INTRODUCTION
Hypoxemia is a frequent finding after lung transplantation (LTx) (1-2). The underlying mechanisms include alveoli collapse, diffuse alveolar damage, ventilation-perfusion mismatch, and alveolar-capillary membrane damage (3-5).
Primary graft dysfunction (PGD) represents a multifactorial injury to the transplanted lung that develops in 15-25% of patients during the first days after transplantation; it is variously referred to as "ischemia-reperfusion injury" and "early graft dysfunction" (6). PGD is characterized by severe hypoxemia, lung edema, and the radiographic appearance of diffuse pulmonary opacities in the absence of another identifiable cause (7). Despite significant advances in organ preservation, surgical technique, and perioperative care, PGD is responsible for significant morbidity and mortality after lung transplantation (8-9).
Most patients recover with intensive care unit (ICU) support that includes non-invasive and invasive ventilation, negative fluid balance, and nitric oxide. However, some patients with severe PGD develop refractory hypoxemia, resulting in shock, multiorgan failure, and mortality in 60% of cases (10-12). During the past few years, highlighted by the influenza-A H1N1 epidemic, gas exchange support using an extracorporeal membrane oxygenator (ECMO) has been used as life-saving therapy in severe cases of respiratory failure (13-15). We report the case of a patient with a severe form of PGD after lung transplantation who was successfully supported using veno-venous ECMO until respiratory recovery.
CASE DESCRIPTION
A 20-year-old female patient with cystic fibrosis underwent bilateral lung transplantation without cardiopulmonary bypass at InCor of Hospital das Clínicas of the University of São Paulo. During the previous six months, the patient was hospitalized four times due to worsening dyspnea and hypoxemia. Just before lung transplantation, the patient presented with pneumonia and right lung atelectasis, with an increased need for oxygen and non-invasive ventilation (Figure 1).
Figure 1.

Chest X-ray showing a diffuse opacity of the right lung that is compatible with atelectasis.
Bilateral lung transplantation (LTx) was performed without complications. The ischemic time of the left graft was 660 minutes and that of the right graft was 415 minutes. The patient was not exposed to allogeneic blood transfusion, and fluid resuscitation was carried out with lactated Ringer's solution and albumin. At the end of the surgery, the patient had a lactate level of 6 mmol/L and a mixed venous saturation (ScVO2) of 75%, and the cardiac output was 4.8 L/min. After a 16-hour procedure, the patient was brought to the ICU using mechanical ventilation (MV), intubated and received norepinephrine (0.15 μg/Kg/min).
The patient presented no complications during the immediate postoperative period and was weaned from MV 18 hours after ICU arrival. However, on the third day after surgery, the patient developed respiratory failure due to severe hypoxemia (PO2/FiO2 of 130 mmHg), with normal filling pressures (a central venous pressure of 7 mmHg and a wedge pressure of 12 mmHg). A chest X-ray revealed diffuse bilateral patchy opacities (Figure 2).
Figure 2.
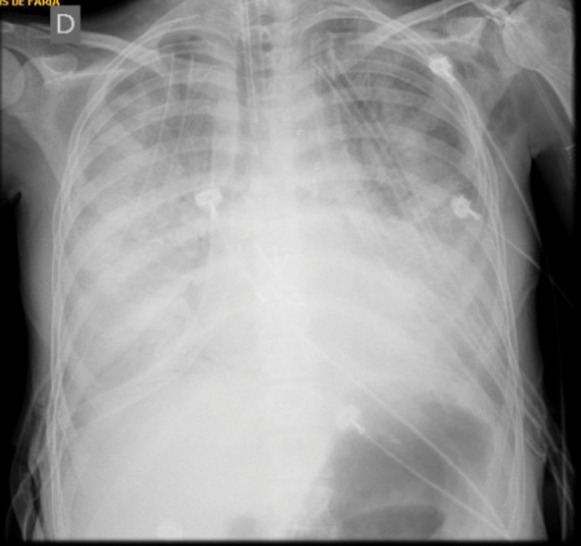
Chest X-ray immediately after orotracheal intubation showing diffuse bilateral opacities that are compatible with primary graft dysfunction after lung transplantation
After approximately three hours of non-invasive mechanical ventilation and forced diuresis, respiratory function and gas exchange worsened (PO2/FiO2 of 100 mmHg and PaCO2 of 124 mmHg), and the hemodynamics of the patient progressively deteriorated. She presented a mean blood pressure of 50 mmHg, profuse sweating, and delayed peripheral perfusion. The patient was then placed under assisted pressure-controlled mechanical ventilation with an inspired oxygen fraction (FiO2) of 1.0, a positive end-expiratory pressure (PEEP) of 14 cmH2O, an inspiratory pressure of 26 cmH2O (12 cmH2O driving pressure), an inspiratory time of 0.80 seconds and a respiratory rate of 30. Applying these parameters, the arterial blood gas presented a PaO2 of 54 mmHg, a PaCO2 of 118 mmHg, a pH of 7.12 and an oxygen saturation of 80%. Subsequent tests revealed a progressive worsening of the physiological parameters, with a ScVO2 of 48% and lactate of 8 mmol/L. Hypoxemia and hypercapnia were persistent and refractory to recruitment maneuvers, with PEEP values of 20-40 cmH2O. A transesophageal echocardiogram was performed and showed no abnormality at the pulmonary vein anastomoses.
