Abstract
Background/aim
To assess the impact of open versus laparoscopic surgery in cirrhotic patients undergoing a cholecystectomy using the Nationwide Inpatient Sample (NIS).
Methods
All patients with cirrhosis who underwent a cholecystectomy (open or laparoscopic) between 2003 and 2006 were queried from the NIS. Associated complications including infection, transfusion, reoperation, liver failure and mortality were determined.
Results
A total of 3240 patients with cirrhosis underwent a cholecystectomy: 383 patients underwent an open cholecystectomy (OC) whereas 2857 patients underwent a laparoscopic cholecystectomy (LC), which included 412 patients converted (LCC) from a LC to an OC. Post-operative infection was higher in OC as opposed to a laparoscopic cholecystectomy (TLC) or LCC (3.5% versus 0.7% versus 0.2%, P < 0.0001). The need for a blood transfusion was significantly higher in the OC and LCC groups as compared with the TLC group (19.2% versus 14.4% versus 6.2%, P < 0.0001). Reoperation was more frequent after OC or LCC versus TLC (1.5% versus 2.5% versus 0.8%, P = 0.007). In-hospital mortality was higher after OC as compared with TLC and LCC (8.3% versus 1.3% versus 1.4%, P < 0.0001).
Conclusion
Patients with cirrhosis have increased in-hospital morbidity and mortality after an open as opposed to a laparoscopic or conversion to an open cholecystectomy. LC should be the preferred initial approach in cirrhotic patients.
Introduction
A laparoscopic cholecystectomy (LC) is the standard approach in treating benign gallbladder diseases. The advantages of LC over an open cholecystectomy (OC) are well established and documented. More than 700 000 operations are performed each year with satisfactory results.1 While LC has become the standard treatment for symptomatic cholelithiasis, it is not always the first choice undertaken by surgeons in cirrhotic patients with calculus biliary tract disease. The incidence of gallbladder disease in cirrhotic patients is more than double that for non-cirrhotic adults.2–10 As the number of cirrhosis cases in the US is on the rise, more biliary tract operations in cirrhosis patients will be performed.3–6,9,10 Therefore, a verified and uniform approach to the selection of treatment modalities in this group of patients must be established. This will undoubtedly lead to a better understanding and reduction of complications seen in cirrhosis patients.
The definitive treatment of decompensated cirrhosis is liver transplantation. While the number of donors remains limited, the number of patients living with cirrhosis continues to increase. This trend will lead to an increase in co-morbid conditions including biliary tract disease.11 Factors implicated in the higher incidence of gallstone formation include hypersplenism, increased levels of oestrogen, and increased intravascular haemolysis with a reduction in gallbladder emptying and motility.10
Surgical literature throughout the 1980s has uniformly reported discouraging results when biliary surgery was attempted on cirrhotic patients.3,4,8,9,12,13 In 1992, the National Institute of Health (NIH) consensus statement on LC defined those with end-stage cirrhosis with portal hypertension to be poor candidates for LC.14 Surgeons were reluctant to attempt LC in patients with cirrhosis owing to its perceived complications and practical inexperience with LC. Since then, multiple authors have identified and reported advantages of LC over OC in this particular group of patients, leading the way for a more regular use of this minimally invasive procedure. Still, no uniform consensus has been established in studies and in the surgical community in reference to the procedure selection in cirrhotic patients.
The purpose of this study was to assess the impact of surgical approach selection in cirrhotic patients undergoing a cholecystectomy on the outcome using the Nationwide Inpatient Sample (NIS). This is the largest population-based and geographically representative all-payer database of hospital discharges in the US.
Methods
Data source
This retrospective cohort study examined the outcomes of a cholecystectomy in cirrhosis patients using discharge data from the Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), and Agency for Healthcare Research and Quality. The NIS is the largest all-payer inpatient care database in the US, which contains about 20% of stratified samples of U.S. community hospitals. The stratification is based on five hospital characteristics: geographical region (Northeast, Midwest, West and South), control [government non-Federal (public), private not for profit (voluntary) and private investor-owned (proprietary)], location (urban or rural), teaching status (teaching or non-teaching) and bed size (small, medium and large). It contains data from about 8 million hospital stays each year.
