Abstract
Objectives
Metabolic syndrome has received attention as a risk factor for cardiovascular disease, with particular importance attached to visceral fat accumulation, which is associated with lifestyle-related diseases and is strongly correlated with waist circumference. In this study, our aim is to propose waist circumference cut-off values that can be used as a marker for fatty liver based on a sample of workers receiving health checkups in Japan.
Methods
This study was conducted in a total of 21,866 workers who underwent periodic health checkups between January 2007 and December 2007. The mean age of the subjects was 47.4 years for men (standard deviation [SD]: 8.0) and 44.7 years for women (SD: 6.9). Evaluation included abdominal ultrasound and measurement of waist circumference, body mass index, fasting blood glucose, triglycerides, high-density lipoprotein cholesterol, and blood pressure.
Results
Based on receiver operating characteristic curve analysis, the optimal waist circumference cut-off values were shown as 85.0 cm (sensitivity 0.72, specificity 0.69) for men and 80.0 cm (sensitivity 0.75, specificity 0.78) for women.
Conclusion
Abdominal ultrasound is the most efficient means of diagnosing fatty liver, but this examination seldom occurs because the test is not routinely performed at workers' health checkups. In people found to have a high risk of fatty liver, recommendations can be made for abdominal ultrasound based on the waist circumference cut-off values obtained in this study. That is, waist circumference can be used in high risk individuals as an effective marker for early detection of fatty liver.
Keywords: Waist circumference, Fatty liver, Health-check examination, Ultrasonography, Receiver operating characteristic (ROC) curve analysis
Introduction
According to the cause-of-death statistics provided by the Japanese Ministry of Health, Labor, and Welfare (JMHLW), cerebrovascular disease and cardiovascular disease caused by obesity and arteriosclerosis account for about 30% of all deaths. Risk factors for these diseases include lifestyle factors and metabolic syndrome (visceral fat syndrome) due to the accumulation of visceral fat this involves. Urgent measures are required to reduce the prevalence of these risk factors in Japan. One such measure was the implementation in 2008 of "specific health checkups" and "specific counseling guidance" with a focus on visceral fat-type obesity [1]. This led to the adoption of waist circumference (WC) as a marker for visceral fat-type obesity and the assessment of risk based on lifestyle.
Together with growing knowledge of the concept of metabolic syndrome, the relationship between visceral fat accumulation and lifestyle-related diseases such as hypertension, diabetes mellitus, and lipid abnormalities has become increasingly clear [2-6]. Implementing specific health checkups and counseling guidance aims to prevent the onset or progression of lifestyle-related diseases as a cause of cardiovascular events, which is advantageous because the early screening of candidates can promote a reduction in the number of persons with or at risk for such diseases.
One example of visceral fat accumulation is fatty liver, which is a condition characterized by excess accumulation of triglycerides (TG) in hepatocytes. The major causes include obesity, excess alcohol consumption, and endocrine diseases such as diabetes. Fatty liver is promoted by overeating, lack of exercise, and the westernization of dietary habits. The prevalence of fatty liver detected at health checkups has been increasing over the years: 12.6% in 1989, 30.3% in 1998 [7], and 39.6% and 18.2% in 2002 in males and females, respectively [8]. Fatty liver, in terms of visceral fat accumulation, is also strongly associated with metabolic syndrome.
In a 2005 study, a strong correlation was found between histogram indices of aspartate transaminase (AST), alanine aminotransferase (ALT), gamma-glutamyl transpeptidase (γ-GTP) and fatty liver [9]. Kawabe et al. [10] reported that the AST/ALT ratio was better than AST, ALT, and γ-GTP as a marker for fatty liver. Yamada et al. [11] found that body mass index (BMI) and lipid test results, glucose level, and uric acid values were significant risk factors for predicting the probability of fatty liver development. Although studies such as these have been performed using biochemical test values as markers for fatty liver, no known studies have quantitatively specified and demarcated the use of WC as a marker for fatty liver.
