INTRODUCTION
Recent advances in surgical techniques have trended toward minimally invasive procedures. Currently, a laparoscopic approach has become the gold standard for splenectomy because it is an effective, reliable technique requiring a shorter hospitalization period with fewer surgical complications, less morbidity, and better esthetic results (1). However, as the number of ports increases in laparoscopy, there is an increase in the incidence of morbidity, including port entrance hernias and infection, internal organ injury, poorer esthetic results, and most importantly, bleeding. Morbidity resulting from the use of multiple ports has prompted the development of techniques using fewer ports (2).
Herein, we demonstrate the applicability of glove port single-incision laparoscopy, with a review of the surgical literature.
CASE DESCRIPTION
A 33-year-old female who initially presented with spontaneous nosebleeds was diagnosed with immune thrombocytopenic purpura (ITP) and had been followed for two years. After the patient developed steroid resistance, a splenectomy was planned. She had previously undergone surgery for a perforated peptic ulcer. A physical examination identified a midline incision scar above the abdomen. Ultrasonography indicated that the spleen was of normal size. No intravenous antibiotics were administered preoperatively. The patient was treated with cortisol for the surgery.
SURGICAL TECHNIQUE
With the patient in the 30° right lateral decubitus position, the abdominal cavity was entered through a 22-mm incision parallel to the skin folds at the left midclavicular line. A surgical glove port was formed using an extra-small ALEXIS wound protector (Applied Medical, Rancho Santa Margarita, CA, USA) and a size 7.5 standard surgical glove (Figures 1 and 2). One 12-mm and two 5-mm trocars were placed through incisions made in the glove fingers. Following CO2 insufflation, adhesions around the gastrosplenic ligament, which were caused by the previous peptic ulcer surgery, were dissected using an ultrasonic dissector. The spleen was suspended with a SILS clinch 36 grasper (Covidien, Mansfield, MA, USA) and dissected from its ligaments with the help of a harmonic dissector. After the hilum of the spleen was exposed, it was cut using an Endo-GIA II stapler (60-mm long, 2.5-mm staples, Auto Suture; US Surgical, Norwalk, CT) (Figure 3). The spleen was placed in a 15-mm bag (EndoCatch II, Autosuture, Covidien, Mansfield, MA, USA) (Figure 4), crushed, and removed from the abdominal cavity through the ALEXIS port. The procedure took 45 min. No intraoperative complications occurred during surgery.
Figure 1.

Glove port preparation.
Figure 2.

The glove port.
Figure 3.
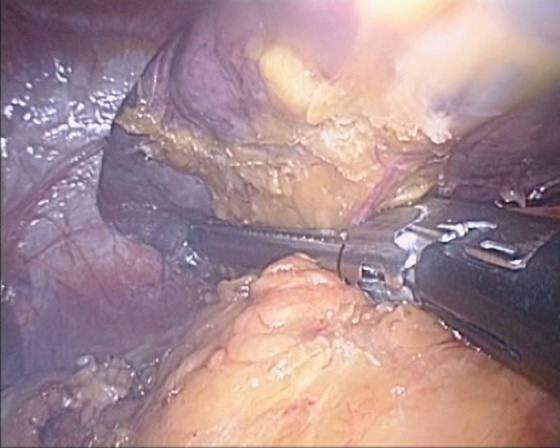
Cutting the hilum of the spleen using an Endo-GIA II stapler.
Figure 4.

