Abstract
A case of primary amyloidosis of urinary bladder was presented with painless heamaturia and irritative urinary symptoms. Radiological imaging showed multiple small masses within the urinary bladder with suspicion of multiple transitional cell carcinomas within the urinary bladder. Cystoscopy confirmed the multiple masses within the urinary bladder, some showing haemorrhagic papules and papillary projections over the masses. Histopathology of the biopsy material was negative for the malignancy. Immunostaining of the biopsy material with Congo red stain showed the presence of amyloid fibrils within the biopsy material. Further investigations of systemic illness exclude the secondary amyloidosis. Transurethral resection was done. Patient showed improvement after the resection and no recurrence was observed during follow up. The purpose of this case presentation is to create awareness among the urologists to think for the rare entity of urinary amyloidosis especially if the histopathology is negative for the malignant cells.
Introduction
Amyloidosis consists of extracellular deposition of amyloid, a protein with a fibrillary structure, in one or more body sites. It was first described by Virchow in 1853. The organs commonly involved are urinary bladder, lung, larynx, skin, tongue and the region around the eye. In the urinary tract, amyloid deposition usually starting from kidney to renal pelvis, ureters, urinary bladder and urethra. The kidney is nearly always involved in secondary amyloidosis and in approximately 50% of the cases of primary amyloidosis. However, in primary amyloidosis urinary bladder is usually involved. Understanding of this condition is of clinical interest because primary amyloidosis affecting only the bladder may be easily confused with an infiltrating tumor because of its appearance on imaging as well as on Cystoscopy, misleading the diagnosis to malignancy. (1) Accurate diagnosis depends on biopsy of the bladder lesion with Immunostaining of the biopsy material with Congo red stain, showing negative malignant cells on histopathology and presence of amyloid fibrils on Cong red staining. It is to be stressed that Immunostaining of the biopsy material is the key for the diagnosis. The treatment is usually conservative with transurethral resection. Long term follow up with imaging and Cystoscopy is required.
Case report
A Sixty one year old male patient presented with painless gross heamaturia and irritative voiding symptoms for few days. He was hypertensive and on antihypertensive medication. General physical examination was unremarkable. Hemoglobin was 9 mg/dl and his blood chemistry was normal. Urine was negative for Bence Jones protein. Urine cytology showed slightly atypical pseudo papillary clusters analysis numerous red blood cells. Initial Ultrasound examination of the urinary bladder showed small mass in the posterior wall of urinary bladder, suggestive of transitional cell carcinoma (Fig 1). Further evaluation with CT scan of abdomen and pelvis was done showing multiple small lesions in the posterior bladder wall without bladder wall infiltration to the adjacent structures (Fig 2). No systemic deposits were seen. No ascites was defined. Cystoscopy confirmed 2 raised erythematous lesions less than 1 cm in the left lateral wall and 2 in the posterior edematous wall of urinary bladder (Fig. 3). Histopathology of the biopsied material showed no malignant cells (Fig 4). Immunostaining of the biopsied material with Congo red stain confirmed the presence of amyloid fibrils in the biopsy material (fig.5) confirming the diagnosis of urinary bladder amyloidosis. Further investigation of the rest of the organs did not show the presence of amyloid. A diagnosis of primary amyloidosis of urinary bladder was established. Transurethral resection of the lesions was done. Patient showed improvement after resection and followed for one year with Ultrasound examination and CT scan with no evidence of recurrence. See table 1 for summary.
Fig. 1.
Ultrasound examination showing small polypoidal mass in the posterior wall of urinary bladder
Fig. 2.
CT scan showing nodular masses in the posterior wall of urinary bladder. No adjacent infiltration seen.
Figure 3.
Cystoscopy showing urinary bladder nodules with edematous wall.