Diseases and procedures of interest
The population of interest was all adult patients (age ≥18 years) with cirrhosis who underwent a cholecystectomy (OC or LC) between 2003 and 2006. The disease status and procedures were categorized according to the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM).
Groups with ICD-9-CM codes
All patients with a primary diagnosis of calculus of the gallbladder (ICD-9-CM codes: 574.00, 574.01, 574.10, 574.11, 574.20, 574.21) and a primary procedure of an OC (ICD-9-CM codes: 51.22) or LC (ICD-9-CM codes: 51.23), with the secondary diagnosis of cirrhosis (ICD-9-CM codes: 571.2, 571.5, 571.6) were included in this study. Some patients with a LC had conversion to an OC (ICD-9-CM codes: v64.4, v64.41). A summary of the ICD-9-CM codes used is summarized in Table 1.
Table 1.
ICD-9 codes used in this study
| Calculus of gallbladder | 574.00, 574.01, 574.10, 574.11, 574.20, 574.21 |
| Cirrhosis | 571.2, 571.5, 571.6 |
| Laparoscopic cholecystectomy | 51.23 |
| << conversion to open >> | V64.4, V64.41 |
| Open cholecystectomy | 51.22 |
| Postoperative infection | 998.1, 998.59, 682.2, 567.22 |
| PRBCs blood transfusion | 99.03, 99.04 |
| Post-operative haemorrhage | 998.1, 998.11, 998.12 |
| Reoperation | 54.12, 39.98 |
| Liver failure | 570, 572.2, 572.4 |
| Ascites | 789.5 |
| Portal hypertension | 456.0, 456.1, 456.20, 456.22, 572.3 |
Outcome variables
The primary outcome for this study was in-hospital mortality. The post-operative complications were also outcomes of interest, including: post-operative infection (ICD-9-CM codes: 998.1, 998.59, 682.2, 567.22), ascites (ICD-9-CM codes: 789.5), packed red blood cells transfusion (ICD-9-CM codes: 99.03, 99.04), post-operative haemorrhage (ICD-9-CM codes:998.1, 998.11, 998.12), reoperation (ICD-9-CM codes: 54.12, 39.98) and liver failure (ICD-9-CM codes: 570, 572.2, 572.4).
Statistical analysis
The weighted number of procedures and rates were calculated to take into consideration the stratified sampling design of NIS data. Patient characteristics were summarized using means, standard deviations (SDs), frequencies and percentages. Wilcoxon's rank sum test was used to compare the age distributions between the groups. The Rao–Scott chi-square test was used to compare discrete variables between or among groups. Multiple logistic regression models were used to assess the association between types of procedures and in-hospital mortality while controlling for potential confounding variables. The analyses were conducted using the R language with a ‘survey’ package.15–17
Results
Operative procedures
Three hundred and eighty-three of the 3240 cholecystectomies were planned OCs. Of the 2857 LCs, 412 (14.4%) were converted to open (LCC) and 2445 were laparoscopic (TLC). These data are summarized in Fig. 1.
Figure 1.
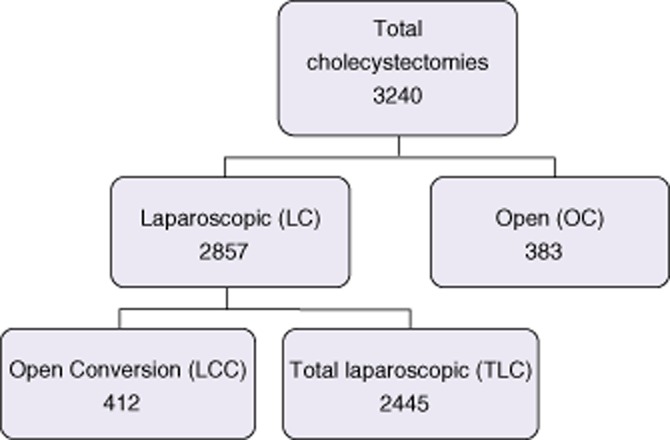
Operative procedures
Demographic data
Demographic information is shown in Table 2. There were no significant differences between the groups studied with respect to age, race and insurance status. Females were more likely to have TLCs than LCCs or OCs.
