Summary
We performed aneurysm embolization in seven patients using a self-expandable Neuroform stent (Boston Scientific/Target, Fremont, CA) and coils to cover the aneurysm neck and fill the aneurysm sac. Seven patients with an average age of 45 were treated in the period from October 2002 to July 2003.
The aneurysm lesions involved the basilar trunk in one case, the basilar-superior cerebellar artery in one case, the internal carotid artery in four cases, and the middle cerebral artery in one case. The ruptured lesions involved the internal carotid artery in one case and the middle cerebral artery in one case. We used a Neuroform stent measuring 4.5 × 20 mm in four cases, 4.5 × 15 mm in two cases, 3.5 × 20 mm in one case, and 3.5 × 15 mm in one case. We performed aneurysm coil embolization after Neuroform stenting in all cases without development of neurological deficits caused by the interventional procedure.
In performing these procedures, we investigated the efficacy and limitations of the Neuroform stent system for intracranial aneurysms. The advantages of Neuroform self-expanding stents include better flexibility and adaptability to different vessel sizes, but this stent system presents various technical difficulties during delivery.
Key words: intracranial aneurysm, broad neck aneurysm, Neuroform stent and coils
Introduction
Stent deployment can now be performed for treatment of intracranial aneurysms and especially broad neck aneurysms, due to recent advances in interventional neuroradiology1,2.
Here, we present our current experience with minimally invasive endovascular repair using the Neuroform stent system and coils to cover the aneurysm neck and fill the aneurysm sac, and we discuss the efficacy and limitations of the Neuroform stent system for intracranial aneurysms.
Material and Methods
We performed aneurysm embolization in seven cases using a self-expandable Neuroform stent and coils to cover the aneurysm neck and fill the aneurysm sac. We performed this procedure in seven patients aged 32 to 63years, from October 2002 to July 2003. The interventional procedures were done under general anesthesia in all cases. The aneurysm lesions involved the basilar trunk in two cases, the internal carotid artery in four cases (ophth in three and cavernous in one) and the middle cerebral artery (pseudoaneurysm) in one case. The ruptured lesions involved the internal carotid-ophthalmic artery in one case and the middle cerebral artery in one case. We used Neuroform stents measuring 4.5 × 20 mm in four cases, 4.5 × 15 mm in two cases, 3.5 × 20 mm in one case and 3.5 × 15 mm in one case. In all cases we performed aneurysm coil embolization, with the microcatheter being passed through the stent strut immediately after Neuroform stenting in six cases and three weeks after stenting in one case.
Results
In all cases we were able to perform aneurysm coil embolization after Neuroform stenting without neurological deficits being caused by the interventional procedure. However, one patient (MCA pseudoaneurysm) died due to secondary abscess formation due to a parenchymal haematoma.
Regarding stent delivery, technical difficulties were experienced in four cases using the ordinary Neuroform stent delivery system. Because of this, we changed the delivery method in one of the four cases and used a coil pusher instead of the Neuroform stent stabilizer in the other three cases, in order to deliver the stents. Follow-up was performed using MRA, CTA, DSA or a combination thereof.
