Abstract
Although the ocular higher order aberrations degrade the retinal image substantially, most studies have investigated their effect on vision only under monocular conditions. Here, we have investigated the impact of binocular higher order aberration correction on visual performance and binocular summation by constructing a binocular adaptive optics (AO) vision simulator. Binocular monochromatic aberration correction using AO improved visual acuity and contrast sensitivity significantly. The improvement however, differed from that achieved under monocular viewing. At high spatial frequency (24 c/deg), the monocular benefit in contrast sensitivity was significantly larger than the benefit achieved binocularly. In addition, binocular summation for higher spatial frequencies was the largest in the presence of subject’s native higher order aberrations and was reduced when these aberrations were corrected. This study thus demonstrates the vast potential of binocular AO vision testing in understanding the impact of ocular optics on habitual binocular vision.
OCIS codes: (330.0330) Vision, color, and visual optics; (330.1400) Vision - binocular and stereopsis; (330.4300) Vision system - noninvasive assessment; (330.4595) Optical effects on vision; (330.4460) Ophthalmic optics and devices; (330.7327) Visual optics, ophthalmic instrumentation
1. Introduction
Optical and surgical methods, such as adaptive optics(AO) [1–5], phase plates [6,7], customized soft contact lenses [8,9] and laser refractive surgery [10] have been proposed to compensate higher order aberrations to provide improvement in vision beyond conventional sphero-cylindrical refraction. Significant improvements in visual acuity (VA) [2,3], contrast sensitivity (CS) [1,2,5] and real-life tasks [4] have been demonstrated following higher order aberration correction. However, most studies on optical correction of higher order aberrations are limited to monocular vision, although the normal human visual system is binocular resulting from the convergence of two monocular channels. It has long been known that binocular visual performance is superior to monocular performance, a phenomenon commonly referred to as binocular summation [11]. The magnitude and characteristics of binocular summation have been studied for many aspects of visual function [11–17]. In particular, CS and VA are known to be enhanced by a factor of approximately √2 and 1.1, respectively [11,12]. However, binocular summation is not entirely determined by neural factors in the visual system, but also depends on interocular differences in optical quality. This is evident from previous studies of binocular vision in the presence of interocular difference in optical quality, pertaining to anisometropia [18,19], addition of monocular defocus [20], interocular differences in higher order aberrations [21], corneal shape [22,23], contrast and spatial frequency [24]. Such interocular differences in optical aberrations occur routinely after clinical procedures such as laser refractive surgery [23,25]. In general, binocular summation has been observed to decrease with increasing interocular difference in optical quality [20,22]. On the other hand, a compensatory role of binocular summation in the presence of ocular aberrations was demonstrated recently. Plainis et al. [26] showed that binocular summation increased with increasing defocus in both eyes, suggesting that binocular vision ameliorates the effect of defocus. In the presence of such profound interactions of the optical aberrations with the binocular visual system, it is of both scientific and clinical interest to be able to non-invasively investigate the role of ocular aberrations on normal binocular vision. Among other questions relevant to binocular vision and customized optical correction, one that begs investigation is whether the visual benefit upon higher order aberration correction, hitherto estimated monocularly, transfers similarly to binocular vision. In addition, the role of optical aberrations on stereopsis demands further investigation [27]. To this end, optical systems for simultaneous measurement of ocular aberration have been demonstrated [28,29]. Also, AO has been introduced in such vision testing instruments either in one eye or in both eyes simultaneously to examine the effect of higher order aberration manipulation on binocular vision [30,31]. Fernandez et al. [31] demonstrated an effective binocular AO vision simulator by employing a single wavefront sensor and a liquid crystal device as the wavefront corrector. Employing a liquid crystal device in an AO system requires the use of monochromatic polarized light for testing vision. In this article, a binocular AO system based on deformable mirrors as the wavefront corrector is introduced to study binocular visual performance in normal polychromatic viewing conditions. The improvement in binocular vision after either a correction of spherical aberration (SA) or all higher order aberrations in both eyes is investigated in a group of young normal subjects. The same measures under monocular viewing are obtained to aid in understanding the effect of binocular summation with corrected and native retinal image quality. Finally, the implication of this investigation on wavefront-guided treatments is discussed.
2. Methods
2.1. Subjects
The University of Rochester Research Review Board approved this research and all subjects signed an informed consent form before their participation in this study. All procedures involving human subjects were in accordance with the tenets of the Declaration of Helsinki. Five young subjects (age: 27 ± 2.4 yo) were enrolled in this study. All subjects reported normal eye health in a standard ophthalmic examination and did not require any spherocylindrical correction in a clinical refraction. Paralysis of accommodation and dilation of both pupils in all subjects was achieved with 1% tropicamide ophthalmic solution. The average higher order RMS wavefront error was 0.35 ± 0.11 and 0.31 ± 0.04 μm in the right and left eyes, respectively, of the 5 subjects.
