Abstract
Context
Estimates of DSM-IV disorder prevalence are high; stringent criteria to define need for services are desired.
Objective
To present US national data on the prevalence and sociodemographic correlates of 12-month serious emotional disturbance (SED), defined by the US Substance Abuse and Mental Health Services Administration, from the National Comorbidity Survey Replication Adolescent Supplement.
Design
The National Comorbidity Survey Replication Adolescent Supplement is a national survey of DSM-IV anxiety, mood, behavior, and substance disorders among US adolescents.
Setting
Dual-frame household and school samples of US adolescents.
Participants
Total of 6483 pairs of adolescents aged 13 to 17 (interviews) and parents (questionnaires).
Main Outcome Measures
The DSM-IV disorders were assessed with the World Health Organization Composite International Diagnostic Interview and validated with blinded clinical interviews based on the Schedule for Affective Disorders and Schizophrenia for School-Age Children. Serious emotional disturbance was operationalized as a DSM-IV/Composite International Diagnostic Interview disorder with a score of 50 or less on the Children’s Global Assessment Scale (ie, moderate impairment in most areas of functioning or severe impairment in at least 1 area). Concordance of Composite International Diagnostic Interview SED diagnoses with blinded Schedule for Affective Disorders and Schizophrenia for School-Age Children diagnoses was good.
Results
The estimated prevalence of SED was 8.0%. Most SEDs were due to behavior (54.5%) or mood (31.4%) disorders. Although respondents with 3 or more disorders made up only 29.0% of those with 12-month DSM-IV/Composite International Diagnostic Interview disorders, they constituted 63.5% of SEDs. Predictive effects of high comorbidity were significantly greater than the product of their disorder-specific odds ratios and consistent across disorder types. Associations of sociodemographic variables with SED were generally nonsignificant after controlling for disorder type and number.
Conclusions
The high estimated 12-month prevalence of DSM-IV disorders among US adolescents is largely due to mild cases. The significant between-disorder differences in risk of SED and the significant effect of high comorbidity have important public health implications for targeting interventions.
Epidemiologic surveys consistently find that more than one-fourth of all US children and adolescents meet criteria for 1 or more recent DSM-IV mental disorders.1,2 This proportion is so high that it raises questions about the clinical significance of DSM-IV criteria3 and about estimates of the magnitude of unmet need for treatment.4 Consistent with these questions, research has shown that, as with adults,5 prevalence estimates of child and adolescent mental disorders decrease substantially when special impairment requirements are imposed in making diagnoses.6 Nonetheless, precise data on the population severity distributions of child and adolescent mental disorders are lacking.
This report presents data on severity distributions for DSM-IV mental disorders among the adolescents who participated in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A).7 To our knowledge, the NCS-A is the first survey in the United States to assess a wide range of DSM-IV disorders in a national sample using fully structured diagnostic interviews. We distinguish DSM-IV disorders that do vs do not qualify for the Substance Abuse and Mental Health Services Administration definition of serious emotional disturbance (SED),8 focusing on disorder-specific distributions and sociodemographic correlates. Previous research6,9 has estimated that 4% to 13% of US adolescents meet 12-month criteria for SED, although none of the previous studies of SED was based on a national sample using a fully structured diagnostic interview. Previous NCS-A reports described the sample design,7,10 measurements,11 and validity of diagnostic assessments7,10–12 along with lifetime prevalence of DSM-IV disorders.13 A companion article2 in this issue documents that the disorders assessed in the NCS-A are highly prevalent and persistent throughout adolescence.
METHODS
SAMPLE
The companion article2 in this issue describes the sample in detail. In brief, adolescents (aged 13–17) were interviewed from February 5, 2001, through January 31, 2004, in parallel household (n=904; 86.8% response rate) and school (n=9244; 82.6% response rate) samples.7,10 The high percentage (72.0%) of non-participating initially selected schools in the school sample was replaced with matched replacement schools that were shown in a methodologic study to yield prevalence data comparable with those obtained in the household sample from students in nonparticipating schools.10 One parent-surrogate of each participating adolescent was asked to complete a self-administered questionnaire about the adolescent’s developmental history and mental health (82.5% conditional response rate in the household and 83.7% in the school sample). This report focuses on the 6483 adolescent-parent pairs with complete data. Incomplete parent data were taken into consideration by weighting procedures discussed elsewhere.7,10
Parental written informed consent and adolescent assent were obtained before completing the surveys. Each respondent was given $50 for participation. The recruitment consent procedures were approved by the human subjects committees of both Harvard Medical School and the University of Michigan. Weights were used for within-household probability of selection and deviation from census population sociodemographic or geographic distributions, and the household and school samples were then merged with adjustments for differential design effects.7,10
MEASURES
Diagnostic Assessment
As described in more detail in the companion article,2 adolescents were administered the fully structured Composite International Diagnostic Interview (CIDI)14 modified to simplify language and use examples relevant to adolescents.11 The 15 DSM-IV disorders that were assessed included mood disorders, anxiety disorders, behavior disorders, eating disorders, and substance disorders. There were no other exclusionary diagnoses. The DSM-IV distress and impairment criteria and organic exclusion rules were used in making diagnoses. Hierarchy rules were used with the exceptions of oppositional-defiant disorder with or without conduct disorder and substance abuse with or without dependence. Briefer parent questionnaires assessed disorders for which parent reports have previously been shown to play a large part in diagnosis: behavior disorders15 and depression and dysthymia.16 As described in more detail in the companion article,2 an NCS-A clinical reappraisal study documented good concordance between diagnoses based on the CIDI and diagnoses based on blinded clinical reappraisal interviews.12 Parent and adolescent reports in the CIDI were combined at the symptom level using an “or” rule (except in the case of attention-deficit disorder for which only parent reports were used for evidence of low validity of adolescent reports) because results showed that this optimized concordance with blinded clinical diagnoses.
