Abstract
Background
An air embolus is a recognized but rare complication of a partial hepatectomy. The aim of this report was to describe the diagnosis and management of a large paradoxical air embolus during hepatic resection.
Methods
Case report.
Results
A single patient report of a massive paradoxical air embolus during an extended right hepatectomy is described. The diagnosis was confirmed by trans-oesophageal echo (video provided). After failed conservative management an emergency cardiopulmonary bypass was instituted with a successful outcome.
Conclusion
Surgeons and anaesthetists involved in hepatic surgery should be aware of signs, investigations and management of this life-threatening intra-operative complication.
During a hepatectomy, an air embolus can occur as a consequence of a hepatic vein or a tributary being opened.1 This combined with sub-ambient pressure in the vein can result in a pressure gradient favouring air entry.2 In addition, compression and manipulation of the inferior vena cava (IVC) at its junction with the hepatic veins can result in a Venturi effect whereby a high flow rate in the compressed vessel causes air to entrain via numerous openings of the small hepatic venous or IVC tributaries.1 As a consequence, large air emboli can enter the right side of the heart and cause cardiopulmonary collapse.2 In the presence of an atrial or ventricular septal defect3 or simply by transpulmonary passage,4,5 a left-sided or paradoxical air embolus (PAE) can occur with devastating sequelae.2 This study describes a situation in which a large right- and left-sided air embolus occurred and details the subsequent management of it during an extended right hepatectomy.
A 43-year-old female presented with a diagnosis of carcinoid syndrome from an ileal primary with hepatic metastasis. A pre-operative echocardiogram showed no structural cardiac abnormality. After a small bowel resection to control the primary and regional disease a potentially curative hepatic resection was planned to achieve symptomatic control of both carcinoid syndrome resistant to octreotide and the local mass effect. The tumour was 14 cm in diameter and involved the confluence of the right and middle hepatic veins and compressed the retro-hepatic vena cava (Fig. 1). As part of the pre-operative planning it was elected to perform this surgery in the cardiac theatre with a cardiac team on standby in case of the need for veno-veno bypass to allow safe resection and or reconstruction of the inferior vena cava. Anaesthesia aimed at maintaining a central venous pressure of less than 5 mmHg was instituted. After hepatic mobilization it became apparent that the liver could not be returned to the abdomen as it resulted in caval compression and profound hypotension. Dissection could only be continued with the liver constantly supported by the surgeons. The right hepatic vein and short hepatic veins were divided allowing the termination of the middle hepatic vein to be visualized. In the process of isolating the middle hepatic vein a small tear occurred but was effectively controlled during a short period of total vascular exclusion. However, while controlling this, the patient became cardiovascularly unstable with a sudden decrease in systolic blood pressure (SBP) to 65 mmHg and heart rate (HR) to 30 beats/min associated with widened QRS complexes on ECG and T wave inversion. SpO2 decreased from 97% to 64% and ETCO2 from 34kPa to 20kPa. Simultaneously CVP increased from <5 mmHg to 25 mmHg. In an attempt to restore circulation repeated 10 mcg boluses of noradrenaline and then adrenaline were given along with increasing rates of continuous infusion up to 12 μg/min of each. An air embolus was suspected on intra-operative ultrasound and confirmed with a transoesophageal echocardiogram (TOE) performed approximately 10 min after the start of deterioration. This showed air bubbles in both ventricles and severe impairment of the right ventricular function (Video S1, S2). In spite of escalating medical therapy to improve the patient's cardiovascular status no improvement was seen and a decision to proceed to an emergency sternotomy and cardiopulmonary bypass was instituted. Almost immediately after commencement of cardio-pulmonary bypass the HR returned to 90 beats/min and ECG changes returned to normal. However, air continued to enter the bypass circuit indicating an ongoing source of an air embolus and on further mobilization of the liver, a small hole in the intrahepatic portion of the middle hepatic vein which was not bleeding was identified and closed. Evidence of air entrainment ceased. In spite of full anticoagulation with heparin it was elected that a hepatectomy would proceed on bypass as the right lobe was ischaemic and could not be returned to the abdomen. Subsequent to the hepatic resection the anticoagulation was reversed with a combination of clotting factors and blood products. Haemostasis was satisfactory at the end of the procedure. The patient was weaned from cardiopulmonary bypass after 1 h. A repeat TOE a further hour later showed marked improvement in right ventricular function (Video S3). The patient had an uneventful post-operative recovery and was discharged 10 days later with no neurological deficits.
Figure 1.