2.2. Binocular adaptive optics system
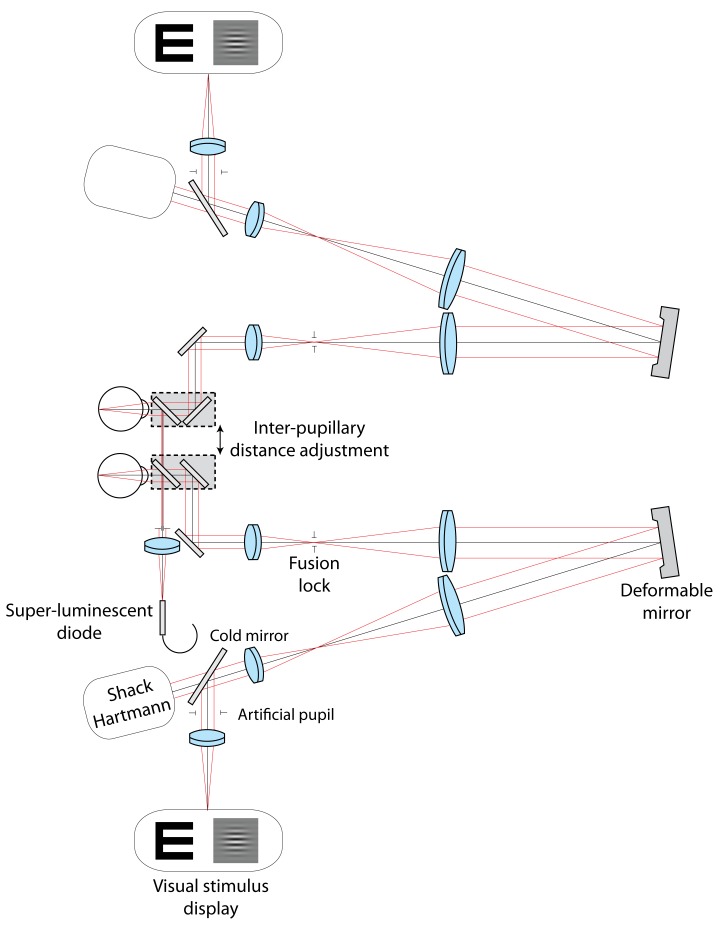
A binocular AO system for vision testing was constructed with two identical monocular AO channels. Figure 1 shows the optical layout of the system. Each monocular AO system consisted of a Shack-Hartmann wavefront sensor, a large-stroke deformable mirror (Imagine Eyes: Mirao-52) and a visual stimulus display. This AO system is described in detail elsewhere [32,33]. A single super-luminescent diode (Δλ = 40 nm at λ = 840 nm) was used as a laser beacon for wavefront sensing in both eyes. The remaining corresponding optical components in both the monocular AO systems had identical specifications.
Fig. 1.
Optical layout of the binocular AO system for vision testing. The system consists of two identical monocular channels. Each monocular system consists of a deformable mirror, Shack-Hartmann wavefront sensor and visual stimulus display.
An optical path for psychophysical testing using visible wavelengths was incorporated in each system by using a cold mirror. Aberrations were controlled over a 6.5 mm pupil with AO while the stimuli for VA and CS testing were viewed through an artificial adjustable pupil placed conjugate to the eye’s pupil and set to 6 mm. For monocular vision testing, the untested eye was occluded. Aberrations were corrected continuously, in real-time and closed loop at 12 Hz, during the psychophysical test so that optical quality could be reliably maintained. In binocular viewing, both the AO systems were operated concurrently. The subjects were asked to blink at their discretion during psychophysics, at which points the correction was temporarily suspended. AO closed-loop gain of 90-100% was employed to ensure fast convergence of correction within 1-3 iterations after blink. To minimize fixation disparity, two identical apertures placed in the retinal conjugate planes of both AO channels served as a binocular fusion lock. These apertures were set to a retinal extent of 2 deg and were concentric with the visual field of 1 deg for both VA and CS. Under binocular viewing, subjects reported single vision without diplopia. Head movements were stabilized in all subjects using a bite bar mount. The eyes’ pupils were monitored continuously using a camera focused at the pupil planes. For every subject, inter-pupillary distance was adjustable using a translational stage between 50 and 80 mm in accordance with population statistics [34].
VA was measured using a tumbling letter ‘E’ test at 100% contrast in white light using the four-alternate forced-choice method. The black letter on a white background was displayed on a digital light projector (Sharp PG-M20X) placed at the retinal plane in each system, which corresponded to optical infinity for each eye. For a 6 mm pupil, the retinal illuminance was adjusted to 60 cd/m2 using neutral density filters. The test was initiated by the observer with a keypress following which the observer responded to the orientation of a letter ‘E’ displayed for 500 ms in one of 4 orientations (0, 90, 180, 270 deg). The response was followed by auditory feedback and an inter-stimulus interval of 500 ms. The letter size was adjusted according to the QUEST [35] paradigm in 30 stimulus presentations. Acuity threshold was taken as the letter size for which 62.5% of the responses were correct. Four threshold measurements were averaged per optical condition.
CS was measured similarly using a two-alternate forced choice method where the observer discriminated between vertical and horizontal 2-D Gabor functions. The spatial frequencies tested were 4, 8, 16 and 24 c/deg. The 2-D Gabor functions consist of a sinusoidal luminance distribution of the spatial frequency under test, overlaid with a Gaussian envelope. The Gaussian window eliminates high spatial frequencies at the edges of the stimulus which are otherwise present when using a sharp rectangular window. For generating low-contrast stimuli, a video-switcher [36] was employed in conjunction with a gamma-calibrated cathode-ray-tube monitor (NEC Multisync fp950) to increase the luminance resolution up to 14-bit. The monitor was placed at the retinal plane and the retinal illuminance for a 6 mm pupil was 10 cd/m2. Stimuli were displayed for 250 ms followed by the observer’s response, auditory feedback and an inter-stimulus interval of 250 ms. The contrast was adjusted according to the QUEST [35] paradigm in 40 stimulus presentations. The threshold was taken as the contrast at which 75% of the responses were correct. Two QUEST staircases corresponding to different spatial frequencies were randomly interleaved during each measurement trial. Three threshold measurements were averaged per optical condition and spatial frequency.
2.3. Experimental conditions
The visual performance measurements were performed under 3 optical conditions: (a) defocus and astigmatism correction only, (b) correction of SA in addition to defocus and astigmatism, (c) correction of all monochromatic aberrations. Henceforth in this article, these are referred to as baseline correction, SA correction and complete correction, respectively. First, the monocular measurements were performed in each eye, with the fellow eye occluded. In each condition, subjects monocularly adjusted the defocus using the Badal system (not shown in figure) to optimize image quality for a 20/40 Snellen letter ‘E’. VA and CS were subsequently measured while the optical quality was maintained with AO. The same measurements were then obtained when the subjects viewed the visual stimulus binocularly. In this case, the aberration manipulation was performed concurrently in both eyes. The aberration correction conditions were randomized during both monocular and binocular vision testing. Visual benefit under conditions (b) and (c) was quantified as the ratio of visual performance of condition (b) or (c) to condition (a). Binocular summation was defined as the ratio of binocular visual performance to the better eye’s monocular visual performance.
