are known to be fatally poisonous.1 Amateur hunters often mistake poisonous mushrooms for edible mushrooms. They then harvest them to eat and give to others, leading to a string of poisonous events and even deaths. Fatal poisonings commonly occur when mushrooms belonging to the genus Amanita, such as Amanita phalloides, are consumed, as these mushrooms contain the lethal toxin, amatoxin.2 However, other cases of poisoning by other species of mushrooms have been reported.3-5
Podostroma cornu-damae is a rare species of fungus belonging to the Hyocreaceae family. Its fruit body is highly toxic, containing trichothecene mycotoxins. Several fatal cases of poisoning by Podostroma cornu-damae have been reported in Japan,6 but to our knowledge no cases have ever been reported in Korea. Here, we report two cases of poisoning by Podostroma cornu-damae.
CASE REPORT
Case 1
A 64-year old man visited the emergency department with a 10-day history of fever, desquamation on his palms, soles and scalp (Fig. 1). He had a medical history of hypertension and was currently taking medication. Upon admission, his vital signs included a blood pressure of 77/55 mm Hg, heart rate of 114 beats/min, respiratory rate of 18 times/min and a body temperature of 38.2℃. He complained of a fever, chilling sensation, generalized weakness, mild headache, and a sore throat. He did not complaint of chest pain, dyspnea, abdominal pain or diarrhea. Also there were no symptoms of paresthesia or visual disturbance. Physical examination revealed an alert mentality, poor skin turgor, a dried tongue and lips, mild throat injection, desquamation on his palms and soles, and hair loss. Initial laboratory tests showed pancytopenia with a white blood cell (WBC) count of 120/µL [absolute neutrophil count (ANC) 20/µL], hemoglobin (Hb) of 11.2 g/dL, and a platelet count of 5000/µL; elevated erythrocyte sedimentation rate (135 mm/hr) as well as C-reactive protein (159 mg/L) and ferritin (898 µg/L); and normal blood urea nitrogen (BUN), serum creatinine (Cr) (20.4/0.82 mg/dL), aspartate aminotransferase (AST)/alanine aminotransferase (ALT) (15/20 IU/L) and total bilirubin (0.8 mg/dL). A simple chest X-ray did not reveal any abnormal findings, and an abdominal-pelvic CT scan, which was performed to evaluate the causes of the pancytopenia and intraabdominal infection focus, did not show any hepatosplenomegaly or infiltrating mass lesion in the liver or spleen, abnormal enlargement of intraabdominal lymph nodes, or any abnormal finding as to the cause of the severe sepsis. Treatment comprising fluid resuscitation with crystalloid and the use of norepinephrine was also performed. Also, intravenous penicillin G (400 million IU, q 4 hrs), clindamycin (600 mg, q 8 hrs), and intravenous immunoglobulin (2 g/kg) were administered considering the possibility of streptococcal toxic shock syndrome.
Fig. 1.
This picture shows the desquamation on the sole of the Case 1 patient.
On hospital day (HD) 2, the patient's high temperature was sustained and pancytopenia was aggravated with a WBC count of 90/µL (ANC 20/µL), Hb of 6.3 g/dL, and a platelet count of 5000/µL, despite the administration of granulocyte-colony stimulating factor and a transfusion of packed red blood cell and platelet concentrate. However, because of prolonged shock and high inotropic demand, bone marrow aspiration and biopsy could not be performed. Multiple organ failure developed with elevated BUN/Cr (56.8/2.51 mg/dL), AST/ALT (3414/873 IU/L), total bilirubin (4.6 mg/dL) and ferritin (>15000 µg/L). The patient complained of dyspnea, and his respiratory rate was 30 times per minute. Arterial blood gas analysis revealed mild hypoxemia (PaO2 73 mm Hg under administration of 2 liters per minute of oxygen through nasal cannula). Chest X-ray showed newly developed consolidations in both lower lung fields. We then changed the patient's antibiotics to piperacillin/tazobactam (2.25 g, q 6 hrs) and vancomycin (1 g, q 24 hrs) for the treatment of pneumonia and neutropenic severe sepsis.
Methicillin sensitive Staphylococcus aureus and Klebsiella pneumoniae, which were susceptible to the given antibiotics, were grown in a blood culture upon admission. The patient received mechanical ventilation and continuous renal replacement therapy beginning on HD 4 because of acute respiratory distress syndrome and acute renal failure in the intensive care unit. On HD 6, the patient expired as a result of intractable multiple organ failure. The patient's severe pancytopenia was not recovered until death.