Waist circumference is reported to be closely correlated with visceral fat accumulation [12,13]. We believe that visceral fat accumulation, as representative of fatty liver, could be assessed by applying the WC cut-off values obtained in this study and by performing abdominal ultrasound in selected high-risk patients. The aims of this study were thus to 1) compare clinical values between fatty and healthy liver groups, and 2) to provide the optimal WC cut-off values for screening for fatty liver.
Materials and Methods
Subjects
The data used in the present study consisted of the results of employee health checks conducted at a medical examination center between January and December 2007 for employees from 225 companies within the manufacturing, finance and service industries, as well as in local government. Japanese companies are required to implement annual occupational health checkups, which are conducted by medical examination centers that meet national standards and hold related individual contracts with various types of businesses such as those mentioned above. Checkup parameters comprise statutory items established by the government alongside optional tests.
Among 225,602 employees (from 225 companies), a total of 30,650 (13.6%) were from 99 companies that offered ultrasound examination as an optional test. Complete clinical data including WC, BMI, fasting blood sugar (FBS), hemoglobin A1c (HbA1c), TG, high-density lipoprotein-cholesterol (HDL-C), and systolic and diastolic blood pressure were available for 23,740 of the 30,650 employees who underwent optional abdominal ultrasound screening. After excluding 1,874 employees (1,326 men, 548 women) due to hypertension, hyperlipidemia, current diabetes treatment and positivity for hepatitis B and C, data from 21,866 subjects (11,509 men, 10,357 women) were analyzed.
The study protocol was approved by the Ethics Committee of the Association for Preventive Medicine of Japan. No data were collected that could be used for identification.
Fatty liver diagnostic criteria
General purpose ultrasound diagnostic imaging scanners were used for abdominal ultrasound screening at a frequency of 3-5 MHz to produce B mode images, which display levels of brightness based on reflected ultrasound intensity.
Patients satisfying all four items of the diagnostic criteria were diagnosed with fatty liver, while those satisfying less than four items were given the diagnosis of fatty liver change (mild fatty liver). In the present study, individuals of the latter type were included in the fatty liver group as they represented potential cases of fatty liver.
Measurement of WC
Based on the diagnostic criteria for metabolic syndrome, WC was measured in a standing position, during quiet breathing, at the level of the umbilicus. If there was marked fat accumulation with the umbilicus displaced downwards, WC was measured at a point midway between the lower rib margin and the anterior superior iliac spine.
Statistical analysis
The frequency of subjects diagnosed with fatty liver and healthy liver by sex and age was examined using the abdominal ultrasound findings, and the results were divided among age groups representing 5-year intervals. In addition, between the fatty liver group and the healthy liver group, clinical values by sex, including WC, BMI, FBS, HbA1c, TG, HDL-C, systolic blood pressure, and diastolic blood pressure were compared. Blood samples were collected after overnight fasting. Two-group comparisons were analyzed by Student's unpaired t-test.
To assess the utility of WC as a marker of fatty liver, the optimal cut-off values, sensitivity, specificity, and receiver operating characteristic (ROC) area under the curve (AUC) were calculated by sex.
WC was classified in 2-cm intervals starting from 70 cm. The proportion of subjects with fatty liver by WC category and sex was determined.