3. Results
3.1. Binocular higher order aberration correction
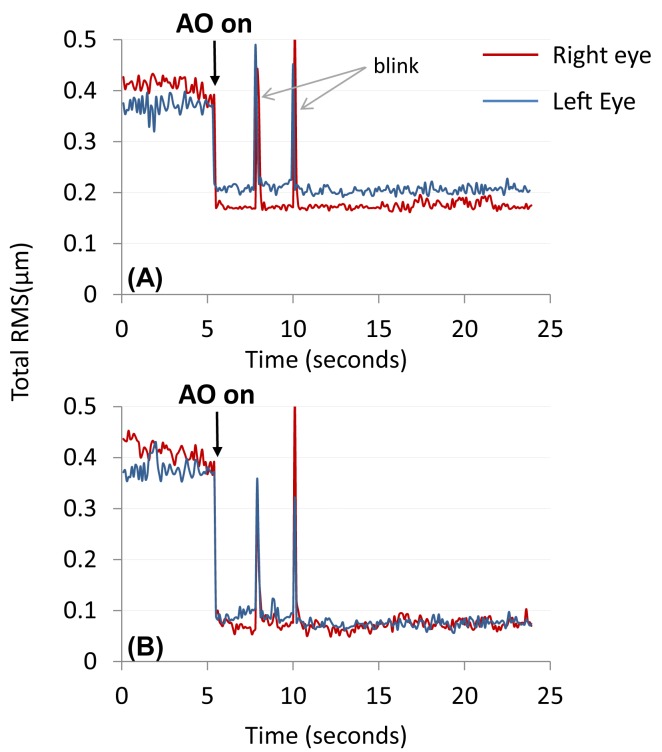
Table 1 shows the summary of optical quality in the 5 subjects, i.e. their native SA and total higher order aberrations over a 6 mm pupil. The variability of the wavefront measurements was smaller than 0.02 µm RMS across subjects and optical conditions. Figure 2 shows the representative time-course of total RMS in one subject for both eyes during vision testing. The arrow signifies the time-point when AO correction was initiated. With a high closed-loop gain, the desired optical quality was achieved immediately upon AO correction and remained stable in both eyes. The peaks in the time-course correspond to blinks during testing at which points, the correction was suspended. With baseline correction, the mean ± standard deviation RMS was 0.34 ± 0.12 µm and 0.30 ± 0.05 µm in the right and left eyes, respectively. In the SA correction condition, the residual RMS of SA was reduced to around 0.01 µm. In this condition, the mean ± standard deviation RMS of the remaining higher order aberrations in the subjects was 0.31 ± 0.07 µm and 0.26 ± 0.04 µm in the right and left eyes, respectively. Upon complete correction of all aberrations, the residual RMS was around 0.08 µm in both eyes of all subjects. The RMS optical error was not statistically different between both eyes in any of the conditions (p > 0.1).
Table 1. Summary of optical quality over 6 mm pupil in the 5 subjects for both eyes.
| Subject # | Spherical aberration (µm) | Higher order aberration (µm) | |||
| OD | OS | OD | OS | ||
| 1 | 0.23 | 0.22 | 0.44 | 0.31 | |
| 2 | 0.30 | 0.18 | 0.46 | 0.35 | |
| 3 | 0.01 | −0.05 | 0.21 | 0.27 | |
| 4 | 0.17 | 0.20 | 0.40 | 0.35 | |
| 5 | −0.07 | −0.03 | 0.24 | 0.26 | |
Fig. 2.
Representative time-course of total RMS for (A) SA correction and (B) complete correction during the visual performance testing for 1 subject. Peaks in the time course correspond to blinks.
3.2. Visual benefit of binocular higher order aberration correction
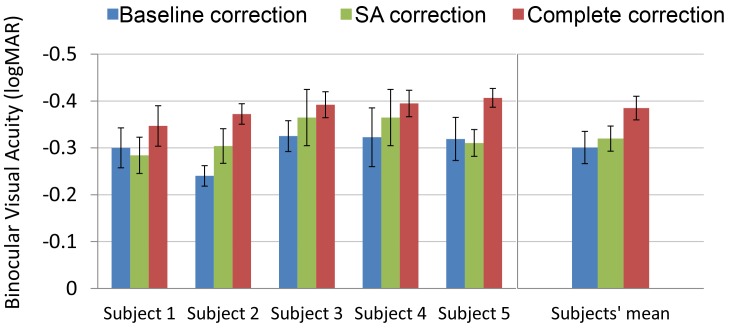
Figure 3 shows the binocular VA under the 3 conditions for all the 5 subjects. The VA at baseline was −0.30 ± 0.03 logMAR on average. With SA correction, there was slight improvement by a factor of 1.05 on average in the 5 subjects in binocular VA. However, a paired t-test revealed that this improvement was not statistically significant (p = 0.27). The maximum improvement in VA from −0.24 to −0.30 logMAR upon SA correction was demonstrated in subject 2, who had the maximum magnitude of SA (OD: 0.30 µm, OS: 0.18 µm). Complete correction improved VA in all subjects, on average by a factor of 1.22 compared to baseline and this improvement was statistically significant (p < 0.05). Subject 2, who had the largest magnitude of higher order RMS (OD: 0.46 µm, OS: 0.35 µm), expectedly demonstrated the maximum benefit in VA from complete correction by a factor of 1.36.
Fig. 3.
Binocular visual acuity under the 3 conditions for the 5 subjects and their average. On average, binocular SA correction provided an improvement by a factor of 1.05 while binocular complete correction improved visual acuity by a factor of 1.22 compared to baseline.