Table 2.
Demographic data
| Characteristics | OC | LC | Comparisons P-value | |||
|---|---|---|---|---|---|---|
| TLC & LCC | TLC | LCC | OC versus TLC & LCC | OC versus TLC versus LCC | ||
| No. of procedures | 383 | 2857 | 2445 | 412 | ||
| Weighted no. of procedures | 1852 | 13809 | 11794 | 2015 | ||
| Age (mean ± SD) | 62.6 ± 14.5 | 61.3 ± 13.6 | 61.4 ± 13.6 | 60.8 ± 13.0 | 0.134 | 0.155 |
| Femalea | 897 (48.4%) | 6984 (50.6%) | 6105 (51.8%) | 879 (43.6%) | 0.422 | 0.006 |
| Raceb | 0.949 | 0.842 | ||||
| White | 889 (68.1%) | 7203 (67.8%) | 6114 (67.5%) | 1089 (69.5%) | ||
| Black | 120 (9.2%) | 1020 (9.6%) | 869 (9.6%) | 151 (9.6%) | ||
| Hispanic | 226 (17.3%) | 1853 (17.4%) | 1589 (17.5%) | 264 (16.8%) | ||
| Asian or Pacific Islander | 32 (2.4%) | 221 (2.1%) | 182 (2.0%) | 39 (2.5%) | ||
| Native American | 5 (0.4%) | 105 (1.0%) | 105 (1.2%) | 0 (0%) | ||
| Other | 33 (2.5%) | 225 (2.1%) | 200 (2.2%) | 25 (1.6%) | ||
| Insurance statusc | 0.325 | 0.536 | ||||
| Medicare | 983 (53.1%) | 7076 (51.3%) | 6080 (51.6%) | 996 (49.5%) | ||
| Medicaid | 295 (15.9%) | 1755 (12.7%) | 1509 (12.8%) | 246 (12.2%) | ||
| Private including HMO | 439 (23.7%) | 3743 (27.1%) | 3154 (26.8%) | 589 (29.3%) | ||
| Self-pay | 69 (3.7%) | 702 (5.1%) | 613 (5.2%) | 89 (4.4%) | ||
| No charge | 9 (0.5%) | 102 (0.7%) | 89 (0.8%) | 13 (0.6%) | ||
| Other | 56 (3.0%) | 414 (3.0%) | 336 (2.9%) | 77 (3.9%) | ||
| Teaching statusd | 741 (40.4%) | 4481 (32.5%) | 3654 (31.1%) | 827 (41.2%) | 0.006 | <0.0001 |
| Diabetes mellituse | 489 (27.0%) | 4097 (30.0%) | 3499 (30.0%) | 598 (30.2%) | 0.244 | 0.501 |
| Hypertensione | 701 (38.7%) | 6293 (46.0%) | 5445 (46.6%) | 848 (42.7%) | 0.009 | 0.010 |
| Alcohol abusee | 320 (17.6%) | 1998 (14.6%) | 1650 (14.1%) | 348 (17.5%) | 0.123 | 0.063 |
| Congestive heart failuree | 284 (15.7%) | 1426 (10.4%) | 1262 (10.8%) | 164 (8.3%) | 0.002 | 0.002 |
| Chronic pulmonary diseasee | 378 (20.9%) | 2302 (16.8%) | 1957 (16.7%) | 345 (17.4%) | 0.057 | 0.148 |
| Coagulopathye | 391 (21.6%) | 1788 (13.1%) | 1554 (13.3%) | 234 (11.8%) | <0.0001 | <0.0001 |
| Fluid and electrolyte disorderse | 507 (28.0%) | 2259 (16.5%) | 1924 (16.5%) | 335 (16.9%) | <0.0001 | <0.0001 |
| Obesitye | 113 (6.2%) | 1360 (9.9%) | 1130 (9.7%) | 230 (11.6%) | 0.028 | 0.039 |
| Renal failuree | 141 (7.8%) | 798 (5.8%) | 718 (6.1%) | 80 (4.0%) | 0.147 | 0.091 |
| Deficiency anaemiase | 255 (14.1%) | 1237 (9.0%) | 1022 (8.7%) | 215 (10.8%) | 0.003 | 0.004 |
| Hypothyroidisme | 129 (7.1%) | 1174 (8.6%) | 1005 (8.6%) | 168 (8.5%) | 0.320 | 0.628 |
One patient in TLC did not have gender information.