Representative cases
Case 1
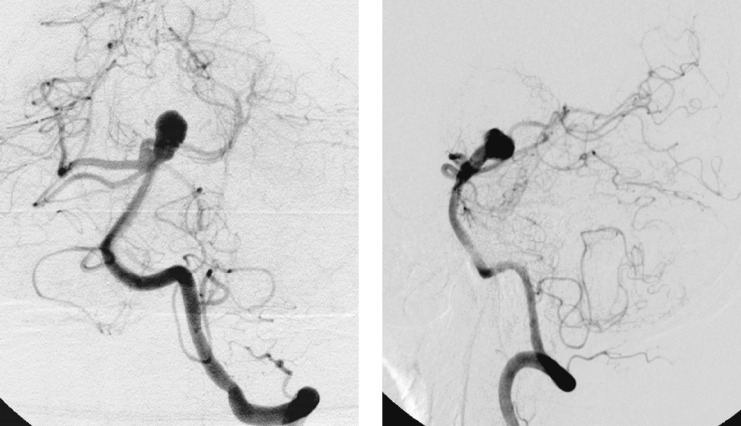
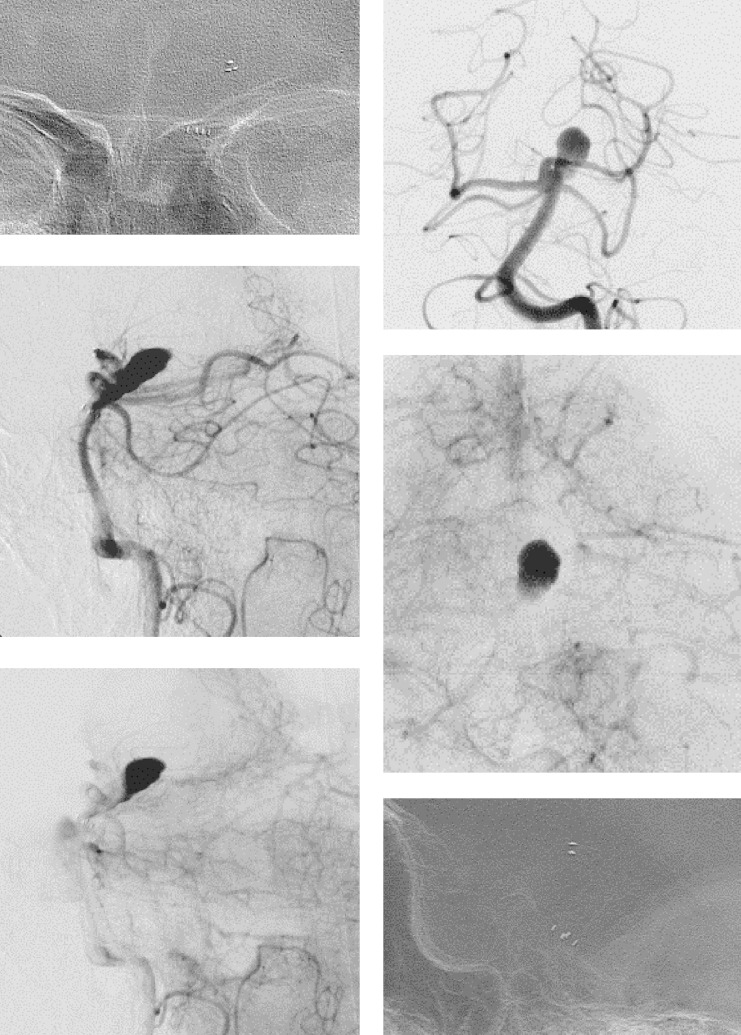
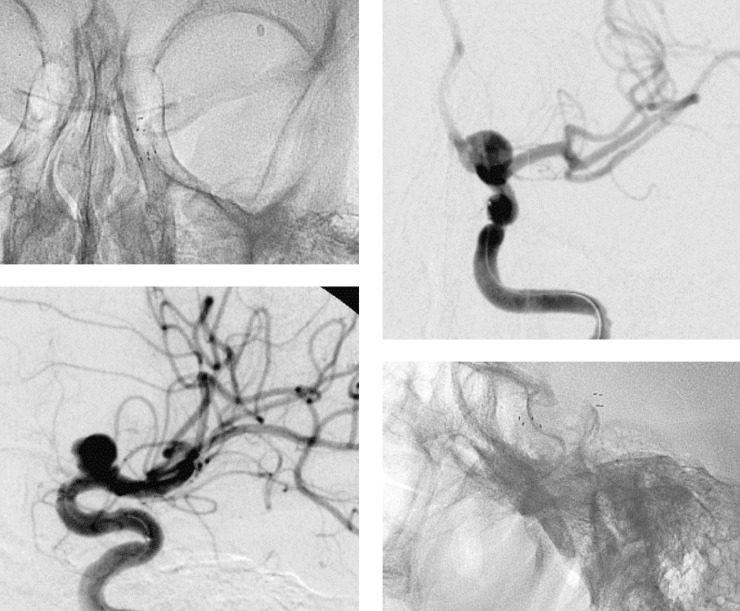
A 62-year old male was shown to have a nonruptured left basilar-superior cerebral artery aneurysm in left vertebral angiography (figure 1). We performed aneurysm embolization using a Neuroform stent of size 4.5 × 20 mm to initially cover the aneurysm neck (figure 2), and we then used coiling to fill the aneurysm sac as the microcatheter was passed through the stent strut immediately after Neuroform stenting (figure 3). It was not particularly difficult to deliver the Neuroform stent to the lesion site using the usual Neuroform delivery system.
Figure 1.