Disorder Severity
The Substance Abuse and Mental Health Services Administration defines SED as “a diagnosable mental, behavioral, or emotional disorder of sufficient duration to meet diagnostic criteria specified within DSM-III-R,” and “that resulted in functional impairment which substantially interferes with or limits the child’s role or functioning in family, school, or community activities.”8(p29425) This definition was operationalized in the NCS-A clinical reappraisal study by defining respondents with 1 or more 12-month DSM-IV Schedule for Affective Disorders and Schizophrenia for School-Age Children disorders as serious (SED) cases if they scored 50 or less on the Children’s Global Assessment Scale (CGAS).17 A CGAS score of 50 or less can be obtained either by having moderate impairment in functioning in most areas of living (eg, fears and anxieties that lead to gross avoidance behavior, episodes of aggression, or antisocial behavior) or severe impairment in at least 1 area (eg, suicidal preoccupation and ruminations or frequent anxiety attacks). Respondents who were not classified as having an SED were classified as moderate cases if they had CGAS scores of 51 through 60 (variable functioning, with sporadic difficulties in several but not all areas of living) and mild cases otherwise.
Although the CIDI adolescent survey and parent questionnaire included many measures of impairment, they could not be used to construct CGAS scores directly because the latter are based on clinical ratings. However, we were able to use these survey measures to generate a close approximation of CGAS. This was done using regression-based imputation, a standard approach for establishing individual-level estimates of missing data in large-scale surveys in which information on important variables is missing for some cases.18 In this approach, data available in the survey that are known from some other data set (in this case, the NCS-A clinical reappraisal sample) to predict the missing variable are used to generate a prediction equation for that variable in the other data set. The coefficients from that prediction equation are then used in the main survey to generate predicted values of the missing variable. When the predictors are strongly related to the missing variable, as was the case in the NCS-A impairment variables predicting CGAS scores in the NCS-A clinical reappraisal sample, quite accurate individual-level measures of the missing variable can be generated in this way.
Cross-validated stepwise regression analysis performed in the NCS-A clinical reappraisal sample using information about 12-month DSM-IV disorder prevalence and severity was used to predict clinical ratings of SED. (Detailed results are available on request from the corresponding author.) The area under the receiver operating characteristic curve, a measure of concordance that is fairly insensitive to prevalence,19 showed that the estimate of SED based on the prediction equation had strong individual-level concordance with clinical ratings in comparison with both moderate or mild (0.85) and mild (0.82) disorders. On the basis of these results, the coefficients in the prediction equation were used to estimate whether each respondent in the larger NCS-A sample met criteria for serious, moderate, or mild 12-month disorder. These imputed scores were then used as outcomes in a series of logistic regression analyses performed in the total NCS-A sample to study the substantive predictors of SED. To build in information about imputation inaccuracy to significance tests, the multiple imputation20 method was used to adjust estimates of standard errors.
Sociodemographic Variables
Sociodemographic variables examined as predictors of SED include age, sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), parental educational level (less than high school, high school, some college, or college graduate), family income (low [defined as no more than 1.5 times the official federal poverty line], low-average [1.5–3 times the poverty line], high-average [3–6 times the poverty line], or high [≥6 times the poverty line]), number of siblings, birth order, number of biological parents living with the adolescent, urbanicity (census metropolitan areas, nonmetropolitan urban counties, and rural counties), and census region (Northeast, Midwest, South, or West).
ANALYSIS METHODS
The distribution of disorder severity was examined for each 12-month DSM-IV/CIDI disorder using cross-tabulations. Multivariate regression models were then used to predict log-odds of SED among respondents with disorders from information about the type and number of disorders. This analysis was performed only in the subsample of respondents with a 12-month DSM-IV/CIDI disorder because the focus was on the predictors of severity among respondents with disorders. Both additive and nonadditive models were considered, and the best-fitting model was selected using the Bayesian information criterion.21 The regression coefficients and standard errors from the best-fitting model were exponentiated to produce odds ratios (ORs) and 95% CIs. Population-attributable risk proportions (PARPs) were calculated to estimate the proportion of serious cases associated with each disorder that would not have occurred in the absence of a given predictor disorder or set of disorders under the model if the regression coefficients represented causal effects of the predictor disorders. The simulations were produced by generating a predicted probability of each value on the severity distribution twice for each respondent from the best-fitting model: the first time using all model coefficients and the second time setting to zero the coefficients associated with the predictor disorder(s) of interest. Population-attributable risk proportion was defined as 1 - R, where R represents the ratio of the mean predicted probability in the second specification divided by the mean predicted probability in the first specification. So, for example, if the mean predicted probability decreases by 30% after deleting a given set of predictor disorders, PARP would be defined as 0.30.
As the NCS-A data are both clustered and weighted, the design-based method of jackknife repeated replications based on the 42 NCS-A sampling strata was used to produce standard errors of logistic regression coefficients. The coefficients and standard errors were exponentiated to produce ORs and 95% CIs. The significance of predictor sets was evaluated using Wald F tests based on design-adjusted coefficient variance-covariance matrices. Statistical significance was consistently evaluated using 2-sided tests with an α level of .05.
RESULTS
PREVALENCE AND SEVERITY OF 12-MONTH SED
The estimated prevalence (SE) of 12-month SED is 8.0% (1.3%) among NCS-A respondents with complete adolescent-parent data. Given that the estimated 12-month prevalence of any disorder is 42.6% (1.2%), then 18.8% (8.0% ÷ 42.6%) of respondents with a disorder meet criteria for SED (Table 1). Much higher proportions of cases are rated either mild (58.2%) or moderate (22.9%). The highest proportions rated serious are associated with conduct disorder (59.8%) and oppositional-defiant disorder (43.8%). Adolescents who meet criteria for 3 or more 12-month disorders are significantly more likely to be rated serious (43.1%) than those with 2 disorders (12.1%) or 1 disorder (8.5%) (F2,39 = 17.7; P <.001). Indeed, although respondents with 3 or more disorders make up less than one-third (29.0%) of people with 12-month disorders, they constitute nearly two-thirds (63.5%) of those with SED.
Table 1.