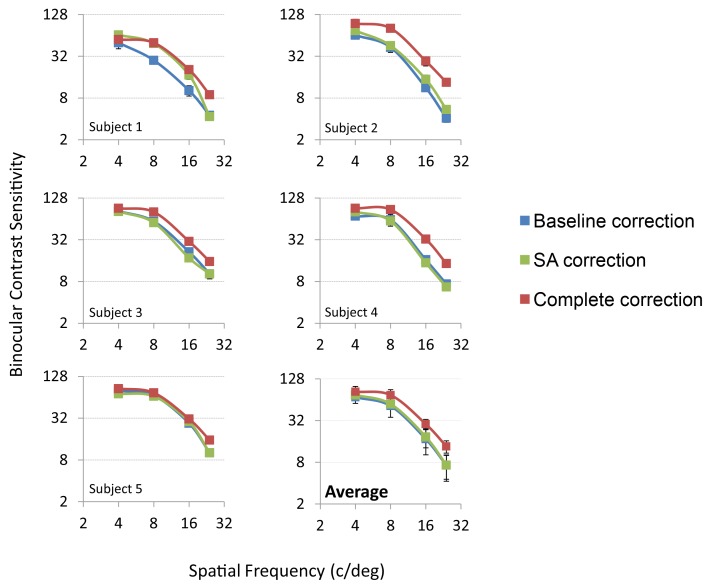
Figure 4 shows the average binocular CS function under the 3 conditions for all the 5 subjects. Binocular SA correction led to an average improvement in CS by a factor of 1.1, 1.1, 1.2 and 1.1 at 4, 8, 16 and 24 c/deg respectively. This improvement was not statistically significant for any spatial frequency (p>0.05 for all spatial frequencies). Complete correction improved CS by a factor of 1.2, 1.5, 1.8 and 2.1 at 4, 8, 16 and 24 c/deg respectively (p < 0.05 across all spatial frequencies). Subjects 1, 2 and 4 had higher order RMS errors greater than 0.30 µm in both eyes and thus also correspondingly demonstrated the maximum visual benefit of complete correction. From both VA and CS, it was observed that binocular SA correction provided relatively small benefit over baseline correction. However, complete binocular correction provided significant improvement in visual performance over SA correction and baseline.
Fig. 4.
Binocular contrast sensitivity under the 3 conditions for the 5 subjects and their average. On average, binocular SA correction led to an average improvement in contrast sensitivity by a factor of 1.1, 1.1, 1.2 and 1.1 at 4, 8, 16 and 24 c/deg, respectively, compared to baseline. At the same frequencies, binocular complete correction improved contrast sensitivity by a factor of 1.2, 1.5, 1.8 and 2.1, respectively.
3.3. Binocular vs. monocular visual benefit
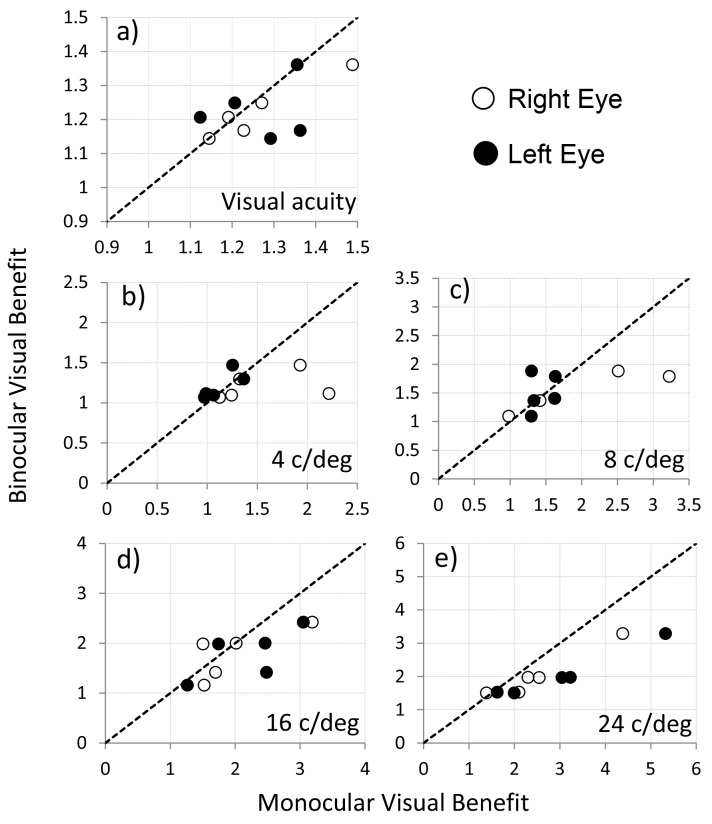
Figure 5 compares the binocular visual benefit to the monocular case. The visual benefits correspond to the improvement in VA (a) and CS for all spatial frequencies (b-e) upon complete correction over baseline. The x-axis and y-axis show the monocular and binocular visual benefit, respectively. The dashed line represents equality in benefit between binocular and monocular viewing; data points lying above the line indicate higher binocular visual benefit as compared to monocular visual benefit and vice-versa. The open and filled symbols represent the visual benefit for one subject for the right and left eye, respectively. For VA, the average binocular visual benefit was smaller than the monocular case, but the difference was not statistically significant (p > 0.05). For CS, the binocular visual benefit was not different than the monocular visual benefit for 4 and 8 c/deg. However, for 16 and 24 c/deg, the binocular visual benefit was smaller than the monocular benefit on average. This difference tended towards statistical significance for 16 c/deg (p = 0.07) and was statistically significant for 24 c/deg (p < 0.05). On average between subjects, the binocular visual benefit of complete correction was smaller than monocular visual benefit at 16 c/deg by 11% and 23% for the right and left eyes respectively. At 24c/deg, the binocular visual benefit was smaller than the monocular case by 24% and 48% for the right and left eyes respectively. Therefore, for higher spatial frequencies, the monocular visual benefit achieved upon higher order aberration correction overestimated the improvement in binocular vision obtainable by such correction.
Fig. 5.