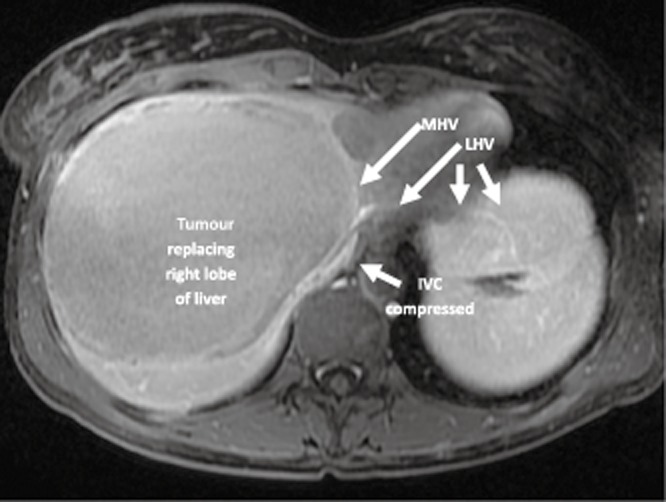
Magnetic resonance imaging (MRI) showing a tumour replacing the right lobe of the liver and compressing the inferior vena cava (IVC). The tumour can be seen compressing the origin of the middle hepatic vein (MHV) and the left hepatic vein (LHV)
The morbidity and mortality as a result of an air embolism depends on the volume as well as the rate of air entry.2,6 Animal models have assessed the volume of air necessary to provoke circulatory collapse. As a single bolus, this has been found to be 7.5–15 ml/kg in dogs.7 In humans this has been reported to be 200–300 ml or 3–5 ml/kg.8,9 The rate of air entrainment is also of importance because of the time taken for the lungs to dissipate intrapulmonary gas.2 In animal models, air infused directly into the right ventricle at a rate of 0.05 ml/kg/min can be completely filtered by the lungs and remained undetectable to TOE.6 If the volume or rate of air entry exceeds the ‘filtration’ capacity of the lungs then PAE can arise from intrapulmonary passage and ‘spill-over’ to the left ventricle.6
The variables of rate and volume of air entrained are in turn impacted on by the position of the patient and the height of the portal of air entry relative to the right side of the heart, because of the effects of gravity on venous pressure. This is exemplified by the high incidence of an air embolism during craniotomies performed in the sitting position2 and during genitourinary surgeries performed in the Trendelenburg position.2 The position of this patient was supine throughout the procedure within the abdominal cavity. This had two consequences which increased the risk of an air embolus after opening of the hepatic vein; the hepatic veins were elevated above the right heart and once holed, the hole was stented open by the elevated position allowing a large amount of air to entrain. The combination of the position of the hole and the low CVP meant that the opening was not easily detectable by the surgeons as there was no evidence of overt bleeding. It was not until the patient was on bypass and further entrainment of air was detected that it lead to an additional search for a breach in the venous architecture.
In spite of maximal medical interventions the patient's status was perilous. The decision by the cardiac surgeon to proceed to bypass was made on the premise that with a major air embolus, the right ventricle becomes filled with ‘froth’ and although it is contracting an air lock is generated resulting in compromised cardiac output (Video S2). This situation could only be remedied by surgical intervention. In retrospect the filling of the right upper quadrant with large volumes of fluid2 or flooding the abdominal cavity with carbon dioxide10 might have helped the situation.
The development of a PAE was also unusual. PAE can arise from a septal defect such as that of a patent foramen ovale (PFO)3 or passage through the lungs.4,5 A probe patent PFO or a small PFO undetected by TOE could allow passage of air into the L heart and the systemic circulation under the conditions of elevated R heart pressure and pulmonary arterial pressure (PAP) generated by an air embolus, or form controlled ventilation and use of positive end-expiratory pressure (PEEP) intra-operatively. Probe patent PFOs are common and have an incidence of about 25% in the general population.11 In the patient described the TOE demonstrated very high right atrial pressure with bowing of the intra atrial septum towards the left atrium and a dilated hypokinetic right ventricle (Video S1, S2).
The lungs normally provide a ‘filter’ for small amounts of air bubbles, preventing transpulmonary passage by trapping air and allowing its dissolution into the blood. Intrapulmonary shunts occur in the setting of pulmonary arteriovenous malformation (AVM), or direct arteriovenous communications and dilated pre-capillaries in the lungs shown to be present in end-stage hepatic disease (up to 47%)12 but are also present in normal individuals although less commonly.13,14 Previous case reports have demonstrated an intra-operative PAE arising from intrapulmonary arteriovenous shunts in patient with no known liver or pulmonary disease.5 Passage of air through the lungs occurs if the volume or rate of air entrainment is sufficient but the presence of an intrapulmonary shunt would have enhanced this.5,15 In this patient, the entrainment of a large amount of air trapped in the right ventricle would have increased the PAP, causing dilatation of pulmonary precapillaries and may have forced open anatomical shunts, facilitating the transpulmonary passage of larger air bubbles.14,15 The development of the PAE within the left ventricle could have contributed further to myocardial ischemia as a result of coronary artery embolization as suggested by increased echogenicity and severely impaired myocardial function of the right ventricle.