RACE: In the data, 756 out of 3240 patients (23.3%) did not have record. The comparisons among the groups were based on the available records.
Insurance status: four patients did not have the records.
Hospital teaching status: seven patients did not have records of hospital teaching status.
Thirty-seven patients did not have the records of comorbidities.
OC, open cholecystectomy; LC, laparoscopic cholecystectomy; LCC, open conversion; TLC, total laparoscopic; HMO, Health Maintenance Organization.
Complications analysed based on the intent to treat
Post-operative infections were significantly higher in the OC group compared with the LC patients (3.5% versus 0.6%; P < 0.0001, respectively) (Table 3). Post-operative haemorrhage was higher in the OC patients compared with the LC patients (6.6% versus 3.9%; P = 0.01, respectively) as was the number of packed red blood cell (PRBC) transfusions in the OC as compared with the LC patients (19.2% versus 7.4%; P < 0.0001, respectively). There was no difference in the re-operation rate of the OC as compared with the LC patients (P = 0.431). Liver failure was significantly higher in the OC group compared with the LC patients (7.0% versus 1.4%; P < 0.0001, respectively).
Table 3.
Complications
| Outcomes | OC | LC | Comparisons P-value | |||
|---|---|---|---|---|---|---|
| TLC & LCC | TLC | LCC | OC versus TLC & LCC | OC versus TLC versus LCC | ||
| Weighted no. of procedures | 1852 | 13809 | 11794 | 2015 | ||
| Post-operative infection | 66 (3.5%) | 89 (0.6%) | 84 (0.7%) | 5 (0.2%) | <0.0001 | <0.0001 |
| Post-operative haemorrhage | 122 (6.6%) | 537 (3.9%) | 348 (3.0%) | 189 (9.4%) | 0.01 | <0.0001 |
| PRBCs transfusion | 355 (19.2%) | 1023 (7.4%) | 733 (6.2%) | 290 (14.4%) | <0.0001 | <0.0001 |
| Reoperation | 27 (1.5%) | 141 (1.0%) | 91 (0.8%) | 50 (2.5%) | 0.431 | 0.007 |
| Liver failure | 129 (7.0%) | 197 (1.4%) | 168 (1.4%) | 29 (1.4%) | <0.0001 | <0.0001 |
| Ascites | 333 (18.0%) | 1339 (9.7%) | 1108 (9.4%) | 231 (11.5%) | <0.0001 | <0.0001 |
| Mortalitya | 153 (8.3%) | 185 (1.3%) | 160 (1.4%) | 25 (1.3%) | <0.0001 | <0.0001 |
Four patients did not have the data for mortality.
OC, open cholecystectomy; LC, laparoscopic cholecystectomy; LCC, open conversion; TLC, total laparoscopic; PRBC, packed red blood cell.
Complications based on actual operations
Post-operative infection was significantly higher in the OC group compared with TLC and LCC patients (3.5% versus 0.7% versus 0.2%; P < 0.0001, respectively) (Table 3). Post-operative hemorrhage was higher in the OC and LCC patients compared with the TLC group (6.6% versus 9.4% versus 3.0%; P < 0.0001, respectively). A PRBC transfusion was given more often in OC and LCC patients compared with the TLC group (19.2% versus 14.4% versus 6.2%; P < 0.0001, respectively). The reoperation rate was higher in the OC and LCC patients compared with the TLC group (1.5% versus 2.5% versus 0.8%; P = 0.007, respectively). The liver failure rate was significantly higher in the OC group compared with TLC and LCC patients (7.0% versus 1.4% versus 1.4%; P < 0.0001, respectively).
