Abstract
Background
The aim of this study was assessment the risk management status of waste anesthetic gases in academicals hospitals in Iran to prevent from harmful effects of these gases on employees’ health.
Methods:
A descriptive-analytic study was designed in 2011. Standard structured checklist developed by ECRI institute (Emergency Care Research Institute) was applied. Checklists were filled onsite through direct observation and interviews with anesthesia personnel in 46 operating rooms at 4 hospitals from all of the hospitals under affiliation of Isfahan University of Medical Sciences. These hospitals were selected based on the number of surgical beds.
Results:
Total means score of WAGs risk management status was 1.72 from the scale of 3. In the studied operating rooms, only 28% complied with predetermined standards, 16% needed improvement and 56% had no compliance. Total mean scores of compliance in planning, training and evaluation and monitoring of waste anesthetic gases were weak and equipment and work activity was at medium level.
Conclusion:
The risk management status of waste anesthetic gases in the hospitals to be weak, therefore operating room personnel are exposed to medium to high level of these gases. The hospital mangers should prepare and apply scavenging equipment, development of control program, quality improvement, risk management and maintenance of anesthesia equipment. Finally, ongoing monitoring and evaluation, education to personnel and modification of policy and procedures and improvement of work activities should be considered.
Keywords: Risk management, Waste anesthetic gas, Assessment
Introduction
All operating-room personnel are continuously exposed to trace concentrations of anesthesia agents. Inhalation gases and vapors that leak into the workplace due to medical and research procedures are defined as waste anesthetic gases (WAGs) (1). These gases may leak from the patient’s anesthesia breathing circuits because of malabsorption of gases ventilated into patient’s lungs during anesthesia. In addition small amounts of volatile anesthetic gases leak from anesthesia machines because the anesthesia machines are not airtight (2). WAGs may be exhaled by patients recovering from anesthesia in the postanesthesia care unit. Anesthesia agents are lipid soluble so those agents eliminated through exhalation without being metabolized in the patient body and the anesthesia machines transfer these gases very slowly into the surrounding without any changes (3, 4).
Waste anesthetic gases including both nitrous oxide and halogenated anesthetics (halothane, enflurane, isoflurane, desflurane, sevoflurane, and methoxyflurane) that over-exposure of them, may produce health effects and hazards to operating-room personnel. Anesthesiologists, surgeons, dentists, nurse anesthetists, operating-room nurses, operating-room technicians, recovery-room nurses and other operating-room personnel are exposed to these gases (5). Gas exposure and its effects is based on concentration of agent, measured in parts per million (ppm), and length of time the exposure (6). Despite a few number of studies that show no effects of anesthetic gases on the health (7) many studies demonstrated that there was a causes-and-effect relationship between health problems and being exposure to waste anesthetic gases. Based on these result, exposure to excess amounts of these gases, even for a short time, may create short-term and long-term effects on personnel health. Short-term symptoms are including drowsiness, headache, irritability, fatigue, nausea, drowsiness, poor judgment and loss of coordination. Tran. N and et.al in 2000, Showed when personnel leave workplace, symptom of fatigue disappears (8). Chronic symptoms of over-exposure can include reproductive effects, kidney and liver diseases. Rogers B. in 1986, showed that exposure to high levels of WAGs can cause cellular, mutagenic, carcinogenic, teratogenic effects and miscarriages in spouses of exposed workers or birth defects in their offspring. The Similar result of a case-control study indicated that incidence of cancer, renal and hepatic disease, infertility, congenital abnormalities and premature births, in the exposed group are higher than non-exposed group (9).
American Society of Anesthesiologists (ASA) and the National Institute for Occupational Health and Safety (NIOSH) are concerned about adverse effects of trace anesthetic gases. So, performed commonly many studies for exploration of adverse heath effect in operating rooms workers, whose that were exposure WAGs (10). The goal of these organizations is quantify the consequences of waste anesthetic gas exposure through standards and recommendations to prevention, control and reduction of release WAGs, measurement, monitoring, scavenging and workplace practices.
