Abstract
Background
Thalassemia is the most common monogenic disease in South-East of Iran. Despite the 70% reduction in Iranian thalassemia cases after thalassemia control comprehensive program, 601 affected babies were born in Sistan and Balouchistan Province, Iran from 2002 to 2010, so this study aims at investigating the causes of new thalassemia cases.
Methods:
Data from this retrospective cross-sectional study was collected through interviews and information in the patients’ hospital records.
Results:
Data revealed that 52.4% of fathers and 78.4% of mothers of thalassemic children had elementary education or less. In addition, 78.6% of the couples did not undergo premarital screening for thalassemia and 71.2% of the couples were not notified of their own minor thalassemia until a child was born with major thalassemia. Of the diagnosed minor couples, about 25% did PND and the others did not carry out because mothers were unaware of proper gestational age and of the importance of this issue, financial problems, and the husbands’ disagreement to take the tests. Moreover, 16 mothers, in spite of being diagnosed of having a major fetus, refused to terminate the pregnancy.
Conclusion:
The most preventable causes for affected births include couples’ unawareness of being minor and unawares of the PND importance and process.
Keywords: Thalassemia, Prevention, Prenatal diagnosis, Premarital screening, Iran
Introduction
Thalassemia is the most common monogenic disease in Iran as well as many countries of the Middle East and the Mediterranean region. It has been reported in over 60 countries of the world, together composing the so-called thalassemia belt. Thalassemia is an inherited disease, through which the person receives a defective gene from the father and another from the mother. Due to the disease’s characteristic inability to construct hemoglobin, the person must depend on blood transfusion. The inefficiency of the patient’s blood-making system and the continuous blood transfusion cause the received red blood cells to become slippery, leading to the accumulation of iron in various organs of the body. The gradual increase of iron, in turn, damages tissues and creates numerous problems for the patient (1, 2).
The frequency of minor β-thalassemia varies in different parts of Iran. This frequency is reported to be 10% in northern regions and 4–8% in other regions (3). At present, Sistan and Baluchistan with 2050 major thalessemic patients in a subtropical area in the south-east of Iran holds the highest rate of thalassemia in the country (4).
Not very long ago, children with major thalassemia usually died in the first decade of their lives, but now the improved treatment processes, preserving hemoglobin level and applying proper iron chelators, have increased their life expectancy considerably. Despite the efforts to develop a treatment based on gene therapy and bone marrow transplantation which is at the moment highly expensive and not easily affordable by an ordinary family, no effective successes have so far been achieved. Moreover, conventional treatment involving blood transfusions and iron chelating are costly. Therefore, preventive approaches seem to be more applicable and reasonable. One of the most effective approaches to reduce the disease incidence is screening couples for β-thalassemia, prenatal diagnosis (PND) and selective abortion based on which countries with high incidence of thalassemia like Italy, Greece and Cyprus have significantly reduced the number of thalassemia cases (5, 6). In line with the above objectives, a couple of studies have been conducted since 1993 to determine the country’s widespread mutations with the goal of investigating the possibility of PND in Iran. It should be noted that until early 1996, the samples would be sent abroad and thereafter PND was initiated first in Iran Pasteur Institute and then was followed in some medical sciences universities and in some private institutions inside the country. Meanwhile, the Iranian Thalassemia Association was established and some activities were carried out in relation to blood and medicine supply in addition to research on thalassemia. In this regard, the Iranian Ministry of Health and Medical Education established centers for PND in highly prevalent thalassemia provinces in the country; Zahedan PND of thalassemia center was established in 2002. The statistics provided by National Thalassemia Committees indicate that the number of new cases of thalassemia in Iran after the implementation of screening strategies and the establishment of PND centers resulted in a 70% reduction in the expected annual birth rate of thalassemia cases (7). Sistan and Baluchistan province with a ratio of 1 to 27 of Iranian population hosts a high rate of about 25% (70 cases) of new cases of Iranian thalassemia each year. The number of new cases in provinces that historically had even more incidences of thalassemia than Sistan and Baluchistan province has reduced by observing the national protocols for thalassemia prevention, leaving them in a better position.
