Abstract
Most patients who present to a cardiologist with syncope will have vasovagal (reflex) syncope. A busy syncope practice will often also see patients with postural tachycardia syndrome, often presenting with severe recurrent presyncope. Recognition of this “syncope confounder” might be difficult without adequate knowledge of their presentation, and this can adversely affect optimal management. Patients with postural tachycardia syndrome exhibit an excessive increase in heart rate ≥ 30 bpm within 10 minutes of standing (in the absence of orthostatic hypotension), in addition to chronic symptoms of orthostatic intolerance. Postural tachycardia syndrome can often be differentiated from vasovagal syncope by its hemodynamic pattern during tilt table test and differing clinical characteristics. This article will briefly review the presentation of postural tachycardia syndrome, its putative pathophysiology and an approach to non-pharmacological and pharmacological management.
Keywords: syncope, vasovagal, postural tachycardia syndrome, treatment, medications, non-pharmacological, postural tachycardia syndrome, vasovagal syncope, autonomic dysfunction, syncope, blood pressure, heart rate
Introduction
While most cases of syncope are due to vasovagal syncope (VVS), more common than syncope is presyncope. Cardiologists working in a syncope clinic or in a tilt table laboratory will realize that a common confounder of vasovagal syncope and presyncope is postural tachycardia syndrome (POTS; primarily presenting with presyncope). Table 1 highlights some contrasting clinical characteristics between these 2 disorders. These disorders can have distinct hemodynamic patterns during tilt table testing. During head up tilt:
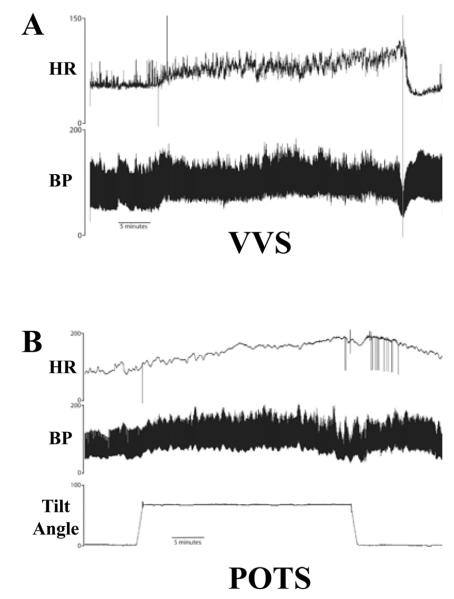
Patients with VVS will often hold a steady blood pressure (BP) for several minutes (often >10 minutes) post head-up tilt, before they develop symptoms and drop their BP rapidly (Fig. 1a).
Patients with POTS do not usually drop their BP with head-up tilt. Rather, they classically have an excessive increase in their heart rate (HR) (Fig 1b). This article will review of the presentation, putative pathophysiology, investigation approach and treatment of postural tachycardia syndrome.
Table 1.
Clinical Comparison of Vasovagal Syncope and Postural Tachycardia Syndrome
| Features | Vasovagal Syncope |
Postural Tachycardia Syndrome |
|---|---|---|
| Typical age | Any age; 1st episode usually in 2nd/3rd decade |
13-50 years |
| Gender (% Female) | 60% | 85% |
|
Symptoms with
Body Position Change |
After prolonged sitting or standing |
Immediately with sitting or standing |
| Syncope | +++ | +/− |
| Presyncope | + | ++++ |
|
Orthostatic
Hypotension |
+/− (usually only at time of faint) |
+/− |
|
Hemodynamic
Pattern with Head Up Tilt |
Sudden drop in BP & HR |
Early increase in HR≥30bpm |
BP - blood pressure; HR - heart rate.
Figure 1. Head-up tilt test traces from a patient with Vasovagal Syncope (VVS; Panel A) and postural tachycardia syndrome (POTS; Panel B).