Disorder-Specific Severity Distributions of 12-Month DSM-IV/CIDI Disorders in 6483 Adolescentsa
| Disorder | Severity Distribution, % (SE)
|
||
|---|---|---|---|
| Seriousb | Moderateb | Mildb | |
| Mood disorders | |||
| Major depressive episode/dysthymia | 35.6 (5.2) | 31.0 (6.4) | 33.4 (6.7) |
| Bipolar disorderc | 30.5 (5.8) | 26.5 (12.1) | 43.1 (10.7) |
| Any mood disorder | 32.4 (4.5) | 29.8 (7.4) | 37.8 (7.7) |
| Anxiety disorders | |||
| Agoraphobiad | 22.1 (7.4) | 25.9 (15.5) | 52.0 (15.9) |
| Generalized anxiety disorder | 32.0 (8.6) | 21.0 (8.9) | 47.1 (9.0) |
| Social phobia | 23.9 (5.1) | 23.8 (9.3) | 52.3 (9.0) |
| Specific phobia | 19.6 (5.1) | 16.8 (11.6) | 63.7 (10.6) |
| Panic disordere | 35.4 (12.6) | 21.2 (10.3) | 43.4 (10.9) |
| Posttraumatic stress disorder | 27.7 (7.0) | 23.8 (11.1) | 48.5 (10.4) |
| Separation anxiety disorder | 25.0 (8.1) | 25.5 (8.9) | 49.5 (10.9) |
| Any anxiety disorder | 18.4 (3.4) | 19.6 (10.3) | 62.0 (9.6) |
| Behavior disorders | |||
| Attention-deficit/hyperactivity disorder | 35.4 (8.2) | 40.6 (14.0) | 24.0 (10.6) |
| Oppositional-defiant disorder | 43.8 (7.8) | 24.3 (6.8) | 31.9 (8.9) |
| Conduct disorder | 59.8 (8.4) | 21.1 (9.4) | 19.2 (8.6) |
| Eating disordersf | 27.5 (10.0) | 26.0 (15.1) | 46.5 (16.6) |
| Any behavior disorder | 33.6 (5.1) | 30.2 (9.4) | 36.2 (9.6) |
| Substance disorders | |||
| Alcohol abuseg | 26.4 (5.7) | 21.4 (8.2) | 52.1 (9.2) |
| Drug abuseg | 33.8 (6.1) | 19.2 (7.3) | 47.0 (7.1) |
| Any substance disorder | 29.1 (5.0) | 19.2 (6.7) | 51.7 (7.1) |
| No. of disorders | |||
| Any disorder | 18.8 (2.9) | 22.9 (9.8) | 58.2 (9.5) |
| Exactly 1 disorder | 8.5 (3.8) | 19.1 (12.4) | 72.4 (12.1) |
| Exactly 2 disorders | 12.1 (2.5) | 25.3 (10.9) | 62.5 (10.4) |
| ≥3 Disorders | 43.1 (6.2) | 28.3 (7.1) | 28.6 (7.0) |
Abbreviation: CIDI, Composite International Diagnostic Interview.
See Table 2 in the companion article2 in this issue for information on 12-month prevalence of disorders.
See the “Disorder Severity” subsubection in the “Measures” section of the “Methods” section for definitions of serious, moderate, and mild disorders.
Bipolar disorder includes bipolar I, bipolar II, and subthreshold bipolar disorder.
With or without a history of panic disorder.
With or without agoraphobia.
Eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating behavior.
With or without dependence.
MULTIVARIATE ASSOCIATIONS OF DISORDER TYPE AND NUMBER WITH SED
The best-fitting model to predict SED among respondents with 1 or more 12-month disorders includes 14 dummy predictor variables for type of disorder (compared with the omitted category of separation anxiety disorder) plus summary measures from exactly 2 to 4 or more distress disorders (ie, generalized anxiety disorder, post-traumatic stress disorder, separation anxiety disorder, major depression, or dysthymia) or behavior disorders. (Detailed results of model-fitting are available on request.) The type-of-disorder coefficients are significant as a set (F13, 28= 52.9; P <.001), indicating that disorder types differ in risk of SED (Table 2). By far the highest OR is associated with conduct disorder (18.4), followed by depression (4.5) and panic disorder (3.9).
Table 2.
Best-fitting Model of Predictive Associations Between Type and Number of 12-Month DSM-IV/CIDI Disorders and 12-Month SED Among 2647 Respondents With 1 or More 12-Month Disordersa
| Disorder | OR (95% CI) | PARPb |
|---|---|---|
| Mood disorders | ||
| Major depressive episode/dysthymia | 4.5* (3.8–5.5) | 30.0 |
| Bipolar disorderc | 0.9 (0.7–1.3) | 2.2 |
| Any mood disorder | … | 31.4 |
| Anxiety disorders | ||
| Agoraphobiad | 0.8 (0.4–1.3) | 1.5 |
| Generalized anxiety disorder | 1.6* (1.2–2.3) | −0.6 |
| Social phobia | 1.3* (1.0–1.7) | 2.2 |
| Specific phobia | 1.6* (1.3–2.0) | 9.8 |
| Panic disordere | 3.9* (2.6–5.9) | 2.3 |
| Posttraumatic stress disorder | 2.2* (1.3–3.6) | 2.9 |
| Separation anxiety disorderf | 1.0 | −2.2 |
| Any anxiety disorder | … | 10.9 |
| Behavior disorders | ||
| Attention-deficit/hyperactivity disorder | 3.1* (2.3–4.2) | 8.4 |
| Oppositional-defiant disorder | 2.5* (1.9–3.4) | 15.6 |
| Conduct disorder | 18.4* (13.6–25.0) | 35.9 |
| Eating disordersg | 1.0 (0.7–1.5) | −1.3 |
| Any behavior disorder | … | 54.5 |
| Substance disorders | ||
| Alcohol abuseh | 1.3 (0.9–1.8) | −1.3 |
| Drug abuseh | 1.3* (1.1–1.6) | 2.8 |
| Any substance disorders | … | 1.9 |
| No. of distress/behavior disorderi | ||
| Exactly 2 disorders | 0.8 (0.6–1.2) | … |
| Exactly 3 disorders | 1.0 (0.5–1.9) | … |
| ≥4 Disorders | 6.1* (1.5–24.7) | … |
Abbreviations: CIDI, Composite International Diagnostic Interview; OR, odds ratio; PARP, population-attributable risk proportions; SED, serious emotional disturbance.