Case 2
A 60-year old woman, the wife of Case 1, was admitted to our hospital due to a sore throat on the first day and a fever on the third day of the husband's hospitalization. Upon admission, her vital signs included a blood pressure of 131/67 mm Hg, heart rate of 102 beats/min, respiratory rate of 18 times/min and a body temperature of 39.2℃. She did not have any previous medical or medication history. There were no symptoms of dyspnea, abdominal pain, vomiting, diarrhea or paresthesia. Physical examination showed alert mentality, a dried tongue and lips, throat injection and purpura of both lower extremities without desquamation. Initial laboratory tests indicated severe pancytopenia with a WBC count level of 350/µL (ANC 30/µL), Hb of 9.7 g/dL, and a platelet count of 4000/µL; as well as an elevated erythrocyte sedimentation rate (107 mm/hr), C-reactive protein (274 mg/L) and ferritin (747 µg/L). Other laboratory and image tests showed no signs of any other problems. Accordingly, the transfusion of platelet concentrate and antibiotic therapy with piperacillin/tazobactam (4.5 g, q 8 hrs), vancomycin (1 g, q 12 hrs) were initiated. The patient's medical history concerning previous medications was again questioned as the patient's clinical manifestations developed in a similar pattern to that of Case 1. We found that the couple harvested and dried wild mushrooms from a nearby forest, which were mistaken as Ganoderma lucidum, the previous summer, and had been drinking water from the boiled mushrooms daily for over a month before admission. We asked the agricultural microbiology team of the National Academy of Agricultural Science in Korea to identify the patient's remaining mushrooms and found a piece of the poisonous mushroom Podostroma cornu-damae among samples of Ganoderma lucidum (Figs. 2 and 3).
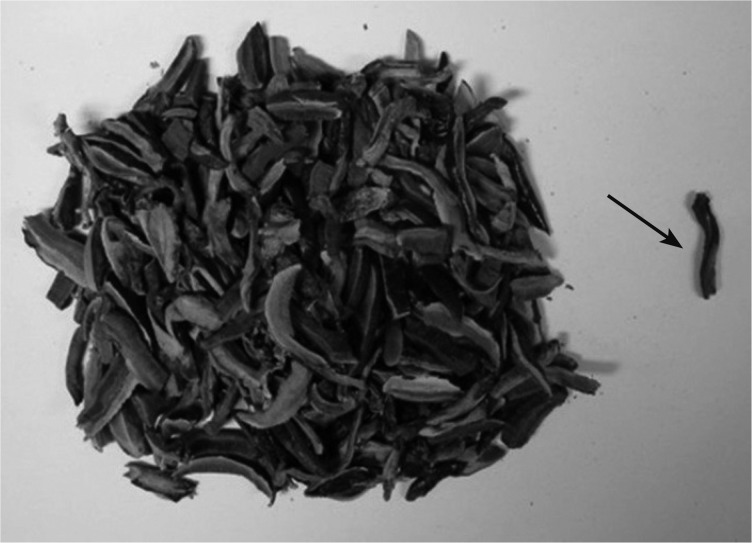
Fig. 2.
Analysis of the remaining mushrooms by the agricultural microbiology team of the National Academy of Agricultural Science. Left clusters of mushrooms are Ganoderma lucidum, while the piece on the right (arrow) turned out to be Podostroma cornu-damae.
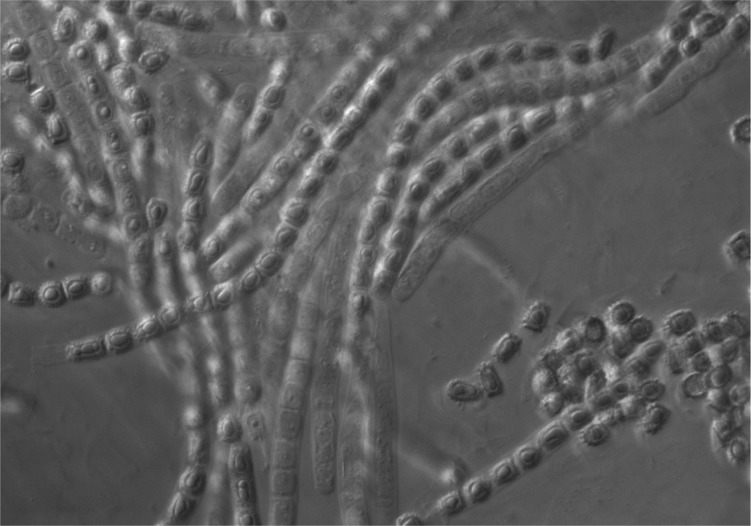
Fig. 3.
This figure shows the spores of Podostroma cornu-damae (×100).
Because of prolonged severe pancytopenia, bone marrow biopsy was performed at HD 11, and revealed hypocellular marrow (average of less than 10% cellularity). Initial blood culture showed no growth of any micro-organisms. However, the patient's fever did not subside, so antibiotics were administered continuously to try to treat the patient's neutropenic fever. On HD 24, the patient recovered from pancytopenia and the fever subsided. On HD 25, we stopped the administration of antibiotics, and on HD 27, the patient was discharged without any complications.
