Abstract
Obesity in humans is associated with increased bone mass. Leptin, a hormone produced by fat cells, functions as a sentinel of energy balance, and may mediate the putative positive effects of body mass on bone. We performed studies in male C57Bl/6 wild type (WT) and leptin-deficient ob/ob mice to determine whether body mass gain induced by high fat intake increases bone mass and, if so, whether this requires central leptin signaling. The relationship between body mass and bone mass and architecture was evaluated in 9-week-old and 24-week-old WT mice fed a regular mouse diet. Femora and lumbar vertebrae were analyzed by micro computed tomography. In subsequent studies, slowly and rapidly growing ob/ob mice were injected in the hypothalamus with a recombinant adeno-associated virus containing the leptin gene (rAAV-lep) or a control vector, rAAV-GFP (green fluorescent protein). The mice were maintained on a regular control diet for 5 or 7 weeks and then subdivided into groups and either continued on the control diet or fed a high fat diet (45% of kcal from fat) for 8 weeks. In the WT mice, femoral and vertebral bone mass was positively correlated with body mass (Pearson’s r = 0.65–0.88 depending on endpoint). rAAV-lep therapy dramatically decreased body mass (−61%) but increased femur length. However, in the distal femur and lumbar vertebra, rAAV-lep therapy reduced cancellous bone volume/tissue volume, trabecular number and trabecular thickness, and increased trabecular spacing. The high fat diet increased body mass, irrespective of vector treatment. Total femur bone volume, length, cross-sectional volume, and cortical volume and thickness were increased in mice with increased body mass, independent of rAAV treatment. In the distal femur, increased body mass had no effect on cancellous architecture and there were no vector × body mass interactions. In WT mice, increased body mass resulted in increased (+33%) vertebral cancellous bone volume/tissue volume. Increased body mass had minimal independent effect on cancellous vertebral bone mass in ob/ob mice. Taken together, these findings suggest that increased body mass has a positive effect on femur cortical bone mass that is independent of leptin signaling.
Keywords: osteoporosis, peak bone mass, μCT, obesity, weight, body mass
1. Introduction
A low peak bone mass predisposes individuals to osteoporosis, a disease that contributes to over two million fractures annually in the United States alone [1]. The acquisition of bone mass occurs primarily during childhood and the decade following puberty, and is tightly coupled to energy metabolism. A low bone mass and increased fracture risk are associated with anorexia, whereas high bone mass and reduced fracture risk are associated with obesity [2, 3]. The increased bone mass in obese individuals has been attributed to systemic factors (e.g., elevated sex steroid and leptin levels) and increased skeletal loading due to increased body mass. Although body mass has a strong positive effect on bone mineral density in load-bearing bones of both sexes [4], lean body mass is more highly correlated with bone mass than is fat mass [5]. Furthermore, mechanical loading has direct effects on cultured osteoblasts and ex vivo dynamic loading stimulates bone formation [6]. In addition, disuse induced by sciatic neurotomy, hindlimb unloading, tendonotomy, casting or limb immobilization using a sling results in bone loss at the site(s) of immobilization [7]. Taken together, these observations suggest that increased weight bearing contributes, but may not be the sole factor, for determining the positive relationship between body mass and bone mass.
Leptin, the protein product of the ob (Lep) gene [8], is a pleiotropic hormone that acts on multiple organs, including bone. Leptin is produced predominantly by fat cells, functions as a sentinel of energy balance, and may influence bone metabolism. However, leptin has been variously reported to have bone anabolic, anti-resorptive, and anti-osteogenic effects [9–12].
The precise mechanisms of leptin action on the skeleton are not fully understood. In part, this is because the hormone has the potential to affect bone through multiple pathways; one or more indirect pathways involving central/hypothalamic relays [10, 13, 14] and a direct pathway involving the binding of leptin to its receptors on cartilage and bone cells [9, 11, 15–18]. The direct action of leptin on bone and cartilage cells is readily apparent in cell culture [15, 16, 18, 19]. Bone is highly innervated and some of the indirect effects of leptin on bone may be mediated through the sympathetic arm of the autonomic nervous system [20, 21]; the binding of leptin to its receptors in the hypothalamus stimulates the peripheral cells of the sympathetic nervous system to release noradrenalin which, in turn, could influence bone formation via adrenergic receptors expressed on osteoblasts [10, 14]. However, adrenergic receptors are widely distributed. Thus, changes in sympathetic tone could have collateral effects on bone. Additional indirect effects may be mediated through changes in systemic metabolic bone regulatory factors such as vitamin D, PTH, sex steroids, stress hormones, insulin, IL-6 and IGF-I [22–27].
The obese ob/ob mouse, which cannot produce leptin due to an inactivating mutation in the leptin gene, has skeletal abnormalities and exhibits a mosaic skeletal phenotype. Compared to wildtype (WT) mice, ob/ob mice have reduced bone length and reduced overall bone mass and strength [11, 12, 19, 28–30]. These findings suggest leptin is required for optimal peak bone growth and quality. However, ob/ob mice have increased cancellous bone in their vertebra [10, 29], suggesting that the skeletal response to leptin is bone-specific (long bones versus vertebrae) and/or compartment-specific (cortical versus cancellous envelope).
We have recently employed leptin gene transfer technology by non-replicative, non-immunogenic and non-pathogenic virus vector (rAAV) to augment leptin availability selectively in the hypothalamus and determine if hypothalamic leptin, in addition to reversing established obesity, corrects abnormalities in bone architecture in ob/ob mice [30]. In brief, long-duration (15 weeks) hypothalamic rAAV-lep gene therapy in ob/ob mice restored all bone measurements to values that did not differ from WT mice. Specifically, leptin gene therapy increased femur length and total femur bone volume and decreased distal femur cancellous bone volume. Circulating leptin was not detected in the rAAV-lep treated mice. We interpret the results as evidence that increasing hypothalamic leptin in ob/ob mice to levels sufficient to prevent obesity abolishes the skeletal abnormalities that accompany the inability to produce leptin. Importantly, an additional 15 weeks of hypothalamic leptin gene therapy (total 30 weeks) had no additional effect on femur length, total femur bone mass or cancellous bone volume in distal femur or lumbar vertebra.
The objective of the present study was to evaluate the effects of global leptin deficiency, and selective central repletion of leptin on the response of long bones and vertebrae to body mass gain induced by a high fat diet. To accomplish this goal, we investigated WT and ob/ob mice as well as the effects of hypothalamic leptin expression following a single intracerebroventricular (icv) injection of rAAV-lep.
2. Materials and Methods
2.1. Experiment 1
A preliminary study was performed to determine if a positive relationship between body mass and bone mass exists in normal mice fed a standard diet ad libitum. To accomplish this, 20 male 8-week-old C57BL/6 ( WT) mice were obtained from Jackson Laboratory (Bar Harbor, Maine). Ten mice were sacrificed one week after arrival. The remaining 10 animals were maintained (2–3 mice/cage) in a temperature- and light-controlled room and fed a normal diet (LM-485, Teklad, Madison, WI; caloric density 3.4 kcal/g, 11% of kcal from fat) ad libitum for an additional 15 weeks and sacrificed at 24 weeks of age. The experimental protocol was approved by the Institutional Animal Care and Use Committee at Oregon State University where the study was conducted. Two additional studies were performed to evaluate the role of leptin in mediating the skeletal response to increased body mass.
2.2. Experiment 2
Eight to ten-week-old, male, leptin-deficient ob/ob (weighing 40–50 g) mice (Jackson Laboratory, Bar Harbor, Maine) were used in the experiment. The animals were housed in individual cages in a temperature (21–23°C)- and light-controlled room (lights on 6am–6pm) under specific pathogen-free conditions. Food and water were available ad libitum to all mice. The experimental protocol was approved by the Institutional Animal Care and Use Committee at the University of Florida (Gainesville, FL) where the study was conducted.