Results
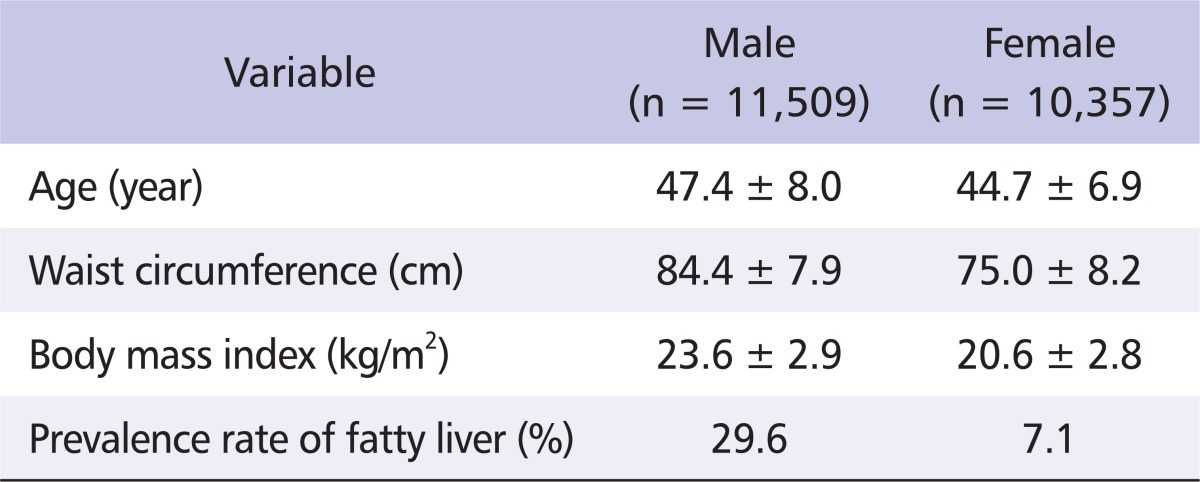
Table 1 shows the subject characteristics. The mean age was 47.4 years for men and 44.7 years for women. Among subjects, those with a diagnosis of fatty liver based on abdominal ultrasound numbered 3,402 men (29.6%) and 737 women (7.1%).
Table 1.
The characteristics of the study subjects
Values are presented as mean ± standard deviation or number.
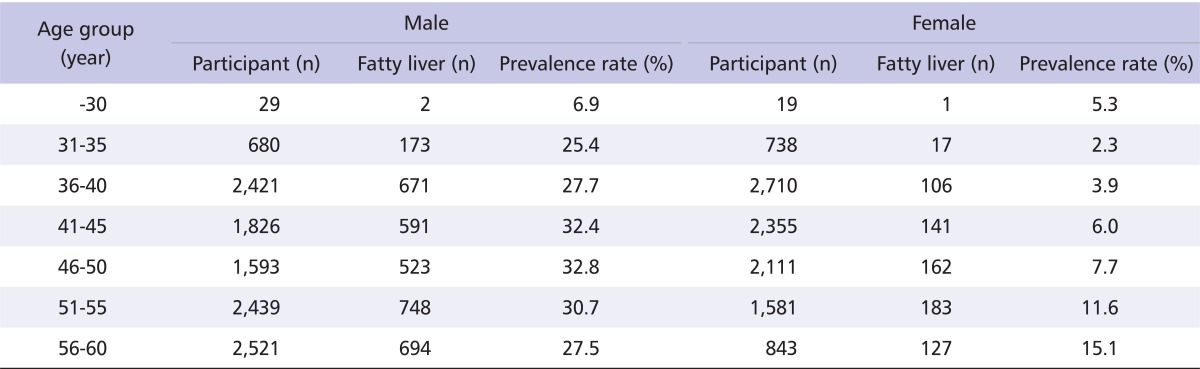
The prevalence of fatty liver by age classification (age divided into 5-year groups) and sex was examined. The proportion of subjects diagnosed with fatty liver increased with age, and a high prevalence was seen in men in their 40s. In women, the prevalence of fatty liver was relatively low, but increases were seen after the age of 50 (Table 2).
Table 2.