Although Iranian Ministry of Health prevention strategies have led to a significant reduction in the number of new thalassemia patients in many provinces, unfortunately 601 major cases were added to the thalassemia population in Sistan and Baluchistan province in spite of carrying out accountable number of PND of thalassemia on at-risk couples between 2002–2010. This study aimed at identifying the occurrence causes of new thalessemic patients in Sistan and Baluchistan province, Iran.
Materials and Methods
This retrospective cross-sectional study was conducted on all the children with major thalassemia who were born after the establishment of PND Center in Sistan and Baluchistan province, south-east of Iran in 2002.The study protocol was approved by the ethic committee of the deputy of research in Zahedan University of Medical Sciences. The requested data was collected using a developed questionnaire and from the information in the hospital records of patients. The standardization of the questionnaire was initially performed on 15 thalessemic parents in two stages with a one-month interval, and after confirmation of the questions, the study proceeded.
Thereafter and in the first stage, a list was developed of all the children who were born after 2002 with major thalassemia and who had been referred to thalassemia centers for blood transfusions in all districts of the province. At the time of each child’s appointment for blood transfusion, the parents were interviewed, and their answers to the questionnaire were recorded in the forms.
After completion of the questionnaires and coding them, the data were entered into a data bank and were analyzed by SPSS, version 15. The descriptive statistics were used to express the central indices (mean, variance, and median), frequency index (standard deviation, range) as well as percentage. The collected information was coded, and the anonymity of samples was preserved.
Results
This study evaluated 601 children under 8 years of age who were diagnosed with major thalassemia. The average age of fathers with major thalassemia children was 35.6±9 years, and that of mothers was 29.6±7 years. Every 27.4±4.7 days, the patients received 211.1±74.36 ml of blood on average. The fathers of 96.6% and the mothers of 98.6% of major thalassemia children were still living. In the study population, 83.1% of major thalassemia children’s parents had consanguineous marriages. In among major thalassemia 90.5% of children born were associated with the Balouch tribe, 8% with Sistani and 1.5% with the ethnic groups.
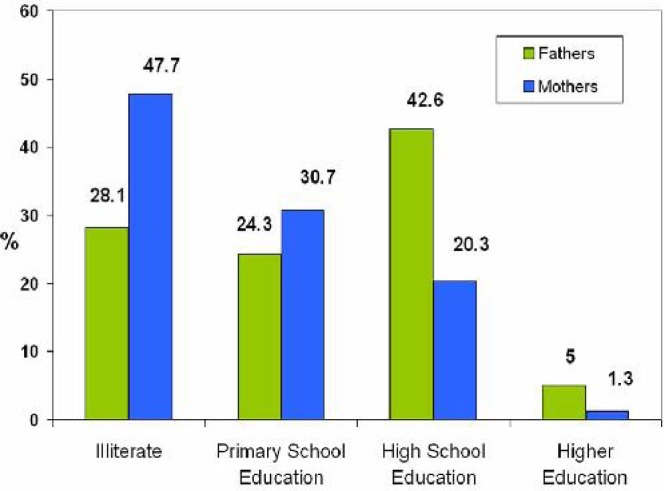
About 52.4% of fathers and 78.4% of mothers had elementary education and less (Fig. 1). With 43.8%, blood group O of the ABO system had the highest frequency in major thalassemia children. In addition, 91.1% of the patients had antigen D of the Rh system, that is, only 8.3% of major thalassemia children lacked the antigen D.
Fig. 1:
Parental education level of children suffering from major thalassemia who were born after starting Prenatal Diagnosis Center of thalassemia in Zahedan, capital of Sistan & Baluchistan province in Iran (2002)
Of all couples, 22.3% had one or more major thalessemic children (19.3% had one, 3% had two and 1% had three affected children). Of the families studied, 4.1% had dead thalassemia children, 22.3% of all couples had between one to three thalessemic children in those with first cousin relationship and 21.9% had between one to eight thalessemic children in the second cousin relationship.