2.2a. Construction and Packaging of rAAV Vectors
The rAAV-lep and rAAV-green fluorescent protein (rAAV-GFP, control vector) vectors were constructed and packaged as described elsewhere [31]. In brief, the vector pTR-CBA-Ob EcoRI fragment of pCR-rOb containing rat leptin cDNA was subcloned into rAAV vector plasmid pAAVβGEnh after deleting the EcoRI fragment carrying the β-glucoronidase cDNA sequence [32–36]. The control vector, rAAV-GFP, was similarly constructed to encode the GFP gene [32, 34–36].
2.2b. Vector Administration
For vector administration, the mice were anesthetized with sodium pentobarbital (60 mg/kg, ip), placed on a Kopf stereotaxic apparatus with mouse adapter for icv injection, and injected icv with either rAAV-lep (9×107 particles; n=17) or rAAV-GFP (9×107 particles; n=17). The coordinates employed for microinjector placement in the 3rd cerebroventricle were 0.3 mm posterior to bregma, 0.0 lateral to midline, and 4.2 mm below the dura [37]. Procedures to verify icv injections are detailed elsewhere [31–34, 37–43].
2.2c. Diets
At 7 weeks post-vector injection (16 weeks of age; an age when the mice are approaching skeletal maturity), rAAV-GFP and rAAV-lep groups were divided into two groups each: one group continued to consume the regular chow diet (control diet) (LM-485, Teklad, Madison, WI) and the other was switched to a high fat diet (45 % of kcal from fat, primarily from lard; Research Diets, New Brunswick, NJ; n= 8 – 9/group) fed ad libitum for 8 weeks. The caloric density of the control diet was 3.4 kcal/g, whereas the caloric density of the high fat diet was 4.7 kcal/g. The ingredient and nutrient composition of the two diets was not identical. However, according to the manufacturers, both diets were nutritionally complete. The mice were sacrificed at 24 weeks of age. Food intake, body mass, hormone levels (e.g., leptin and insulin), and hypothalamic mRNA expression in response to central rAAV-lep gene therapy in this experiment are detailed elsewhere [37].
2.3. Experiment 3
When placed on the high fat diet, the animals in experiment 2 were mature. Bone mass is rapidly accrued in the interval immediately following puberty. To establish the effect of growth rate, we performed an additional experiment in post-pubertal mice. The design for Experiment 3 was similar to Experiment 2 with the exception that 4-week-old, male, leptin-deficient ob/ob (weighing 27–31 g) and WT mice (16–18 g) (Jackson Laboratory, Bar Harbor, Maine) were used in the experiment. After a one-week acclimation, the ob/ob mice were anesthetized and injected with rAAV-lep or rAAV-GFP. The WT mice were left untreated. At 5 weeks post-vector injection (10 weeks of age), rAAV-GFP and rAAV-lep groups were divided into two groups each: one group continued to consume the control regular chow diet and the other was switched to the high fat diet consumed ad libitum for 8 weeks as in Experiment 2. At 10 weeks of age, the WT mice were also divided into two subgroups: one group continued to consume the regular control diet and the other was switched to the high fat diet. The mice were sacrificed at 18 weeks of age. The effect of central rAAV-lep gene therapy and high fat diet on body mass and hormone levels (e.g., leptin and insulin) in this experiment are detailed elsewhere [24].
2.4. Tissue Collection and Analyses
For tissue collection, the mice were anesthetized with sodium pentobarbital (60 mg/kg; ip) and killed by exsanguination. Femora and 3rd lumbar vertebrae (LV3) were excised for analysis. Micro computed tomography (microCT) was used for nondestructive three-dimensional evaluation of bone architecture. In mice from Experiments 1 and 2, right femora were scanned using a Scanco μCT40 scanner (Scanco Medical AG, Basserdorf, Switzerland) at a voxel size of 12 × 12 × 12 µm (x-ray voltage 55 kVP) and evaluated at a threshold of 265 (gray scale, 0–1,000) determined empirically. A similar procedure was used to scan LV3 in mice from Experiments 1, 2, and 3. Entire femora (cancellous + cortical bone) were evaluated followed by evaluation of cortical bone at the femoral midshaft and cancellous bone in the distal femoral metaphysis. For the femoral midshaft, 100 slices (1.2 mm) of bone were evaluated and total cross-sectional tissue volume (cortical and marrow volume, mm3), cortical volume (mm3), marrow volume (mm3) and cortical thickness (µm) were measured. For the femoral metaphysis, 200 slices (2.4 mm) of bone were measured and included secondary spongiosa only. Analysis of the lumbar vertebra included the total bone (Experiment 1 only) and the entire region of secondary spongiosa between the cranial and caudal growth plates. Direct cancellous bone measurements in the femur and lumbar vertebra included: cancellous bone volume (bone volume unadjusted for tissue volume, mm3), cancellous bone volume/tissue volume (volume of total tissue occupied by cancellous bone, %), trabecular thickness (mean thickness of individual trabeculae, µm), 4) trabecular number (number of trabeculae within the samples tissue, 1/mm), and trabecular separation (the distance between trabeculae, µm) [44].
2.5. Statistical Analysis
A Pearson’s correlation coefficient was used to determine the relationship between body mass and bone volume and architecture in 9- and 24-week-old WT mice fed control diet in Experiment 1. The effects of vector administration (with 2 levels, rAAV-GFP and rAAV-lep), body mass (with 2 levels: normal and high) and their interaction were investigated for each dependent variable using a two-way ANOVA. Least-squares means (LS-means) were produced when the interaction term was significant. Femur length and volume was not directly measured in several specimens (n= 9/34 distributed across treatment groups) in Experiment 2 due to minor damage, usually to the femoral head, during tissue recovery. A multiple imputation based on correlation of existing endpoints was used to estimate the missing values [45]. A t-test was used to evaluate diet effects on bone in WT mice in Experiment 3. All statistical analyses were performed using the SAS program (SAS, Cary, NC). Differences were considered significant at p<0.05. All data are presented as mean±SE.
3. Results
Experiment 1
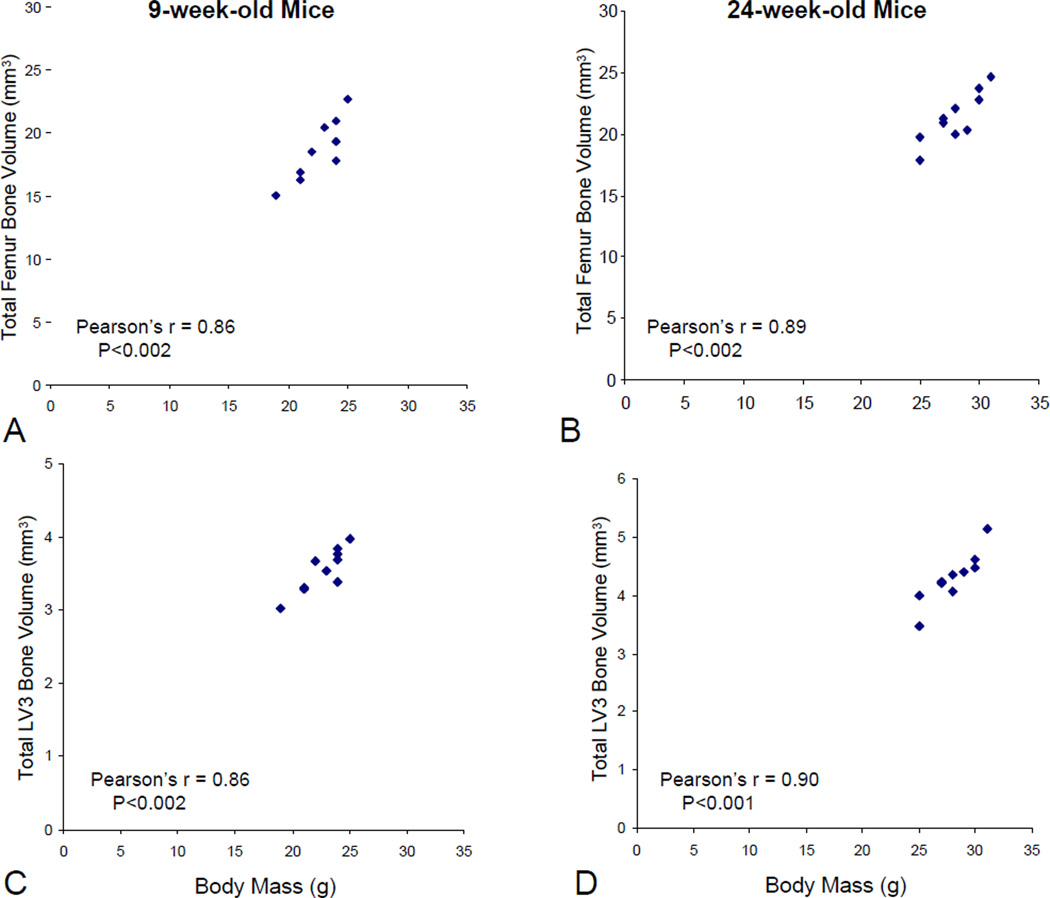
The objective of Experiment 1 was to determine the relationship between body mass and bone volume in growing (9 weeks old) and adult (24 weeks old) male C57BL/6 mice fed regular control diet. Positive correlations between terminal body mass and total femur bone volume were observed at both 9 and 24 weeks of age (Figure 1a–b). Positive correlations were likewise observed between body mass and cortical bone at the femoral midshaft (cross-sectional volume, cortical volume, and cortical thickness) as well as body mass and cancellous bone (cancellous bone volume and cancellous bone volume/tissue volume) in the distal femur in mice of both age groups (Table 1). The Pearson’s correlation coefficient ranged from 0.68 to 0.89, indicating that body mass accounted for 46–79% of variation in bone mass depending on site and age examined. Significant positive correlations were also noted between body mass and total vertebral bone volume (Figure 1c–d) and vertebral cancellous bone volume (Table 1) in both 9- and 24-week-old mice. The Pearson’s correlation coefficient ranged from 0.65 to 0.90 depending on site and age examined. In contrast, a significant relationship between body mass and vertebral cancellous bone volume adjusted for tissue volume was not detected in either the 9- or 24-week-old mice (Table 1).