Given the imminent risk of death from refractory hypoxemia, six hours after invasive mechanical ventilation, the ECMO team at our institution began veno-venous ECMO support as a rescue procedure. Using the Seldinger technique, 20-Fr draining cannulae were inserted into the left common femoral vein, and a return cannula was placed into the right jugular vein. The location was guided using ultrasound. A centrifuge magnetic pump with a polymethylpentene oxygenation membrane (Rotaflow/Jostra Quadrox, Maquet Cardiopulmonary AG, Hirrlinger, Germany) was used. Initially, the blood flow was maintained at 500 mL per minute until the system was filled with blood. The blood flow and sweeper (gas) flow were subsequently increased to 2,000 mL per minute. The blood flow and sweeper flow were then manipulated to target a peripheral oxygen saturation of at least 90%. Anticoagulation with heparin was started with 15 U/Kg of heparin per hour, with the aim of reaching an activated partial thromboplastin time ratio of 1.5–2.0. After two hours of veno-venous ECMO support, gas analysis revealed increasing of PO2/FiO2 to 220, decreased levels of PaCO2 to 45 mmHg, and improvement of the physiologic parameters (lactate 2.5 mmol/L, ScVO2 of 75%) and weaning of norepinephrine.
Mechanical ventilation was adjusted to achieve a positive end-expiratory pressure (PEEP) of 10 cmH2O, an inspired fraction of oxygen (FiO2) of 0.4, a driving pressure lower than 10 cmH2O, and a respiratory rate of 10 breaths per minute (5). The parameters that were checked daily included arterial blood gases, clots in the system that were visible through transillumination, pump campanula auscultation, and flowmeter lubrification to maintain a good signal quality.
The ECMO blood flow was adjusted to maintain the PaO2 above 55 mmHg, and the sweeper flow was adjusted to maintain the pH≥7.3 (through PaCO2 modulation). Fentanyl was used as an analgesic and sedative to reach a Richmond agitation sedation scale (RASS) score of zero and no pain. The body temperature was kept between 36 and 37 degrees Celsius using an external apparatus adapted to the ECMO system (Figure 3).
Figure 3.

A patient in intensive care receiving mechanical ventilation and ECMO therapy.
A weaning (autonomy) test from ECMO support was carried out daily. Five days after treatment, the patient presented a PO2/FiO2 of 230 mmHg, and the FiO2 set was adjusted to 0.6 in the ECMO. The sedation was interrupted, and as patient maintained adequate arterial saturation and a respiratory rate of 20 breaths per minute while in spontaneous mode in mechanical ventilator with FiO2 of 0.30, she was successfully weaned from invasive ventilation. The patient stayed in ECMO during the next two days in an awake and cooperative state with no pain, at which point she was considered able to have the ECMO support removed. The decannulation was performed at the bedside without complications. The patient was discharged from the ICU after recovering lung function without complications.
DISCUSSION
Respiratory support with extracorporeal membrane oxygenation (ECMO) has been used since 1971, with varied results (16-19). In 2009, the influenza-A epidemic renewed the interest in this therapy, which had shown efficacy in treating refractory hypoxemia in many patients worldwide (20-21). The CESAR trial revealed a reduction in mortality at six months with ECMO compared with conventional protective mechanical ventilation in severe ARDS patients (22).