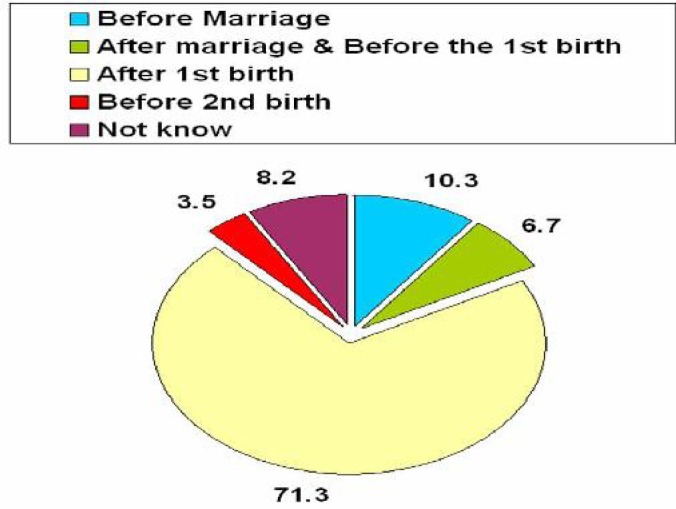
At the time of their marriage, 78.6% of the studied couples had not undergone premarital screening for thalassemia (PST) which includes tests measuring CBC and HbA2. In addition a full 70.4% of all couples had not been notified about their own minor thalassemia after the birth of their child with major thalassemia (Fig. 2).
Fig. 2:
Time of attitude being minor in couples whose affected children were born after Starting Prenatal Diagnosis Center of Thalassemia in Zahedan, capital of Sistan & Balouchestan province in Iran (2002)
Meanwhile, of the couples who had been diagnosed to be minor thalessemic and introduced to PND Center, 50.9% did not refer to the center due to lack of awareness about the gestational age, unwillingness of husband and relatives, and lack of awareness about the importance of the issue. Of the couples who were introduced to the center, 25% did not return for Chronic Villous Sampling, the second stage of prenatal diagnosis, due to financial problems and unawareness of the sever consequences of their decision.
Discussion
The soaring costs of health and treatment, and social and psychological problems in addition to sever medical complications of major thalassemia patients due to the absence of absolute treatment have caused thalassemia to be considered the most important problem of the health system in high-frequency regions. The screening, counseling and PND approaches have resulted in significant reduction in the incidence of new cases of thalassemia in some countries, including Iran. The results of this study indicated that absence of PST, and unawareness of the importance of prevention by using PND because of financial problems and a misconception of the sever consequences of refusing to follow the procedures are the most important causes of new cases of thalassemia in south-east of Iran despite the fact that there are significant numbers of PND of thalassemia.
The results showed that about 80% of parents of the children studied are married under no official registration and without PST. In minor couples in each pregnancy there is a 25% chance of their giving birth to affected child. And so, over 80% of these couples enjoy consanguineous marriages and since mothers in this region have multiple pregnancies (usually more than three pregnancies), thalessemic children chance is an estimate of 100%. Unfortunately, the trend of consanguineous marriages is more prevalent in rural areas, and the number of carrier couples who have not passed the basic PST is continually increasing, which means they are likely be notified about their own minor thalassemia several years later, after the birth of a major thalassemia child. Therefore, it seems that in the first step the clerics who venture to wed should be trained regarding the importance of premarital tests and prevention approaches, including PND. These trainings will allow the screening strategies to be performed better and if the couples have religious questions about the abortion they will face more appropriate responses by the clergymen. And as the second important step, the personnel of rural and urban health centers that are responsible for antenatal care should be provided with the necessary training on thalassemia screening tests so as to offer counseling and educate couples so that the basic stage of screening can be carried out; then, if required, higher levels of diagnosis can be extended during the first three months of pregnancy by a university thalassemia counselor.
