Abstract
Purpose
To examine the prevalence of difficult psychiatrist-patient interactions of 20 psychiatrists in the South Texas Psychiatric PBRN, determine what characteristics were associated with “difficult” patients, and compare findings with previous studies in primary care.
Methods
During a 2-month observational study, psychiatrists collected patient information on setting, demographics, diagnoses, medications and rated the patients using a Difficult Doctor Patient Relationship Questionnaire (DDPRQ-10) which had previously been used and validated in the primary care setting.
Results
A total of 905 valid data cards were collected. Difficult patients were identified in 15% of the sample. Diagnoses of schizophrenia, alcohol/substance abuse, and personality disorder were associated with difficulty. Psychiatrists least burdened by difficult patients were older, in solo practice, and worked 51-55 hours per week.
Conclusions
This cross-sectional study demonstrates that psychiatrists encounter difficult patients at a similar rate (15%) as do primary care physicians. Mentoring programs and structured treatment interventions for the most difficult patient groups may assist all physicians who treat psychiatric patients whether in specialty, family medicine, or other primary care settings.
Introduction
Clinically difficult patients have been studied in the primary care literature, but there is relatively little literature on difficult psychiatric patients and none on the characteristics of the physicians who treat these patients. In a medicine subspecialty and surgical outpatient study, O’Dowd wrote of difficult patients, “They evoke an overwhelming mixture of exasperation, defeat, and sometimes plain dislike that causes the heart to sink when they consult”(1). Despite the ubiquitous nature of these patients, there is relatively little literature on difficult psychiatric patients and none on the characteristics of the psychiatrists who treat these patients (2-6).
In a medicine subspecialty and surgical outpatient study, physicians identified unexplained symptoms, psycho-social problems, and untreatable illness as the primary reasons for difficulty (7). Interestingly, doctors rated patients as difficult if they could not meet their own personal expectations or the individual patient’s expectations (7). The leading patient characteristics included: psychological problems, psychosocial issues, multiple physical problems, communication problems, and unrealistic expectations. The primary care physicians were characterized as working long hours, and lacking training in counseling and communication skills.
A systematic review of the psychiatric literature between 1979-2004 found 94 articles mentioning difficult patients but few containing empirical data (4). They concluded there were 3 characteristics of difficult patients, “Unwilling care-avoiders, ambivalent care-seekers and demanding care-claimers” (4). Examples of a professional’s negative feelings toward difficult patients were anger, guilt, helplessness, powerlessness, dislike and disappointment.
Hahn developed a quantitative measure, the Difficult Doctor-Patient Relationship Questionnaire (DDPRQ-10), to examine the prevalence of “difficult” patients in the primary care setting and the association of difficulty with physical and mental disorder, functional impairment, health care utilization and satisfaction with medical care (5). He found that physicians rated 15% of 627 patients as difficult. Difficult patients were more likely to have a psychiatric disorder, vague somatic complaints, higher medical utilization and dissatisfaction with their care. This study followed an earlier one conducted by Hahn which developed the questionnaire and found a prevalence of “difficult patients” at 10-20% (6). In the earlier study, difficult patients were characterized by higher rates of somatization, personality disorder and Axis I pathology.
The relevant literature is very limited in psychiatric settings, and in available primary care studies findings consistently point to psychiatric and psychological variables contributing to physicians rating their patients as difficult. Since primary care settings typically include services for psychiatric disorders, and since specific data for psychiatric populations and associated difficulty is lacking, this area represents a gap in the existing knowledge applicable in psychiatry and primary care.
The purpose of this study was to identify the prevalence of difficulty in a psychiatric setting, to examine physician and patient variables associated with patient difficulty, to compare these findings with those in prior studies of different populations (mostly primary care) and to consider how these findings might inform all physicians who treat mental health disorders whether in psychiatry or primary care settings.
Methods
Study Design, Setting and Subjects
This study was an observational cross-sectional study conducted by 20 psychiatrist members of the South Texas Psychiatry Practice Based Research Network in Spring of 2010. The settings included eight solo practices, five small group practices and seven large group practices. All members of the research network were invited to participate in the study and none who volunteered were excluded.