In conjunction with lung transplantation, ECMO may be useful as a temporary support for respiratory failure while patients are waiting for the organ and after transplantation in cases of refractory hypoxemia (23-25). Most cases of severe hypoxemia after LTx are due to PGD and result in high rates of mortality. A few single-center experiences have been reported, with relatively few cases of ECMO after LTx (26-27). The Extracorporeal Life Support Organization (ELSO) registry, which was established to improve the quality and outcome of extracorporeal life support (ECLS) in patients treated with ECMO, currently includes 151 post-LTx patients with PGD (28). The mean age is 35±18 years. Indications for LTx included acute respiratory distress syndrome, (15%), cystic fibrosis (15%), idiopathic pulmonary fibrosis (8%), primary pulmonary hypertension, (10%), emphysema (15%), acute lung failure (11%), other (23%), and unknown (3%). The ECMO run time was 140±212 hours. Veno-venous ECMO was used in 25 patients, veno-arterial in 89 patients, and other modes in 15 patients (unknown in 22 patients). ECMO was discontinued in 93 patients because of lung recovery. It was also discontinued in 29 patients with multiorgan failure, 22 patients who died with no further specification, and seven patients for other reasons. In total, 63 (42%) of the patients survived the hospital stay. The major complications during ECMO included hemorrhage (52%), hemodialysis (42%), neurologic complications (12%), cardiac complications (28%), inotropic support (77%), and sepsis (15%) (28).
In our patient, ECMO was placed on the third day after LTx due to refractory hypoxemia and hypercapnic acidosis. The patient presented no complications of the treatment, and the duration spent in ECMO was 168 hours. The V-V ECMO allowed adequate ventilatory support and resulted in a reversion of the acidosis and shock. The choice of ECMO modality (veno-venous or veno-arterial) depends on the hemodynamic stability and need for cardiac support (29). The veno-venous system is usually preferred in stable patients because it involves an easier implant technique and fewer bleeding and thrombotic complications. In our patient, veno-venous ECMO was used once the patient presented a normal ejection fraction without right ventricle dysfunction, and the shock was interpreted as a consequence of hypoxemia and acidosis. After a few hours of treatment and the recovery of oxygenation, the shock reversed, highlighting the right indication of the system.
Although the ELSO registry was not primarily established to study ECMO in LTx, it provides valuable insights and evidence that there is indeed an appreciable salvage rate with the use of ECMO for PGD after LTx (28). Clearly, this is a high-risk patient population, and no single center can accumulate a large volume of ECMO experience for this specific indication.
The case under discussion underscores the importance of ECMO as a rescue therapy in patients undergoing lung transplantation who develop severe hypoxemia. The main challenges of this treatment are addressing the clear indications, costs, system availability, and team training.
The Hospital das Clínicas ECMO team was innovative in Brazil and has become a referral center with physicians, nurses, and physiotherapists to assist patients and train individuals to administer ECMO. In a recent paper from this team, a 40% survival rate was described when using ECMO as a respiratory and/or cardiovascular support (30).