Binocular vs. monocular visual benefit for visual acuity (a) and contrast sensitivity (b)-(e) for different spatial frequencies. Each data point represents the visual benefit for one subject for the complete correction condition under monocular (x-axis) and binocular (y-axis) viewing. The dashed line represents equality in visual benefit between binocular and monocular viewing.
3.4. Binocular summation
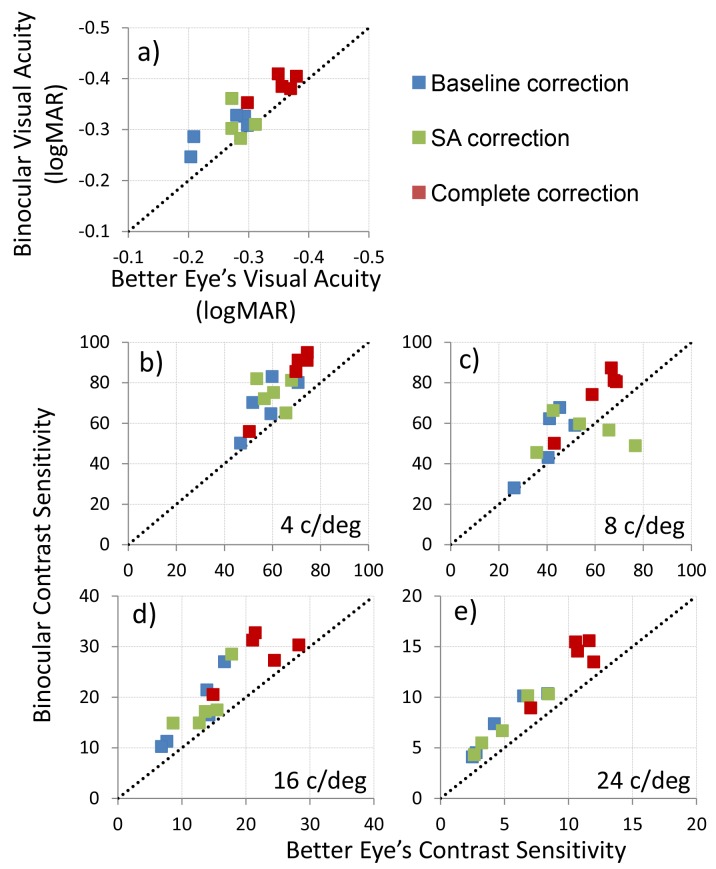
Figure 6 shows the monocular (better eye) and binocular VA (a) and CS for all spatial frequencies (b)-(e) for the three optical correction conditions. The x-axis and y-axis represent the better monocular visual performance and binocular visual performance, respectively, while the dashed line represents equality between the two. Data points lying above this dashed line indicate superior binocular performance, demonstrating binocular summation. Binocular VA and CS were better than the monocular case across all three optical conditions. Binocular summation in VA was equal to 1.1 or 10% on average between subjects for all three optical conditions. Binocular summation in CS was equal to1.4, 1.3, and 1.3 for baseline, SA correction and complete correction on average between subjects and spatial frequencies. For any given spatial frequency, no statistical difference was observed between the optical conditions. However, with increasing spatial frequency, the paired t-test p-values decreased when comparing binocular summation at baseline and complete correction. Four out of five subjects demonstrated increased binocular summation at baseline compared to complete correction for 16 c/deg and 24 c/deg. A paired t-test comparing binocular summation at baseline and complete correction, however, did not reveal significance at these frequencies (p = 0.37 for 16 c/deg and p = 0.08 for 24 c/deg).
Fig. 6.
Binocular vs. better monocular visual acuity (a) and contrast sensitivity (b)-(e) for the three optical conditions. Each data point represents the visual performance for one subject for one correction condition under monocular (x-axis) and binocular (y-axis) viewing. The dashed line represents equality in visual performance between binocular and monocular viewing.
4. Discussion
We have implemented a binocular AO system for vision testing to investigate how the binocular visual performance is affected by higher order aberrations. The visual benefit upon SA and higher order aberration correction, hitherto estimated monocularly, was thus measured for the first time in binocular vision. In addition, corresponding monocular measurements were performed to investigate the binocular summation properties as retinal image quality is improved by correcting higher order aberrations. Complete binocular correction provided significant improvement in VA and CS over correction of SA and lower order aberrations. However, the increased binocular summation in the presence of optical aberrations might undermine the binocular visual benefit of aberration correction compared to the monocular case for higher spatial frequencies.
4.1. Improvement in visual performance with higher order aberration correction
On average across subjects, an improvement in VA by a factor of 1.05 ± 0.09 and CS by a factor of 1.11 ± 05 on average across spatial frequencies was obtained from binocular SA correction. Although no studies have investigated the visual benefit obtained after binocular SA correction, Piers et al. [37] have measured the benefit in monocular vision testing. Over a 4.8mm pupil, they measured an average improvement in VA by 10% and CS at 3, 6 and 15 c/deg by 32% for correction of 0.149µm SA while other higher order aberrations were left uncorrected. Lower visual benefit of SA correction in our study can be explained in part by the larger uncorrected chromatic and higher order aberration for a larger 6 mm pupil. Visual performance with complete binocular correction was improved significantly. The benefit was reflected to a greater extent in CS compared to VA. This is due to the steep falloff of the CS function at higher spatial frequencies which are relevant to the VA task [2]. Accordingly, the improvement in retinal image contrast does not provide an equivalent improvement in the spatial bandwidth, leading to the smaller benefit in VA. The binocular visual benefit of complete correction increased with spatial frequency, similar to the monocular case. The binocular visual benefit at 16 and 24 c/deg was 1.8 and 2.0 upon complete correction. Yoon and Williams [2] measured a similar visual benefit of a factor of 2 at the same spatial frequencies under monocular condition. In the present study, the measured binocular visual benefit was smaller than the monocular benefit of 2.3 and 2.6 in the right and left eyes respectively at 16 and 24 c/deg. Therefore, at high spatial frequencies, the improvement in visual performance upon complete correction of higher order aberrations is diminished in binocular viewing compared to monocular viewing.