Panel A: With VVS, the heart rate (HR) and blood pressure (BP) increases a little bit at the onset of tilt, and they are maintained for over 25 minutes before a sudden precipitous drop in BP before the table is returned to the supine position. Panel B: With POTS, the BP often increases a little bit with head-up tilt, and starts to return to baseline when the table returns to the supine position. Traces are reprinted with permission from reference 27.
Hemodynamic Physiology of Standing: Healthy and POTS
With the assumption of an upright posture, there is a downward shift of ~500 ml of blood to the dependent areas (mainly abdomen and legs). This gravitational shift in blood results in decreased venous return, decreased cardiac output and eventually decreased BP 1 (Fig 2a). This “unloads” the baroreceptors, and triggers a reflex sympathetic activation with a resultant increase in HR and systemic vasoconstriction (countering the initial decline in BP). In a healthy individual, the net effect of assumption of upright posture is an increase in HR of 10-20 bpm, a minimal change in systolic BP, and a ~5 mmHg increase in diastolic BP.
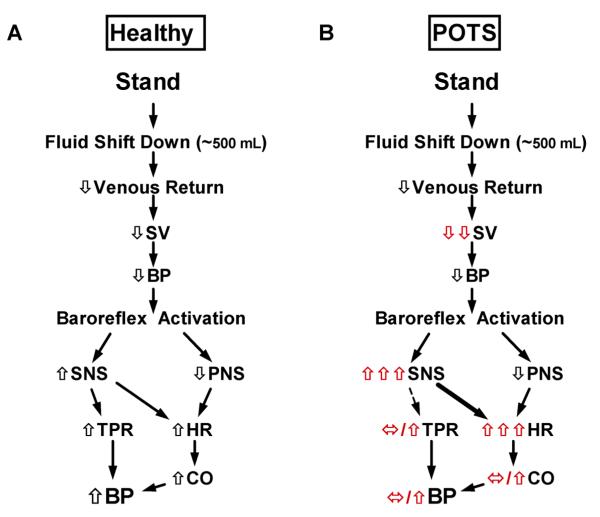
Figure 2. Physiology of Standing in a Healthy Individual and Patient with POTS.
Panel A: With the assumption of an upright posture in a healthy individual, there is a downward shift of ~500 ml of blood with a decrease in venous return, stroke volume (SV) and eventually blood pressure (BP) 1. This “unloads” the baroreceptors, and triggers reflex sympathetic nervous system (SNS) activation with a resultant increase in heart rate (HR) and systemic vasoconstriction (countering the initial decline in BP). In a healthy individual, the net effect of assumption of upright posture is an increase in HR of 10-20 bpm, a minimal change in systolic BP, and a ~5 mmHg increase in diastolic BP. Panel B: In patients with POTS, the initial response to upright posture can include a profound drop in SV. With engagement of the baroreflex, there can be a vigorous increase in SNS tone and an exaggerated increase in HR. The BP may remain unchanged or even increase if there is excessive SNS mediated vasoconstriction. Presyncope can result from the excessive HR increase and/or the increased SNS tone. CO – cardiac output; PNS – parasympathetic nervous system; TPR – total peripheral resistance.
In patients with POTS (Fig 2b), the initial response to upright posture can include a profound drop in stroke volume. With engagement of the baroreflex, there can be a vigorous increase in sympathetic tone and an exaggerated increase in HR. The blood pressure may remain unchanged or even increase if there is excessive sympathetically mediated vasoconstriction. Presyncope can result from the excessive tachycardia and/or the increased sympathoneural tone.
POSTURAL TACHYCARDIA SYNDROME
Patients with POTS demonstrate an excessive increase in HR in response to upright posture (in the absence of orthostatic hypotension) with improvement in symptoms on lying down 1, 2.
It is estimated that there are ~500,000 Americans diagnosed with POTS in the United States 3, with 80-90% female patients 1, 4, 5, often of childbearing age 1, 6.
POTS Diagnostic Criteria (Table 2)
Table 2.