Left vertebral angiography (A: Anterior-Posterior view, B: Lateral view) showing a left basilar-superior cerebellar artery aneurysm.
Figure 2.
Left vertebral angiography and a skull X-ray (A: A-P, B: lat.) recorded post-stenting.
Figure 3.
Left vertebral angiography and a skull X-ray (A: A-P, B: lat.) recorded post-coiling after stenting.
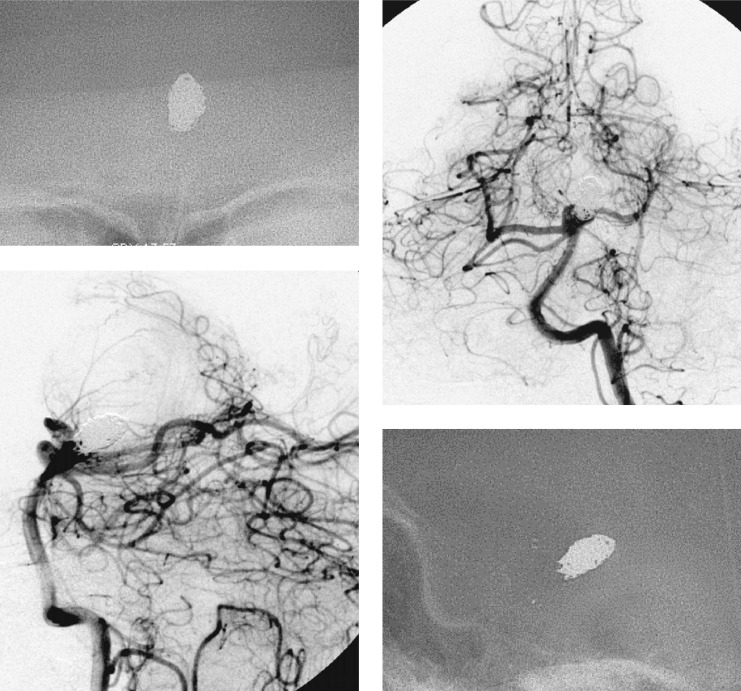
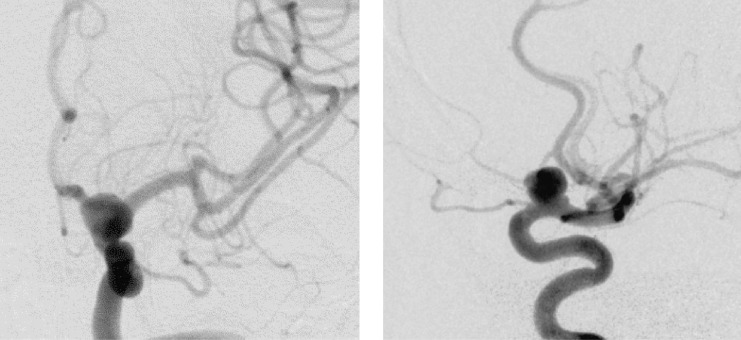
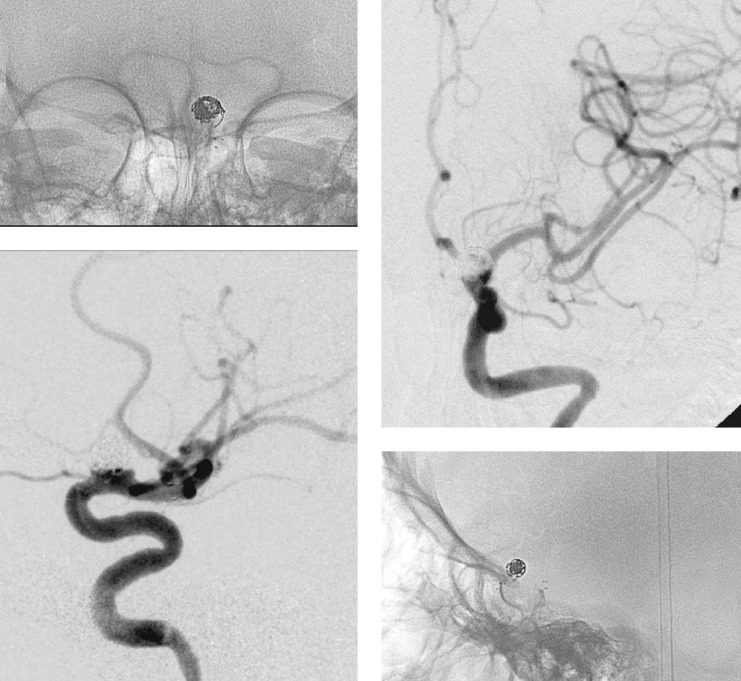
Case 2
A 44-year old female was shown to have a non-ruptured left internal carotid-ophthalmic artery aneurysm in left internal carotid angiography (figure 4). In this case, we were able to get the stent system to reach the lesion site without any particular difficulty, using the usual Neuroform delivery system. However, it was hard to deliver the Neuroform stent because proximal tortuous vessels prevented delivery of the stent to cover the aneurysm neck.