Mortality
Mortality was significantly higher in the OC group compared with the LC (TLC and LCC) group (8.3% versus 1.3%; P < 0.0001) (Table 3). After controlling for potential confounding factors which were significantly different between the OC and LC groups at the 0.1 level of significance, the LC group had a significantly lower chance of mortality as compared with the OC group [adjusted odds ratio (OR): 0.202, 95% confidence interval (CI): (0.121, 0.339), P < 0.0001]. While controlling the same factors, both LC groups (TLC and LCC) had significantly lower mortality as compared with the OC group [TLC: adjusted OR: 0.202, 95% CI: (0.118, 0.345), P < 0.0001; LCC: adjusted OR: 0.203, 95% CI: (0.079, 0.527), P = 0.001]. There was no difference in the mortality rate when comparing the LCC group with the TLC group [adjusted OR: 1.006, 95% CI: (0.393, 2.577)].
Discussion
This retrospective analysis of a large dataset supports the laparoscopic approach for cholecystectomy in cirrhotic patients. While this hypothesis would optimally be tested with a prospective randomized trial no such study has been undertaken. One meta-analysis found only three prospective trials with a total of 220 patients.5,18,19 Although the power of the study was low, the conclusion supports the concept that a laparoscopy should be the initial approach. Similarly, a previous meta-analysis study also used a limited group of cirrhotic patients undergoing LC to deduct parallel results.20 Multiple retrospective studies also compare well to our findings.20–23 This study provides an update to previous articles, while broadening the evidence pool using a large dataset.
Our study identified several major advantages of LC over OC, some of which have been documented in previous articles. Even patients who had to be converted (LCC) to an open cholecystectomy, had lower infection, transfusion and liver failure rates and comparable reoperation rates to the OC group. Moreover, including the LCC in the LC group (intent-to-treat) did not increase the risk of operation that was seen in the OC group. One possible explanation is that the dissection done during LC may decrease the amount of time spent during the open part of the procedure below the operative time of OC. We suspect that the total open operative has a direct impact on the complication rate of the operative procedure.
It should be noted that mortality rates in cirrhotic patients who had abdominal surgery have declined in the 2000s, presumably as a result of improved medical management and critical care.6 Overall, the complication rate inferred in this study is much lower than when OC is the initial approach. A large retrospective study analysing admissions for acute cholecystitis (AC) using the NIS data for all patients, identified an overall mortality rate of 0.5% for LC and 4% for OC. This study demonstrated an increased mortality for patients undergoing OC over LC (8.3% and 1.3%, respectively). This can be attributed to the medically complex patient population that has been evaluated in this study. Importantly, this study demonstrates a six-fold increase in mortality rate when OC is compared with LC. While there may be some pre-selection bias, it is difficult to explain such a morbid outcome on this basis alone. Even more remarkable is a similarly low mortality rate noted in LCC when compared with LC.
Indications for conversion include massive adhesions, inability to define the anatomy and bleeding not readily controlled laparoscopically.24,25 Common bile duct exploration and suspected bile duct injury are other factors commonly leading to OC conversion.24,25 The conversion rate of 14%, documented from the NIS data, is much higher when compared with the majority of the studies addressing this subject.5,10,18,19,26–36 Surgical publications are often permeated with findings that reflect well on the author/surgeon who has performed the procedures in question. Rarely are mediocre results published, possibly contributing to an exaggerated and often misleading results. The NIS data sample gathers above and below par performances, closely reflecting the true national level.
An analysis of 1.4 million patients who underwent a cholecystectomy for AC,23 revealed a decreased conversion rate from 14% in 2000 to 11% in 2005. This conversion rate in the cirrhotic patients was similar to the AC population. While the conversion rate for LC in cirrhotic patients may invariably remain higher than non-cirrhotic patients, it would be hoped that through a more widespread use of LC in this patient population, a steady decline in the conversion rate would be seen.
This study identified only 89 (0.6%) post-operative infections in patients who initially underwent a LC or were eventually converted to OC, whereas a rate of 3.7% is noted in the group that had OC as the initial approach. These data are consistent with post-operative infection rates identified in other studies. Puggioni et al. analysed 17 publications from 1993 to 2001, and found 0% and 0.13% infection rates in LC versus OC, respectively.20 The overall increase in infection rates when compared with Puggioni's results could be attributed to the steady increase in infection rates over time in all surgical subspecialties. Also, it cannot be excluded that the meta-analysis was performed on published ‘favourable’ results. A more recent prospective study would have to be performed in order to extract sensible comparisons.