4.2. Impact of higher order aberration correction on binocular summation
Binocular summation for VA and CS with baseline correction obtained in our study was consistent with previous studies [11,12]. The binocular summation factor has been calculated in this study using the ratio of binocular to the better of monocular visual performance. It has been suggested that using the better of the monocular performances is a more robust method of computing binocular summation to account for asymmetries in performance between the two eyes [38]. Alternatively, in the presence of asymmetries in CS between eyes, Baker et al. [39] have suggested the adjustment of the contrast in the less sensitive eye to equate monocular detectability in order to get unbiased estimates of binocular summation. In our study, when comparing the monocular optical quality between the left and right eye for the three conditions in terms of the RMS error, no significant difference was observed on average. Similarly, no statistically significant difference was observed in the VA and CS of the left and right eye of subjects.
Binocular summation in threshold contrast detection has been known to be around √2 or 40%, first introduced by Campbell and Green [11]. They observed that binocular and monocular contrast sensitivities had high spatial frequency cutoffs of 61 and 57 c/deg respectively, offset in the frequency domain by 4 c/deg. Cagenello et al. suggested that the improvement in binocular VA can be explained by a threshold contrast summation of the high spatial frequencies, which effectively increases the high spatial frequency cutoff of the CS function by 4 c/deg. This corresponds to around 11% improvement in high contrast VA [12]. In addition, it has been shown that the amount of binocular summation increases with decreasing contrast [40–42], increasing eccentricity [43] and increasing spherical defocus blur [26]. For instance, when letter contrast is decreased, percentage improvements in VA as high as 40% have been observed [42]. This can be explained by noticing that reducing contrast will degrade acuity such that the monocular and binocular high spatial frequency cutoffs shift towards lower spatial frequencies. At these poorer acuities, an improvement of 4 c/deg represents a larger percentage improvement than at better acuities. More recently, Plainis et al. [26] have demonstrated increased binocular summation in high contrast VA and visual evoked potentials in the presence of reduced retinal image contrast caused by defocus-induced blur. They observed that binocular summation increased with induction of defocus, while the corrected in-focus retinal image demonstrated the least summation. Ocular higher order aberrations also degrade image contrast. As observed previously, this might lead to a similar increase in summation when compared to an image whose contrast is improved by correcting higher order aberrations. In the present study, the two subjects with the largest magnitude of native higher order aberrations, hence the most significant degradation in retinal image contrast, demonstrated a reduction in binocular summation by 50% upon complete correction for VA. Similarly, 4 out of the 5 subjects demonstrated increased binocular summation for CS with baseline correction compared to that with complete correction. The results observed here of increasing summation with decreasing contrast are consistent with the concept of response saturation after binocular combination when high stimulus energies and low noise are present. Absence of binocular summation in high contrast vernier acuity and reduction of summation with increasing stimulus energy for an orientation discrimination task were explained similarly using response saturation [40,41]. Therefore, the absolute optical quality in the two eyes also might play an important role in governing binocular summation. This might especially be important in eyes whose optical quality is severely degraded due to corneal abnormalities. In addition to the absolute optical quality, the interocular difference in aberrations between the two eyes will also determine the benefit accruable upon binocular AO correction. In the present study, the relatively low interocular difference in optical quality in the normal subjects with baseline correction did not affect binocular summation. However, in clinical cases of laser refractive surgery, large interocular asymmetries are observed post-op leading to reduced binocular summation and stereopsis [23,25]. In such cases, binocular higher order aberration correction to improve the optical quality and reduce the interocular difference in aberrations will substantially improve binocular visual performance. Another important factor is the inherent fixation disparity of the subjects, which when corrected accurately can also improve binocular performance [44].
4.3. Implications for customized binocular vision correction
A significant benefit upon binocular optical correction is expected from wavefront-guided treatments for higher order aberrations such as with customized contact lenses, refractive and cataract surgery. The dependence of binocular summation on optical quality has important implications for estimates of improvement one might obtain from such customized vision correction strategies. The high spatial frequencies, where the optical quality is most compromised, elicit the most advantage from an optical correction. However, the decrease in binocular summation with an improvement in optical quality diminishes this advantage when comparing binocular vision to monocular vision. Therefore, including binocular summation into the monocular estimates of visual performance improvement would lead to a more comprehensive representation of binocular vision after wavefront-guided treatments. Further complex interactions between the binocular visual system and the ocular optics can be investigated using the binocular AO platform for testing visual performance. Of particular interests are the questions in physiological optics where binocular vision cannot be simply approximated as a sequential extension of monocular vision, but a simultaneous convergence of two monocular channels. In this respect, investigating stereopsis in the presence of manipulated ocular optics such as multifocal ophthalmic aids and monovision to alleviate presbyopia can be considered as important examples where the simultaneous convergence of two monocular inputs is imperative for probing normal binocular visual function. Thus, in addition to offering a powerful avenue for furthering clinical insight into the field of customized vision correction, binocular AO vision testing presented here also has significant potential for providing a comprehensive understanding of habitual binocular vision.
In summary, binocular higher order aberration correction, in particular complete correction provided significant improvement in binocular visual performance. In addition, binocular summation for higher spatial frequencies was the largest in the presence of subject’s native higher order aberrations and was reduced when these aberrations were corrected. This can be considered as a compensatory effect exhibited by the binocular visual system to reduce the impact of optical blur and thus might undermine the binocular visual benefit compared to that measured monocularly.
Acknowledgments
This research has been supported by NIH/NEI grant RO1EY 014999, Research to Prevent Blindness (RPB) and NIH training grant T32EY007125.