Based on a model that includes predictors for 14 of the 15 types of disorders (compared with the omitted category of separation anxiety disorder); counts of 2, 3, and 4 or more distress or behavior disorders; and controls for independent sociodemographic variables (ie, age at interview, sex, and race/ethnicity). See Table 2 in the companion article2 in this issue for information on 12-month prevalence of disorders. By independent sociodemographic variables we mean the subset of sociodemographic variables that could not plausibly be caused by the respondent’s SED. This was the best-fitting model from a wide variety of models compared using the Bayesian information criterion as the measure of model fit. Model selection was not sensitive to the criterion used because other criteria examined also selected this as the best-fitting model. The 14 disorder-specific ORs differ significantly among themselves (F13,29 = 52.9; P < .001), whereas the 3 number-of-disorders coefficients are significant as a set (F3,39 = 3.4; P = .03). Asterisks indicate OR is significant using 2-sided tests with an α level of .05.
The PARP is the proportion of cases of SED predicted under the model to be due to each of the disorders considered here. See the “Analysis Methods” subsection in the “Methods” section for a description of the simulation method used to calculate PARP. The PARP estimates do not sum to 100% because PARP is calculated by deleting 1 disorder or class of disorders from the model at a time, resulting in the effects of comorbidity being included in each of the estimates.
Bipolar disorder includes bipolar I, bipolar II, and subthreshold bipolar disorder.
With or without a history of panic disorder.
With or without agoraphobia.
Separation anxiety disorder is the contrast category, with an implicit OR of 1.0.
Eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating behavior.
With or without dependence.
No predictor variable for having exactly 1 disorder was included in the model because this would have been collinear with the coefficients associated with the individual disorders. The disorder-specific coefficients consequently can be interpreted as effects of pure disorders (ie, disorders that occur to respondents who have exactly 1 disorder), whereas the coefficients associated with numbers of disorders can be interpreted as deviations from the ORs associated with the products of these disorder-specific effects among respondents with more than 1 disorder.
The number-of-disorders coefficients, which can be considered global interactions between number and type of disorders, are also significant as a set (F3,39=3.4; P =.03) because of a strongly elevated OR associated with having 4 or more disorders (6.1).
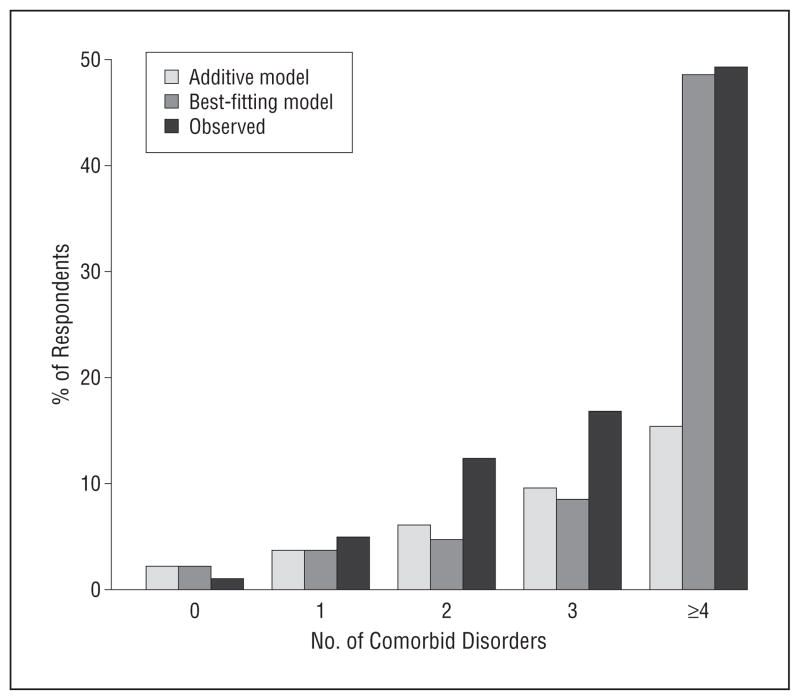
This elevated OR means that incremental increases in ORs associated with high comorbidity are greater than the product of their disorder-specific ORs. The dramatic increase in risk of SED among adolescents with 4 or more disorders can be seen graphically by comparing the observed distribution with the predicted probabilities of this outcome among respondents with 1, 2, 3, and 4 or more disorders in the additive and interactive models. The Figure shows clearly that the interactive model is much more consistent with the observed data than is the additive model.
Figure.
Comparison of the observed distribution of serious emotional disturbance by number of comorbid disorders. The predicted distributions are based on an additive model and on the best-fitting interactive model.
The fact that the interactive model with a single term for 4 or more disorders fits the observed data better than a model that allowed for a separate interaction between number and each of the 15 separate types of disorder means that the interactive effect of number of disorders is fairly consistent across the range of disorder types considered here. That is, the multiplier of the 4-way interaction coefficient over the expected value based on an additive model is relatively constant for all the 4-way interactions in the data. Further exploratory analysis found no evidence of differential importance of particular disorders in the 292 distinct 4-way interactions observed among disorders in the sample. (Detailed results are available on request.)
POPULATION-ATTRIBUTABLE RISK PROPORTIONS
Calculation of PARPs shows that much higher proportions of SED are due to behavior disorders (54.5%) than to mood (31.4%), anxiety (10.9%), or substance (1.9%) disorders (Table 2). The PARP components across all disorders sum to more than 100% because the calculation of PARP is made by deleting a single disorder at a time, which means that the effects of comorbidity are counted multiple times. The disorders with the highest PARPs are conduct disorder (35.9%), major depression (30.0%), oppositional-defiant disorder (15.6%), specific phobia (9.8%), and attention-deficit/hyperactivity disorder (8.4%). The high PARP for conduct disorder occurs despite a relatively low prevalence (5.4%) because of the high OR of conduct disorder predicting SED (18.4). The high PARP for depression, in comparison, is due to the conjunction of a high prevalence (13.3%) with a high OR (4.5). The lower, but nonetheless substantial, PARPs associated with oppositional-defiant and attention-deficit/hyperactivity disorders are due to intermediate prevalence (8.3%–6.3%) and moderately elevated ORs (2.5–3.1), whereas the high PARP associated with specific phobia is due to high prevalence (16.3%) in conjunction with a modestly elevated OR (1.6). Eating disorders are the only behavior disorders without significantly elevated ORs, raising the question whether eating disorders should be thought of as behavior disorders.