Diagnostic Criteria for Postural Tachycardia Syndrome
|
POTS is defined as the presence of symptoms of orthostatic intolerance for >6 months accompanied by a HR increase of ≥30 bpm within 10 min of assuming an upright posture in the absence of orthostatic hypotension (fall in BP >20/10 mmHg). The syndrome must occur in the absence of prolonged bed rest, medications that impair autonomic regulation (e.g. diuretics, vasodilators, diuretics, sympatholytics or certain antidepressants), or any other chronic debilitating disorders that might cause tachycardia (such as dehydration, anemia or hyperthyroidism). Orthostatic tachycardia is necessary, but not sufficient to make the diagnosis of POTS; typical symptoms are also required.
POTS Clinical Features
Symptoms in POTS patients include lightheadedness, shortness of breath, palpitations, tremulousness, chest discomfort, headache, visual disturbances, mental clouding (“brain fog”), and nausea. Only a minority (~30%) of patients with POTS has frank syncope, but daily or almost daily pre-syncope occurs. Chest pains are common, but almost never due to coronary artery obstruction. Most patients complain of significant exercise intolerance and extreme fatigue, even to activities of daily living. Some patients with POTS will also meet diagnostic criteria for chronic fatigue syndrome 7.
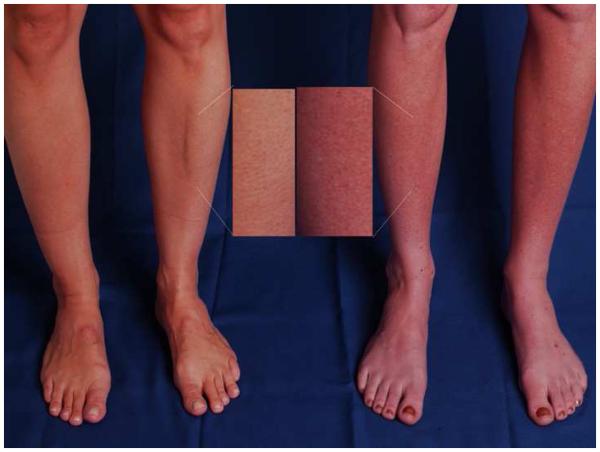
The most striking physical feature of POTS is the severe tachycardia that develops on standing from a supine position. Recent data suggests that there is a significant circadian variability in the orthostatic tachycardia in patients with POTS, with greater orthostatic tachycardia in the morning than in the evening 8. Another remarkable physical feature of POTS is the dependent acrocyanosis that occurs in close to 50% of patients with POTS (Fig 3) 1. These patients experience a dark red-blue discoloration of their legs, which are cold to the touch.
Figure 3. Acrocyanosis in Postural Tachycardia Syndrome (POTS).
A striking physical feature in POTS is the gross change in leg skin color that can occur with standing. The panel shows the legs of a healthy subject (Left Panel) and a POTS patient (Right Panel) who have each been standing for 5 minutes. The POTS patient (Right Panel) has significant dark red mottling of her legs extending up to the knees while standing, while the healthy subject does not have a similar discoloration. Figures are reprinted with permission from reference 1.
POTS Pathophysiology
Tachycardia on standing is a final common pathway of many pathophysiological processes. POTS is a heterogeneous syndrome rather than a single disease. Over the last 20 years, much has been learned about specific sub-types within POTS, although categorizing the individual patient remains difficult. Some pathophysiological phenotypes include the following:
Neuropathic POTS – some patients likely have a form of dysautonomia, with preferential denervation of sympathetic nerves innvervating the lower limbs 2, 9, 10.
Chronic Hypovolemia – Many patients with POTS have a low blood volume when formally assessed 4, 11, 12. We 4, 13 and others 14 have reported irregularities in the renin-angiotensin-aldosterone system with low aldosterone that may contribute to abnormal renal sodium handling and hypovolemia in POTS.