References and links
- 1.Liang J., Williams D. R., Miller D. T., “Supernormal vision and high-resolution retinal imaging through adaptive optics,” J. Opt. Soc. Am. A 14(11), 2884–2892 (1997). 10.1364/JOSAA.14.002884 [DOI] [PubMed] [Google Scholar]
- 2.Yoon G. Y., Williams D. R., “Visual performance after correcting the monochromatic and chromatic aberrations of the eye,” J. Opt. Soc. Am. A 19(2), 266–275 (2002). 10.1364/JOSAA.19.000266 [DOI] [PubMed] [Google Scholar]
- 3.Rossi E. A., Weiser P., Tarrant J., Roorda A., “Visual performance in emmetropia and low myopia after correction of high-order aberrations,” J. Vis. 7(8), 14 (2007). 10.1167/7.8.14 [DOI] [PubMed] [Google Scholar]
- 4.Sawides L., Gambra E., Pascual D., Dorronsoro C., Marcos S., “Visual performance with real-life tasks under adaptive-optics ocular aberration correction,” J. Vis. 10(5), 19 (2010). 10.1167/10.5.19 [DOI] [PubMed] [Google Scholar]
- 5.de Gracia P., Marcos S., Mathur A., Atchison D. A., “Contrast sensitivity benefit of adaptive optics correction of ocular aberrations,” J. Vis. 11(12), 5 (2011). 10.1167/11.12.5 [DOI] [PubMed] [Google Scholar]
- 6.Navarro R., Moreno-Barriuso E., Bará S., Mancebo T., “Phase plates for wave-aberration compensation in the human eye,” Opt. Lett. 25(4), 236–238 (2000). 10.1364/OL.25.000236 [DOI] [PubMed] [Google Scholar]
- 7.Burns S. A., Marcos S., Elsner A. E., Bara S., “Contrast improvement of confocal retinal imaging by use of phase-correcting plates,” Opt. Lett. 27(6), 400–402 (2002). 10.1364/OL.27.000400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dietze H. H., Cox M. J., “Correcting ocular spherical aberration with soft contact lenses,” J. Opt. Soc. Am. A 21(4), 473–485 (2004). 10.1364/JOSAA.21.000473 [DOI] [PubMed] [Google Scholar]
- 9.Sabesan R., Jeong T. M., Carvalho L., Cox I. G., Williams D. R., Yoon G., “Vision improvement by correcting higher-order aberrations with customized soft contact lenses in keratoconic eyes,” Opt. Lett. 32(8), 1000–1002 (2007). 10.1364/OL.32.001000 [DOI] [PubMed] [Google Scholar]
- 10.MacRae S. M., Schwiegerling J., Snyder R., “Customized corneal ablation and super vision,” J. Refract. Surg. 16, S230–S235 (2000). [DOI] [PubMed] [Google Scholar]
- 11.Campbell F. W., Green D. G., “Monocular versus binocular visual acuity,” Nature 208(5006), 191–192 (1965). 10.1038/208191a0 [DOI] [PubMed] [Google Scholar]
- 12.Cagenello R., Arditi A., Halpern D. L., “Binocular enhancement of visual acuity,” J. Opt. Soc. Am. A 10(8), 1841–1848 (1993). 10.1364/JOSAA.10.001841 [DOI] [PubMed] [Google Scholar]
- 13.Blake R., Fox R., “The psychophysical inquiry into binocular summation,” Percept. Psychophys. 14(1), 161–185 (1973). 10.3758/BF03198631 [DOI] [Google Scholar]
- 14.Lindblom B., Westheimer G., “Binocular summation of hyperacuity tasks,” J. Opt. Soc. Am. A 6(4), 585–589 (1989). 10.1364/JOSAA.6.000585 [DOI] [PubMed] [Google Scholar]
- 15.Heravian J. S., Jenkins T. C., Douthwaite W. A., “Binocular summation in visually evoked responses and visual acuity,” Ophthalmic Physiol. Opt. 10(3), 257–261 (1990). 10.1111/j.1475-1313.1990.tb00861.x [DOI] [PubMed] [Google Scholar]
- 16.Legge G. E., “Binocular contrast summation—I. Detection and discrimination,” Vision Res. 24(4), 373–383 (1984). 10.1016/0042-6989(84)90063-4 [DOI] [PubMed] [Google Scholar]
- 17.Legge G. E., “Binocular contrast summation—II. Quadratic summation,” Vision Res. 24(4), 385–394 (1984). 10.1016/0042-6989(84)90064-6 [DOI] [PubMed] [Google Scholar]
- 18.Legras R., Hornain V., Monot A., Chateau N., “Effect of induced anisometropia on binocular through-focus contrast sensitivity,” Optom. Vis. Sci. 78(7), 503–509 (2001). 10.1097/00006324-200107000-00013 [DOI] [PubMed] [Google Scholar]
- 19.Anera R. G., Jiménez J. R., Villa C., Rodríguez-Marín F., Gutiérrez R., “Technical note: Pre-surgical anisometropia influences post-LASIK binocular mesopic contrast sensitivity function,” Ophthalmic Physiol. Opt. 27(2), 210–212 (2007). 10.1111/j.1475-1313.2006.00458.x [DOI] [PubMed] [Google Scholar]
- 20.Pardhan S., Gilchristt J., “The effect of monocular defocus on binocular contrast sensitivity,” Ophthalmic Physiol. Opt. 10(1), 33–36 (1990). 10.1111/j.1475-1313.1990.tb01103.x [DOI] [PubMed] [Google Scholar]
- 21.Jiménez J. R., Castro J. J., Jiménez R., Hita E., “Interocular differences in higher-order aberrations on binocular visual performance,” Optom. Vis. Sci. 85(3), 174–179 (2008). 10.1097/OPX.0b013e31816445a7 [DOI] [PubMed] [Google Scholar]
- 22.Cuesta J. R. J., Anera R. G., Jiménez R., Salas C., “Impact of interocular differences in corneal asphericity on binocular summation,” Am. J. Ophthalmol. 135(3), 279–284 (2003). 10.1016/S0002-9394(02)01968-2 [DOI] [PubMed] [Google Scholar]