Data Collection
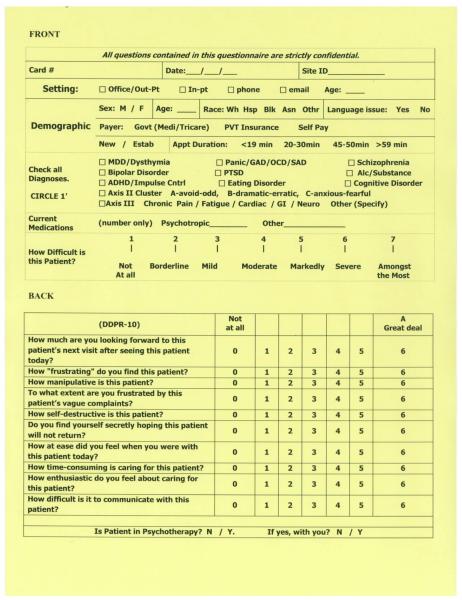
We asked psychiatrists to complete a data card (Refer to Figure 1) on 50 consecutive patients during a two month period. Patients could be inpatient, outpatient, new or established. Cards were completed for all patient encounters via face-to-face meetings or phone calls. Physicians completed data on the patient setting, demographics, diagnoses, patient medications, presence of a language issue, payment method, and appointment duration. Patients were then rated using the DDPRQ-10 which had been previously used in the primary care setting (5,6). The DDPRQ-10 was selected for its brevity, established reliability, and validity in the primary care setting. It is a 10-item Likert scale with items scored from 1(not at all) to 6 (a great deal); total scores range from 10-60. The cut point used to determine patient difficulty category (Difficult/Not Difficult) for the 10-item instrument was based upon the 30-item DDPRQ cut point which demonstrated high construct validity and has been described previously (6). Patients receiving a score of 30 or greater were categorized as difficult (5). Internal reliability of the DDPRQ-10 instrument for the current study showed acceptable consistency (Cronbach alpha= 0.88). Physicians also rated each patient using a single 7-point Likert item “How difficult is this patient?” which included responses that ranged from “Not at All” to “Amongst the Most”. Additionally, physicians provided personal data regarding age, gender, years in practice, practice setting, years in current setting, and workload hours per week. “Burdened Psychiatrists” were defined as psychiatrists who saw a greater percentage of difficult patients.
Figure 1.
Data Collection Instrument Completed by Practice-based Research Network (PBRN) Members.
Analyses
Simple descriptive statistics were used to characterize the distribution of study values including frequencies, percentages, means and standard deviations or medians and inter-quartile ranges for each variable. Associations between categorical variables were examined by Pearson’s χ2 test or Fishers Exact test as appropriate. The Kruskal-Wallis Test was used to assess associations between categorical variables and continuously distributed variables. Spearman rank correlation with 95% confidence interval was used to assess association between difficulty assessment scores. All statistical tests were performed at the two-sided 0.05 level of statistical significance and all statistical analyses were conducted using SAS Version 9.2 (SAS Institute, Cary, NC).
Results
Over a two-month period, data for 935 patients was collected by 20 psychiatrists. Most psychiatrists turned in 48 to 50 data cards, although one physician returned 31 cards and another returned 7. We had 9 psychiatrists score 28 patients (3.0%) by telephone. The DDPRQ-10 scores ranged from 10 to 57 (Mean (SD) = 21.1 (9.2); Median [Q1,Q3] = 19 [15, 25]). Of the 935 physician-patient interactions, 905 responses were complete and available for analysis, and 133 were scored greater than 30 on the DDPRQ-10 and categorized as “difficult.” Of the 20 psychiatrists, 2 did not identify any difficult patients, while 6 identified 83 (62%) of the 133 difficult patients. One physician did not complete the DDPRQ-10 scale for his/her patients, and the remaining 11 psychiatrists identified between 1and 9 difficult patients each.
