INTRODUCTION
Fitz-Hugh-Curtis syndrome is an inflammatory disease of the liver capsule that occurs as a complication of pelvic inflammatory disease in approximately 25% of cases. The most common etiological agents are Chlamydia trachomatis and Neisseria gonorrhoeae. Classically, it manifests as acute right upper quadrant pain, which can sometimes be confused with pyelonephritis or a primitive condition of hepatobiliary origin or the digestive tract. A correct diagnosis is often difficult. Ultrasonography and computed tomography (CT) may be helpful in the differential diagnosis of other forms of peritonitis localized in the right abdominal quadrants, and serology, urine cultures and cervical swabs are generally used to isolate the responsible organism. The differential diagnosis could include Chilaiditi syndrome (interposition of a colonic segment between the liver and diaphragm with occlusion) or exudative peritonitis from salpingitis. We describe the clinical case of a 24-year-old Caucasian woman who presented with acute right upper quadrant pain, positive Murphy's sign, neutrophilic leukocytosis, and fever.
CASE DESCRIPTION
We report the clinical case of a 24-year-old Caucasian woman who was treated in November 2011. She presented with pain in the right upper quadrant associated with fever and neutrophilic leukocytosis. She was a light smoker, nulliparous, and sexually active. In the previous two years, she had taken estrogen-progestin oral therapy for hypertrichosis associated with a polycystic ovary. She reported recurrent episodes of vaginitis in the last year. The patient presented to our hospital due to pain in the right upper abdominal quadrant that had lasted for three days, fever, abdominal distention, and obstipation of feces and gases associated with an episode of vomiting. These symptoms appeared to coincide with her menstrual cycle. The patient was hemodynamically stable, and her abdomen appeared globular, distended, and barely palpable, particularly in the right upper quadrant, with torpid peristalsis. Murphy's and Blumberg's signs were positive, but Rovsing's and McBurney's signs were negative. Her blood test results were as follows: Hb 12.7 g/dL, WBC 16,020, neutrophils 87.6%, PLT 194,000, INR 1.05, ratio 1, urea 16 mg/dL, fibrinogen 858 mg/dL, creatinine 1.1 mg/dL, ALT 23 IU/L, AST 32 IU/L, amylase 20 IU/L, total bilirubin 1.35 mg/dL, direct bilirubin 0.91 mg/dL, sodium 136 mEq/L, potassium 3.48 mEq/dL, LDH 281 IU/L, CRP 30.27 mg/dL, ferritin 450 ng/ mL, and ESR 82 mm/h. A physical-chemical examination of her urine showed rare lower urinary tract epithelial cells, rare urothelial cells, rare erythrocytes, and 3-4 leukocytes per field. Chest X-ray showed the accentuation of broncho-vascular markings and mild obliteration of the sinuses bilaterally. An abdominal radiograph showed no free air or hydroaeric levels below the diaphragm. Despite the negative results of the blood tests, we suspected that the pain had a hepatobiliary cause. We therefore performed liver ultrasonography, which showed an enlarged liver, no dilation of the intra- or extra-hepatic bile ducts, and a gallbladder with thickened walls and a multilayered appearance, which was similar to the findings in inflammatory disorders. Gallstones were not observed in the lumen of the gallbladder, which had a layer of perihepatic and pericholecystic effusion (Figure 1). A focal area of unclear nature with a lack of homogeneity was observed in the middle layer of the left kidney (Figures 2 and 3). The patient was transferred to our department for further investigation. MRI confirmed the ultrasonographic results described previously and more clearly demonstrated that the alteration of the left kidney was pyelonephritis. The patient was examined by a gynecologist, who noted abundant leucorrhoea and vulvo-vaginal erythema and therefore performed trans-vaginal ultrasonography, which showed a normal uterus and endometrium and ovarian polycystosis. Vaginal and cervical swabs were collected to identify pathogenic microorganisms; these swabs were positive for Candida albicans and Ureaplasma urealyticum. Gene amplification by PCR was positive for Chlamydia trachomatis. Finally, we came to a conclusive diagnosis of pelvic inflammatory disease (PID) and perihepatitis resulting in cholecystitis caused by C. trachomatis, which constituted FHC syndrome. Previous antibiotic treatment with piperacillin and tazobactam was replaced by a single intravenous dose of 2 g of azithromycin, which led to a gradual decrease in pain and inflammation markers within approximately 72 hours. After three weeks, the patient was in good general condition, with no pain on palpation in the right hypochondriac region, negative swab results and normalization of the ultrasound and laboratory results.
Figure 1.