Prevalence of fatty liver by sex and age classification
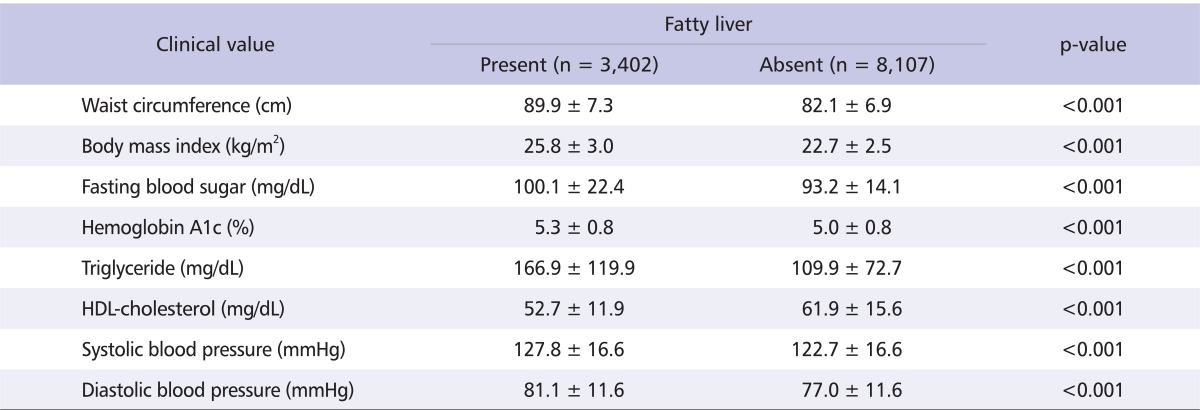
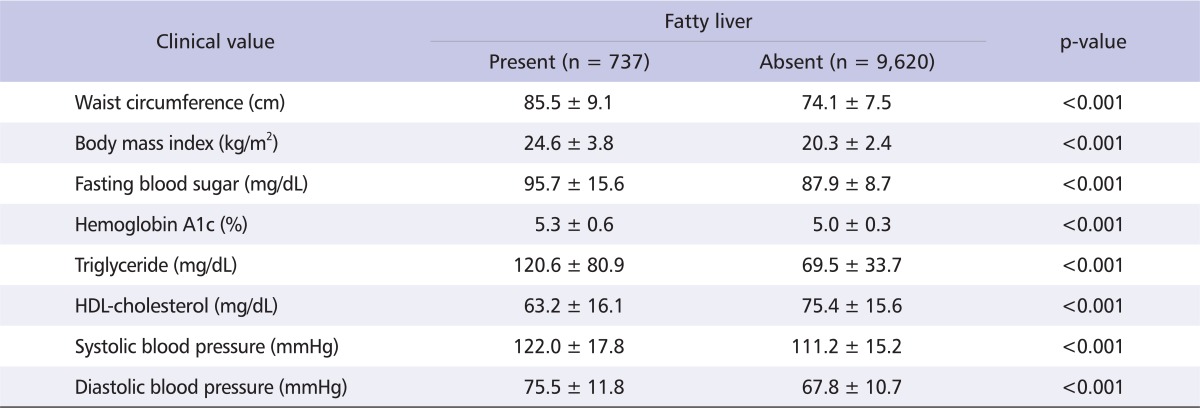
Clinical values were compared between the fatty liver group (subjects with a diagnosis of fatty liver) and the healthy liver group. Other than HDL-C, all test values in the fatty liver group were significantly higher in both men and women. In the male fatty liver group, the mean WC exceeded the metabolic syndrome diagnostic criterion of 85 cm and BMI exceeded the obesity criterion of 25 (Tables 3, 4).
Table 3.
Comparison of clinical values between the fatty liver group and the healthy liver group (males; n=11,509)
Values are presented mean ± standard deviation.
HDL: high-density lipoprotein.
Table 4.
Comparison of clinical values between the fatty liver group and the healthy liver group (female; n = 10,357)
Values are presented mean ± standard deviation.
HDL: high-density lipoprotein.