Table 1 lists the 10 items in the DDPRQ-10 along with the percentage of patients rated difficult by each individual item.
Table 1.
The Difficult Doctor-Patient Relationship Questionnaire Ten-Item Version (DDPRQ-10)
| % of Patients Rated Difficult by Itemb |
||
|---|---|---|
| Itema | Difficult (n=133) |
Not Difficult (n=772) |
| 1. How much are you looking forward to this patients next visit after today?c | 92 | 38 |
| 2. How frustrating do you find this patient? | 80 | 9 |
| 3. How manipulative is this patient? | 46 | 3 |
| 4. To what extent are you frustrated by this patients vague complaints? | 55 | 4 |
| 5. How self-destructive is this patient? | 39 | 6 |
| 6. Do you find yourself secretly hoping this patient will not return? | 54 | 2 |
| 7. How at ease did you feel with this patient today?c | 64 | 18 |
| 8. How time-consuming is caring for this patient? | 61 | 10 |
| 9. How enthusiastic do you feel about caring for this patient?c | 90 | 34 |
| 10. How difficult is it to communicate with this patient? | 53 | 6 |
Based on a DDPR-10 score > 30, out of 905 patients, 133 were Difficult and 772 were Not Difficult
Each item was scored on a six-point scale: 1=Not at all, 6=A great deal
Responses were dichotomized by coding raw scores of 4 through 6 on each item as Difficult
Item was reversed for scoring (1=A great deal, 6=Not at all)
Table 2 presents the demographic characteristics of the patients by difficulty category. Patients with language issues, new patients, inpatients and those with government payment source (Medicare, Medicaid, and TriCare) were significantly associated with difficulty category. The length of the appointment, patient age category, sex, and race were not associated with difficulty.
Table 2.
Demographic characteristics by difficulty category for 905 patients with DDPRQ-10 scores
| Characteristic | Difficulta n (%) |
Not Difficu lt n (%) |
|
|---|---|---|---|
| Total Number | 133 (14.7) | 772 (85.3) | |
| Age category | |||
| 43 or younger | 68 (15.5) | 372 (84.5) | |
| Older than 43 | 64 (14.1) | 390 (85.9) | |
| Sex | |||
| Male | 71 (14.1) | 431 (85.9) | |
| Female | 62 (15.6) | 335 (84.4) | |
| Race | |||
| White | 65 (13.1) | 430 (86.9) | |
| Hispanic | 43 (15) | 244 (85) | |
| Black | 15 (24.6) | 46 (75.4) | |
| Asian/Other | 3 (25) | 9 (75) | |
| Language Issuec | |||
| Yes | 8 (33.3) | 16 (66.7) | |
| No | 92 (12.4) | 650 (87.6) | |
| Statusb | |||
| New | 24 (22.6) | 82 (77.4) | |
| Established | 95 (14.5) | 561 (85.5) | |
| Settingc | |||
| Office/Out-Pt | 100 (13.5) | 643 (86.5) | |
| In-Pt | 25 (25.3) | 74 (74.7) | |
| Phone | 3 (10.7) | 25 (89.3) | |
| Paymentb | |||
| Govt(Medi/Tricare) | 81 (16.9) | 398 (83.1) | |
| PVT Insurance | 11 (10.2) | 97 (89.8) | |
| Self Pay | 28 (10) | 252 (90) | |
| Appointment Duration | |||
| <19 min | 30 (15.9) | 159 (84.1) | |
| 20-30 min | 39 (12.3) | 277 (87.7) | |
| 45-50 min | 22 (10.6) | 186 (89.4) | |
| >51 min | 15 (15.6) | 81 (84.4) |
Difficult category contains patients with DDPRQ-10 score >30
p < 0.05
p < 0.01
Table 3 describes patient diagnoses and medication use by difficulty category. Diagnoses of schizophrenia, personality disorder, cognitive disorder, alcohol / substance abuse, depression, any Axis III symptom, any anxiety disorder, and PTSD were significantly associated with patient difficulty category. Patients diagnosed with schizophrenia, personality disorder, cognitive disorder, and alcohol or substance abuse were significantly more likely to receive scores greater than 30 and be placed in the “difficult” category. Patients diagnosed with depression, any Axis III symptom, any anxiety disorder, and PTSD were significantly more likely to be assigned scores less than or equal to 30 and be placed in the “not difficult” category. Diagnoses of ADHD, eating disorder and bipolar disorder were not associated with difficulty category. Patients participating in any psychotherapy, and those receiving psychotherapy from the psychiatrist, were significantly less likely to be given a “difficult” score (> 30).