SOCIODEMOGRAPHIC CORRELATES
Sociodemographic variables are significant overall predictors of SED among respondents with 12-month disorders (F25,14 = 250.3; P < .001) (Table 3). Relative odds in the multivariate model are elevated among respondents who are age 16 (1.5 compared with ages 13–14), whose parents are high school graduates or had some post–high school education (1.5–1.6 compared with college graduates), and who live with neither or only 1 biological parent (5.2-1.9, respectively, compared with those living with both parents). Serious emotional disturbance is significantly less prevalent among non-Hispanic blacks (0.6 compared with non-Hispanic whites). No other significant associations exist in the multivariate model between any of the sociodemographic variables considered here and SED. Further analyses found that bivariate associations do not differ markedly from the multivariate associations reported here. (Detailed results are available on request.)
Table 3.
Sociodemographic Correlates of 12-Month DSM-IV/CIDI SED Without and With Controls for Type and Number of 12-Month Disorders Among 2647 Respondents With 1 or More Disordersa
| Correlate | OR (95% CI)
|
|
|---|---|---|
| Without Controls | With Controls | |
| Age, y | ||
| 17–18 | 1.2 (0.7–1.9) | 1.0 (0.8–1.3) |
| 16 | 1.5* (1.1–2.0) | 1.1 (0.9–1.3) |
| 15 | 1.2 (0.8–1.7) | 1.0 (0.8–1.3) |
| 13–14 | 1.0 [Reference] | 1.0 [Reference] |
| F3,38 | 2.6 | 0.3 |
| Sex | ||
| Male | 1.0 [Reference] | 1.0 [Reference] |
| Female | 1.0 (0.8–1.2) | 1.0 (0.9–1.2) |
| F1,38 | 0.0 | 0.6 |
| Race | ||
| Hispanic | 1.4 (0.7–2.6) | 1.2 (0.9–1.5) |
| Non-Hispanic black | 0.6* (0.4–0.9) | 0.8* (0.7–1.0) |
| Other | 0.8 (0.5–1.2) | 0.9 (0.7–1.2) |
| Non-Hispanic white | 1.0 [Reference] | 1.0 [Reference] |
| F3,38 | 2.9* | 4.9* |
| Parental educational levelb | ||
| Less than high school | 1.1 (0.8–1.6) | 1.0 (0.9–1.2) |
| High school graduate | 1.5* (1.1–2.1) | 1.2 (1.0–1.4) |
| Some college | 1.6 (1.0–2.5) | 1.2 (1.0–1.5) |
| College graduate | 1.0 [Reference] | 1.0 [Reference] |
| F3,38 | 2.7 | 2.0 |
| Family incomec | ||
| Low | 0.8 (0.5–1.3) | 1.0 (0.8–1.2) |
| Low-average | 1.1 (0.6–1.8) | 1.1 (0.9–1.4) |
| High-average | 1.0 (0.8–1.4) | 1.1 (0.9–1.3) |
| High | 1.0 [Reference] | 1.0 [Reference] |
| F3,38 | 0.8 | 0.9 |
| Census region | ||
| Northeast | 1.9 (0.6–6.0) | 1.1 (0.8–1.5) |
| Midwest | 1.3 (0.8–2.2) | 1.2 (0.9–1.5) |
| South | 1.0 (0.6–1.6) | 1.0 (0.8–1.3) |
| West | 1.0 [Reference] | 1.0 [Reference] |
| F3,38 | 2.4 | 1.4 |
| Urbanicity | ||
| Census major metropolitan area | 1.3 (0.8–2.0) | 1.0 (0.7–1.2) |
| Other urbanized county | 1.1 (0.8–1.5) | 1.0 (0.8–1.2) |
| Rural county | 1.0 [Reference] | 1.0 [Reference] |
| F2,39 | 0.7 | 0.1 |
| No. of biological parents living with the adolescent | ||
| 0 | 5.2* (2.3–11.4) | 1.3 (1.0–1.7) |
| 1 | 1.9* (1.3–2.6) | 1.1 (0.9–1.4) |
| 2 | 1.0 [Reference] | 1.0 [Reference] |
| F2,39 | 9.1* | 2.7 |
| Birth order | ||
| Oldest | 1.1 (0.6–1.8) | 0.8 (0.6–1.1) |
| Middle | 0.9 (0.5–1.5) | 0.8 (0.6–1.2) |
| Youngest | 1.0 (0.6–1.7) | 0.8 (0.6–1.2) |
| Only | 1.0 [Reference] | 1.0 [Reference] |
| F3,38 | 1.2 | 0.5 |
| No. of siblingsd | ||
| ≥3 | 1.1 (0.7–1.6) | 1.0 (0.8–1.2) |
| 2 | 1.1 (0.8–1.4) | 1.0 (0.8–1.2) |
| 0–1 | 1.0 [Reference] | 1.0 [Reference] |
| F2,39 | 0.3 | 0.2 |
Abbreviations: CIDI, Composite International Diagnostic Interview; OR, odds ratio; SED, serious emotional disturbance.
Based on a multivariate model that includes all the sociodemographic correlates as predictors of SED estimated in the subsample of respondents with 1 or more 12-month disorders. The model with controls also includes as predictors the variables in the best-fitting model of type and number of disorders in Table 2. See Table 1 for the distribution of the sociodemographic predictor variables. Asterisks indicate OR is significant using 2-sided tests with an α level of .05.
Educational level was coded at the higher of the 2 levels when parents differed in levels of education.
For classification of family income, see the “Sociodemographic Variables” subsubsection in the “Measures” subsection in the “Methods” section.