Figure 1.
Correlation between body mass and total femur bone volume (a and b) and body mass and total vertebra (LV3) bone volume (c and d) in 9 and 24-week-old male C57BL/6 mice, respectively, fed standard mouse chow (Experiment 1).
Table 1.
Correlation between body mass and cortical bone in the midshaft femur and cancellous bone in the distal femur and 3rd lumbar vertebra (Experiment 1).
| 9-week-old Mice |
24-week-old Mice |
|||
|---|---|---|---|---|
| Pearson's r | P< | Pearson's r | P< | |
| Midshaft Femur | ||||
| Cross-sectional volume (mm3) | 0.81 | 0.005 | 0.88 | 0.01 |
| Cortical volume (mm3) | 0.88 | 0.001 | 0.86 | 0.02 |
| Cortical thickness (µm) | 0.80 | 0.006 | 0.75 | 0.05 |
| Distal Femur | ||||
| Bone volume (mm3) | 0.69 | 0.03 | 0.80 | 0.02 |
| Bone volume/Tissue volume (%) | 0.68 | 0.04 | 0.68 | 0.05 |
| Lumbar Vertebra | ||||
| Bone volume (mm3) | 0.65 | 0.04 | 0.82 | 0.004 |
| Bone volume/Tissue volume (%) | 0.59 | NS | 0.55 | NS |
NS, Not significant
Experiment 2
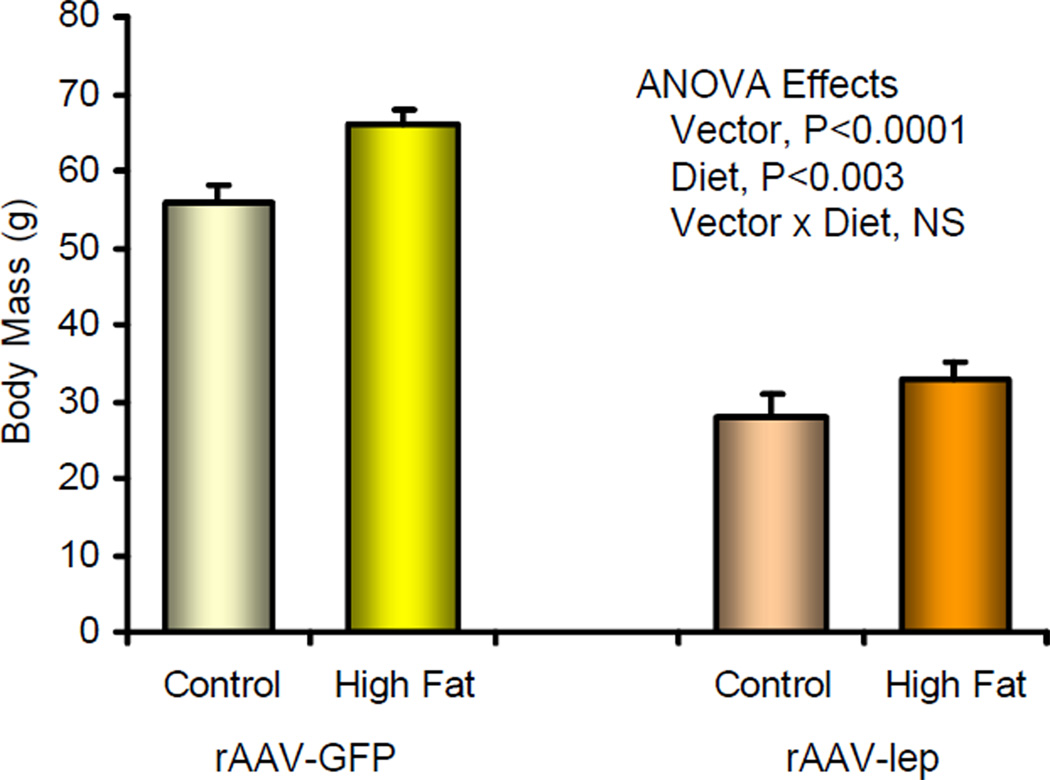
The objective of Experiment 2 was to evaluate the effects of global leptin deficiency and selective central leptin repletion on the skeletal response to body mass gain induced by high fat intake. The effect of central leptin gene therapy (vector) and high fat diet on body mass is shown in Figure 2. Central rAAV-lep treatment resulted in lower body mass, whereas high fat diet resulted in higher body mass. The high fat diet increased body mass in both the rAAV-GFP-treated and rAAV-lep-treated mice without increased caloric intake [37]. There was no interaction between vector administration and diet, indicating that high fat intake results in increased body mass, irrespective of central leptin.
Figure 2.
Effect of central leptin gene therapy and high fat diet on body mass in ob/ob mice administered either rAAV-GFP (control vector) or rAAV-lep icv (Experiment 2). All data are mean ± SE. NS, not significant, P>0.05.