Table 3.
Diagnoses and medication by difficulty category for 905 patients with DDPRQ-10 scores
| Difficulta | Not Difficult |
|
|---|---|---|
| Schizophrenia, n (%)d | 25 (18.8) | 54 (7) |
| Personality Disorder, n (%)d | 48 (36.1) | 103 (13.3) |
| Cognitive Disorder, n (%)c | 25 (18.8) | 78 (10.1) |
| Alcohol/Substance Abuse, n (%)b | 24 (18) | 80 (10.4) |
| ADHD, n (%) | 27 (20.3) | 192 (24.9) |
| Eating Disorder, n (%) | 3 (2.3) | 5 (0.6) |
| Bipolar, n (%) | 34 (25.6) | 146 (18.9) |
| Depression, n (%)c | 39 (29.3) | 329 (42.6) |
| Axis III symptoms, n (%)c | 28 (21.1) | 261 (33.8) |
| Anxiety, n (%)b | 19 (14.3) | 188 (24.4) |
| PTSD, n (%)b | 6 (4.5) | 84 (10.9) |
| Psychotherapy, n (%)c | 54 (47.4) | 436 (61.8) |
| Psychotherapy with MD, n (%)d | 20 (20.4) | 254 (38.5) |
| # of Psychological Medications, Median [Q1,Q3]b | 3 [1,3] | 2 [1,3] |
| # of Other Medications, Median [Q1,Q3]c | 0 [0,3] | 1 [0,5] |
Q1= first quartile; Q3 = third quartile
Difficult category contains patients with DDPRQ-10 score >30; Not Difficult category contains patients with DDPRQ-10 score ≤30.
p<0.05
p<0.01
p < 0.001
When doctor-patient interactions were assessed using a single global 7-point Likert item “How difficult is this patient?” 31.9% were reported to be “Not at all” difficult, 11.2% borderline, 18.1% mild, 19.3% moderate, 9.7% markedly, 5.6% severe, and 4.1% were “Amongst the Most” difficult. Spearman rank correlation between score values of DDPRQ-10 (range 10 to 60) and the single difficulty item (range 1 to 7) was 0.67 (95% CI= 0.64, 0.71).
We also examined individual physician characteristics (not shown in any table) and found that younger psychiatrists (31 to 40 years of age) had an increased burden (24.5%) (greater percentage of difficult patients) compared with all other age groups (13.3% , 41-50 years; 13.2%, 51-60 years; 11.9%, >60 years), p=0.003. Practicing in a group of 5 or more physicians (20%) increased physician burden compared with a group of 2 to 5 physicians (15.2%) or solo physicians (10.5%), p=0.002. Working an average of 51 to 55 hours per week lowered physician burden (5%) compared with other workloads (17.8%, <40 hours; 16.1%, 40-45 hours; 17.3%, 46-50 hours; 13.8%, >55 hours), p=0.04. Physician years in practice, years in current setting, and gender were not associated with physician burden.
Discussion
This observational cross-sectional study shows a 15% prevalence of difficulty in a psychiatric patient population, a rate that is similar to the rates of difficulty found in previous primary care populations by Hahn and others. We acknowledge that psychiatrists were the study population and this population differs from family physicians and internal medicine clinicians. While previous studies pointed to an increased rate of difficulty with psychiatric and psychological problems, this study is unique in its emphasis on patients considered difficult within the psychiatric population (5).