Studies from the pre-laparoscopic era have emphasized the association between transfusion requirements and mortality8,9 and advised against a cholecystectomy in cirrhotic patients. In a small but carefully controlled randomized study, laparoscopic surgery was been shown to reduce blood loss and eliminate transfusion requirements in cirrhotic patients undergoing a cholecystectomy.37 In a subsequent and larger retrospective study,33 a LC was safely done in 23 of 26 patients for a conversion rate of 12%. Two of the three converted patients had to have open surgery because of uncontrolled bleeding in the bed of the liver. In spite of these two patients, the 26 patients who were in the LC group had a shorter length of hospital stay, less operative blood loss (no transfusion requirements) and less wound problems as compared with the OC group.
There are a number of limitations in this study as a consequence of using an administrative database. It could not determined whether the portal hypertension was present pre- or post-operatively. If present pre-operatively, it may have influenced the surgical approach. One of the main outcomes was in-hospital mortality. The database does not allow patients to be followed after discharge, and a longer follow-up post-discharge may have led to higher mortality rates. This database does not record the length of operative time. In addition it does not stratify if elective or emergent cases were initially performed laparoscopically and their conversion rates. The patient selection was likely affected by presentation of biliary tract disease (acute versus chronic) and degree of compensated versus uncompensated cirrhosis or Child–Turcotte–Pugh and model for end-stage liver disease (MELD) score. Furthermore, the database does not allow the correlation of complication rates with Child–Pugh classification or the MELD score.9,26,27,34
In summary, this study analysed the outcomes of operative therapy for biliary tract disease in cirrhosis patients in the United States. This study suggests that LC is well tolerated in cirrhotic patients. The advantages of LC are: decreased post-operative infection, haemorrhage, transfusion rate, liver failure and mortality rates. Smaller studies have shown similar results in support of our conclusions.5,18,19,25,31,38 Based on the results of this study, the use of OC as the first-line therapy for cirrhosis patients should be questioned. Given the comparable outcomes between the LC and LCC as opposed to OC, the laparoscopic approach should be the preferred initial approach in cirrhotic patients requiring a cholecystectomy. With continuous improvement in the field of minimally invasive surgery, more patients with cirrhosis will benefit from the laparoscopic approach for the treatment of symptomatic biliary tract disease.
Conflicts of interest
None declared.
References
- 1.Ahrendt SA. Calculous biliary disease. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, et al., editors. Sabiston's Textbook of Surgery. 17th edn. Philadelphia: Saunders; 2007. pp. 1612–1615. [Google Scholar]
- 2.Bouchier IA. Postmortem study of the frequency of gallstones in patients with cirrhosis of the liver. Gut. 1969;10:705–710. doi: 10.1136/gut.10.9.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bloch RS, Allaben RD, Walt AJ. Cholecystectomy in patients with cirrhosis. A surgical challenge. Arch Surg. 1985;120:669–672. doi: 10.1001/archsurg.1985.01390300019003. [DOI] [PubMed] [Google Scholar]
- 4.Aranha GV, Sontag SJ, Greenlee HB. Cholecystectomy in cirrhotic patients: a formidable operation. Am J Surg. 1982;143:55–60. doi: 10.1016/0002-9610(82)90129-5. [DOI] [PubMed] [Google Scholar]