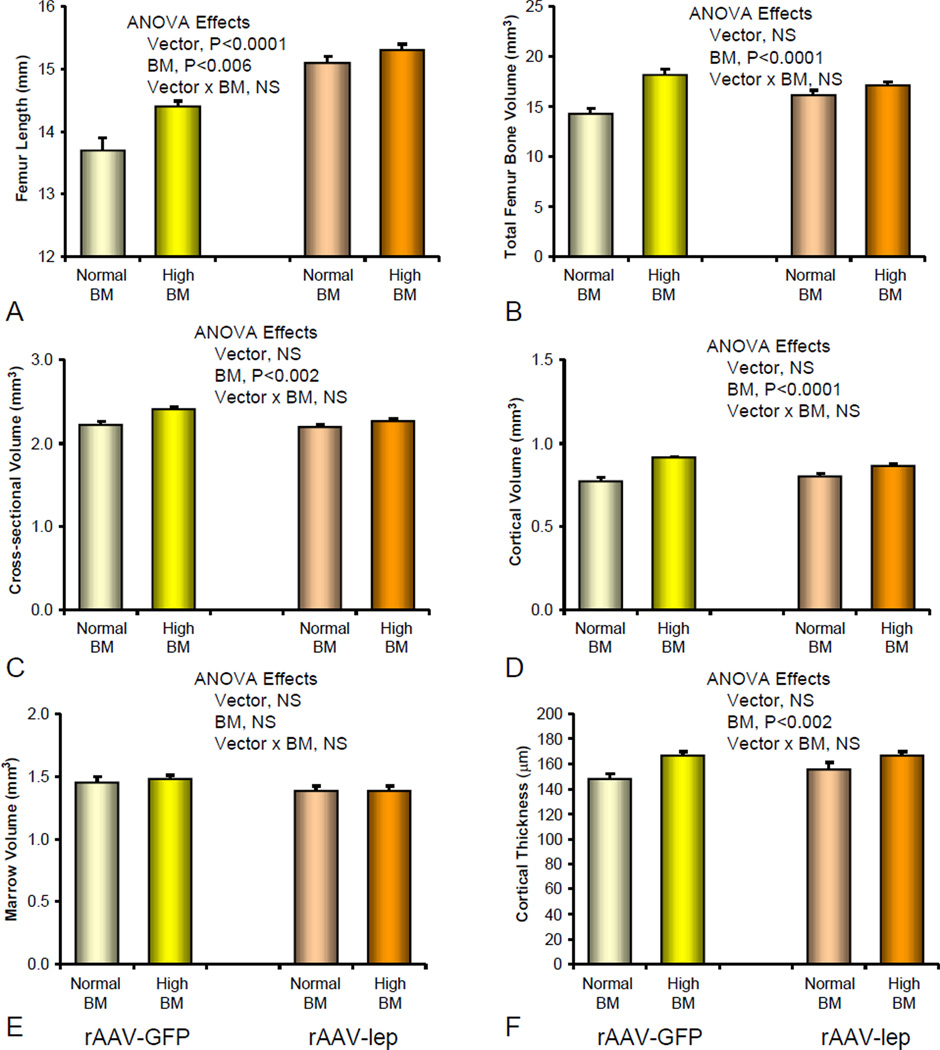
The effect of central leptin gene therapy and increased body mass due to high fat intake on bone volume and architecture in the femur is shown in Figures 3–4. Femora were longer in rAAV-lep-treated mice compared to rAAV-GFP-treated mice and longer in the heavier mice fed high fat diet than those fed control diet (Figure 3a). rAAV-lep treatment had no effect on total femur bone volume whereas increased body mass resulted in greater total femur bone volume (Figure 3b). There was no interaction between vector treatment and body mass for either femur length or total femur bone volume, indicating that increased body mass results in increased femoral bone mass, irrespective of central leptin.
Figure 3.
Effect of central leptin gene therapy and increased body mass (BM) on femur length (a) total femur bone volume (b), midshaft femur cross-sectional volume (c), midshaft femur cortical volume (d), midshaft femur marrow volume (e), and midshaft femur cortical thickness (f) in ob/ob mice administered either rAAV-GFP (control vector) or rAAV-lep icv (Experiment 2). All data are mean ± SE. NS, not significant, P>0.05.
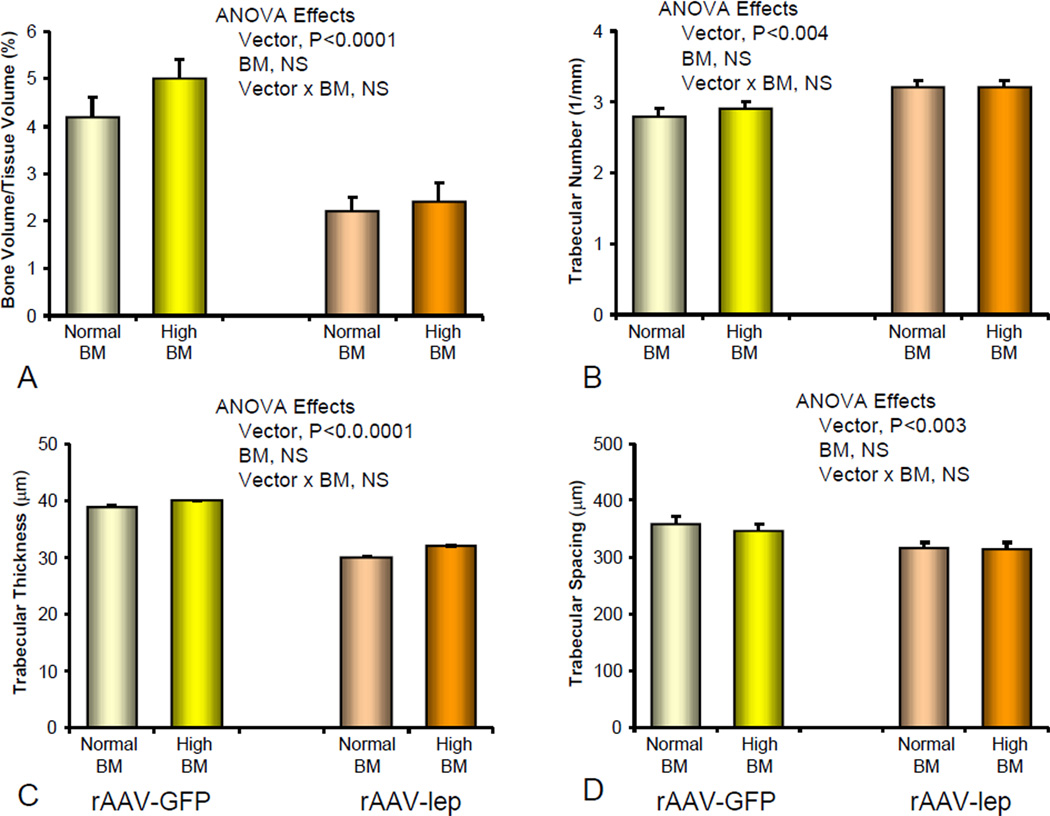
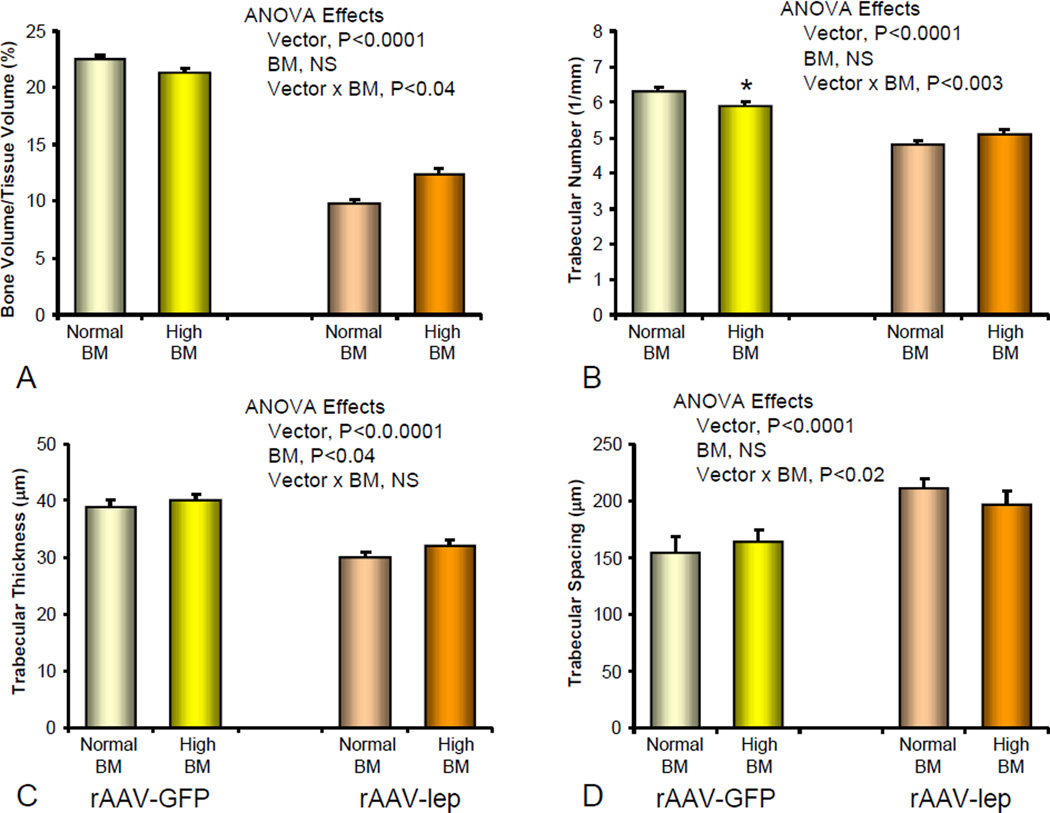
Figure 4.