We found that psychiatrists were more likely to rate a patient as difficult if they had a diagnosis of schizophrenia, alcohol/substance abuse, or personality disorder, which are all diagnoses that are correlated with high rates of disability and prolonged course. Perhaps surprisingly, we found that patients with the most medical co-morbidity (more Axis III diagnoses) were less often rated as difficult. In previous studies of primary care patients, vague somatic complaints were associated with greater percentages of difficulty, however specific medical co-morbidities were not (6). It is possible that higher rates of disability and prolonged course explain why both vague somatic complaints in primary care and chronic/relapsing mental illness in psychiatric care increase difficulty rates.
We found that the youngest psychiatrists were most likely to rate more patients as “difficult,” a finding that was similar to a previous British primary care study (8). It is helpful for primary care clinicians to recognize when to refer these “difficult” patients for psychiatric treatment. Family medicine residency training could address recognition of negative counter-transference or negative feelings, the importance of referrals when these interactions occur, and the assurance that every clinician encounters these “heart sink” patients whether treated in early or mid-career (1).
In the current climate of US medical care reform, rates of patients “difficulty” may be affected. We have seen a push by payers for briefer, less frequent office visits to reduce costs. However, our data showed that patients who received psychotherapy from their psychiatrist were less likely to be rated as “difficult.” Psychotherapy takes time, however reimbursement pressures provide incentives for psychiatrists to perform less psychotherapy. Moving toward briefer and less frequent visits may therefore undermine the physician patient relationship.
Labeling a patient as “difficult” may be construed as pejorative because it suggests that the patient is to blame for the physician’s frustration. The authors do not believe that patients themselves are difficult, but interactions can be. Internal and external factors both contribute to negative (and positive) feelings in working with certain patients. “Difficulty” is a clinical sign to be recognized and addressed in order to provide appropriate psychiatric care (9). Recently, Eckert (10) stated, “Resistance to treatment does not reflect upon the patient, but only on our improving our repertoire of treatment.” This cross-sectional study is not concluding that factors associated with difficulty are the cause of the problem, rather they are markers to alert the physician of potential issues which may affect his/her desire to provide the best clinical care.
The proportion of “difficult” patients may increase due to Health Care Reform. Briefer and “more productive visits” will be emphasized to reduce costs. However, time is a variable in difficult encounters. Our data showed that although duration of patient visit was not significantly correlated with difficulty, patients receiving psychotherapy from their psychiatrist were rated as less difficult. Changes which may cause appointment durations to decrease in an effort for clinicians to see more patients may ultimately result in an increase of difficult encounters. If we are not careful, the physician-patient relationship may be undermined in this process.
Limitations
Some limitations exist in interpreting the findings from this study. The research design was cross-sectional and relied on the psychiatrists to complete the cards unprompted which resulted in some missing data. Additionally, the method used to collect the data, the “card system,” was not tested for reliability and validity across study sites. Nor was there any assessment of the original medical records to verify the results recorded by the psychiatrists. In addition, our patient sample differed from a nationally representative sample of US office-based psychiatric practices (11-12) in multiple ways. Our sample had more males, fewer Whites, more Hispanics, more patients were ‘self-paid”, and a much larger number utilized “Government payment-Medicare/Medicaid/Tri-Care”. Finally, the psychiatrist-participant pairs were not a randomly selected sample, each volunteered to participate knowing the research question ahead of time. This could have caused the identified prevalence to not accurately represent the true prevalence for all psychiatrist-patient relationships.
Another limitation of our study involves the potential for misclassification. We had no gold standard by which to definitively classify patients as truly difficult versus not. For a pseudo-gold standard, we used a 7-point Likert scale to reflect the physician expert global assessment. In dichotomizing the DDPRQ-10, we used the cut point suggested by the Hahn et al in their 1996 paper. However, this cut point was selected based upon the distribution of difficulty scores involving the 30-item version of the DDPRQ, and tests of construct validity have strongly supported it (6). Nevertheless, as we did not directly assess a global, direct dichotomous measure of perceived patient difficulty (Yes/No), it is possible that some patients were misclassified.