The importance of this discussion is to call attention to the need to develop experience and perform more studies in patients treated with ECMO to better study the outcomes, determine the optimum treatment strategies, and optimize the patient and device selection, thus improving the outcomes of patients who require this unique therapy.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Dhillon GS, Zamora MR, Roos JE, Sheahan D, Sista RR, Van der Starre P, et al. Lung transplant airway hypoxia: a diathesis to fibrosis. Am J Respir Crit Care Med. 2010;182(2):230–6. doi: 10.1164/rccm.200910-1573OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luckraz H, Goddard M, McNeil K, Atkinson C, Charman SC, Stewart S, et al. Microvascular changes in small airways predispose to obliterative bronchiolitis after lung transplantation. J Heart Lung Transplant. 2004;23(5):527–31. doi: 10.1016/j.healun.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Kamler M, Nowak K, Bock M, Herold U, Motsch J, Hagl S, et al. Bronchial artery revascularization restores peribronchial tissue oxygenation after lung transplantation. J Heart Lung Transplant. 2004;23(6):763–6. doi: 10.1016/j.healun.2003.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Ware LB, Golden JA, Finkbeiner WE, Matthay M. Alveolar Epithelial Fluid Transport Capacity in Reperfusion Lung Injury after Lung Transplantation. Am J Respir Crit Care Med. 1999;159(3):980–8. doi: 10.1164/ajrccm.159.3.9802105. [DOI] [PubMed] [Google Scholar]
- 5.Meade Granton JT, Matte-Martyn A, McRae K, Weaver B, Cripps P. A Randomized Trial of Inhaled Nitric Oxide to Prevent Ischemia–Reperfusion Injury after Lung Transplantation. AmJ Respir Crit Care Med. 2003;167(11):1483–9. doi: 10.1164/rccm.2203034. [DOI] [PubMed] [Google Scholar]
- 6.Christie JD, Kotloff RM, Ahya VN, Tino G, Pochettino A, Gaughan C, et al. The Effect of Primary Graft Dysfunction on Survival after Lung Transplantation. Am J Respir Crit Care Med. 2005;171(11):1312–6. doi: 10.1164/rccm.200409-1243OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kotloff RM, Thabut G. Lung Transplantation. Am J Respir Crit Care Med. 2011;184(2):159–71. doi: 10.1164/rccm.201101-0134CI. [DOI] [PubMed] [Google Scholar]
- 8.Daud SA, Yusen RD, Meyers BF, Chakinala MM, Walter MJ, Aviva A, Aloush AA. Impact of Immediate Primary Lung Allograft Dysfunction on Bronchiolitis Obliterans Syndrome. Am J Respir Crit Care Med. 2007;175(5):507–13. doi: 10.1164/rccm.200608-1079OC. [DOI] [PubMed] [Google Scholar]
- 9.Christie JD, Kotloff RM, Ahya VN, Tino G, Pochettino A, Gaughan C, et al. The effect of primary graft dysfunction on survival after lung transplantation. Am J Respir Crit Care Med. 2005;171(11):1312–6. doi: 10.1164/rccm.200409-1243OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan SU, Salloum J, O'Donovan PB, Mascha EJ, Mehta AC, Matthay MA, et al. Acute pulmonary edema after lung transplantation: the pulmonary reimplantation response. Chest. 1999;116(1):187–94. doi: 10.1378/chest.116.1.187. [DOI] [PubMed] [Google Scholar]
- 11.Thabut G, Vinatier I, Stern J, Leseche G, Loirat P, Fournier M, et al. The Effect of Primary Graft Dysfunction on Survival after Lung Transplantation. Chest. 2002;121(6):1876–82. doi: 10.1378/chest.121.6.1876. [DOI] [PubMed] [Google Scholar]
- 12.Christie JD, Carby M, Bag R, Corris P, Hertz M, Weill D. Report of the ISHLT Working Group on Primary Lung Graft Dysfunction. II. Definition. A consensus statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2005;24(10):1454–9. doi: 10.1016/j.healun.2004.11.049. [DOI] [PubMed] [Google Scholar]
- 13.Noah MA, Peek GJ, Finney SJ, Griffiths MJ, Harrison DA, Grieve R, et al. Referral to an Extracorporeal Membrane Oxygenation Center and Mortality Among Patients With Severe 2009 Influenza A(H1N1) JAMA. 2011;306(15):1659–68. doi: 10.1001/jama.2011.1471. [DOI] [PubMed] [Google Scholar]
- 14.Schout D, Hajjar LA, Galas FR, Uip DE, Levin AS, Caiaffa Filho HH, et al. Epidemiology of human infection with the novel virus influenza A (H1N1) in the Hospital das Clínicas, São Paulo, Brazil—June-September 2009. Clinics. 2009;64(10):1025–30. doi: 10.1590/S1807-59322009001000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hajjar LA, Schout D, Galas FR, Uip DE, Levin AS, Caiaffa Filho H, et al. Guidelines on management of human infection with the novel virus influenza A (H1N1)—a report from the Hospital das Clínicas of the University of São Paulo. Clinics. 2009;64(10):1015–24. doi: 10.1590/S1807-59322009001000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davies A, Jones D, Bailey M, Beca J, Bellomo R, Blackwell N, et al. Extracorporeal Membrane Oxygenation for 2009 Influenza A(H1N1) Acute Respiratory Distress Syndrome. JAMA. 2009;302(17):1888–95. doi: 10.1001/jama.2009.1535. [DOI] [PubMed] [Google Scholar]