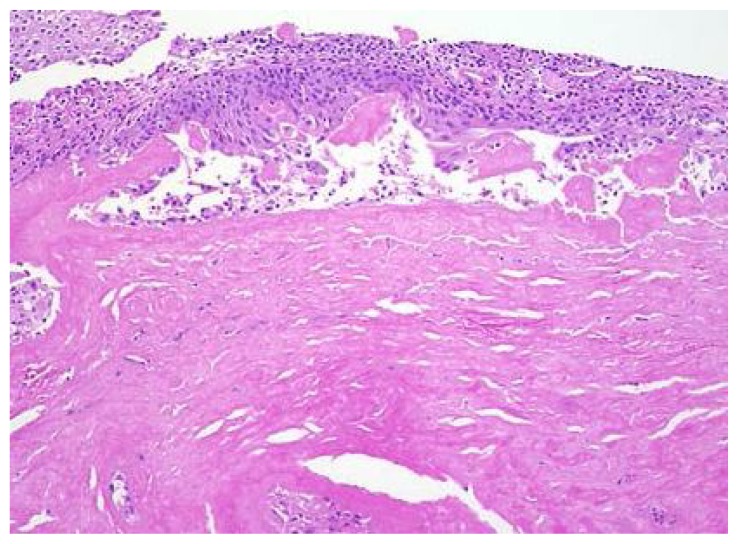
Figure 4.
Histopathology showing pink amorphous material in the lamina propria.
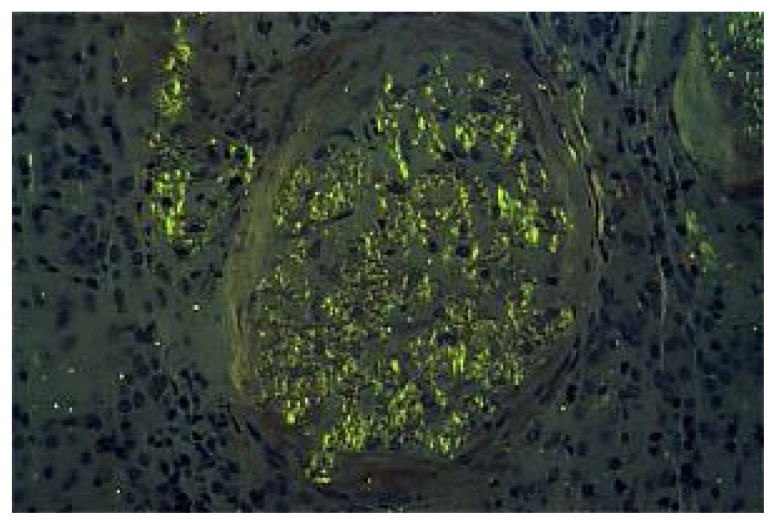
Fig 5.
Congo red stains of biopsy material showing characteristic “apple-green” birefringence of amyloid deposition.
Table 1.
Summary of presentation
| Age/sex | Clinical presentation | Previous genitourinary history | Systemic illness | Imaging diagnosis | Cystoscopy | Immunostaining with Congo red stain | Treatment |
|---|---|---|---|---|---|---|---|
| 61 year male | Gross heamaturia, voiding irritative symptoms | Nil | Hypertension only | Multiple small masses in the urinary bladder | Multiple small masses in the urinary bladder with hemorrhages and papillary projections | Amyloid fibrils | Transurethral resection of masses |
Discussion
Amyloidosis refers to a variety of conditions in which amyloid protein are abnormally deposited in organs and/or tissues. (2) Symptoms vary widely depending upon the site of amyloid deposition. Amyloidosis may be inherited or acquired. (3)
Primary amyloidosis arises from a disease with disordered immune cell function such as multiple myeloma and other immunocyte abnormalities. Secondary (reactive) amyloidosis is those occurring as a complication of some other chronic inflammatory or tissue destructive disease. (4) In the urinary tract, deposition of amyloid can occur anywhere, starting from kidney to renal pelvis, ureters, urinary bladder, urethra and even penis.