Future research should address noted limitations of this study. The study method should be further tested for reliability and validity, and then repeated on a random national sampling of psychiatric patients both in specialty and primary care settings. If, as suggested by our study, patients in the hospital, with language barriers, Medicare/Medicaid/TriCare funding, and certain diagnoses are at increased risk of being experienced as difficult, perhaps strategies could be developed to better care for these populations. Greater knowledge about the nature of difficult patient interactions may aid in systematic approaches to decrease difficulty and improve the quality of patient care.
Conclusion
To date, this is the largest study to quantitatively examine the prevalence of difficult patients in psychiatric practice. The difficulty rate of 15% is similar to the rates of patient difficulty in non-psychiatric populations in previous studies. Patient difficulty rates were highest for the youngest psychiatrists indicating a potential for interventions with mentoring programs. High rates of difficulty in populations with poor outcomes indicates a need for structured treatment programs for severely ill patients. Based on these findings, psychiatrists and family physicians who give psychiatric care would do well to collaborate to improve treatments. The good news for burdened physicians is that things get better with experience.
Acknowledgements
The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 RR 025767-02S1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
None of the authors have a conflict of interest.
References
- 1.O’Dowd TC. Five years of heartsink patients in general practice. British Medical Journal. 1988;297:528–530. doi: 10.1136/bmj.297.6647.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neill JR. The Difficult Patient: Identification and Response. J Clinical Psychiatry. 1979 May;Vol 40(5):209–212. [PubMed] [Google Scholar]
- 3.Robbins JM, Beck PR, Mueller DP, et al. Therapists’ Perceptions of Difficult Psychiatric Patients. Journal of Mental and Nervous Disease. 1988;176:4980–497. doi: 10.1097/00005053-198808000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Koekkoek B, van Meijel V, Hutschemaekers G. Difficult Patients in Mental Health Care: A Review. Psychiatric Services. 2006;57:795–802. doi: 10.1176/ps.2006.57.6.795. [DOI] [PubMed] [Google Scholar]
- 5.Hahn SR, Kroenke K, Spitzer RL, et al. The Difficult Patient: Prevalence, Psychopathology, and Functional Impairment. J Gen Int Med. 1996;11:1–8. doi: 10.1007/BF02603477. [DOI] [PubMed] [Google Scholar]
- 6.Hahn SR, Thompson KS, Wills TA, et al. The Difficult Doctor-Patient Relationship: Somatization, Personality, and Psychopathology. J Clin Epidemiol. 1994;47:647–657. doi: 10.1016/0895-4356(94)90212-7. [DOI] [PubMed] [Google Scholar]
- 7.Sharpe M, Mayou R, Seagroatt V, et al. Why Do doctors find some patients difficult to help? Quarterly J of Medicine. 1994;87:187–193. [PubMed] [Google Scholar]
- 8.Krebs EE, Garrett JM, Konrad TR. The difficult doctor? Characteristics of physicians who report frustration with patients: an analysis of survey data. BMC Health Services Research. 2006;6:128. doi: 10.1186/1472-6963-6-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roberts LW, Dyer AR. Caring for Difficult Patients. Focus. 2003;Vol 1(No.4):453–458. [Google Scholar]
- 10.Eckert, Marianne Horney . Address to The American Academy of Psychoanalysis and Dynamic Psychiatry. Honolulu, HI: May 12, 2011. [Google Scholar]
- 11.Mojtabai R, Olfson M. National Trends in Psychotherapy by Office-Based Psychiatrists. Arch Gen Psychiatry. 2008;65(8):962–970. doi: 10.1001/archpsyc.65.8.962. [DOI] [PubMed] [Google Scholar]
- 12.Mojtabai R, Olfson M. National Trends in Psychotropic Medication Polypharmacy in Office-based Psychiatry. Arch Gen Psychiatry. 2010;67(1):26–36. doi: 10.1001/archgenpsychiatry.2009.175. [DOI] [PubMed] [Google Scholar]