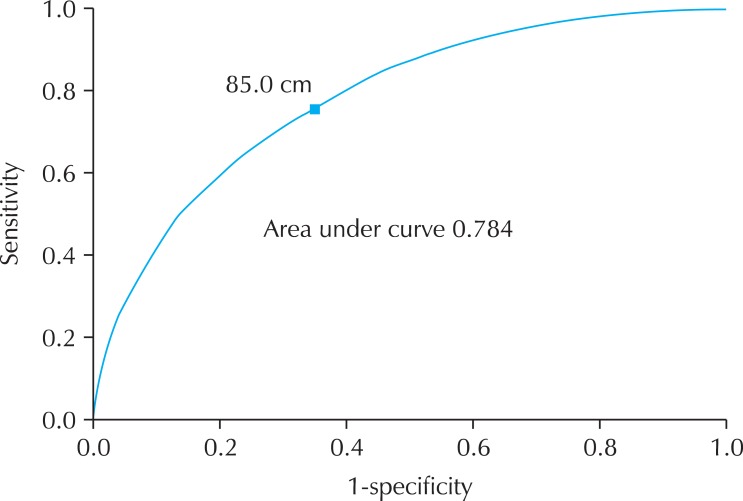
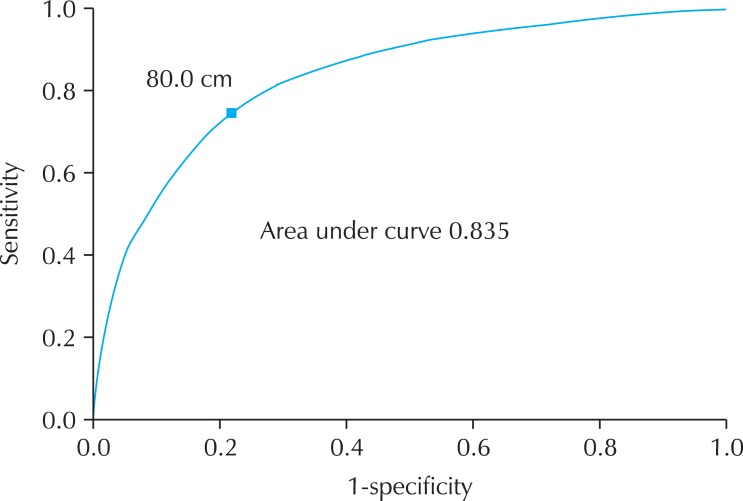
As a marker for fatty liver, the optimal cut-off values for WC were calculated using an ROC curve. As seen from the ROC curves in Fig. 1 and Fig. 2, the shortest distance from the left upper corner and the maximum product of sensitivity and specificity was at 85.0 cm in men (sensitivity 0.72, specificity 0.69) and 80.0 cm in women (sensitivity 0.75, specificity 0.78).
Fig. 1.
Receiver operating characteristic (ROC) curve (males). As seen from the ROC curves, the shortest distance from the left upper corner and the maximum product of sensitivity and specificity was 85.0 cm in men (sensitivity 0.72, specificity 0.69). These were defined as the optimal waist circumference cut-off values for men.
Fig. 2.
Receiver operating characteristic (ROC) curve (females). As seen from the ROC curves, the shortest distance from the left upper corner and the maximum product of sensitivity and specificity was 80.0 cm in women (sensitivity 0.75, specificity 0.78). These were defined as the optimal waist circumference cut-off values for women.