- 5.Hamad MA, Thabet M, Badawy A, Mourad F, Abdel-Salam M, Abdel-Rahman M, et al. Laparoscopic versus open cholecystectomy in patients with liver cirrhosis: a prospective, randomized study. J Laparoendosc Adv Surg Tech A. 2010;20:405–409. doi: 10.1089/lap.2009.0476. [DOI] [PubMed] [Google Scholar]
- 6.Kogut K, Aragoni T, Ackerman NB. Cholecystectomy in patients with mild cirrhosis. A more favorable situation. Arch Surg. 1985;120:1310–1311. doi: 10.1001/archsurg.1985.01390350090019. [DOI] [PubMed] [Google Scholar]
- 7.Leone N, Garino M, De Paolis P, Pellicano R, Fronda GR, Rizzetto M. Laparoscopic cholecystectomy in cirrhotic patients. Dig Surg. 2001;18:449–452. doi: 10.1159/000050192. [DOI] [PubMed] [Google Scholar]
- 8.McSherry CK, Glenn F. The incidence and causes of death following surgery for nonmalignant biliary tract disease. Ann Surg. 1980;191:271–275. doi: 10.1097/00000658-198003000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwartz SI. Biliary tract surgery and cirrhosis: a critical combination. Surgery. 1981;90:577–583. [PubMed] [Google Scholar]
- 10.Conte D, Barisani D, Mandelli C, Bodini P, Borzio M, Pistoso S, et al. Cholelithiasis in cirrhosis: analysis of 500 cases. Am J Gastroenterol. 1991;86:1629–1632. [PubMed] [Google Scholar]
- 11.Kim WR, Brown RS, Jr, Terrault NA, El-Serag H. Burden of liver disease in the united states: summary of a workshop. Hepatology. 2002;36:227–242. doi: 10.1053/jhep.2002.34734. [DOI] [PubMed] [Google Scholar]
- 12.Garrison RN, Cryer HM, Howard DA, Polk HC., Jr Clarification of risk factors for abdominal operations in patients with hepatic cirrhosis. Ann Surg. 1984;199:648–655. doi: 10.1097/00000658-198406000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doberneck RC, Sterling WA, Jr, Allison DC. Morbidity and mortality after operation in nonbleeding cirrhotic patients. Am J Surg. 1983;146:306–309. doi: 10.1016/0002-9610(83)90402-6. [DOI] [PubMed] [Google Scholar]
- 14.Bernardo WM, Aires FT. Is laparoscopic cholecystectomy safe in patients with liver cirrhosis? Rev Assoc Med Bras. 2011;57:360–361. [PubMed] [Google Scholar]
- 15.Lumley T. Analysis of complex survey samples. J Stat Software. 2004;9:1–19. [Google Scholar]
- 16.Lumley T. Survey: analysis of complex survey samples. 2009. R package version 3.16.
- 17.R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R foundation for statistical computing; 2008. ISBN 3-900051-07-0. Available at http://www.R-project.org (last accessed 19 September 2012) [Google Scholar]
- 18.Ji W, Li LT, Wang ZM, Quan ZF, Chen XR, Li JS. A randomized controlled trial of laparoscopic versus open cholecystectomy in patients with cirrhotic portal hypertension. World J Gastroenterol. 2005;11:2513–2517. doi: 10.3748/wjg.v11.i16.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El-Awadi S, El-Nakeeb A, Youssef T, Fikry A, Amir A, AbdEl Hamid TM, et al. Laparoscopic versus open cholecystectomy in cirrhotic patinets: a prospective randomized study. Int J Surg. 2009;7:66–69. doi: 10.1016/j.ijsu.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 20.Puggioni A, Wong LL. A metaanalysis of laparoscopic cholecystectomy in patients with cirrhosis. J Am Coll Surg. 2003;197:921–926. doi: 10.1016/j.jamcollsurg.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen GC, Laveist TA, Segev DL, Thuluvath PJ. Race is a predictor of in-hospital mortality after cholecystectomy, especially in those with portal hypertension. Clin Gastroenterol Hepatol. 2008;6:1146–1154. doi: 10.1016/j.cgh.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 22.Csikesz NG, Nguyen LN, Tseng JF, Shah SA. Nationwide volume and mortality after elective surgery in cirrhotic patients. J Am Coll Surg. 2009;208:96–103. doi: 10.1016/j.jamcollsurg.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Csikesz NG, Tseng JF, Shah SA. Trends in surgical management for acute cholecystitis. Surgery. 2008;144:283–289. doi: 10.1016/j.surg.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 24.Bingener-Casey J, Richards ML, Strodel WE, Schwesinger WH, Sirinek KR. Reasons for conversion from laparoscopic to open cholecystectomy: a 10-year review. J Gastrointest Surg. 2002;6:800–805. doi: 10.1016/s1091-255x(02)00064-1. [DOI] [PubMed] [Google Scholar]