Although respondents with no siblings are coded 0 on all 3 number of siblings dummy variables, the category of having 0 siblings is identical to the category of being an only child in the birth order variable. As a result, the coefficients in the number of siblings variable (2 or ≥3 siblings) are contrasted with the deleted category of having 1 sibling.
Sociodemographic variables also predict SED when we control for type and number of disorders (F25,14 = 119.4; P< .001), although the only individually significant sociodemographic factor is being non-Hispanic black (0.8 compared with non-Hispanic whites). We found no significant interactions between type and number of disorders and sociodemographic variables. (Detailed results are available on request.)
COMMENT
Three important sampling limitations are noteworthy: that the school-level response rate was quite low, that the individual-level response rate was relatively low, and that the sample excluded adolescents not enrolled in school, the homeless, and non-English speakers. Methodologic analyses reported elsewhere10 reduce concern about the first limitation because no evidence of bias due to school replacement was found. However, the finding in previous methodologic studies that nonrespondents have rates of mental illness higher than those of respondents implies that the second limitation most likely led prevalence estimates to be conservative and possibly biased estimates of disorder-specific associations with SED.22 The third limitation reduces the generalizability of our findings.
Two other noteworthy limitations involve measurement. First, diagnoses were based on fully structured adolescent lay interviews and parent self-administered questionnaires, the latter assessing only a subset of diagnoses. Second, imputation was used to define disorder severity. Concern about the first limitation is somewhat reduced by the good concordance of survey diagnoses with blinded clinical reappraisal diagnoses,12 although survey prevalence estimates of simple phobia and oppositional-defiant disorder are substantially higher than clinical estimates. The second limitation is likely to have introduced imprecision but not bias into the prevalence estimate of SED, but it could have introduced bias into estimates of the associations of specific disorders with SED to the extent that we predicted SED associated with some disorders better than SED associated with other disorders.23
In the context of these limitations, the finding that the high overall 12-month prevalence of DSM-IV/CIDI disorders in the NCS-A is due largely to mild cases (58.2%) is consistent with previous studies of children24 and adults.25 Serious emotional disturbance is found among 8.0% of all adolescents (18.8% × 42.6%), an estimate in the middle of the range of previous prevalence estimates.9,24,26 The finding that behavior disorders are associated with the highest risk of SED (3 of the 5 highest PARPs) is consistent with data from a number of previous studies.24,26,27 The finding that depression and panic disorder are also associated with an elevated risk of SED is consistent with evidence from previous studies of both children24 and adults.5
The finding of only 8.0% of 12-month disorders meeting criteria for SED is not a reflection of the overdiagnosis of 12-month disorder in the CIDI. Indeed, as noted earlier, our clinical reappraisal study showed clearly that the CIDI does not substantially overdiagnose DSM-IV disorders.12 It is quite a different matter to ask whether these results suggest that the current DSM-IV system overdiagnoses, a position taken by a number of commentators.28,29 However, this is an issue well beyond the scope of this report. A related issue is whether these results imply that only a small proportion of youths with a DSM-IV disorder needs treatment. Again, this is an issue that goes beyond the scope of this article. However, a case might be made for the appropriateness of nonintensive treatment for even the mildest of cases (eg, short-term behavioral treatment of specific phobias). Furthermore, mild adolescent disorders are powerful predictors of serious adult disorders.30
The finding of a strong positive interaction involving high comorbidity (≥4 disorders) predicting SED is broadly consistent with evidence in previous studies that comorbidity is associated with high severity.31–33 The existence of this interaction in conjunction with evidence from the NCS-A as well as other studies34–36 that a substantial proportion of adolescents have high comorbidity raises the question whether the parcellation of symptom clusters into many different disorders in DSM-IV is correct. However, this issue far exceeds the scope of this article. A more tractable issue is that the interaction has important implications for intervention targeting. In particular, if the primary goal of intervention is to treat the bulk of youths with current serious disorders, our results suggest that the focus should be on disorders with the highest PARPs, which include a trio of 3 behavior disorders (conduct disorder, oppositional-defiant disorder, and attention-deficit/hyperactivity disorder) and depression, with a special emphasis on multimorbidity37 (ie, ≥4 disorders). However, if cost-effectiveness is also an intervention goal, we have to consider that previous research has found treatment effectiveness to be lower among patients with certain,38 although not all,39 comorbidities. The rational response to these complexities is far from obvious because we are aware of no data to evaluate the relative effectiveness of intervening early with pure cases to prevent the onset of comorbidity vs targeting cases that are already comorbid as a focus of special attention. Some consideration of the timing and content of comorbidity is needed to optimize the value of outreach efforts from a public health perspective.
We found few sociodemographic correlates of SED among respondents with 12-month disorders. However, in the earlier companion article in this issue2 we documented significant sociodemographic correlates of 12-month prevalence of individual disorders consistent with those found in previous studies. This means that sociodemographic variables, while systematically correlated with the presence vs absence of disorders, are for the most part not systematically related to severity of disorders among people with 12-month disorders. The strongest sociodemographic correlate of severity of 12-month disorders is not living with both biological parents. However, this association becomes nonsignificant when we control for type and number of disorders, suggesting that type and number of disorders mediate the association between living with biological parents and SED. Further analysis (results available on request) showed that the high prevalence of behavior disorders among adolescents not living with their biological parents explains the gross predictive effect of this sociodemographic variable. Race/ethnicity is the only sociodemographic variable that remained significantly related to severity after controlling for type of disorder, with non-Hispanic blacks having significantly lower odds of SED than non-Hispanic whites with the same profile of disorders. This finding might be thought of as inconsistent with the results of the National Health Interview Survey, which reported higher rates of SED among non-Hispanic black and Hispanic youths than non-Hispanic whites,40 but the comparison is inappropriate because we focused in this report on predicting severity among adolescents with disorders rather than among all adolescents. The seeming inconsistency of our failure to find strong socioeconomic predictors of SED with previous studies26 can be understood in the same way, as the juxtaposition of these results can be interpreted as meaning that the associations of sociodemographic variables with SED are due to more basic associations with specific disorders. Serious emotional disturbance, according to this interpretation, is much more a function of multivariate disorder profiles than sociodemographic predispositions, with high comorbidity playing an especially critical role. Finally, whether the bulk of youths with SED are the unlucky few who happen to have 4 or more separate disorders or those who have an as-yet undefined single disorder that is poorly characterized in the current DSM-IV system is an issue that, although beyond the scope of this investigation, requires close examination in future studies.