The kidney is nearly always involved in secondary amyloidosis and in approximately 50% of the cases of primary amyloidosis. This is in contrast to the urinary bladder, which is usually affected in primary localized amyloidosis.
Painless heamaturia is a presenting symptom of amyloidosis. However, infections, calculi, neoplasms, drugs and blood clotting disorder can cause heamaturia.
According to Malek et al study, there were only 160 cases reported in the literature so far for the primary amyloidosis of urinary bladder. (5)
Localized amyloidosis poses a diagnostic problem because of its nonspecific presenting symptoms and uncharacteristic cystoscopy appearance, as well as radiological appearances which may mimic inflammatory lesion or a neoplastic lesion. Cystoscopy may shows nodular-to-polypoidal, single or multiple masses
Histopathological examination is necessary may miss the diagnosis of amyloidosis if simultaneous Immunostaining is not done. (7) On Congo red staining, the material shows the classical apple-green birefringence under polarized light.
Management is conservative with transurethral resection of the mass. Few reports showed in cases of recurrent mild heamaturia intravesical dimethyl sulfoxide seems to be useful, intractable hemorrhage due to the bladder involvement of systemic amyloidosis. (8)
For follow up, periodic cystoscpic examination is recommended.
Conclusion
Primary bladder amyloidosis of urinary bladder is a rare disease, presenting as painless gross heamaturia. Radiological imaging is usually misleading mimicking with malignancy. Cystoscopy shows polypoidal mass and cannot exclude the amyloidosis. Histopathology is mandatory to exclude the malignancy. Immunostaining the biopsy with Congo red stain is the only means to reach the correct diagnosis. Transurethral resection or coagulation and conservative treatment are best options for the treatment. Long term follow up is required.
References
- 1.Lehtonen T, Makinen J, Wikstrom S. Localized amyloidosis of urinary bladder. Eur Urol. 1991;20:113–6. doi: 10.1159/000471677. [DOI] [PubMed] [Google Scholar]
- 2.Strong GI, Kelsey D, Hoch W. Primary amyloid disease of bladder. J Urol. 1974;112:463–6. doi: 10.1016/s0022-5347(17)59763-3. [DOI] [PubMed] [Google Scholar]
- 3.Ferch R, Haskell R, Farebrother T. Primary amyloidosis of urinary bladder and ureter. Br J Urol. 1997;80:953–4. doi: 10.1046/j.1464-410x.1997.t01-1-00329.x. [DOI] [PubMed] [Google Scholar]
- 4.Dias R, Fernandez M, Patel RC, de Shadarevian JJ, Lavengood RW. Amyloidosis of renal pelvis and urinary bladder. Urology. 1979;14:401–4. doi: 10.1016/0090-4295(79)90092-x. [DOI] [PubMed] [Google Scholar]
- 5.Malek RS, Wahner-Roedler DL, Gertz MA, Kyle RA. Primary localized amyloidosis of the bladder: Experience with dimethyl sulfoxide therapy. J Urol. 2002;168:1018–20. doi: 10.1016/S0022-5347(05)64564-8. [DOI] [PubMed] [Google Scholar]
- 6.Tirzaman O, Wahner-Roedler DL, Malek RS, Sebo TJ, Li CY, Kyle RA. Primary localized amyloidosis of the urinary bladder: A case series of 31 patients. Mayo Clin Proc. 2000;75:1264–8. doi: 10.4065/75.12.1264. [DOI] [PubMed] [Google Scholar]
- 7.Grainger R, O’Riordan B, Cullen A, Kelly D, Heaney J. Primary amyloidosis of lower urinary tract. Urology. 1988;31:14–6. doi: 10.1016/0090-4295(88)90563-8. [DOI] [PubMed] [Google Scholar]
- 8.Mandhani A, Srivastava A, Kumar A, et al. Localized primary amyloidosis of the genitourinary tract: Does conservation help? Urol Int. 2004;73:280–2. doi: 10.1159/000080843. [DOI] [PubMed] [Google Scholar]