Hyperadrenergic POTS – Many patients have evidence of a hyperactive sympathetic nervous system, indicated by a standing plasma norepinephrine level >600 pg/ml 6. In most cases, the hyperadrenergic state is compensatory for another disorder (e.g. hypovolemia, blood pooling). Occasionally, the underlying problem may be excessive sympathetic discharge, with very high levels of upright norepinephrine. Patients can sometimes have large increases in BP on standing.
Norepinephrine Reuptake Transporter Deficiency - A specific genetic abnormality with a loss of function mutation in the norepinephrine transporter has been identified in a kindred with hyperadrenergic POTS 15. Clearance of synaptic norepinephrine is likely impaired as a result of this mutation. Many psychiatric drugs inhibit the norepinephrine reuptake transporter, recreating an orthostatic tachycardia phenotype in previously unaffected subjects 16, 17.
Mast Cell Activation Disorder - Some POTS patients have mast cell degranulation without an overt trigger. These patients have episodic flushing and abnormal increases in urine methylhistamine (the primary urinary metabolite of histamine) 18.
Investigation of POTS (Table 3)
Table 3.
Diagnostic Tests in Postural Tachycardia Syndrome (POTS)
| Diagnostic Test | Comments |
|---|---|
| Orthostatic challenge | Increase in HR ≥30bpm within 10 minutes of upright posture required for diagnosis |
| Electrocardiogram/Cardiac Monitoring | Rule out any abnormal cardiac conduction; Confirm sinus (and not ectopic) tachycardia |
| Echocardiogram | Rule out structural heart abnormalities |
| Supine and upright plasma NE | Plasma NE ≥600pg/ml suggestive of a hyperadrenergic response |
| Autonomic Function Test | Intact (and sometimes vigorous) HR & BP recovery with Valsalva |
| Blood Volume Assessment | A significant proportion of POTS patients have low blood volume |
| Other blood test: hemogram, electrolytes, thyroid function, celiac panel, Vitamin B12 and serum iron panel |
To rule other medical conditions that can promote sinus tachycardia |
HR – heart rate; NE – norepinephrine; BP – blood pressure
Orthostatic Challenge – POTS diagnostic criteria require an increase in HR of ≥30 bpm within 10 minutes of upright posture (tilt or standing, even though these are not identical 19.
Confirm Sinus Tachycardia - POTS patients should have only sinus tachycardia. An electrocardiogram should be done routinely to rule out the presence of an accessory bypass tract or any abnormalities of cardiac conduction. A Holter monitor might prove useful to exclude a re-entrant dysrhythmia, especially if the patient gives a history of paroxysmal tachycardia with a sudden onset and offset.
Echocardiogram – Required in individual cases when there is doubt about the structural integrity of the heart.
Supine and Upright Plasma Norepinephrine - The supine norepinephrine is often high normal in patients with POTS, while the upright norepinephrine is usually elevated (>600 pg/ml). This likely reflects the exaggerated sympathoneural tone that is present in many patients while upright.
Autonomic Function Tests – Responses are usually intact or exaggerated to both cardiovagal testing (sinus arrhythmia), and Valsalva BP in Phase II & IV.
Blood Volume Assessment - The blood volume is low in many patients with POTS 4, and this can be assessed in many Nuclear Medicine laboratories.
Blood Tests – complete blood count and electrolyte panel; thyroid function tests, celiac panel with gastrointestinal symptoms, vitamin B12 and iron indices.
Non-Pharmacological Treatment of POTS (Table 4)
Table 4.
Non-Pharmacological Treatment for POTS
| Measures | Mechanism | Comments |
|---|---|---|
| Exercise training | Blood volume expansion and reverses cardiac deconditioning |
Improves quality of life & physiology (if patient can complete exercise program) |
| Physical Maneuvers | ||
| Squatting | Enhances venous return | May prevent syncope |
| - Sit with feet folded up |
Prevents blood pooling | May prevent syncope |
| Waist high compression garments |
Prevents blood pooling | start with 30-40 mmHg pressure for compression garments; can be uncomfortable (hot & itchy) and fashion tragedy |
| Aggressive fluid intake | Blood volume expansion | 8 – 10 cups of water/day |
| Increased sodium intake | Blood volume expansion | Up to 200 mEq Na+/day |
| Saline IV 1-2L PRN | Blood volume expansion | “Rescue” therapy for decompensation |
Remove potentially contributory medications – especially venodilators (such as nitrates), diuretics, and norepinephrine reuptake transporter inhibiting drugs.