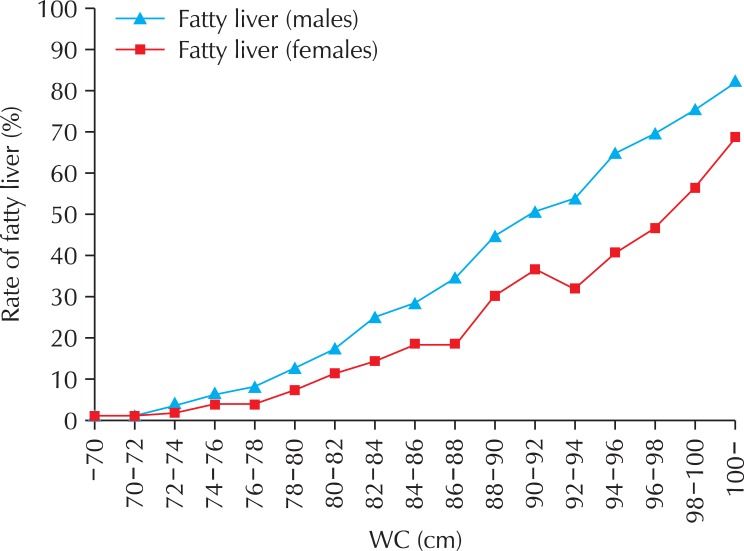
WC was classified at 2-cm intervals and the prevalence of fatty liver by WC category was examined. In both men and women, increases in WC were correlated to increases in the prevalence of fatty liver (Fig. 3).
Fig. 3.
Rate of fatty liver by waist circumference (WC). WC was classified in 2-cm intervals and the prevalence of fatty liver by WC category was examined. In both men and women, as WC increased, the prevalence of fatty liver also increased.
Discussion
In this study, we assessed WC, which is an indicator of the degree of visceral fat accumulation, as a marker for fatty liver by analyzing ROC curves to demonstrate their relationship. Based on the ROC curves shown in Fig. 1 and Fig. 2, the optimal WC cut-off values were 85.0 cm in men and 80.0 cm in women.
Compared to the WC cut-off values used in the JMHLW specific health checkups (85.0 cm in men and 90.0 cm in women), our findings did not differ much for men, but in women, there was a 10 cm discrepancy. It has been previously assumed that men typically have visceral fat-type obesity and that women typically have subcutaneous fat-type obesity [14]. The rate of coexisting metabolic syndrome is known to be higher with visceral fat-type obesity than with subcutaneous fat-type obesity [15]. However, our study found that even in women with a WC < 90.0 cm, which is below the criteria for obesity in the JMHLW health checkups, visceral fat accumulation representative of fatty liver was present. Men have a higher prevalence of fatty liver and if undiscovered and left untreated, this progresses to become a risk factor for lifestyle-related diseases such as hypertension, diabetes, and hyperlipidemia. Our results for men matched the WC cut-off point for obesity in the JMHLW health checkups, but in women, our results were lower. Lifestyle guidance at an early stage, with an emphasis on diet, exercise, and careful follow-up evaluation, is important for fatty liver prevention.
Additionally, clinical values including blood pressure, glucose, and lipid values were significantly higher in patients with fatty liver than in those subjects with a healthy liver. Fatty liver is reversible and may be associated with a good prognosis. Kojima et al. [7] observed that fatty liver appeared when BMI increased and disappeared when BMI decreased. If the underlying cause can be treated, for example by weight control through improvements in lifestyle, fatty liver can be cured. However, due to the absence of severe symptoms or the fact that clinical values are often in the normal range in mild fatty liver, lifestyle guidance can be difficult to implement and the need for patient behavior modification may not be recognized.
Although visceral fat area can be measured by X-ray or computed tomography, this is not feasible in all patients in terms of both cost effectiveness and radiation exposure. Abdominal ultrasound is the most useful examination for diagnosis of fatty liver, but this is not routinely performed at occupational health checkups, and the condition is thus seldom diagnosed. Studies have reported that even in non-obese patients, fatty liver is a risk factor for lifestyle-related diseases [16-18]. Fatty liver is strongly correlated with visceral fat and is associated with a high rate of coexisting lifestyle-related diseases such as hypertension, diabetes, and hyperlipidemia [19,20]. For this reason, a marker that is able to to screen persons at high risk for fatty liver is needed. In a study examining the prevalence of lifestyle-related disease based on the severity of fatty liver, Hamaguchi et al. [8] reported that severe fatty liver was associated with a higher prevalence of hypertension, diabetes, and hyperlipidemia than was mild fatty liver.