Acknowledgments
Funding/Support: The NCS-A is supported by grants U01-MH60220, R01-MH66627, and U01MH060220-09S1 from the National Institute of Mental Health with supplemental support from the National Institute on Drug Abuse, the Substance Abuse and Mental Health Services Administration, the Robert Wood Johnson Foundation (grant 044780), and the John W. Alden Trust. The work of Dr Merikangas is supported by the National Institute of Mental Health Intramural Research Program. The work of Dr Zaslavsky is supported by grant R01-MH66627 from the National Institute of Mental Health. The World Mental Health Data Coordination Centers have received grants R01-MH070884, R13-MH066849, R01-MH069864, and R01-MH077883 from the National Institute of Mental Health; R01-DA016558 from the National Institute on Drug Abuse; and FIRCA R03-TW006481 from the Fogarty International Center of the National Institutes of Health; and support from the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, and the Pan American Health Organization. The World Mental Health Data Coordination Centers have also received unrestricted educational grants from AstraZeneca; Bristol-Myers Squibb; Eli Lilly and Company; GlaxoSmithKline, Inc; Ortho-McNeil; Pfizer, Inc; sanofi-aventis; and Wyeth.
Role of the Sponsors: The sponsors had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; and the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Kessler takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors had full access to all the data in the study.
Disclaimer: The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or US Government.
Online-Only Material: Visit http://www.archgenpsychiatry.com to listen to an author podcast about this article.
Additional Information: A complete list of NCS-A publications can be found at http://www.hcp.med.harvard.edu/ncs. A public use version of the NCS-A data set is available for secondary analysis. Instructions for accessing the dataset can be found at http://www.hcp.med.harvard.edu/ncs/index.php. The NCS-A is performed in conjunction with the World Health Organization World Mental Health Survey Initiative. A complete list of World Mental Health publications can be found at http://www.hcp.med.harvard.edu/wmh/.
Additional Contributions: We thank the staff of the World Mental Health Data Collection and Data Analysis Coordination Centers for assistance with instrumentation, fieldwork, and consultation on data analysis.
Financial Disclosure: Dr Kessler has been a consultant for AstraZeneca; Analysis Group; Bristol-Myers Squibb; Cerner-Galt Associates; Eli Lilly and Company; GlaxoSmithKline, Inc; HealthCore, Inc; Health Dialog; Integrated Benefits Institute; John Snow, Inc; Kaiser Permanente; Matria, Inc; Mensante; Merck & Co, Inc; Ortho-McNeil Janssen Scientific Affairs; Pfizer, Inc; Primary Care Network; Research Triangle Institute; sanofi-aventis; Shire US, Inc; SRA International, Inc; Takeda Global Research & Development; Transcept Pharmaceuticals, Inc; and Wyeth-Ayerst; has served on advisory boards for Appliance Computing II; Eli Lilly & Company; Mindsite; Ortho-McNeil Janssen Scientific Affairs; and Wyeth-Ayerst; and has had research support for his epidemiologic studies from Analysis Group, Inc; Bristol-Myers Squibb; Eli Lilly and Company; EPI-Q; GlaxoSmithKline, Inc; Johnson & Johnson Pharmaceuticals; Ortho-McNeil Janssen Scientific Affairs; Pfizer, Inc; sanofi-aventis; and Shire US, Inc.
References
- 1.Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders, I: methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44(10):972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, He J, Koretz D, McLaughlin KA, Sampson NA, Merikangas KR. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the US National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry. doi: 10.1001/archgenpsychiatry .2011.160. [published online ahead of print December 5, 2011] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Regier DA, Kaelber CT, Rae DS, Farmer ME, Knauper B, Kessler RC, Norquist GS. Limitations of diagnostic criteria and assessment instruments for mental disorders: implications for research and policy. Arch Gen Psychiatry. 1998;55 (2):109–115. doi: 10.1001/archpsyc.55.2.109. [DOI] [PubMed] [Google Scholar]
- 4.Spitzer RL. Diagnosis and need for treatment are not the same. Arch Gen Psychiatry. 1998;55(2):120. doi: 10.1001/archpsyc.55.2.120. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaffer D, Fisher P, Dulcan MK, Davies M, Piacentini J, Schwab-Stone ME, Lahey BB, Bourdon K, Jensen PS, Bird HR, Canino G, Regier DA. The NIMH Diagnostic Interview Schedule for Children version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA study (Methods for the Epidemiology of Child and Adolescent Mental Disorders study) J Am Acad Child Adolesc Psychiatry. 1996;35(7):865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Avenevoli S, Costello EJ, Green JG, Gruber MJ, Heeringa S, Merikangas KR, Pennell BE, Sampson NA, Zaslavsky AM. National Comorbidity Survey Replication Adolescent Supplement (NCS-A), II: overview and design. J Am Acad Child Adolesc Psychiatry. 2009;48(4):380–385. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration. Final notice establishing definitions for (1) children with a serious emotional disturbance, and (2) adults with a serious mental illness. Fed Regist. 1993;58(96):29422–29425. [Google Scholar]
- 9.Friedman RM, Katz-Leavy JW, Manderscheid R, Sondheimer D. Prevalence of serious emotional disturbance in children and adolescents. In: Manderscheid R, Sonnenschein M, editors. Mental Health, United States: 1996. Washington, DC: US Government Printing Office; 1996. pp. 71–89. DHHS publication (SMA) 96–3098. [Google Scholar]