The results of this study showed that only 50% of parents diagnosed with minor thalassemia had referred to the center for the first stage of PND, and 25% of couples referred to the center at this stage had not returned for the second stage of diagnosis. The absence of awareness among mothers regarding gestational age, the unwillingness of the husbands, lack of awareness among mothers on the importance and sever consequences of the issue, and financial problems were among the most important reasons for not referring to the center. The persistence of major thalassemia in Sicily between 1990 to 1996 were mainly due to poor information about prevention programmers, laboratory error, undergoing screening for thalassemia or refusing to take selective abortion of affected cases and difficulty of the diagnosis of minor thalassemia (8). The contraception methods used by couples before and after having thalassemia children did not change significantly. Since approximately 40% of pregnancies were unwanted, also 60% of couples expressed interest in future pregnancies despite having thalassemic children, more focus on education of secure prevention method and gestational age control is vital. However, the current workload of personnel in the thalassemia sector makes it impossible, and this issue requires the recruitment of experienced local midwives who are familiar with Balouch culture (over 90% of patients 6.
Unfortunately, massive budgets are being spent annually for the preparation of posters and educational pamphlets that are not appropriate in terms of the literacy level of the target group. Therefore, regarding the education level of mothers and fathers, it is necessary to use training methods appropriate to the literacy level, so, repetition and perseverance are essential. In this regard, suitable advertisements in the local dialects can be used through provincial TV networks to widely train the populace on the subject. Dehkordi et al found out that using booklets and combined educational methods (lecture, video, and etc) for parents about thalassemia had a significant effect in the prevention and consequences of the disorder (9).
Conclusion
The most important causes of new cases of major thalassemia in Sistan and Baluchistan Province include failure of PST and unawareness of PND importance and process. With appropriate planning for each of the above issues, we can be hopeful about reducing the new incidence of cases of thalassemia in short term.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
We appreciate the Research and Technology Deputy of Zahedan University of Medical Sciences for funding this project as well as Deputy of Health in the University and all the children with thalassemia and their families who assisted us in the course of the project implementation. We also would like to wholeheartedly thank Mr. Abdurrashid Khazaei Feizabad for reading the manuscript for possible linguistic problems. This article is the outcome of the approved project No. 88-1198. The authors declare that there is no conflict of interest.
References
- 1.Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010;5:11–25. doi: 10.1186/1750-1172-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weatherall D, Clegg J. The β-thalassemia syndromes. Oxford: Blackwell Scientific publication; 2001. [Google Scholar]
- 3.Habibzadeh F, Yadollahi M, Merat A, Haghshanas M. Thalassemia in Iran an overview. Arc Iranian Med. 1998;1:27–33. [Google Scholar]
- 4.Miri-Moghaddam E, Zadeh-Vakili A, Rouhani Z, Naderi M, Eshghi P, Khazaei Feizabad A. Molecular basis and prenatal diagnosis of beta-thalassemia among Balouch population in Iran. Prenat Diagn. 2011;31:788–91. doi: 10.1002/pd.2767. [DOI] [PubMed] [Google Scholar]
- 5.Cao A, Rosatelli MC, Galanello R. Control of beta-thalassaemia by carrier screening, genetic counselling and prenatal diagnosis: the Sardinian experience. Ciba Found Symp. 1996;197:137–51. doi: 10.1002/9780470514887.ch8. [DOI] [PubMed] [Google Scholar]
- 6.Cao A, Rosatelli MC, Monni G, Galanello R. Screening for thalassemia: a model of success. Obstet Gynecol Clin North Am. 2002;29:305–28. doi: 10.1016/s0889-8545(01)00006-7. [DOI] [PubMed] [Google Scholar]
- 7.Samavat A, Modell B. Iranian national thalassaemia screening programme. BMI. 2004;329:1134–7. doi: 10.1136/bmj.329.7475.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romeo MA, Di Gregorio F, Russo G. Persistence of Mediterranean anaemia in Sicily. J Med Genet. 1997;34:869–70. doi: 10.1136/jmg.34.10.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dehkordi AH, Heydarnejad MS. Effect of booklet and combined method on parents’ awareness of children with beta-thalassemia major disorder. J Pak Med Assoc. 2008;58:485–7. [PubMed] [Google Scholar]