- 23.Jiménez J. R., Villa C., Anera R. G., Gutiérrez R., del Barco L. J., “Binocular visual performance after LASIK,” J. Refract. Surg. 22(7), 679–688 (2006). [DOI] [PubMed] [Google Scholar]
- 24.Schor C., Heckmann T., “Interocular differences in contrast and spatial frequency: effects on stereopsis and fusion,” Vision Res. 29(7), 837–847 (1989). 10.1016/0042-6989(89)90095-3 [DOI] [PubMed] [Google Scholar]
- 25.Jiménez J. R., Castro J. J., Hita E., Anera R. G., “Upper disparity limit after LASIK,” J. Opt. Soc. Am. A 25(6), 1227–1231 (2008). 10.1364/JOSAA.25.001227 [DOI] [PubMed] [Google Scholar]
- 26.Plainis S., Petratou D., Giannakopoulou T., Atchison D. A., Tsilimbaris M. K., “Binocular summation improves performance to defocus-induced blur,” Invest. Ophthalmol. Vis. Sci. 52(5), 2784–2789 (2011). 10.1167/iovs.10-6545 [DOI] [PubMed] [Google Scholar]
- 27.Vlaskamp B. N., Yoon G., Banks M. S., “Human stereopsis is not limited by the optics of the well-focused eye,” J. Neurosci. 31(27), 9814–9818 (2011). 10.1523/JNEUROSCI.0980-11.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hampson K., Chin S., Mallen E., “Binocular Shack–Hartmann sensor for the human eye,” J. Mod. Opt. 55(4-5), 703–716 (2008). 10.1080/09500340701469674 [DOI] [Google Scholar]
- 29.Kobayashi M., Nakazawa N., Yamaguchi T., Otaki T., Hirohara Y., Mihashi T., “Binocular open-view Shack-Hartmann wavefront sensor with consecutive measurements of near triad and spherical aberration,” Appl. Opt. 47(25), 4619–4626 (2008). 10.1364/AO.47.004619 [DOI] [PubMed] [Google Scholar]
- 30.Hampson K. M., Chin S. S., Mallen E. A., “Dual wavefront sensing channel monocular adaptive optics system for accommodation studies,” Opt. Express 17(20), 18229–18240 (2009). 10.1364/OE.17.018229 [DOI] [PubMed] [Google Scholar]
- 31.Fernández E. J., Prieto P. M., Artal P., “Binocular adaptive optics visual simulator,” Opt. Lett. 34(17), 2628–2630 (2009). 10.1364/OL.34.002628 [DOI] [PubMed] [Google Scholar]
- 32.Sabesan R., Ahmad K., Yoon G., “Correcting highly aberrated eyes using large-stroke adaptive optics,” J. Refract. Surg. 23(9), 947–952 (2007). [DOI] [PubMed] [Google Scholar]
- 33.Sabesan R., Yoon G., “Visual performance after correcting higher order aberrations in keratoconic eyes,” J. Vis. 9(5), 6–, 1–10. (2009). 10.1167/9.5.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.G. Smith and D. Atchison, The Eye and Visual Optical Instruments (Cambridge University Press, 1997). [Google Scholar]
- 35.Watson A. B., Pelli D. G., “QUEST: a Bayesian adaptive psychometric method,” Percept. Psychophys. 33(2), 113–120 (1983). 10.3758/BF03202828 [DOI] [PubMed] [Google Scholar]
- 36.Li X., Lu Z. L., Xu P., Jin J., Zhou Y., “Generating high gray-level resolution monochrome displays with conventional computer graphics cards and color monitors,” J. Neurosci. Methods 130(1), 9–18 (2003). 10.1016/S0165-0270(03)00174-2 [DOI] [PubMed] [Google Scholar]
- 37.Piers P. A., Fernandez E. J., Manzanera S., Norrby S., Artal P., “Adaptive optics simulation of intraocular lenses with modified spherical aberration,” Invest. Ophthalmol. Vis. Sci. 45(12), 4601–4610 (2004). 10.1167/iovs.04-0234 [DOI] [PubMed] [Google Scholar]
- 38.Pardhan S., “A comparison of binocular summation in young and older patients,” Curr. Eye Res. 15(3), 315–319 (1996). 10.3109/02713689609007626 [DOI] [PubMed] [Google Scholar]
- 39.Baker D. H., Meese T. S., Mansouri B., Hess R. F., “Binocular summation of contrast remains intact in strabismic amblyopia,” Invest. Ophthalmol. Vis. Sci. 48(11), 5332–5338 (2007). 10.1167/iovs.07-0194 [DOI] [PubMed] [Google Scholar]
- 40.Bearse M. A., Jr, Freeman R. D., “Binocular summation in orientation discrimination depends on stimulus contrast and duration,” Vision Res. 34(1), 19–29 (1994). 10.1016/0042-6989(94)90253-4 [DOI] [PubMed] [Google Scholar]
- 41.Banton T., Levi D. M., “Binocular summation in vernier acuity,” J. Opt. Soc. Am. A 8(4), 673–680 (1991). 10.1364/JOSAA.8.000673 [DOI] [PubMed] [Google Scholar]
- 42.Home R., “Binocular summation: a study of contrast sensitivity, visual acuity and recognition,” Vision Res. 18(5), 579–585 (1978). 10.1016/0042-6989(78)90206-7 [DOI] [PubMed] [Google Scholar]
- 43.Pardhan S., “Binocular recognition summation in the peripheral visual field: contrast and orientation dependence,” Vision Res. 43(11), 1251–1255 (2003). 10.1016/S0042-6989(03)00093-2 [DOI] [PubMed] [Google Scholar]
- 44.Jiménez J. R., Olivares J. L., Pérez-Ocón F., del Barco L. J., “Associated phoria in relation to stereopsis with random-dot stereograms,” Optom. Vis. Sci. 77(1), 47–50 (2000). 10.1097/00006324-200001000-00013 [DOI] [PubMed] [Google Scholar]