As was said, waste anesthetic gases are having adverse effects on health of employees. Beyond all of the studies in this subject, several studies (11, 12) discussed about ecological and cost benefit of WAGs control. Ishizawa Y, in a review study in 2011, discussed about potential effects of general anesthetic gases on global environment. He said halogenated agents and nitrous oxide could have potential significant effects on global warming and these are recognized as greenhouse gas or important ozone depleting gas. Ishizawa described alternatives ways and new technologies that may prevent from emission of these gases into the atmosphere (4). Also, they indicated that reduction of flow anesthesia gases techniques has economic benefits and reduce the costs of volatile anesthesia. Results showed that reduction of fresh gas flow as 2.0 L/min, lead to saving 50% of the total consumption of any volatile anesthesia agent (13–15). Techniques of low flow anesthesia not only provide economical and ecological benefit, it can improve the quality of patient care too. Because the low flow of anesthesia agents frequently, keeps them moist (16).
All of mentioned issues illustrate the importance of a comprehensive realization from the management of waste anesthetic gases as a major element. So employers, hospital managers and operating room personnel should be aware the potential risks of WAGs and be use recommended guidelines for reduction of exposures. So, the aim of the present this study is assessment the risk management status of waste anesthetic gases in academicals hospitals in Iran to identify deficiencies and problems, provide solutions and planning to prevent from harmful effects of these gases on employees’ health, also ecological and cost effects.
Materials and Methods
A descriptive-analytic study was designed in 2011 to assess the risk management of waste anesthetic gases in Iranian academic hospitals. Instrument for data collection was a structured standard checklist that had been developed by ECRI institute (Emergency Care Research Institute) in November 2007 (17). ECRI institute is an independent nonprofit organization whose mission is to benefit patient care by promoting the highest standards of safety, risk control, quality and cost-effectiveness in healthcare. They accomplish this through our research, publishing, education and consultation. Goal of this institute is to be the world’s most trusted, independent, organization providing healthcare information, research, publishing, education and consultation to organizations and individuals in healthcare (18). The standards of this institute are gathered from important standards and guidelines of American Association of Nurse Anesthetists (AANA), American Society of Anesthesiologists (ASA), and Joint Commission. This checklist will assess the status of risk management of waste anesthetic gases in areas of the anesthesia department that are exposed to a high WAGs. This checklist is including 36 questions about WAGs risk management and assesses the hospitals based on the five dimensions including planning, training, equipment, evaluation and monitoring, work practices in this subject. Validity of checklist was approved through consultation with anesthesia specialists. Content of checklist was compiled with statues of Iranian hospital operating rooms. Our study population, were the hospitals of Isfahan University of Medical Sciences. Four hospitals (Alzahra, Amin, Kashani, Nour and Ali Asghar) affiliated to Isfahan University of Medical Sciences selected as sample referred as A, B, C, and D in the text.
Inclusion criteria of the study were the number of surgical beds. The numbers of elective surgeries beds in these hospitals were more than other hospitals. Mental hospitals and hospitals to perform special surgeries were excluded from the study. Therefore popularization of results to all of Isfahan University hospitals is possible. In other that hospitals agreement with collection of data, hospital administrators were justified than importance of this research. In the next, the researcher directly was referred to surgery departments in hospitals. Checklists were filled through direct observation, interviews with operating room managers, anesthesiologists and anesthesia technicians in 46 operating rooms of four hospitals. Each room surveyed for six consecutive days in one week.
Using descriptive statistics the qualities data converted to quantities data and then these compare together. Total score 3 was selected for excellence status of WAGs risk management in hospitals. Score 1–2 introduced as weak status, score 2–2.5 showed the medium level and 2.5–3 score as a good status. Collected data were analyzed in five dimensions and expressed as means and percentile. Then, the statistical comparisons to assess significant difference in variables between hospitals were done. To statistical analyses one-way ANOVA was used. SPSS statistical program was used for performance all statistical analyses. Version 16 was applied in this study. P-value less than 0.05 were defined as the level of statistically significance. The authors had full access to the data and take responsibility for its integrity.