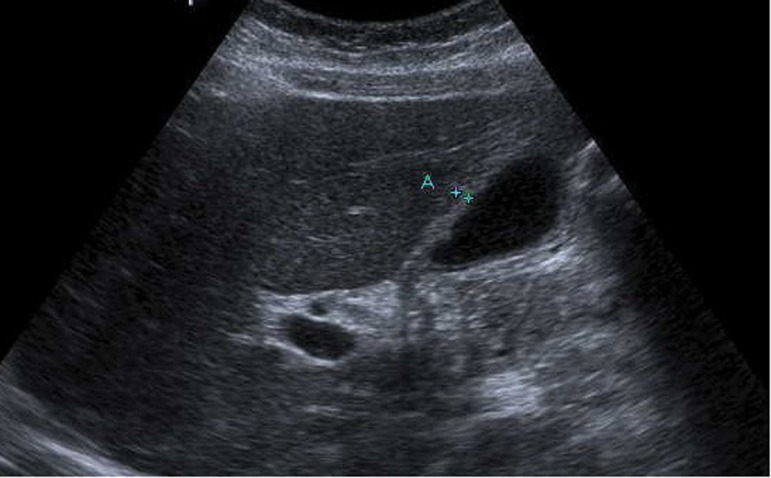
Perihepatic and pericholecystic effusion.
Figure 2.
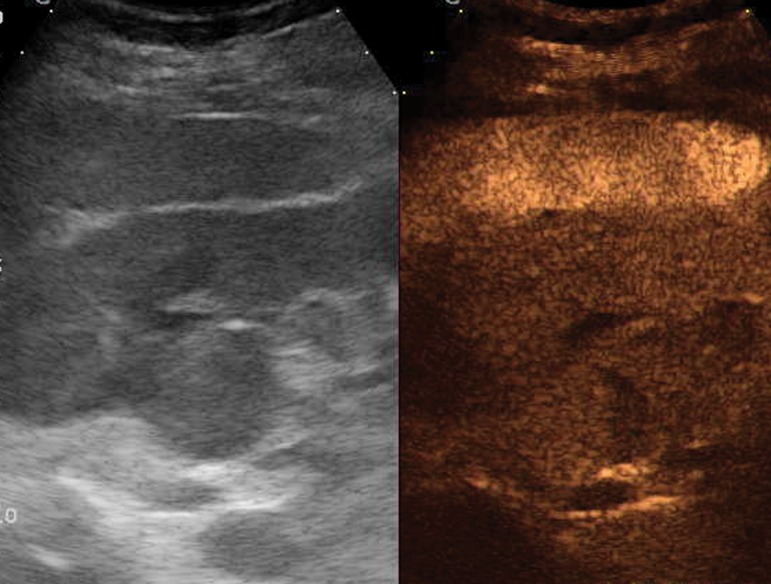
The focal area of pyelonephritis in the left kidney.
Figure 3.
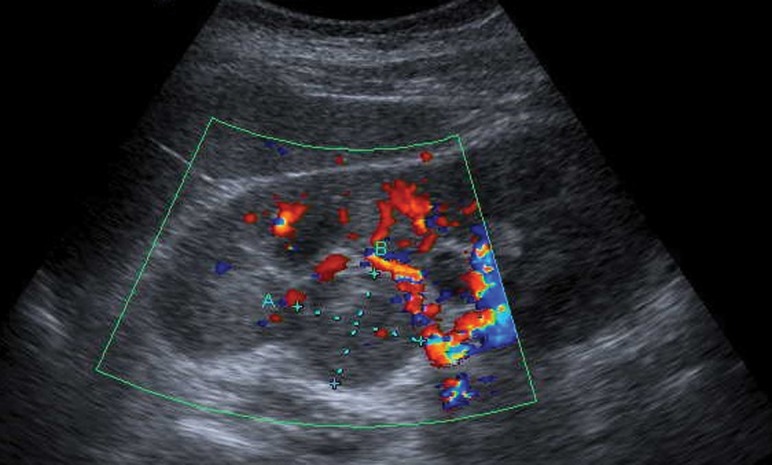
The focal area of pyelonephritis in the left kidney on color Doppler imaging.