Figure 4.
Left internal carotid angiography (A: A-P;Anterior-Posterior view, B: lat.;Lateral view) showing a left internal carotid-ophthalmic artery aneurysm.
This problem may have been due to the weakness of the stabilizer in the delivery system. For this reason, we had no choice but to change the delivery system. The Neuroform stent (4.5 × 20 mm) was placed in a Rebar microcatheter (2.8 French), and then delivered using the whole Neuroform delivery catheter system to cover the aneurysm neck initially (figure 5). Coiling was then used to fill the aneurysm sac as the microcatheter passed through the stent strut immediately after Neuroform stenting (figure 6).
Figure 5.
Left internal carotid angiography and a skull X-ray (A: A-P, B: lat.) recorded post-stenting.
Figure 6.
Left internal carotid angiography and a skull X-ray (A: A-P, B: lat.) recorded post-coiling after stenting.
Discussion
In a previous study, nine patients with broad-necked intracranial aneurysms were treated with balloon-expanding stents (AVE, Medtronic) and coils, and the balloon-expanding stents seemed to provide a better haemodynamic impact on the aneurysmal cavities 1. However, balloon-expanding stent systems sometimes have various associated technical difficulties during delivery, even with non-tortuous and non-atherosclerotic vessels, because such stents are designed for coronary artery use.
We performed aneurysm embolization in seven cases using the self-expandable Neuroform stent, which was developed for intracranial vessels, and then used aneurysm coil embolization to cover the aneurysm neck and fill the aneurysm sac. These Neuroform stenting interventional procedures were performed without causing neurological deficits in any of the cases.
We also investigated the efficacy and limitations of the balloon-expandable stent system and the Neuroform stent system for intracranial aneurysms. Technical difficulties have been observed for the delivery of both stents types1,2. However, Neuroform self-expanding stents offers several advantages, compared with the balloon-expandable stents. These include better flexibility, adaptability to different vessel sizes, less risk of premature detachment at the treated site, and compatibility with MRI.
We consider the Neuroform stent system to be more effective for treatment of intracranial broad necked aneurysms, but it is still not a perfect system. We encountered problems with the delivery system, and problems associated with the stabilizer occurred in four of the seven cases and in cases with proximal tortuous vessels and atherosclerotic vessels. We coped with these difficulties and delivered the Neuroform stents in these cases by changing the delivery method in one case and using a coil pusher instead of the stabilizer in the other three cases.
Therefore, it is important to understand the characteristics of the Neuroform stent for use for an intracranial broad necked aneurysm, and to know how to deal with problems associated with the delivery system when these are encountered in situations similar to those that we experienced. We hope that development of a self-expandable Neuroform stent with safer and easier delivery to an intracranial aneurysm can be achieved. In fact, a second generation stent is now being developed by Boston Scientific, and according to information from the company, Neuroform2 has the characteristics of a lower deployment force and a 25% reduction in delivery force (unofficial data), compared with the first generation Neuroform stent used in the current study.
Conclusions
We investigated the efficacy and limitations of the Neuroform stent system for treatment of intracranial aneurysms. The advantages of Neuroform self-expanding stents include better flexibility and adaptability to different vessel sizes, but this stent system has various associated technical difficulties during delivery.
References
- 1.Han PP, Albuquerque FC, et al. Percutaneous intracranial stent placement for aneurysms. J. Neurosurgery. 2003;99:23–30. doi: 10.3171/jns.2003.99.1.0023. [DOI] [PubMed] [Google Scholar]
- 2.Broadbent LP, Moran CJ, et al. Management of neuroform stent dislodgement and misplacement. Am J Neuroradiol. 2003;24:1819–22. [PMC free article] [PubMed] [Google Scholar]