Effect of central leptin gene therapy and increased body mass (BM) on distal femur bone volume/tissue volume (a), trabecular number (b), trabecular thickness (c), and trabecular spacing (d) in ob/ob mice administered either rAAV-GFP (control vector) or rAAV-lep icv (Experiment 2). All data are mean ± SE. NS, not significant, P>0.05.
rAAV-lep had no significant effect on midshaft cortical bone architecture (Figure 3c–f). In contrast, increased body mass resulted in greater midshaft cross-sectional volume, cortical volume, and cortical thickness. There were no significant vector × body mass interactions for any of the cortical endpoints examined.
In the distal femur, rAAV-lep treatment resulted in lower cancellous bone volume/tissue volume (Figure 4). This was due to lower trabecular thickness in the rAAV-lep in comparison to the rAAV-GFP-treated animals. Increased body mass had no independent effect on cancellous bone volume or architecture, and no significant interactions between vector treatment and body mass were noted.
In the lumbar vertebrae, rAAV-lep resulted in lower cancellous bone volume/tissue volume, lower trabecular number and thickness, and higher trabecular spacing (Figure 5). The heavier animals fed high fat diet had higher trabecular thickness compared to controls. Although significant vector × body mass interactions were noted for cancellous bone volume/tissue volume, trabecular number, and trabecular spacing, only trabecular number was lower in leptin-deficient rAAV-GFP mice consuming high fat diet compared to rAAV-GFP mice consuming control diet.
Figure 5.
Effect of central leptin gene therapy and increased body mass (BM) on vertebral (LV3) bone volume/tissue volume (a), trabecular number (b), trabecular thickness (c), and trabecular spacing (d) in ob/ob mice administered either rAAV-GFP (control vector) or rAAV-lep icv (Experiment 2). All data are mean ± SE. *P<0.05. NS, not significant, P>0.05.
Experiment 3
The first objective of Experiment 3 was to assess the effects of high fat diet-induced gain in body mass on bone in WT mice. In the WT mice, body mass and vertebral cancellous bone volume/tissue volume were higher in mice consuming high fat diet than in mice consuming control diet (Table 2). Significant body mass effects were not detected for trabecular number, thickness or spacing.
Table 2.
Effects of increased body mass (due to high fat intake) on vertebral (LV3) cancellous bone volume and architecture in wildtype mice and in ob/ob mice administered hypothalamic rAAV-GFP (control vector) or rAAV-lep (Experiment 3).
| Wild Type Mice |
ob/ob Mice |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| rAAV-GFP | rAAV-lep | ANOVA (P<) | ||||||||
| Body Mass | ANOVA (P<) |
Body Mass | Body Mass | Vector Treatment |
BM | Vector × BM |
||||
| Endpoint | Normal | High | Normal | High | Normal | High | ||||
| Body mass (g) | 24.5 ± 0.2 | 28.0 ± 1.0 | 0.005 | 55.2 ± 3.1 | 65.1 ± 1.9 | 21.6 ± 0.9 | 23.1 ± 0.8 | 0.0001 | 0.04 | NS |
| Bone volume/Tissue volume (%) | 11.4 ± 0.9 | 15.2 ± 1.0 | 0.016 | 24.0 ± 0.9 | 21.3 ± 1.7 | 9.0 ± 0.5 | 11.0 ± 0.4 | <0.0001 | NS | 0.042 |
| Trabecular number (1/mm) | 4.6 ± 0.2 | 5.0 ± 1.1 | NS | 6.1 ± 0.1 | 5.7 ± 0.1* | 4.7 ± 0.1 | 5.0 ± 0.1* | <0.0001 | NS | 0.008 |
| Trabecular thickness (µm) | 37 ± 2 | 39 ± 1 | NS | 43 ± 1 | 44 ± 1 | 33 ± 1 | 34 ± 1 | <0.0001 | NS | NS |
| Trabecular spacing (µrn) | 217 ± 8 | 198 ± 5 | NS | 159 ± 3 | 169 ± 5 | 213 ± 5 | 197 ± 3* | <0.0001 | NS | 0.008 |
Data are mean ± SE
BM, Body mass
NS, Not significant
Significantly different from Normal within same vector treatment, P<0.05
A second objective of Experiment 3 was to further evaluate global leptin deficiency, and selective central repletion of leptin on the skeletal response to body mass gain induced by a high fat intake. In contrast to Experiment 2, central leptin repletion and the high fat diet were initiated at an earlier age. However, the results of the two studies were nearly identical. As in Experiment 2, central rAAV-lep vector administration in ob/ob mice resulted in lower body mass and lower vertebral cancellous bone volume/tissue volume, lower trabecular number and trabecular thickness, and greater trabecular spacing (Table 2). Body mass had no independent effect on any of the vertebral cancellous bone endpoints evaluated. Significant vector × body mass interactions were noted for bone volume/tissue volume, trabecular number, and trabecular spacing. In the rAAV-GFP ob/ob mice, trabecular number was lower in animals consuming high fat diet in comparison to those consuming control diet. In the rAAV-lep ob/ob mice, trabecular number was higher and trabecular spacing was lower in the heavier animals consuming high fat compared to those consuming control diet.
4. Discussion
The positive relationship between body mass and bone mass in adult humans is well established [2, 3]. The results of our first study demonstrate that there is also a positive relationship between body mass and bone mass in growing and mature WT mice consuming regular mouse chow ad libitum. Leptin is a potential mediator of the effects of body mass on bone. In general, there is a strong positive correlation between adipose tissue mass and serum leptin. Thus, increased serum leptin levels are usually associated with weight gain. However, the relationship between fat and leptin is abolished in leptin-deficient ob/ob mice. We, therefore, evaluated the role of leptin in mediating the skeletal response to increased body mass by comparing the response of WT and leptin-deficient ob/ob mice to a high fat diet. Our results demonstrate that leptin status and body mass have independent as well as interactive effects on bone mass and architecture.
ob/ob mice are obese and compared to WT mice have a mosaic skeletal phenotype; the skeletal abnormalities include a decrease in overall bone mass, but site-specific increases in cancellous bone volume [29]. Administration of leptin to growing ob/ob mice restores bone architecture to near normal [30]. In concordance with our results, Ducy et al. [10] have shown that increasing hypothalamic leptin via short-term (4 weeks) icv infusion results in decreased cancellous bone volume in vertebrae of ob/ob mice. As shown in earlier studies [11, 12, 19, 28, 29], leptin deficiency results in decreased femur length and mass. Furthermore, administration of systemic leptin increases formation of cortical bone and corrects the growth plate abnormalities in ob/ob mice [11, 12, 19, 28, 29]. Increasing body mass through increased high fat intake resulted in an increase in cortical bone mass in femora of WT mice. This was independent of leptin signaling because it also occurred in leptin-deficient ob/ob mice. We interpret these results as evidence that increased body mass and leptin signaling have independent positive effects on cortical bone growth. In contrast, body mass had no independent effect on cancellous bone in distal femur or lumbar vertebra. However, the significant interaction between leptin status and body mass on several bone parameters suggests leptin may play a permissive role in increased body mass-induced bone changes in vertebra.
Circulating leptin was not detected in the rAAV-lep-treated ob/ob mice [37, 43], indicating that systemic leptin is unnecessary for the observed skeletal effects of leptin gene therapy in mice fed either control or high fat diet. Similarly, central but not systemic leptin is required for the observed effect of leptin gene therapy to reduce body mass.