Results
Descriptive statistical according to standards of ECRI institute showed in Table 1–3.
Table 1:
The means of WAGs risk management status in Isfahan teaching hospitals
| Hospitals | |||||
|---|---|---|---|---|---|
| A | B | C | D | P-value | |
| Mean | 1.91 | 1.80 | 1.61 | 1.58 | 0.316 |
| Total mean | 1.72 | ||||
Table 3:
The means of WAGs risk management status stratified by subsets in Isfahan teaching hospitals
| Subset | Hospitals | ||||
|---|---|---|---|---|---|
| A | B | C | D | Total | |
| Planning | 1 | 1 | 1 | 1 | 1 |
| Training | 2.20 | 2 | 1.80 | 1.80 | 1.95 |
| Equipment | 2.14 | 2 | 2 | 2 | 2.03 |
| Evaluation & monitoring | 1.16 | 1 | 1 | 1 | 1.04 |
| Work practices | 2.38 | 2.30 | 1.84 | 1.76 | 2.07 |
Table 1 indicates that the mean score of WAGs risk management in four hospitals (Alzahra, Amin, Kashani, Nour and Ali Asghar) was respectively, 1.91, 1.80, 1.61 and 1.58 that referred as A, B, C, and D in the text. Total score was 1.72. Moreover, analytical statistics showed no significant difference between mean of WAGs risk management status in four hospitals.
The percentile of WAGs risk management status in Isfahan teaching hospitals is shown in Table 2.
Table 2:
The percentile of WAGs risk management status in Isfahan teaching hospitals
| Grade | |||
|---|---|---|---|
| Hospitals | Yes (%) | N/I (%) | No (%) |
| A | 31 | 19 | 50 |
| B | 33 | 25 | 42 |
| C | 25 | 11 | 64 |
| D | 25 | 8 | 67 |
| Total | 28 | 16 | 56 |
Classification of hospital based on the predetermined standards showed that the mean of compliance standards is higher in A hospital than other hospitals. In the all of considered hospitals only 28% of standards were complied with predetermined standards, 16% needed improvement and 56% had no compliance. Needs improvement is defined as when planning was not exactly or implementation was not accurately (Table 2).
The means of WAGs risk management status stratified by subsets indicated in table 3. Comparison of classified standards based on planning, training, equipment, evaluation and monitoring, work practices showed that no significant differences were observed between studied hospitals.
Total mean scores of planning, training, equipment, evaluation and monitoring, practices performance were respectively 1, 1.95, 2.03, 1.04 and 2.07. Overall, based on the total score in table 3, work practices had higher score (2.07) that other sections and standards related to equipment with 2.03 score, put in the next place. Planning had the lower score (1).
In A hospital, training, equipment, evaluation and monitoring and work practices had higher score.
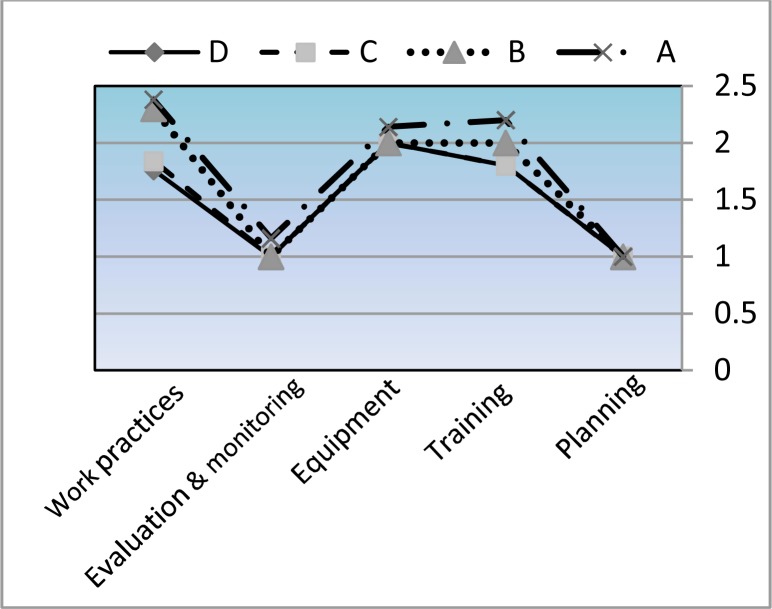
Figure 1 shows that the status of WAGs risk management in all of hospital have a similar pattern. This figure indicates that the total status is weak in planning, training, evaluation and monitoring. Only equipment and work activities are in medium level. Also this figure indicates that A hospital only in training (2.20), equipment (2.14) and work activates (2.38) and B hospital only in work activities (2.30) are in medium level. Hospitals in other situations were weak.