Reconditioning – Patients that have been sedentary or in bed for prolonged periods of time require reconditioning.
Avoid ablating the sinus node – While there are anecdotal reports of benefits with sinus node modification, many patients do poorly post-procedure (potentially with a pacemaker). The underlying problem is not in the sinus node.
Patient Education – Patients should learn to avoid aggravating factors such as dehydration (drink 8-10 cups of water/day and consume ~200 mEq Na+/day), and extreme heat. There are many patient websites, include the Vanderbilt Autonomic Dysfunction site (www.mc.vanderbilt.edu/gcec/adc).
Waist High Compression Garments - 30-40 mmHg of counter-pressure can minimize venous pooling, especially when the patient needs to stand for prolonged periods of time. Unfortunately, they can be hot, itchy and uncomfortable.
IV Saline for POTS
Acute blood volume expansion with intravenous saline 1-2 L is very effective at controlling the heart rate and acutely improving symptoms 20. Due to vascular access issues, this treatment is not practical on a day to day basis, but can be used as a “rescue medicine” at times of decompensation.
Exercise Training for POTS
Exercise has routinely been recommended as a part of the POTS treatment regimen for many years. Unfortunately, POTS patients report feeling debilitated for days post-exertion, limiting compliance with exercise training. Anecdotally, patients that did exercise seemed to have a better long-term prognosis, but it was not certain if this was a selection bias. Fu et al. have recently demonstrated the dramatic benefits of exercise 21. They administered a structured 3 month exercise program to 19 patients with POTS, and showed improved quality of life, reduced orthostatic tachycardia, and increased blood volume, stroke volume and LV mass. This study shows that exercise training is an important treatment in this population. Recommendations regarding exercise training for POTS patients are included in Table 5.
Table 5.
Fu/Levine Exercise Training Protocol for POTS Patients
| Initial Exercise Training |
| Avoid upright exercises |
| Recommend using a rowing machine, recumbent cycle or swimming. |
| Intensity: target heart rate equivalent to 75-80% of maximum steady state. |
| Duration: 3-4 sessions/week for 30-45 minutes/session. |
| Exercise Training Months 2-3 |
| Can begin upright exercise using upright bike, walking, treadmill or jogging |
| Intensity: gradually increase intensity to maximal steady state 1/week and then 2/week. |
| Duration: Increase as patient becomes fit with goal of 5 to 6 hours per week. |
| Resistance Training |
| Focus on lower body |
| Start 1/week for 15-20 minutes/session |
| Gradually increase to 2/week for 45 min/session |
| Long Term Exercise Training |
| Patients encouraged to continue exercise indefinitely |
Recommendations adapted from reference 14.
Pharmacological Treatment of POTS (Table 6)
Table 6.