- 10.Kessler RC, Avenevoli S, Costello EJ, Green JG, Gruber MJ, Heeringa S, Merikangas KR, Pennell BE, Sampson NA, Zaslavsky AM. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Int J Methods Psychiatr Res. 2009;18(2):69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merikangas K, Avenevoli S, Costello J, Koretz D, Kessler RC. National Comorbidity Survey Replication Adolescent Supplement (NCS-A), I: background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48(4):367–369. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Avenevoli S, Green J, Gruber MJ, Guyer M, He Y, Jin R, Kaufman J, Sampson NA, Zaslavsky AM. National Comorbidity Survey Replication Adolescent Supplement (NCS-A), III: concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry. 2009;48(4):386–399. doi: 10.1097/CHI.0b013e31819a1cbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston C, Murray C. Incremental validity in the psychological assessment of children and adolescents. Psychol Assess. 2003;15(4):496–507. doi: 10.1037/1040-3590.15.4.496. [DOI] [PubMed] [Google Scholar]
- 16.Braaten EB, Biederman J, DiMauro A, Mick E, Monuteaux MC, Muehl K, Faraone SV. Methodological complexities in the diagnosis of major depression in youth: an analysis of mother and youth self-reports. J Child Adolesc Psychopharmacol. 2001;11(4):395–407. doi: 10.1089/104454601317261573. [DOI] [PubMed] [Google Scholar]
- 17.Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A Children’s Global Assessment Scale (CGAS) Arch Gen Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 18.Brick JM, Kalton G. Handling missing data in survey research. Stat Methods Med Res. 1996;5(3):215–238. doi: 10.1177/096228029600500302. [DOI] [PubMed] [Google Scholar]
- 19.Kraemer HC. Evaluating Medical Tests: Objective and Quantitative Guidelines. Newburk Park, CA: Sage; 1992. [Google Scholar]
- 20.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley and Sons; 2004. [Google Scholar]
- 21.Kass RE, Raftery AE. Bayes factors. J Am Stat Assoc. 1995;90(430):773–795. [Google Scholar]
- 22.Kessler RC, Little RJ, Groves RM. Advances in strategies for minimizing and adjusting for survey nonresponse. Epidemiol Rev. 1995;17(1):192–204. doi: 10.1093/oxfordjournals.epirev.a036176. [DOI] [PubMed] [Google Scholar]
- 23.Sinharay S, Stern HS, Russell D. The use of multiple imputation for the analysis of missing data. Psychol Methods. 2001;6(4):317–329. [PubMed] [Google Scholar]
- 24.Costello EJ, Angold A, Burns BJ, Erkanli A, Stangl DK, Tweed DL. The Great Smoky Mountains Study of Youth: functional impairment and serious emotional disturbance. Arch Gen Psychiatry. 1996;53(12):1137–1143. doi: 10.1001/archpsyc.1996.01830120077013. [DOI] [PubMed] [Google Scholar]
- 25.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS National Comorbidity Survey Replication. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 26.Costello EJ, Messer SC, Bird HR, Cohen P, Reinherz H. The prevalence of serious emotional disturbance: a re-analysis of community studies. J Child Fam Stud. 1998;7(4):411–432. [Google Scholar]
- 27.Costello EJ, Angold A, Keeler GP. Adolescent outcomes of childhood disorders: the consequences of severity and impairment. J Am Acad Child Adolesc Psychiatry. 1999;38(2):121–128. doi: 10.1097/00004583-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Horwitz AV, Wakefield JC. The Loss of Sadness: How Psychiatry Transformed Normal Sorrow into Depressive Disorder. New York, NY: Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- 29.Lane C. Shyness: How Normal Behavior Became a Sickness. New Haven, CT: Yale University Press; 2007. [Google Scholar]
- 30.Kessler RC, Merikangas KR, Berglund P, Eaton WW, Koretz DS, Walters EE. Mild disorders should not be eliminated from the DSM-V. Arch Gen Psychiatry. 2003;60(11):1117–1122. doi: 10.1001/archpsyc.60.11.1117. [DOI] [PubMed] [Google Scholar]
- 31.Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M. The Maudsley long-term follow-up of child and adolescent depression, 2: suicidality, criminality and social dysfunction in adulthood. Br J Psychiatry. 2001;179:218–223. doi: 10.1192/bjp.179.3.218. [DOI] [PubMed] [Google Scholar]
- 32.Kuhne M, Schachar R, Tannock R. Impact of comorbid oppositional or conduct problems on attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1997;36(12):1715–1725. doi: 10.1097/00004583-199712000-00020. [DOI] [PubMed] [Google Scholar]
- 33.Lewinsohn PM, Rohde P, Seeley JR. Adolescent psychopathology, III: the clinical consequences of comorbidity. J Am Acad Child Adolesc Psychiatry. 1995;34(4):510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- 34.Fergusson DM, Horwood LJ, Lynskey MT. Prevalence and comorbidity of DSM-III-R diagnoses in a birth cohort of 15-year-olds. J Am Acad Child Adolesc Psychiatry. 1993;32(6):1127–1134. doi: 10.1097/00004583-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Kessler RC, Avenevoli S, Costello EJ, Green JG, Lakoma M, McLaughlin KA, Sampson NA, Zaslavsky AM, Merikangas KR. Lifetime prevalence and comorbidity of DSM-IV disorders in the NCS-R Adolescent Supplement (NCS-A) Psychol Med. doi: 10.1017/S0033291712000025. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. J Consult Clin Psychol. 1996;64(3):552–562. [PubMed] [Google Scholar]
- 37.Angst J, Sellaro R, Ries Merikangas K. Multimorbidity of psychiatric disorders as an indicator of clinical severity. Eur Arch Psychiatry Clin Neurosci. 2002;252(4):147–154. doi: 10.1007/s00406-002-0357-6. [DOI] [PubMed] [Google Scholar]
- 38.Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, Holder D. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. J Am Acad Child Adolesc Psychiatry. 1998;37(9):906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Ollendick TH, Jarrett MA, Grills-Taquechel AE, Hovey LD, Wolff JC. Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention-deficit/hyperactivity disorder, and oppositional/conduct disorders. Clin Psychol Rev. 2008;28(8):1447–1471. doi: 10.1016/j.cpr.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 40.Mark TL, Buck JA. Characteristics of US youths with serious emotional disturbance: data from the National Health Interview Survey. Psychiatr Serv. 2006;57(11):1573–1578. doi: 10.1176/ps.2006.57.11.1573. [DOI] [PubMed] [Google Scholar]