Fig. 1:
Pattern of WAGs risk management status stratified by subsets in Isfahan teaching hospitals
Discussion
Exposure to waste anesthesia gases cannot be eliminated, but it can be monitored and controlled (19). Trace concentration of WAGs can help to reduce amount of these agents below the standard levels that recommended by NIOSH, OSHA (20).
According to the results of our study, the risk management status of waste anesthetic gases in studied hospitals is very weak. Therefore, we can expect that the operating room personnel to be exposed a lot of waste anesthetic gases during sequential surgeries. As regards that no significant difference was observed between four hospitals. So, WAGs risk management status is almost similar to each other. The results of this study indicated that planning for reduction of waste anesthetic gases is so weak. Based on surveyed standards in our study, the causes of this matter are: lack of policies and procedures for the control of waste anesthetic gases, deficiency of documented program for maintenance anesthesia equipment and scavenging systems and privation of formal program for testing for waste anesthetic gases in gas lines and vacuum lines. Other studies approved the results of our study. Major sources of anesthetic gas pollution are due to the lack of adequate engineering control systems and the poorly maintained anesthesia equipment (21).
Approximately 91 to 95 % of waste gas concentrations in the operating rooms were cause to incorrect and careless work practices (22). Indeed, even by use of scavenging systems, anesthetic gases were discovered in operating rooms and workers were exposed to these gases. Because, the scavenging is not able that covered the realization of trace anesthetic gases from other parts of machines. Where gases exhaled by recovering patients are not properly controlled by personnel is most likely to be exposed to waste anesthetic gases. This subject reveals that for the control of WAGs, scavenging is not sufficient and additional engineering controls are necessary. Thus, one of reasons emission of WAGs is poor work practices of personnel (21). These are including that connectors, tubing and valves are not maintained and tightly connected, WAGs are not properly vented or scavenged, patients mask or endotracheal coupling is not probably fitted during induction of anesthesia and disconnection of the system (19).
Mean score of work practices in our study showed a medium level but this score is not sufficient and for reach to excellent level, further efforts are necessary. For reach this aim, scavenging practices and recommended guideline should be applied and a follow up survey to approve accuracy of them should be done in the future time. Li SH and et al, indicated malfunction, loose connection or disconnection between the anesthetic machine and the exhaust venting system of operating theater almost doubled the N2O concentrations (23). So, reform of work practices and maintenance of correct performance of scavenging system and connectors can help to minimization the concentrations of waste anesthetic gases in surrounding.
The total mean score of training as one of aspects in control of waste anesthetic gases was in low level. Causes are loss of formal continuing education programs in improvement of work practices, recognition of damaged equipment, policies and procedures to usage of devices for medical and non-medical personnel.
In addition, based on result of our study, preparation and check equipment is at medium level. This issue illustrates that performances of equipment are not accurate and so necessary emprise to promotion of safety and reduction of emission risk should be established and therefore, usage from properly facilities for remove of waste gases should be available.