- 25.Colonval P, Navez B, Cambier E, Richir C, de Pierpont B, Scohy JJ, et al. Is laparoscopic cholecystectomy effective and reliable in acute cholecystitis? Results of a prospective study of 221 pathologically documented cases. Ann Chir. 1997;51:689–696. [PubMed] [Google Scholar]
- 26.Bingener J, Cox D, Michalek J, Mejia A. Can the MELD score predict perioperative morbidity for patients with liver cirrhosis undergoing laparoscopic cholecystectomy? Am Surg. 2008;74:156–159. [PubMed] [Google Scholar]
- 27.Delis S, Bakoyiannis A, Madariaga J, Bramis J, Tassopoulos N, Dervenis C. Laparoscopic cholecystectomy in cirrhotic patients: the value of MELD score and child-pugh classification in predicting outcome. Surg Endosc. 2010;24:407–412. doi: 10.1007/s00464-009-0588-y. [DOI] [PubMed] [Google Scholar]
- 28.Curro G, Iapichino G, Melita G, Lorenzini C, Cucinotta E. Laparoscopic cholecystectomy in child-pugh class C cirrhotic patients. JSLS. 2005;9:311–315. [PMC free article] [PubMed] [Google Scholar]
- 29.Angrisani L, Lorenzo M, Corcione F, Vincenti R. Gallstones in cirrhotics revisited by a laparoscopic view. J Laparoendosc Adv Surg Tech A. 1997;7:213–220. doi: 10.1089/lap.1997.7.213. [DOI] [PubMed] [Google Scholar]
- 30.Cucinotta E, Lazzara S, Melita G. Laparoscopic cholecystectomy in cirrhotic patients. Surg Endosc. 2003;17:1958–1960. doi: 10.1007/s00464-002-8852-4. [DOI] [PubMed] [Google Scholar]
- 31.Llujan JA, Parrilla P, Robles R, Marin P, Torralba JA, Garcia-Ayllon J. Laparoscopic cholecystectomy vs open cholecystectomy in the treatment of acute cholecystitis: a prospective study. Arch Surg. 1998;133:173–175. doi: 10.1001/archsurg.133.2.173. [DOI] [PubMed] [Google Scholar]
- 32.Palanivelu C, Rajan PS, Jani K, Shetty AR, Sendhilkumar K, Senthilnathan P, et al. Laparoscopic cholecystectomy in cirrhotic patients: the role of subtotal cholecystectomy and its variants. J Am Coll Surg. 2006;203:145–151. doi: 10.1016/j.jamcollsurg.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 33.Poggio JL, Rowland CM, Gores GJ, Nagorney DM, Donohue JH. A comparison of laparoscopic and open cholecystectomy in patients with compensated cirrhosis and symptomatic gallstone disease. Surgery. 2000;127:405–411. doi: 10.1067/msy.2000.104114. [DOI] [PubMed] [Google Scholar]
- 34.Schiff J, Misra M, Rendon G, Rothschild J, Schwaitzberg S. Laparoscopic cholecystectomy in cirrhotic patients. Surg Endosc. 2005;19:1278–1281. doi: 10.1007/s00464-004-8823-z. [DOI] [PubMed] [Google Scholar]
- 35.Tuech JJ, Pessaux P, Regenet N, Rouge C, Bergamaschi R, Arnaud JP. Laparoscopic cholecystectomy in cirrhotic patients. Surg Laparosc Endosc Percutan Tech. 2002;12:227–231. doi: 10.1097/00129689-200208000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Yeh CN, Chen MF, Jan YY. Laparoscopic cholecystectomy in 226 cirrhotic patients. experience of a single center in Taiwan. Surg Endosc. 2002;16:1583–1587. doi: 10.1007/s00464-002-9026-0. [DOI] [PubMed] [Google Scholar]
- 37.Yerdel MA, Koksoy C, Aras N, Orita K. Laparoscopic versus open cholecystectomy in cirrhotic patients: a prospective study. Surg Laparosc Endosc. 1997;7:483–486. [PubMed] [Google Scholar]
- 38.Scott TR, Sucker KA, Bailey RW. Laparoscopic cholecystectomy: a review of 12397 patients. Surg Laparosc Endosc. 1992;2:191–198. [PubMed] [Google Scholar]


