Abstract
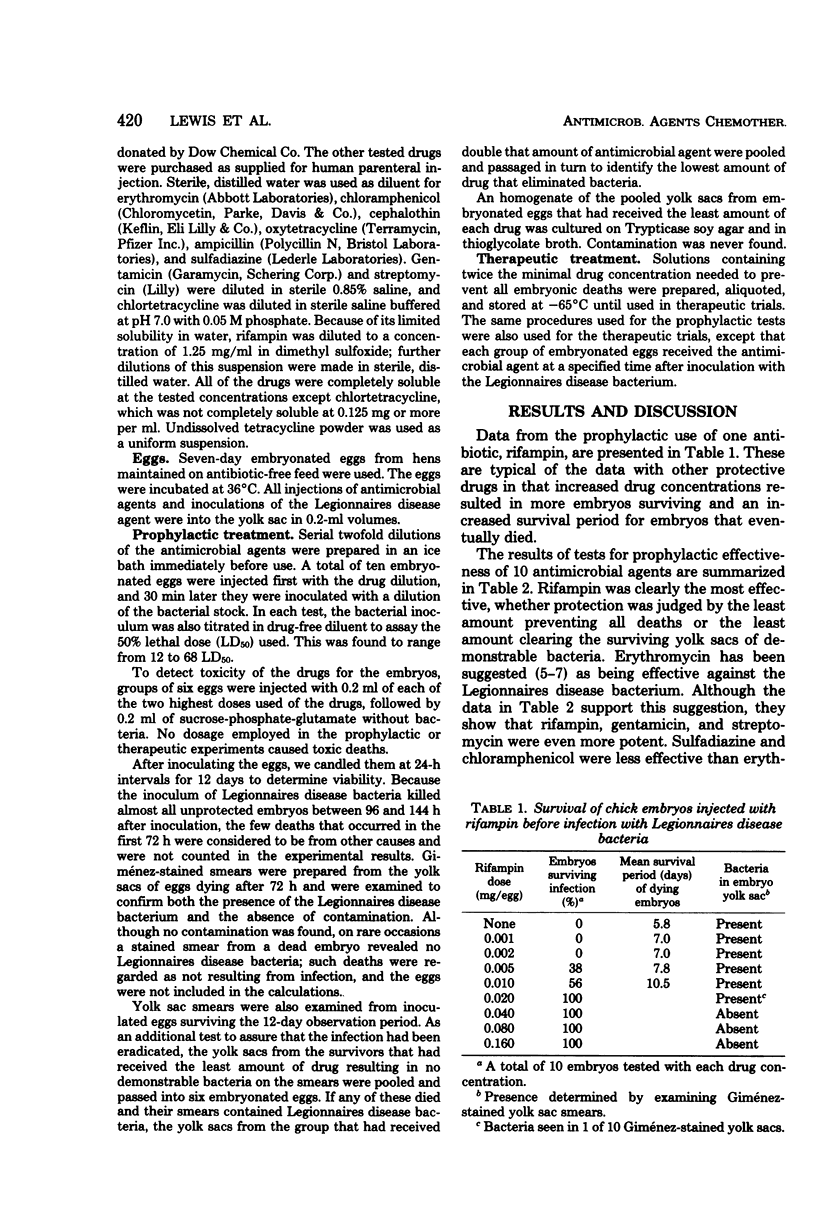
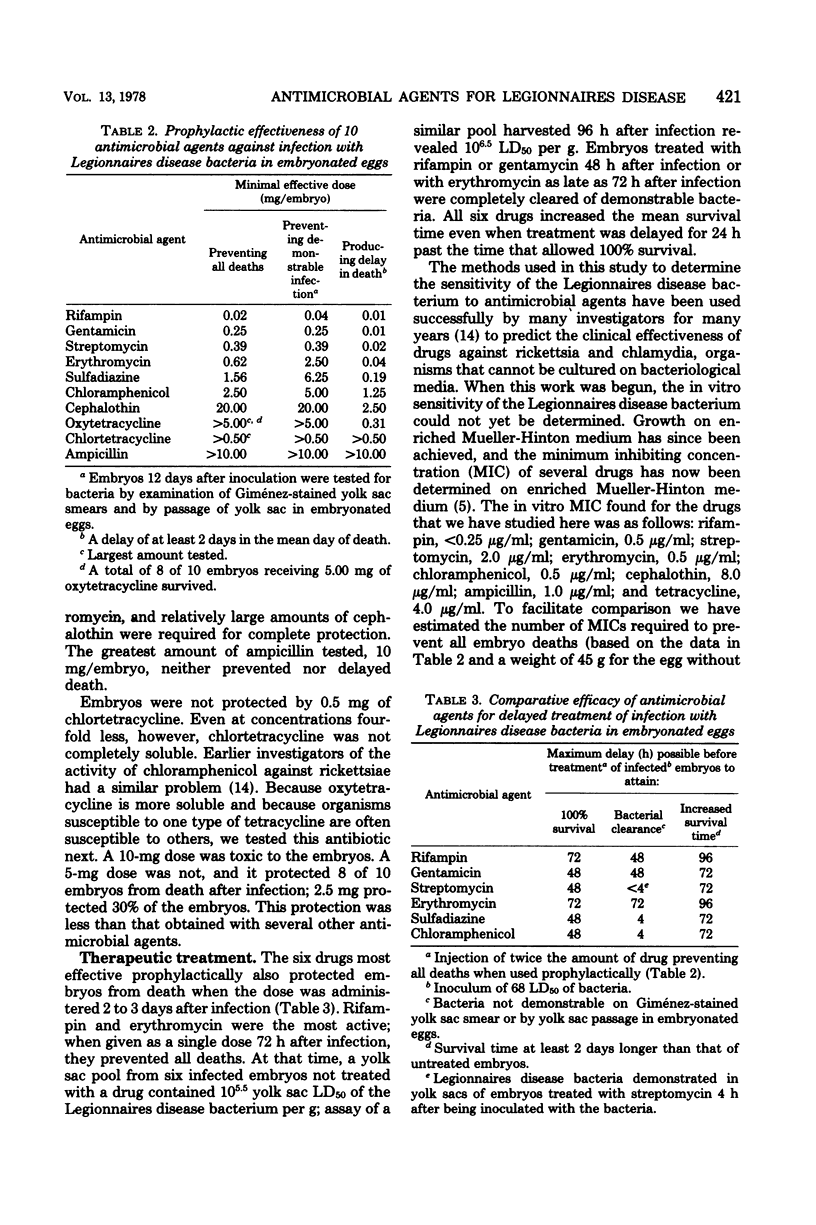
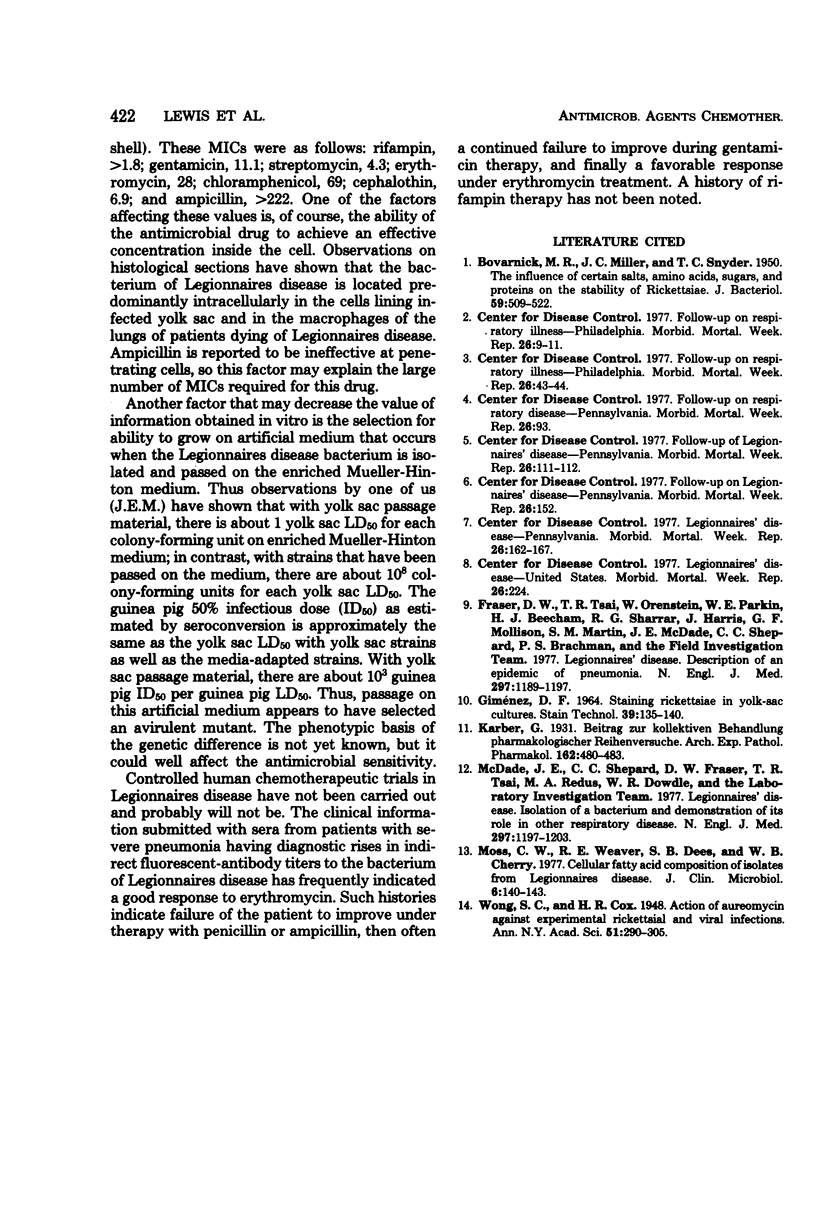
The susceptibility of the Legionnaires disease bacterium to various antimicrobial agents was determined by inoculation of embryonated eggs via the yolk sac. When administered prophylactically, the minimal dose of drug preventing all deaths due to the infection was as follows: rifampin, 0.02 mg; gentamicin, 0.25 mg; streptomycin, 0.39 mg; erythromycin, 0.62 mg; sulfadiazine, 1.56 mg; chloramphenicol, 2.50 mg; and cephalothin, 20.0 mg. Smaller amounts delayed deaths, and larger or equal amounts rendered the embryos free of infection. Oxytetracycline in the largest tested amount, 5.0 mg, protected 80% of the embryos from death, and as little as 0.31 mg delayed death. Chlortetracycline (0.50 mg) and ampicillin (10.0 mg) were ineffective. The six most effective drugs