Leptin deficient ob/ob obese mice develop multiple abnormalities in homeostatic regulatory pathways as evidenced by elevated corticosterone and decreased thyroid hormone levels [46]. Loss of leptin restraint on insulin secretion and glucose metabolism in ob/ob mice increases the risk for developing type 2 diabetes and gonadal insufficiency results in sterility [37, 43, 47, 48]. However, it is unlikely that the ob/ob phenotype is entirely due to leptin deficiency. Studies in Balb/cJ mice suggest that modifier genes alter the sterile-obese phenotype of ob/ob mice by reducing their obesity and stimulating their reproductive system despite the absence of leptin [49]. Nevertheless, the importance of leptin is illustrated by the observation that rAAV-lep treatment reverses the abnormalities in ob/ob mice [47, 48].
Increased adiposity in ob/ob mice is associated with increased blood levels of proinflammatory cytokines such as IL-6 and C-reactive protein [24]. Also, ob/ob mice have elevated serum IGF-I levels and can develop secondary hyperparathyroidism, hypercalcemia and abnormalities in vitamin D metabolism [25, 27]. A high fat diet may also impact bone regulatory factors such as insulin, IGF-I and proinflammatory cytokines [50–52]. Regarding bone, sex steroids, proinflammatory cytokines, corticosterone, thyroxine, insulin, vitamin D, parathyroid hormone and IGF-I influence bone growth and turnover. Changes in these hormones and cytokines may play a role in the skeletal adaptation to a high fat diet, leptin deficiency, or hypothalamic rAAV-lep treatment. Thus, our data does not distinguish between the direct effects of leptin or body mass on bone from indirect effects mediated by these intermediates.
Obesity resulting from a high fat diet may be the result of decreased leptin signaling. Resistance to leptin has been postulated to occur due to reduced leptin entry across the blood brain barrier despite chronic systemic hyperleptinemia [42, 43, 53–55] or down regulation of leptin receptor signaling [56]. Alternatively, inadequate leptin signaling may be due to suboptimal hypothalamic leptin levels [57] or an opposing regulatory mechanism [58]. Central leptin therapy bypasses the blood brain barrier by providing a local source of leptin in the hypothalamus. This approach results in long duration body mass reduction in wild type and genetically obese ob/ob mice [26, 37, 43, 47, 48], indicating that this method does not down regulate the leptin receptor. Our replication of the effect of daily systemic and central injections [59, 60] indicates that leptin produced by increased leptin transgene expression [26, 37, 43, 47, 48] was biologically active for the duration of the 15-week experiments described here, a finding that is in agreement with even longer studies performed in rodents [26, 31, 42, 61].
It has been reported that the central effects of leptin on bone metabolism are mediated by increased sympathetic signaling [10, 14]. Neither sympathectomy nor capsaicin treatment of neonatal rats had an effect on bone growth. However, the skeletal response to a mechanical perturbation was altered [20]. Interestingly, sensory denervation increased, whereas sympathectomy decreased the normal response. Thus, leptin acting through the central nervous system may influence the bone anabolic response to increased body mass. Loading has a direct stimulatory effect on osteoblasts in culture [62] and on sympathectomized limbs [63]. It is possible, however, that the adaptive effects of leptin and body mass are more readily apparent at low levels of loading. This could explain the lack of a requirement for leptin signaling in the femur. This possibility is supported by the observation that the response of bone to systemic factors can vary between skeletal sites depending upon the magnitude of loading [64].
Severe dietary restriction, rather than a genetic defect, is the most common cause of leptin insufficiency in humans [65]. It is, therefore, possible that leptin insufficiency, as well as a low body mass, contributes to the low bone mass in adolescents with eating disorders. The composition of the normal and high fat diets in our studies was not identical. Therefore, we cannot rule out the possibility that bone active components of the diet contribute to the skeletal changes associated with a high fat diet. However, there was a significant correlation between body mass and bone mass in mice fed normal diet (Experiment 1). This result suggests that the increase in bone mass associated with feeding mice a high fat diet is associated with the increase in body mass and not the diet per se.
In summary, increased body mass has a positive effect on bone mass in WT mice. This was found to be the case in animals consuming normal and high fat diets. Studies in the ob/ob mice demonstrate that leptin is not required for increased cortical bone volume associated with increased body mass but may play a role in the positive effects of body mass gain on cancellous bone volume. These differential effects of leptin and body mass on various skeletal sites may help explain the complex skeletal phenotype in ob/ob mice.
Acknowledgements
This work was supported by grants from the National Institute of Health (DK 37273 and 27372 to S.P. Kalra and AA 011140 to R.T. Turner) and the Center for Healthy Aging Research, Oregon State University (to U.T. Iwaniec).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Literature Cited
- 1.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 2.Asomaning K, Bertone-Johnson ER, Nasca PC, Hooven F, Pekow PS. The association between body mass index and osteoporosis in patients referred for a bone mineral density examination. J Womens Health (Larchmt) 2006;15:1028–1034. doi: 10.1089/jwh.2006.15.1028. [DOI] [PubMed] [Google Scholar]
- 3.Viapiana O, Gatti D, Dalle Grave R, Todesco T, Rossini M, Braga V, Idolazzi L, Fracassi E, Adami S. Marked increases in bone mineral density and biochemical markers of bone turnover in patients with anorexia nervosa gaining weight. Bone. 2007;40:1073–1077. doi: 10.1016/j.bone.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Felson DT, Zhang Y, Hannan MT, Anderson JJ. Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res. 1993;8:567–573. doi: 10.1002/jbmr.5650080507. [DOI] [PubMed] [Google Scholar]
- 5.Wang MC, Bachrach LK, Van Loan M, Hudes M, Flegal KM, Crawford PB. The relative contributions of lean tissue mass and fat mass to bone density in young women. Bone. 2005;37:474–481. doi: 10.1016/j.bone.2005.04.038. [DOI] [PubMed] [Google Scholar]
- 6.Sawakami K, Robling AG, Ai M, Pitner ND, Liu D, Warden SJ, Li J, Maye P, Rowe DW, Duncan RL, Warman ML, Turner CH. The Wnt co-receptor LRP5 is essential for skeletal mechanotransduction but not for the anabolic bone response to parathyroid hormone treatment. J Biol Chem. 2006;281:23698–23711. doi: 10.1074/jbc.M601000200. [DOI] [PubMed] [Google Scholar]
- 7.Turner RT, Evans GL, Lotinun S, Lapke PD, Iwaniec UT, Morey-Holton E. Dose-response effects of intermittent PTH on cancellous bone in hindlimb unloaded rats. J Bone Miner Res. 2007;22:64–71. doi: 10.1359/jbmr.061006. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]