In conclusion, a clinically significant air embolus during liver resection is an extremely rare but life-threatening situation. Hepatic surgeons and their anaesthetists should be aware of the presenting symptoms and treatment options. Particular learning points from the events described include the fact that ongoing entrainment occurred in spite of the surgeons being aware of the diagnosis. The immediate availability of cardiac team almost certainly saved this patients life.
Conflicts of interest
No declared.
Supporting information
Additional Supporting Information may be found in the online version of this article:
Video S1. Four chamber mid-oesophageal view of the heart shows air bubbles in all four chambers, dilatation of the right ventricle and atrium and severely impaired right ventricular function. As a result of severely raised RA pressure the thin fossa membrane of the interatrial septum bulges prominently into the left atrium. It is not clear if the bubbles in the left heart have traversed the lung or have travelled through a patent foramen ovale.
Video S2. Less than 30 s later many of the bubbles have cleared allowing greater appreciation of the severity of the right ventricle impairment and of a large bubble trapped in the right ventricle between the tricuspid valve and the anterior wall.
Video S3. Two hours later the air bubbles have cleared. The right heart size has dramatically decreased and right ventricular systolic function appears near normal.
Please note: Wiley-Blackwell are not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.Hatano Y, Murakawa M, Segewa H, Nishida Y, Mori K. Venous air embolism during hepatic resection. Anesthesia. 1990;73:1282–1285. doi: 10.1097/00000542-199012000-00036. [DOI] [PubMed] [Google Scholar]
- 2.Mirski MA, Vijay Lele A, Fitzsimmons L, Toung TJK. Diagnosis and treatment of vascular air embolism. Anesthesia. 2007;106:164–177. doi: 10.1097/00000542-200701000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Thiery G, Le Corre F, Sauvanett A, Belghiti J, Marty J. Paradoxical air embolism during orthoptic liver transplantation:diagnosis by transoesophageal echocardiography. Eur J Anaesth. 1999;16:342–345. doi: 10.1046/j.1365-2346.1999.00479.x. [DOI] [PubMed] [Google Scholar]
- 4.Lee SY, Choi BIW, Kim JS, Park KS. Paradoxical air embolism during hepatic resection. Br J Aaesth. 2002;88:136–138. doi: 10.1093/bja/88.1.136. [DOI] [PubMed] [Google Scholar]
- 5.Rademaker BMP, Groenman FA, Van der Wouw PA, Bakkum EA. Paradoxical gas embolism by transpulmonary passage of venous emboli during hysteroscopic surgery: a case report and discussion. Br J Anaesth. 2008;101:230–233. doi: 10.1093/bja/aen138. [DOI] [PubMed] [Google Scholar]
- 6.Butler BD, Hills BA. Transpulmonary passage of venous air emboli. J Appl Physiol. 1985;59:543–547. doi: 10.1152/jappl.1985.59.2.543. [DOI] [PubMed] [Google Scholar]
- 7.Alvaran SB, Toung JK, Graff TE, Benson DW. Venous air embolism: comparative merits of external cardiac massage, intracardiac aspiration, and left lateral decubitus position. Anesth Anal. 1978;57:166–170. doi: 10.1213/00000539-197803000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Toung JK, Rossberg MI, Hutchins GM. Volume of air in a lethal venous air embolism. Anesthesia. 2001;94:360–361. doi: 10.1097/00000542-200102000-00031. [DOI] [PubMed] [Google Scholar]
- 9.Martland H. Air embolism: fatal air embolism due to powder insufflators used in gynecological treatments. Am J Surg. 1945;68:164–169. [Google Scholar]
- 10.Webb WR, Harrison LH, Helmcke FR, Camino-Lopez A, Munfakh NA, Heck HA, Jr, et al. Carbon dioxide field flooding minimizes residual intracardiac air after open heart operations. Ann Thorac Surg. 1997;64:1489–1491. doi: 10.1016/S0003-4975(97)00945-4. [DOI] [PubMed] [Google Scholar]
- 11.Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59:17–20. doi: 10.1016/s0025-6196(12)60336-x. [DOI] [PubMed] [Google Scholar]
- 12.Hopkins WE, Waggoner Ad BB. Frequency and significance of intrapulmonary right-to-left shunting in end-stage hepatic disease. Am J Card. 1992;70:516–519. doi: 10.1016/0002-9149(92)91200-n. [DOI] [PubMed] [Google Scholar]
- 13.Tobin CE. Arteriovenous shunts in the peripheral pulmonary circulation in the human lung. Thorax. 1966;21:197–204. doi: 10.1136/thx.21.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkinson MJ, Fagan DG. Postmortem demonstration of intrapulmonary arteriovenous shunting. Arch Dis Child. 1990;65:435–437. doi: 10.1136/adc.65.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eldridge MW, Dempsey JA, Haverkamp HC, Lovering AT, Hokanson JS. Exercise-induced intrapulmonary arteriovenous shunting in healthy humans. J Appl Physiol. 2004;97:797–805. doi: 10.1152/japplphysiol.00137.2004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