Evaluation and monitoring as other surveyed aspect of WAGs risk management was at weak status. Because the waste anesthetic gas levels in all anesthetizing locations not been surveyed during the last year. Exposure levels not monitored at least quarterly and any documents not exist in place. Director of anesthesia services not reviewed the policy for quality improvement and risk management in waste anesthetic gases. Based on the standards of our study operating rooms should be reviewed once in a year by the risk manager or the chief of anesthesia and the clinical engineer responsible for maintaining the anesthesia equipment. Additional review should be considered when significant organizational changes such as the introduction of new procedures, facility changes, equipment changes and new guidelines or practices are happen.
Other studies confirm the importance of this subject. So, based on the recommendations, leaking of all anesthesia equipment should be tested daily (6) and follow up survey would be carried out at a later date (6, 24).
In the all of considered hospitals only 28% of standards complied with predetermined standards. 16% of needed improvement and surprisingly, 56% had no compliance. So it can be causes to lack of application planning and guidelines, false procedure, shortage of monitoring and evaluation programs.
Total mean scores of planning, training, evaluation and monitoring were weak too. So, risk management of waste anesthetic gases should be emphasized on planning, training, evaluation and monitoring in academic hospitals. This does not mean that modification and reform in these aspects are sufficient only. But we need that upgrade of work practices and improvement the procedures. Also, the types of facility and equipment to reach to excellent level are inevitable.
Conclusions
In general, our study conclude that the best means for controlling anesthetic gas concentration is usage a comprehensive, viable and effective system for management of waste anesthetic gases. WAGs risk management status were almost similar in Isfahan University of Medical Sciences hospitals and were week. Thus, unit strategy and policy for achieving to excellent level and coordination between hospitals on behalf of organizations related is helpful.
Conclusion of our study offers major pathways and policies for WAGs risk management based on the standards of ECRI institute. Firstly, preparation of equipment to scavenging of these agents or entrap waste anesthetic gases and vented these gases to outside air by devoted suction is recommended. Secondly, management system should be including development of program for control of WAGs, maintenance of anesthesia equipments, quality improvement and risk management. Thirdly, education to personnel in working with anesthesia cars and doing right tasks should be delivered. Fourthly, ongoing monitoring and evaluation for checking systems to exploration of leakage, air monitoring and medical surveillance should be performed. Finally, work practice controls, personal protective equipment, modification of procedures to improvement of activity should be considered.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
The authors would like to acknowledge and appreciate from all of studied hospitals managers and other participants in interview that help to get the object of this research. The authors declare that there is no conflict of interest.
References
- 1.Foley K. Occupational exposure to trace anesthetics: quantifying the risk. AANA J. 1993;61(4):405–412. [PubMed] [Google Scholar]
- 2.Anesthetic gases: guidelines for workplace exposure. US Department of Labor, Occupational Safety and Health Administration, Office of Science and Technical Assessment. Available from: http://www.osha.gov/dts/osta/anestheticgases/inex.html. Accessed January 25, 2010.
- 3.Frederick E Sieber. Geriatric anesthesia. McGraw-Hill Medical; New York: 2006. p. 92. [Google Scholar]