The subjects in the present study were employees of 99 companies that incorporate ultrasound examination into their health checkups as an optional test. The majority of the 225 companies that implement health checkups offer only the regular health checkup items defined by the government. Ultrasound examination may be offered as an optional test only by those companies that actively promote health management among employees and that can afford it in their benefit program. Currently in Japan, ultrasound examination is recommended for individuals aged ≥ 35 years. Among the employees at the 99 companies that provided ultrasound examination, we compared those aged ≥ 35 years who underwent ultrasound examination (30,002 individuals) with those who did not (52,618 individuals). No significant difference was observed between those aged ≥ 35 years who underwent ultrasound examination and those who did not in mean age (46.4 and 45.3 years) or mean BMI (23.3 and 23.2, respectively). Therefore, selection bias was not regarded as a significant concern in the present study.
In conclusion, when using WC measurements as a marker for fatty liver, it is recommended that individuals with values higher than the cut-off point (85.0 cm, men; 80.0 cm, women) should receive further evaluation by abdominal ultrasound. This would lead to not only an early reduction in the risk of cardiovascular events, but also to the prevention of non-alcoholic steatohepatitis, which is a concern if fatty liver is allowed to progress, as well as a reduction in the risk of cirrhosis and malignant tumors such as hepatocellular carcinoma.
This study found a high prevalence of fatty liver in males in their 40s and females in their 50s. Therefore, we used WC measurements as a preventive marker for fatty liver. This was found to be a simple and easy screening method in our participants.
The findings of the present study demonstrate the potential of WC measurement as a simple, cost-effective screening tool to identify individuals at high risk of fatty liver due to accumulated visceral fat, and thus our findings are significant for the field of occupational health. Ultrasound evaluation of people identified as high risk enables early detection of fatty liver and thus encourages lifestyle improvements at an early stage, thereby decreasing the risk of cerebrovascular disease onset.
Acknowledgments
We wish to sincerely thank everyone at the Association for Preventive Medicine of Japan who cooperated in this study.
Footnotes
An abstract of this paper was presented at the 67th annual meeting of the Japanese Society of Public Health (November 2008, Fukuoka).
No potential conflict of interest relevant to this article was reported.
References
- 1.Standard medical examination and counseling guidance program (latest version) [Internet] Tokyo (Japan): Ministry of Health, Labour and Welfare; 2007. [cited 2012 Mar 30]. Available from: http://www.mhlw.go.jp/bunya/shakaihosho/iryouseido01/info03a.html. [Google Scholar]
- 2.Kato Y, Yoshida T, Nagao K, Futamura Y. The relation between fatty liver and the deadly quartet. Jpn Soc Human Dry Dock. 2003;18:354–358. Japanese. [Google Scholar]
- 3.Otsuki K. The relationship between ultrasonograhically diagnosed fatty liver disease, metabolic syndrome and insulin resintance in adaults. J Gastroenterol Mass Surv. 2004;42:346–351. Japanese. [Google Scholar]
- 4.Shiwa T, Kawanami Y, Yokoyama T. The medical examination data of fatty liver cases and the prediction of fatty liver. J Gastroenterol Mass Surv. 2004;42:580–584. Japanese. [Google Scholar]