- 9.Burguera B, Hofbauer LC, Thomas T, Gori F, Evans GL, Khosla S, Riggs BL, Turner RT. Leptin reduces ovariectomy-induced bone loss in rats. Endocrinology. 2001;142:3546–3553. doi: 10.1210/endo.142.8.8346. [DOI] [PubMed] [Google Scholar]
- 10.Ducy P, Amling M, Takeda S, Priemel M, Schilling AF, Beil FT, Shen J, Vinson C, Rueger JM, Karsenty G. Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell. 2000;100:197–207. doi: 10.1016/s0092-8674(00)81558-5. [DOI] [PubMed] [Google Scholar]
- 11.Hamrick MW, Della-Fera MA, Choi YH, Pennington C, Hartzell D, Baile CA. Leptin treatment induces loss of bone marrow adipocytes and increases bone formation in leptin-deficient ob/ob mice. J Bone Miner Res. 2005;20:994–1001. doi: 10.1359/JBMR.050103. [DOI] [PubMed] [Google Scholar]
- 12.Steppan CM, Crawford DT, Chidsey-Frink KL, Ke H, Swick AG. Leptin is a potent stimulator of bone growth in ob/ob mice. Regul Peptl. 2000;92:73–78. doi: 10.1016/s0167-0115(00)00152-x. [DOI] [PubMed] [Google Scholar]
- 13.Baldock PA, Allison S, McDonald MM, Sainsbury A, Enriquez RF, Little DG, Eisman JA, Gardiner EM, Herzog H. Hypothalamic regulation of cortical bone mass: opposing activity of Y2 receptor and leptin pathways. J Bone Miner Res. 2006;21:1600–1607. doi: 10.1359/jbmr.060705. [DOI] [PubMed] [Google Scholar]
- 14.Takeda S, Elefteriou F, Levasseur R, Liu X, Zhao L, Parker KL, Armstrong D, Ducy P, Karsenty G. Leptin regulates bone formation via the sympathetic nervous system. Cell. 2002;111:305–317. doi: 10.1016/s0092-8674(02)01049-8. [DOI] [PubMed] [Google Scholar]
- 15.Cornish J, Callon KE, Bava U, Lin C, Naot D, Hill BL, Grey AB, Broom N, Myers DE, Nicholson GC, Reid IR. Leptin directly regulates bone cell function in vitro and reduces bone fragility in vivo. J Endocrinol. 2002;175:405–415. doi: 10.1677/joe.0.1750405. [DOI] [PubMed] [Google Scholar]
- 16.Maor G, Rochwerger M, Segev Y, Phillip M. Leptin acts as a growth factor on the chondrocytes of skeletal growth centers. J Bone Miner Res. 2002;17:1034–1043. doi: 10.1359/jbmr.2002.17.6.1034. [DOI] [PubMed] [Google Scholar]
- 17.Thomas T. The complex effects of leptin on bone metabolism through multiple pathways. Curr Opin Pharmacol. 2004;4:295–300. doi: 10.1016/j.coph.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 18.Thomas T, Gori F, Khosla S, Jensen MD, Burguera B, Riggs BL. Leptin acts on human marrow stromal cells to enhance differentiation to osteoblasts and to inhibit differentiation to adipocytes. Endocrinology. 1999;140:1630–1638. doi: 10.1210/endo.140.4.6637. [DOI] [PubMed] [Google Scholar]
- 19.Kishida Y, Hirao M, Tamai N, Nampei A, Fujimoto T, Nakase T, Shimizu N, Yoshikawa H, Myoui A. Leptin regulates chondrocyte differentiation and matrix maturation during endochondral ossification. Bone. 2005;37:607–621. doi: 10.1016/j.bone.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Hill EL, Turner R, Elde R. Effects of neonatal sympathectomy and capsaicin treatment on bone remodeling in rats. Neuroscience. 1991;44:747–755. doi: 10.1016/0306-4522(91)90094-5. [DOI] [PubMed] [Google Scholar]
- 21.Hohmann EL, Elde RP, Rysavy JA, Einzig S, Gebhard RL. Innervation of periosteum and bone by sympathetic vasoactive intestinal peptide-containing nerve fibers. Science. 1986;232:868–871. doi: 10.1126/science.3518059. [DOI] [PubMed] [Google Scholar]
- 22.Bluher S, Mantzoros CS. The role of leptin in regulating neuroendocrine function in humans. J Nutr. 2004;134:2469S–2474S. doi: 10.1093/jn/134.9.2469S. [DOI] [PubMed] [Google Scholar]
- 23.Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89:2583–2589. doi: 10.1210/jc.2004-0535. [DOI] [PubMed] [Google Scholar]
- 24.Dube MG, Torto R, Kalra SP. Increased leptin expression selectively in the hypothalamus suppresses inflammatory markers CRP and IL-6 in leptin-deficient diabetic obese mice. Peptides. 2008;29:593–598. doi: 10.1016/j.peptides.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giovambattista A, Chisari AN, Gaillard RC, Spinedi E. Food intake-induced leptin secretion modulates hypothalamo-pituitary-adrenal axis response and hypothalamic Ob-Rb expression to insulin administration. Neuroendocrinology. 2000;72:341–349. doi: 10.1159/000054603. [DOI] [PubMed] [Google Scholar]
- 26.Kalra SP, Kalra PS. Gene-transfer technology: a preventive neurotherapy to curb obesity, ameliorate metabolic syndrome and extend life expectancy. Trends Pharmacol Sci. 2005;26:488–495. doi: 10.1016/j.tips.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 27.Matsunuma A, Kawane T, Maeda T, Hamada S, Horiuchi N. Leptin corrects increased gene expression of renal 25-hydroxyvitamin D3-1 alpha-hydroxylase and -24-hydroxylase in leptin-deficient, ob/ob mice. Endocrinology. 2004;145:1367–1375. doi: 10.1210/en.2003-1010. [DOI] [PubMed] [Google Scholar]
- 28.Ealey KN, Fonseca D, Archer MC, Ward WE. Bone abnormalities in adolescent leptin-deficient mice. Regul Pept. 2006;136:9–13. doi: 10.1016/j.regpep.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 29.Hamrick MW, Pennington C, Newton D, Xie D, Isales C. Leptin deficiency produces contrasting phenotypes in bones of the limb and spine. Bone. 2004;34:376–383. doi: 10.1016/j.bone.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 30.Iwaniec UT, Boghossian S, Lapke PD, Turner RT, Kalra SP. Central leptin gene therapy corrects skeletal abnormalities in leptin-deficient ob/ob mice. Peptides. 2007;28:1012–1019. doi: 10.1016/j.peptides.2007.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beretta E, Dube MG, Kalra PS, Kalra SP. Long-term suppression of weight gain, adiposity, and serum insulin by central leptin gene therapy in prepubertal rats: effects on serum ghrelin and appetite-regulating genes. Pediatr Res. 2002;52:189–198. doi: 10.1203/00006450-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Dhillon H, Ge Y, Minter RM, Prima V, Moldawer LL, Muzyczka N, Zolotukhin S, Kalra PS, Kalra SP. Long-term differential modulation of genes encoding orexigenic and anorexigenic peptides by leptin delivered by rAAV vector in ob/ob mice. Relationship with body weight change. Regul Pept. 2000;92:97–105. doi: 10.1016/s0167-0115(00)00155-5. [DOI] [PubMed] [Google Scholar]
- 33.Dhillon H, Kalra SP, Kalra PS. Dose-dependent effects of central leptin gene therapy on genes that regulate body weight and appetite in the hypothalamus. Mol Ther. 2001;4:139–145. doi: 10.1006/mthe.2001.0427. [DOI] [PubMed] [Google Scholar]
- 34.Dhillon H, Kalra SP, Prima V, Zolotukhin S, Scarpace PJ, Moldawer LL, Muzyczka N, Kalra PS. Central leptin gene therapy suppresses body weight gain, adiposity and serum insulin without affecting food consumption in normal rats: a long-term study. Regul Pept. 2001;99:69–77. doi: 10.1016/s0167-0115(01)00237-3. [DOI] [PubMed] [Google Scholar]
- 35.Dube MG, Beretta E, Dhillon H, Ueno N, Kalra PS, Kalra SP. Central leptin gene therapy blocks high-fat diet-induced weight gain, hyperleptinemia, and hyperinsulinemia: increase in serum ghrelin levels. Diabetes. 2002;51:1729–1736. doi: 10.2337/diabetes.51.6.1729. [DOI] [PubMed] [Google Scholar]
- 36.Zolotukhin S, Byrne BJ, Mason E, Zolotukhin I, Potter M, Chesnut K, Summerford C, Samulski RJ, Muzyczka N. Recombinant adeno-associated virus purification using novel methods improves infectious titer and yield. Gene Ther. 1999;6:973–985. doi: 10.1038/sj.gt.3300938. [DOI] [PubMed] [Google Scholar]