- 4.Ishizawa Y. Special article: general anesthetic gases and the global environment. Anesth Analg. 2011;112(1):213–217. doi: 10.1213/ANE.0b013e3181fe02c2. [DOI] [PubMed] [Google Scholar]
- 5.Anonymous . Waste anesthetic gases, occupational hazard in hospital, CDC, workplace safety and health. 2007. [Google Scholar]
- 6.Ronaldd D Miller, Roy F cucchiAra, Edvard D miller, et al. Anesthesia. 4th ed. Vol. 4. Churchill livingstone; 1994. pp. 2681–2682. [Google Scholar]
- 7.Anton G L Burm. Occupational hazards of inhalational anaesthetics. Best Practice and Research Clinical Anaesthesiology. 2003;17(1):147–161. doi: 10.1053/bean.2003.0271. [DOI] [PubMed] [Google Scholar]
- 8.Tran N, Elias J, Rosenberg T, Wylie D, Gaborieau D, Yassi A. Evolution of waste anesthetic gases, monitoring strategies, and correlations between nitrous oxide levels and health symptoms. Am Ind Hyg Assoc J. 1994;55(1):36–41. doi: 10.1080/15428119491019249. [DOI] [PubMed] [Google Scholar]
- 9.Moeen K Panni, Stephen B Corn. The Use of a Uniquely Designed Anesthetic Scavenging Hood to Reduce Operating Room Anesthetic Gas Contamination During General Anesthesia. Anesth Analg. 2002;95:656–660. doi: 10.1097/00000539-200209000-00030. [DOI] [PubMed] [Google Scholar]
- 10.McGregor DG., MBBS, FRCA Occupational exposure to trace concentration of waste anesthetic gases. Mayo Clin Proc. 2000;75:273–277. doi: 10.4065/75.3.273. [DOI] [PubMed] [Google Scholar]
- 11.Susan M Ryan, Claus J Nielsen. Global Warming Potential of Inhaled Anesthetics: Application to Clinical Use. International Society for Anaesthetic Pharmacology. 2010;111(1):92–98. doi: 10.1213/ANE.0b013e3181e058d7. [DOI] [PubMed] [Google Scholar]
- 12.Kole TE. Environmental and occupational hazards of the anesthesia workplace. AANA J. 1990;58:327–331. [PubMed] [Google Scholar]
- 13.Miller RD. Anesthesia. 5th ed. Churchill Livingstone; 1999. pp. 74–95. Ch. 4, [Google Scholar]
- 14.Cotter SM, Petros AJ, Dore CJ, Barber ND, White DC. Low flow anaesthesia. Practice, Cost implications and acceptability. Anaesthesia. 1991;46:1009–1012. doi: 10.1111/j.1365-2044.1991.tb09910.x. [DOI] [PubMed] [Google Scholar]
- 15.Feiss P, Demontoux MH, Colin D. Anesthetic gas and vapor saving with minimal flow anesthesia. Acta anaesthesiol Belg. 1990;41:249–251. [PubMed] [Google Scholar]
- 16.Weiskopf RB, Eger EI. Comparing the costs of inhaled anesthetics. Anesthesiology. 1993;79:1413–1418. doi: 10.1097/00000542-199312000-00033. [DOI] [PubMed] [Google Scholar]
- 17.ECRI Institute (Meeting the needs of European Health care) Health care risk control, Anesthesia department. [Resource on the ECRI] Available from: http://www.ecri.org. Accessed November, 2007.
- 18.ECRI Institute (Mission and vision) [Resource on the ECRI] Available from: http://www.ecri.org.uk/about-ecri.htm/. Accessed 1955.
- 19.Duval Smith F. Management of Exposure to Waste Anesthetic Gases. AORN Journal. 2010;91(4):482–494. doi: 10.1016/j.aorn.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 20.McGregor DG, Senjern DH, Mazze RI. Trace nitrous oxide levels in the postanesthesia care unit. Anesth Analg. 1999;89:472–475. doi: 10.1097/00000539-199908000-00042. [DOI] [PubMed] [Google Scholar]
- 21.Potts DL. Occupational exposure of veterinarians to waste anesthetic gases. University of Utah. 1987:62–87. [Google Scholar]
- 22.Whitcher CE, Cohen EN, Trudell JR. Chronic Exposure to Anesthetic Gases in the Operating Room. Anesthesiology. 1971;35:348. doi: 10.1097/00000542-197110000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Li SH, Li SN, Shih HY, Yi HD, Chiang CY. Personnel exposure to waste sevoflurane and nitrous oxide during general anesthesia with cuffed endotracheal tube. Acta Anaesthesiol Sin. 2002;40(4):90–185. [PubMed] [Google Scholar]
- 24.McGregor DG. Task Force on Trace Anesthetic Gases; Committee on Occupational Health of Operating Room Personnel. Trace anesthetic gases in the operating room. ASA Newsletter. 1997. p. 61. Available from: http://www.asahq.org/Newsletters/1997/05_97/Trace_Gases.html. Accessed December 31, 2009.