- 5.Kondo T, Abe M, Ueyama J, Kimata A, Yamamoto K, Hori Y. Use of waist circumference and ultrasonographic assessment of abdominal fat distribution in predicting metabolic risk factors in healthy Japanese adults. J Physiol Anthropol. 2009;28:7–14. doi: 10.2114/jpa2.28.7. [DOI] [PubMed] [Google Scholar]
- 6.Aoyagi K, Kusano Y, Takamura N, Abe Y, Osaki M, Une H. Obesity and cardiovascular risk factors among men and women aged 40 years and older in a rural area of Japan. J Physiol Anthropol. 2006;25:371–375. doi: 10.2114/jpa2.25.371. [DOI] [PubMed] [Google Scholar]
- 7.Kojima S, Watanabe N, Numata M, Ogawa T, Matsuzaki S. Increase in the prevalence of fatty liver in Japan over the past 12 years: analysis of clinical background. J Gastroenterol. 2003;38:954–961. doi: 10.1007/s00535-003-1178-8. [DOI] [PubMed] [Google Scholar]
- 8.Hamaguchi M, Kojima T, Fujii K, Nakajima T, Okuda J, Ida K. Correlations between fatty liver, high brightness pancreas diagnosed by abdominal ultrasonography, and lie-style related disease. Health Eval Promot. 2003;30:567–574. Japanese. [Google Scholar]
- 9.Miki T. Best cut off index of histogram on fatty liver. Jpn Soc Sonogr. 2005;30:9–17. Japanese. [Google Scholar]
- 10.Kawabe H, Yokoyama H, Saitou I. Usefulness of the AST/ALT ratio as the predictive marker of fatty liver evaluated by the ultrasonography. Jpn Med J. 2003;4127:22–26. Japanese. [Google Scholar]
- 11.Yamada H, Hukuzawa Y, Seko R, Kakuta H, Hukasawa H, Kakumu S. Probability of fatty liver-onset and effects of decreased body weight in patients with multiple risk syndrome using logistic regression analysis. J Jpn Diabetes Soc. 2007;50:9–15. Japanese. [Google Scholar]
- 12.Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311:158–161. doi: 10.1136/bmj.311.6998.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sato K, Dohke M, Mizutome N, Kimura R, Makuri A, Matsui A, Hanawa N, Oashi K. Evaluation of metabolic syndrome with respect to the waist circumference and visceral fat area. Ningen Dock. 2008;23:558–563. Japanese. [Google Scholar]
- 14.Saibara T, Toda K, Onishi S. Geriatric and sexial aspects in fatty liver and NASH. Kan Tan Sui. 2005;51:227–233. Japanese. [Google Scholar]
- 15.Inoue S, Torikai Y, Kanai Y. The difference between obesity and adiposity. Medicina. 2005;42:192–195. Japanese. [Google Scholar]
- 16.Kim HJ, Kim HJ, Lee KE, Kim DJ, Kim SK, Ahn CW, Lim SK, Kim KR, Lee HC, Huh KB, Cha BS. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Intern Med. 2004;164:2169–2175. doi: 10.1001/archinte.164.19.2169. [DOI] [PubMed] [Google Scholar]
- 17.Otsuki K. Relationship between ultrasonographic fatty liver and lifestyle-related disease in non-obese adults. J Gastroenterol Mass Surv. 2002;40:542–546. Japanese. [Google Scholar]
- 18.Onodera H, Shibuya D, Iwasaki T, Matsui A, Ono H, Machida N, Abe T. Fatty liver cases without obesity in relation to serum liver function tests, serum lipids levels, alcohol consumption and cigarette smoking habits. Jpn Soc Human Dry Dock. 2002;17:378–382. Japanese. [Google Scholar]
- 19.Uno K, Ikeda S, Yanagimoto N, Tani R, Mori N, Yokotani T, Toba S, Goto A. Study on fatty liver cases without obesity detected in health examination or human dry dock. Jpn Soc Human Dry Dock. 2004;19:574–579. Japanese. [Google Scholar]
- 20.Isono E, Izumi T, Nishida J, Araki R, Mochizuki K, Yoshimura Y, Ichikawa K, Nishiyama H, Bandai Y. Evaluation of hyperlipidemia, hypertention, and fasting hyperglycemia as complications of non-alcoholic fatty liver disease and insulin resistance. Ningen Dock. 2007;22:46–50. Japanese. [Google Scholar]