The spleen was placed in a 15-mm bag, crushed, and removed from the abdominal cavity through the ALEXIS port.
The patient developed tachycardia on the second postoperative day, and her hemoglobin level decreased. Computed tomography showed a hematoma initiating where the spleen had been removed and extending to the pelvis. The patient then underwent a second surgery. With the patient in the same position, another surgical glove port was made, and the abdomen was explored. Bleeding was discovered at the vascular stapler line. The bleeding was sutured laparoscopically. After the intra-abdominal hematoma was drained, the abdominal cavity was irrigated. Finally, a drain was placed at the previous location of the spleen. The patient was discharged from the hospital on the third postoperative day. The pathology report showed congested splenectomy material consistent with ITP.
DISCUSSION
Single-port laparoscopy has been adapted to many surgical procedures (2-8). Other studies have demonstrated that laparoscopic splenectomy can be performed using only one incision (8-11). The advantages of the surgical glove port technique compared to the single-port technique include its ease of placement and use of inexpensive surgical equipment (12,13). The cost difference between these two techniques is an important factor, particularly in developing countries. Additionally, the surgical glove port technique ensures a safer entry while placing the port, and the surgeon has more mobility with the glove port technique than with the single-port technique. However, manipulations performed laparoscopically through a single port are more difficult compared with a standard laparoscopic approach.
More trocars can be placed through the glove fingers by making wider incisions as necessary. In this case, because of previous peptic ulcer surgery, an incision in the hypochondrium was preferred to a transumbilical entry. Consequently, the adhesions resulting from the previous operation posed no problems. A transumbilical entry may be a better esthetic choice in patients with no intraabdominal adhesions. We believe that a transumbilical incision would not cause any technical difficulties.
Another advantage of the surgical glove port compared with the standard laparoscopic splenectomy is that there is no need for a new incision or to enlarge the existing incision to remove the spleen from the abdomen. The disadvantages of this technique include punctures in the glove or ALEXIS port and gas leakage during the surgery. However, these problems are easily resolved during the procedure. In our case, the subsequent hemorrhage was easily treated using the glove-port technique. Although most new techniques are typically more expensive than established techniques, the glove port technique uses less costly, more widely available surgical equipment (12).
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Habermalz B, Sauerland S, Decker G, Delaitre B, Gigot JF, Leandros E, et al. Laparoscopic splenectomy: The clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2010;22(4):821–48. doi: 10.1007/s00464-007-9735-5. [DOI] [PubMed] [Google Scholar]
- 2.Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009;23(7):1419–27. doi: 10.1007/s00464-009-0463-x. [DOI] [PubMed] [Google Scholar]
- 3.Henckens T, Van de Putte D, Van Renterghem K, Ceelen W, Pattyn P, Van Nieuwenhove YJ. Laparoendoscopic single-site gastrectomy for a gastric GIST using double-bended instruments. J Laparoendosc Adv Surg Tech A. 2010;20(5):469–71. doi: 10.1089/lap.2009.0391. [DOI] [PubMed] [Google Scholar]
- 4.Podolsky ER, Curcillo PG 2nd. Single port access (SPA) surgery—a 24-month experience. J Gastrointest Surg. 2010;14(5):759–67. doi: 10.1007/s11605-009-1081-6. [DOI] [PubMed] [Google Scholar]
- 5.Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced recovery after surgery: A consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24(3):466–77. doi: 10.1016/j.clnu.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Rao PP, Bhagwat SM, Rane A. The feasibility of single-port laparoscopic cholecystectomy: A pilot study of 20 cases. HPB (Oxford) 2008;10(5):336–40. doi: 10.1080/13651820802276622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reavis KM, Hinojosa MW, Smith BR, Nguyen NT. Single laparoscopic incision transabdominal surgery sleeve gastrectomy. Obes Surg. 2008;18(11):1492–94. doi: 10.1007/s11695-008-9649-x. [DOI] [PubMed] [Google Scholar]
- 8.Targarona EM, Pallares JL, Balague C, Luppi CR, Marinello F, Hernández P, et al. Single incision approach for splenic diseases: a preliminary report on a series of 8 cases. Surg Endosc. 2010;24(9):2236–40. doi: 10.1007/s00464-010-0940-2. [DOI] [PubMed] [Google Scholar]
- 9.Barbaros U, Dinççağ A. Single incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg. 2009;13(8):1520–3. doi: 10.1007/s11605-009-0869-8. [DOI] [PubMed] [Google Scholar]
- 10.Misawa T, Sakamoto T, Ito R, Shiba H, Gocho T, Wakiyama S, et al. Single-incision laparoscopic splenectomy using the “tug-exposure technique” in adults: results of ten initial cases. Surg Endosc. 2011;25(10):3222–7. doi: 10.1007/s00464-011-1697-y. [DOI] [PubMed] [Google Scholar]
- 11.Srikanth G, Wasim MD, Sajjad A, Shetty N. Single-incision laparoscopic splenectomy with innovative gastric traction suture. J Minim Access Surg. 2011;7(1):68–70. doi: 10.4103/0972-9941.72386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayashi M, Asakuma M, Komeda K, Miyamoto Y, Hirokawa F, Tanigawa N. Effectiveness of a surgical glove port for single port surgery. World J Surg. 2010;34(10):2487–9. doi: 10.1007/s00268-010-0649-3. [DOI] [PubMed] [Google Scholar]
- 13.Ishida H, Okada N, Ishibashi K, Ohsawa T, Kumamoto K, Haga N. Single-incision laparoscopic-assisted surgery for colon cancer via a periumbilical approach using a surgical glove: initial experience with 9 cases. Int J Surg. 2011;9(2):150–4. doi: 10.1016/j.ijsu.2010.10.010. [DOI] [PubMed] [Google Scholar]