DISCUSSION
Classically, pain in the right upper quadrant of the abdomen occurs as a result of hepatobiliary diseases, such as gallstones, cholecystitis, hepatitis, hepatic or sub-phrenic abscess, and herpes zoster (1,2). Right upper quadrant pain, with or without hypogastric consequences, is due to Fitz-Hugh-Curtis (FHC) syndrome in 12-25% of cases, which is characterized by the inflammation of Glisson's capsule concomitant with pelvic inflammatory disease (1,3). FHC syndrome manifests as perihepatitis in association with pelvic inflammatory disease. The syndrome occurs predominantly in young women, who complain of severe right upper quadrant pain during the acute phase that sometimes simulates pleurisy (1,4). In the chronic phase, numerous viscero-visceral and viscero-parietal adhesions are formed, initiating at Glisson's capsule; such cases are diagnosed using explorative laparotomy or laparoscopy (3,5). In the literature, approximately 12-25% of pelvic inflammatory disease cases occur concomitantly with FHC. The frequently involved etiological agents are of bacterial origin, and N. gonorrhoeae and C. trachomatis are among the most common (2,6,7). These microorganisms can travel from the pelvis to infect the surface capsule of the liver or the spleen via the peritoneal fluid (4,8). The symptoms are varied, ranging from simple non-specific pain in the hypogastric region, dysuria and dyspareunia to excessive vaginal secretions (3,9). Although most cases show a normal number of leukocytes, neutrophilic leukocytosis occurred in our case. Liver enzymes are typically normal or only mildly elevated, and ESV and CRP are elevated in almost all cases. The standard examination for the diagnosis is gene amplification by PCR, which has replaced the conventional bacterial cultures and allows for the isolation of microorganisms using cervical, urethral, rectal and throat swabs. Diagnostic tools play a key role in the diagnosis of FHC syndrome, and in particular, ultrasonography and CT are often conclusive, although in our case, MRI was used in consideration of the young age of the patient (10). The final diagnosis is made by integrating several laboratory and instrumental tests to exclude other diseases that occur with acute right upper quadrant pain. We would like to emphasize the particular association between acute left pyelonephritis with urine cultures positive for C. trachomatis and FHC syndrome. In recent years, there has been a progressive increase in the incidence of this syndrome, which is likely due to the continuous improvement of diagnostic techniques. The treatment is pharmacological, and if properly performed after a correct diagnosis, it leads to complete resolution of the clinical case, reducing the duration of hospitalization. Otherwise, incorrect diagnosis in the acute phase followed by inadequate antibiotic treatment may cause the disease to become chronic, with subsequent further complications; in this case, only surgical treatment by laparotomy or laparoscopy can lead to the correct diagnosis and therapy.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Rivero-Sánchez L, López-Soriano EM, Guarner-Aguilar L. Fitz-Hugh-Curtis syndrome: abdominal pain in women of 26 years old. Rev Esp Enferm Dig. 2011;103(10):546–8. doi: 10.4321/s1130-01082011001000009. [DOI] [PubMed] [Google Scholar]
- 2.Huang HH, Tsai CM, Tyan YS. Unusual cause should be kept in mind of abdominal pain in female patient. Fitz-Hugh-Curtis syndrome. Gastroenterology. 2011;140(3):e7–8. doi: 10.1053/j.gastro.2010.02.067. [DOI] [PubMed] [Google Scholar]
- 3.Ricci P, Lema R, Solá V, Fernández C, Fabres C, Fernández E, Pardo J. Fitz-Hugh-Curtis syndrome: Three cases of incidental diagnosis during laparoscopy. J Obstet Gynaecol. 2008;28(3):352–4. doi: 10.1080/01443610802058411. [DOI] [PubMed] [Google Scholar]
- 4.Hong DG, Choi MH, Chong GO, Yi JH, Seong WJ, Lee YS, et al. Fitz-Hugh-Curtis Syndrome: single centre experiences. J Obstet Gynaecol. 2010;30(3):277–80. doi: 10.3109/01443610903576282. [DOI] [PubMed] [Google Scholar]
- 5.Burton E, McKeating J, Stahlfeld K. Laparoscopic management of a small bowel obstruction of unknown cause. JSLS. 2008;12(3):299–302. [PMC free article] [PubMed] [Google Scholar]
- 6.Le Moigne F, Lamboley JL, Vitry T, Salamand P, Milou F, Farthouat P. Usefulness of contrast-enhanced CT scan for diagnosis of Fitz-Hugh-Curtis syndrome. Gastroenterol Clin Biol. 2009;33(12):1176–8. doi: 10.1016/j.gcb.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Woo SY, Kim JI, Cheung DY, Cho SH, Park SH, Han JY, Kim JK. Clinical outcome of Fitz-Hugh-Curtis syndrome mimicking acute biliary disease. World J Gastroenterol. 2008;14(45):6975–80. doi: 10.3748/wjg.14.6975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olson S, McComb PF. Formation of Fitz-Hugh Curtis adhesions due to perihepatitis associated with salpingitis. J Obstet Gynaecol Can. 2010;32(6):533–4. doi: 10.1016/s1701-2163(16)34517-0. [DOI] [PubMed] [Google Scholar]
- 9.MecLean AB. Fitz-Hugh-Curtis syndrome. J Obstet Gynaecol. 2008;28(3):259–60. doi: 10.1080/01443610802042993. [DOI] [PubMed] [Google Scholar]
- 10.Wang CL, Guo XJ, Yuan ZD, Shi Q, Hu XH, Fang L. Radiologic diagnosis of Fitz-Hugh-Curtis syndrome. Chin Med J (Engl) 2009;122(6):741–4. [PubMed] [Google Scholar]