DISCUSSION
Podostroma cornu-damae was first discovered in China in 1895. It was originally described as Hypocrea cornu-damae and then later renamed Podostroma by a Japanese mycologist.7,8 The fungus is known to exist in Japan, China, Java, and also in Korea. It is shaped like a deer's red horn, but in its immature period, it resembles Ganoderma lucidum, which is well known as a health-food.9
In 1999, a group of five people in Japan ate 1 gram of Podostroma cornu-damae found soaked in sake. One of these five people died two days after ingesting the sake.6 Another report included information on 13 cases of ingestion of several centimeters of Podostroma from 1983 to 2008, two of which had died.5 Ingesting only a small amount of this mushroom can be extremely fatal. In 2001, Saikawa, et al.6 discovered the chemical components of the macrocyclic trichothecene group of toxins in the fruit body of this fungus, including satratoxin H 12'-18'-diacetate, satratoxin H 12'-acetate, satratoxin H 13'-acetate, satratoxin H, roridin E, and verucarin J. If poisoned by Podostroma cornu-damae, the common symptoms are diarrhea, vomiting and dehydration in the early stage. This is followed by hypotension, oliguria, changes in perception, and disturbance of consciousness. Without treatment, leukopenia, thrombocytopenia, lamellar desquamation on the palms and face, as well as hair loss can develop. Patients usually die of multiple organ failure, including acute renal injury, disseminated intravascular coagulation and liver necrosis.10 Despite our understanding of the conditions and the chemical background of this poison, there is still no curative treatment available, although one report stated continuous hemodiafiltration, plasma exchange and granulocyte colony stimulating factor with a large volume of intravenous fluid resuscitation resulted in recovery in one patient.11
Unlike other previously reported cases, the cases in this report involved symptoms that appeared one month after first ingesting the poisonous mushrooms. The first patient presented with hypotension, desquamation and multiple organ failure, and died despite undergoing intensive treatment. The second patient complained of only mild symptoms and recovered after conservative care, irrespective of the prolonged severe pancytopenia. According to the analysis of the patients' remaining mushrooms, most of them were Ganoderma lucidum, and only one piece of the dried mushroom turned out to be Podostroma cornu-damae. Therefore, the patients seemed to have ingested only a very small amount of Podostroma cornu-damae. They also did not consume the mushroom directly, but boiled them in water with other pieces of mushrooms. Both patients drank the mushroom water instead of regular drinking water. The second patient said that her husband drank more water than she had. Therefore, we surmised that the small amount of toxin intake over a long period of time influenced the clinical course of the poisoning; however, the exact mechanism by which the toxins poisoned the body at clinical presentation is still unknown.
The information obtained from these two cases can be used to help better treat future patients that present with an unknown cause of neutropenic fever with pancytopenia and desquamation on the palms and soles. Furthermore, physicians should be sure to ask patients about any history of ingesting wild mushrooms, all the while considering the possibility of Podostroma cornu-damae poisoning, when such symptoms appear.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Ford M, Delaney KA, Ling L, Erickson T. Clinical Toxicology. 2001. [Google Scholar]
- 2.Klein AS, Hart J, Brems JJ, Goldstein L, Lewin K, Busuttil RW. Amanita poisoning: treatment and the role of liver transplantation. Am J Med. 1989;86:187–193. doi: 10.1016/0002-9343(89)90267-2. [DOI] [PubMed] [Google Scholar]
- 3.Lee HY, Park CW, Cho JH, Cheon SB, Moon JB. A case of Naematololma Fasciculare poisoning due to misidentification as an edible mushroom. J Korean Soc Emerg Med. 2011;22:181–183. [Google Scholar]
- 4.Shi GQ, Huang WL, Zhang J, Zhao H, Shen T, Fontaine RE, et al. Clusters of sudden unexplained death associated with the mushroom, Trogia venenata, in rural Yunnan Province, China. PLoS One. 2012;7:e35894. doi: 10.1371/journal.pone.0035894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yokoyama K, Gonmori K. [Increase of poisoning by tropical mushrooms in Japan in recent years] Chudoku Kenkyu. 2009;22:240–248. [PubMed] [Google Scholar]
- 6.Saikawa Y, Okamoto H, Inui T, Makabe M, Okuno T, Suda T, et al. Toxic principles of a poisonous mushroom Podostroma cornu-damae. Tetrahedron. 2001;57:8277–8281. [Google Scholar]
- 7.NT P. Enumeration of mushrooms harvested by RR. PP. Soulie at Farges, in eastern Tibet and Su-tchuen. Newsl Mycol Soc Fr. 1895;11:196–199. [Google Scholar]
- 8.Izawa H. Podostroma cornu-damae(pat) Mycobank International Mycological Association; 1994. [Google Scholar]
- 9.Rural Development Administration News. 2012. Beware the toxic mushroom, Podostroma cornu-damae which resembles Ganoderma lucidum. [Google Scholar]
- 10.Koichi M, Haruo T, Toshihiro Y, Masami O, Sadao N, Koichiro K. Case report: food poisoning to death by Podostroma cornu-damae, its case history and autopsy findings. Acta Criminol Med Leg Jan. 2003;69:14–20. [Google Scholar]
- 11.Suzuki M, Katoh Y, Kumagai H, Saitoh M, Ishikawa H, Itoh H, et al. [Successful treatment in a case of podostroma cornu-damae poisoning, a deadly poisonous mushroom] Chudoku Kenkyu. 2002;15:177–182. [PubMed] [Google Scholar]