- 17.Zapol WM, Snider MT, Hill JD, Fallat RJ, Bartlett RH, Edmunds LH, et al. Extracorporeal membrane oxygenation in severe acute respiratory failure. A randomized prospective study. JAMA. 1979;242(20):2193–6. doi: 10.1001/jama.242.20.2193. [DOI] [PubMed] [Google Scholar]
- 18.Thiagarajan RR, Brogan TV, Scheurer MA, Laussen PC, Rycus PT, Bratton SL. Extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in adults. Ann Thorac Surg. 2009;87(3):778–85. doi: 10.1016/j.athoracsur.2008.12.079. [DOI] [PubMed] [Google Scholar]
- 19.Forrest P, Ratchford J, Burns B, Herkes R, Jackson A, Plunkett B, et al. Retrieval of critically ill adults using extracorporeal membrane oxygenation: an Australian experience. Intensive Care Med. 2011;37(5):824–30. doi: 10.1007/s00134-011-2158-8. [DOI] [PubMed] [Google Scholar]
- 20.Extracorporeal Membrane Oxygenation for 2009 Influenza A(H1N1) Acute Respiratory Distress Syndrome. JAMA. 2009;302(17):1888–95. doi: 10.1001/jama.2009.1535. [DOI] [PubMed] [Google Scholar]
- 21.Patroniti N, Zangrillo A, Pappalardo F, Peris A, Cianchi G, Braschi A, et al. The Italian ECMO network experience during the 2009 influenza A(H1N1) pandemic: preparation for severe respiratory emergency outbreaks. Intensive Care Med. 2011;37(9):1447–57. doi: 10.1007/s00134-011-2301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374(9698):1351–63. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 23.Xu L, Li X, Xu M, Gao C, Zhu J, Ji B. Perioperative use of ECMO during double lung transplantation. ASAIO J. 2009;55(3):255–8. doi: 10.1097/MAT.0b013e3181a05795. [DOI] [PubMed] [Google Scholar]
- 24.Park M, Costa EL, Azevedo LC, Afonso Junior JE, Samano MN, Carvalho CR. Extracorporeal membrane oxygenation as a bridge to pulmonary transplantation in Brazil: are we ready to embark upon this new age. Clinics. 2011;66(9):1659–61. doi: 10.1590/S1807-59322011000900027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Azevedo LC, Park M, Costa EL, Santos EV, Hirota A, Taniguchi LU, et al. Extracorporeal membrane oxygenation in severe hypoxemia: time for reappraisal. J Bras Pneumol. 2012;38(1):7–12. doi: 10.1590/s1806-37132012000100003. [DOI] [PubMed] [Google Scholar]
- 26.Bittner HB, Binner C, Lehmann S, Kuntze T, Rastan A, Mohr FW. Replacing cardiopulmonary bypass with extracorporeal membrane oxygenation in lung transplantation operations. Eur J Cardiothorac Surg. 2007;31(3):462–7. doi: 10.1016/j.ejcts.2006.11.050. [DOI] [PubMed] [Google Scholar]
- 27.Ko WJ, Chen YS, Lee YC. Replacing cardiopulmonary bypass with extracorporeal membrane oxygenation in lung transplantation operations. Artif Organs. 2001;25(8):607–12. doi: 10.1046/j.1525-1594.2001.025008607.x. [DOI] [PubMed] [Google Scholar]
- 28.Fischer S, Bohn D, Rycus P, Pierre AF, de Perrot M, Waddell TK, et al. Extracorporeal membrane oxygenation for primary graft dysfunction after lung transplantation: analysis of the Extracorporeal Life Support Organization (ELSO) registry. J Heart Lung Transplant. 2007;26(5):472–7. doi: 10.1016/j.healun.2007.01.031. [DOI] [PubMed] [Google Scholar]
- 29.Thiagarajan RR, Brogan TV, Scheurer MA, Laussen PC, Rycus PT, Bratton SL. Extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in adults. Ann Thorac Surg. 2009;87(3):778–85. doi: 10.1016/j.athoracsur.2008.12.079. [DOI] [PubMed] [Google Scholar]
- 30.Park M, Azevedo LC, Mendes PV, Carvalho CR, Amato MB, Schettino GP, et al. First-year experience of a Brazilian tertiary medical center in supporting severely ill patients using extracorporeal membrane oxygenation. Clinics. 2012;67(10):1157–63. doi: 10.6061/clinics/2012(10)07. [DOI] [PMC free article] [PubMed] [Google Scholar]