- 37.Boghossian S, Dube MG, Torto R, Kalra PS, Kalra SP. Hypothalamic clamp on insulin release by leptin-transgene expression. Peptides. 2006;27:3245–3254. doi: 10.1016/j.peptides.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 38.Bagnasco M, Dube MG, Kalra PS, Kalra SP. Evidence for the existence of distinct central appetite, energy expenditure, and ghrelin stimulation pathways as revealed by hypothalamic site-specific leptin gene therapy. Endocrinology. 2002;143:4409–4421. doi: 10.1210/en.2002-220505. [DOI] [PubMed] [Google Scholar]
- 39.Bagnasco M, Dube MG, Katz A, Kalra PS, Kalra SP. Leptin expression in hypothalamic PVN reverses dietary obesity and hyperinsulinemia but stimulates ghrelin. Obes Res. 2003;11:1463–1470. doi: 10.1038/oby.2003.196. [DOI] [PubMed] [Google Scholar]
- 40.Beretta E, Dhillon H, Kalra PS, Kalra SP. Central LIF gene therapy suppresses food intake, body weight, serum leptin and insulin for extended periods. Peptides. 2002;23:975–984. doi: 10.1016/s0196-9781(02)00021-9. [DOI] [PubMed] [Google Scholar]
- 41.Boghossian S, Lecklin A, Dube MG, Kalra PS, Kalra SP. Increased leptin expression in the dorsal vagal complex suppresses adiposity without affecting energy intake and metabolic hormones. Obesity (Silver Spring) 2006;14:1003–1009. doi: 10.1038/oby.2006.115. [DOI] [PubMed] [Google Scholar]
- 42.Boghossian S, Lecklin A, Torto R, Kalra PS, Kalra SP. Suppression of fat deposition for the life time with gene therapy. Peptides. 2005;26:1512–1519. doi: 10.1016/j.peptides.2005.03.039. [DOI] [PubMed] [Google Scholar]
- 43.Boghossian S, Ueno N, Dube MG, Kalra P, Kalra S. Leptin gene transfer in the hypothalamus enhances longevity in adult monogenic mutant mice in the absence of circulating leptin. Neurobiol Aging. 2007;28:1594–1604. doi: 10.1016/j.neurobiolaging.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 44.Thomsen JS, Laib A, Koller B, Prohaska S, Mosekilde L, Gowin W. Stereological measures of trabecular bone structure: comparison of 3D micro computed tomography with 2D histological sections in human proximal tibial bone biopsies. J Microsc. 2005;218:171–179. doi: 10.1111/j.1365-2818.2005.01469.x. [DOI] [PubMed] [Google Scholar]
- 45.Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York: John Wiley & Sons, Inc.; 1987. [Google Scholar]
- 46.Wang X, Rundle CH, Wergedal JE, Srivastava AK, Mohan S, Lau KH. Loss of sex-specific difference in femoral bone parameters in male leptin knockout mice. Calcif Tissue Int. 2007;80:374–382. doi: 10.1007/s00223-007-9026-0. [DOI] [PubMed] [Google Scholar]
- 47.Ueno N, Dube MG, Inui A, Kalra PS, Kalra SP. Leptin modulates orexigenic effects of ghrelin and attenuates adiponectin and insulin levels and selectively the dark-phase feeding as revealed by central leptin gene therapy. Endocrinology. 2004;145:4176–4184. doi: 10.1210/en.2004-0262. [DOI] [PubMed] [Google Scholar]
- 48.Ueno N, Inui A, Kalra PS, Kalra SP. Leptin transgene expression in the hypothalamus enforces euglycemia in diabetic, insulin-deficient nonobese Akita mice and leptin-deficient obese ob/ob mice. Peptides. 2006;27:2332–2342. doi: 10.1016/j.peptides.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 49.Chehab FF, Qiu J, Mounzih K, Ewart-Toland A, Ogus S. Leptin and reproduction. Nutr Rev. 2002;60:S39–S46. doi: 10.1301/002966402320634823. discussion S68–84, 85–7. [DOI] [PubMed] [Google Scholar]
- 50.Li R, Svenson KL, Donahue LR, Peters LL, Churchill GA. Relationships of dietary fat, body composition, and bone mineral density in inbred mouse strain panels. Physiol Genomics. 2008;33:26–32. doi: 10.1152/physiolgenomics.00174.2007. [DOI] [PubMed] [Google Scholar]
- 51.Lundman P, Boquist S, Samnegard A, Bennermo M, Held C, Ericsson CG, Silveira A, Hamsten A, Tornvall P. A high-fat meal is accompanied by increased plasma interleukin-6 concentrations. Nutr Metab Cardiovasc Dis. 2007;17:195–202. doi: 10.1016/j.numecd.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 52.Sun X, Zemel MB. Calcium and 1,25-dihydroxyvitamin D3 regulation of adipokine expression. Obesity (Silver Spring) 2007;15:340–348. doi: 10.1038/oby.2007.540. [DOI] [PubMed] [Google Scholar]
- 53.Banks WA, Kastin AJ, Huang W, Jaspan JB, Maness LM. Leptin enters the brain by a saturable system independent of insulin. Peptides. 1996;17:305–311. doi: 10.1016/0196-9781(96)00025-3. [DOI] [PubMed] [Google Scholar]
- 54.Frederich RC, Hamann A, Anderson S, Lollmann B, Lowell BB, Flier JS. Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med. 1995;1:1311–1314. doi: 10.1038/nm1295-1311. [DOI] [PubMed] [Google Scholar]
- 55.Van Heek M, Compton DS, France CF, Tedesco RP, Fawzi AB, Graziano MP, Sybertz EJ, Strader CD, Davis HR., Jr. Diet-induced obese mice develop peripheral, but not central, resistance to leptin. J Clin Invest. 1997;99:385–390. doi: 10.1172/JCI119171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Munzberg H, Myers MG., Jr. Molecular and anatomical determinants of central leptin resistance. Nat Neurosci. 2005;8:566–570. doi: 10.1038/nn1454. [DOI] [PubMed] [Google Scholar]
- 57.Kalra SP. Central leptin insufficiency syndrome: an interactive etiology for obesity, metabolic and neural diseases and for designing new therapeutic interventions. Peptides. 2008;29:127–138. doi: 10.1016/j.peptides.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Eiden S, Simon E, Schmidt I. Dose-related steady states of fat loss in long-term leptin-treated ob/ob mice: leptin resistance or desensitization versus counterregulatory signaling. J Comp Physiol. 2005;175:487–497. doi: 10.1007/s00360-005-0009-z. [DOI] [PubMed] [Google Scholar]
- 59.Chen Y, Heiman ML. Chronic leptin administration promotes lipid utilization until fat mass is greatly reduced and preserves lean mass of normal female rats. Regul Pept. 2000;92:113–119. doi: 10.1016/s0167-0115(00)00157-9. [DOI] [PubMed] [Google Scholar]
- 60.Pelleymounter MA, Cullen MJ, Baker MB, Hecht R, Winters D, Boone T, Collins F. Effects of the obese gene product on body weight regulation in ob/ob mice. Science. 1995;269:540–543. doi: 10.1126/science.7624776. [DOI] [PubMed] [Google Scholar]
- 61.Kalra SP, Kalra PS. Subjugation of hypothalamic NPY and cohorts with central leptin gene therapy alleviates dyslipidemia, insulin resistance, and obesity for life-time. Exs. 2006:157–169. doi: 10.1007/3-7643-7417-9_12. [DOI] [PubMed] [Google Scholar]
- 62.Rubin J, Rubin C, Jacobs CR. Molecular pathways mediating mechanical signaling in bone. Gene. 2006;367:1–16. doi: 10.1016/j.gene.2005.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.de Souza RL, Pitsillides AA, Lanyon LE, Skerry TM, Chenu C. Sympathetic nervous system does not mediate the load-induced cortical new bone formation. J Bone Miner Res. 2005;20:2159–2168. doi: 10.1359/JBMR.050812. [DOI] [PubMed] [Google Scholar]
- 64.Westerlind KC, Wronski TJ, Ritman EL, Luo ZP, An KN, Bell NH, Turner RT. Estrogen regulates the rate of bone turnover but bone balance in ovariectomized rats is modulated by prevailing mechanical strain. Proc Natl Acad Sci U S A. 1997;94:4199–4204. doi: 10.1073/pnas.94.8.4199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Farooqi IS. Monogenic human obesity. Front Horm Res. 2008;36:1–11. doi: 10.1159/000115333. [DOI] [PubMed] [Google Scholar]