were studied in an experiment in which they were administered at various times after infection in doses that were twice the minimal prophylactic dose preventing all deaths. In this therapeutic experiment, rifampin, and erythromycin allowed 100% survival when given even 72 h after infection; gentamicin, streptomycin, sulfadiazine, and chloramphenicol did so when given 48 h after infection. All six drugs increased mean survival time when administered 72 h after infection.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BOVARNICK M. R., MILLER J. C., SNYDER J. C. The influence of certain salts, amino acids, sugars, and proteins on the stability of rickettsiae. J Bacteriol. 1950 Apr;59(4):509–522. doi: 10.1128/jb.59.4.509-522.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraser D. W., Tsai T. R., Orenstein W., Parkin W. E., Beecham H. J., Sharrar R. G., Harris J., Mallison G. F., Martin S. M., McDade J. E. Legionnaires' disease: description of an epidemic of pneumonia. N Engl J Med. 1977 Dec 1;297(22):1189–1197. doi: 10.1056/NEJM197712012972201. [DOI] [PubMed] [Google Scholar]
- GIMENEZ D. F. STAINING RICKETTSIAE IN YOLK-SAC CULTURES. Stain Technol. 1964 May;39:135–140. doi: 10.3109/10520296409061219. [DOI] [PubMed] [Google Scholar]
- McDade J. E., Shepard C. C., Fraser D. W., Tsai T. R., Redus M. A., Dowdle W. R. Legionnaires' disease: isolation of a bacterium and demonstration of its role in other respiratory disease. N Engl J Med. 1977 Dec 1;297(22):1197–1203. doi: 10.1056/NEJM197712012972202. [DOI] [PubMed] [Google Scholar]
- Moss C. W., Weaver R. E., Dees S. B., Cherry W. B. Cellular fatty acid composition of isolates from Legionnaires disease. J Clin Microbiol. 1977 Aug;6(2):140–143. doi: 10.1128/jcm.6.2.140-143.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]