Pharmacological Treatment for POTS
| Drug | Dose | Mechanism | Adverse effects | Comments |
|---|---|---|---|---|
| Propranolol | 10-20 mg PO QID |
Beta- adrenergic receptor antagonist |
Bradycardia, hypotension and bronchospasm |
Attenuates symptomatic tachycardia on standing; low doses can help; high doses not tolerated |
| Pyridostigmine | 30-60 mg PO TID |
Acetylcholinesterase inhibitor |
Abdominal cramping: diarrhea; increased sweating |
Attenuates tachycardia and improve symptoms; can be combined with propranolol |
| Fludrocortisone | 0.05–0.2 mg PO daily |
Blood volume expansion; synthetic aldosterone |
Hypertension, fluid retention and hypokalemia |
Most effective when combined with increased dietary salt & water |
| Midodrine | 2.5- 10 mg PO q4h x3/day |
Vasoconstriction; Alpha-1 adrenergic receptor agonist |
Scalp itch, Piloerection, urinary retention and hypertension |
Can improve venous return and decrease reflex tachycardia |
|
Desmopressin
(DDAVP) |
0.2 mg PO occasionally |
Acute blood volume expansion |
Water retention; hyponatremia |
Follow serum [Na+] carefully |
| Methyldopa | 125 mg PO QHS or BID |
Central Sympatholytic False neurotransmitter |
Sedation and hypotension. |
Reduce plasma norepinephrine |
| Clonidine | 0.05-0.2 mg BID (or use a long acting patch) |
Central Sympatholytic Alpha-2 receptor agonist |
Worsens fatigue; sedation & hypotension. |
Reduce plasma norepinephrine |
PO – per os; QID – 4 times per day; TID – 3 times per day; BID – twice per day; QHS – at bedtime;
Volume Expansion
Fludrocortisone 0.05-0.2 mg daily – Many patients with POTS are hypovolemic 4, so fludrocortisone (an aldosterone analogue) is often used. Through enhanced renal sodium retention, it should expand the plasma volume (although the data are poor). Potassium wasting can result in hypokalemia, so serum K+ should be monitored periodically.
Desmopressin 0.2 mg PO PRN (not daily) – Oral desmopressin promotes renal free water retention, and is often used for enuresis. Desmopressin can acutely lower standing HR in POTS and improve symptoms 22. Potential side effects include hyponatremia, edema and headache. Serum Na+ should be monitored periodically during therapy.
Sympatholysis
Propranolol 10-20 mg PO QID – Many patients report intolerance to beta-blockers when first seen at the Vanderbilt Autonomic Dysfunction Center. The vast majority of POTS patients, however, respond well hemodynamically and symptomatically to low doses of propranolol 5. Of note, more complete beta-blockade with higher doses of propranolol cause symptoms to worsen. Long acting propranolol was not found to be helpful 14. This is our 1st line pharmacological agent.
Methyldopa 125mg QHS-BID – Methyldopa is a false neurotransmitter that can lower central sympathetic tone. It is particularly useful in hyperadrenergic patients.
Clonidine 0.05-0.2 mg PO BID (or a long acting patch) - Alpha 2 adrenergic agonist that acts centrally to decrease sympathetic nervous system tone. It can stabilize HR and BP, but it can also cause drowsiness, fatigue and worsen the mental clouding of some patients.
Vasoconstrictor Therapy
Midodrine 5-10mg PO q4H x3/day - Since a failure of vascular resistance may be an integral part of neuropathic POTS, vasoconstrictors such as midodrine (alpha-1 agonist) can be employed 23.
Increasing Vagal Tone
Pyridostigmine 30-60 mg PO TID – Pyridostigmine is a peripheral acetylcholinesterase inhibitor. By increasing synaptic acetylcholine at both the autonomic ganglia and the peripheral muscarinic parasympathetic receptors, pyridostigmine significantly restrains the heart rate in response to standing in patients with POTS 24, 25. Pyridostigmine is most effective in combination with low dose propranolol. Since pyridostigmine enhances bowel motility, it is often not well tolerated in patients with diarrhea-predominant irritable bowel syndrome symptoms 26.
Vanderbilt Approach to Pharmacotherapy for POTS
In addition to initial non-pharmacological approaches, and strong advice about an exercise regimen, most POTS patients require some pharmacotherapy. We will often start with low-dose propranolol. If the patient has hypovolemia, then we will add in fludrocortisone. As 3rd line therapy, if the patient is very hyperadrenergic, then we might consider a central sympatholytic; otherwise midodrine would be our 3rd line agent.
CONCLUSIONS/SUMMARY
POTS is a multisystem disorder of the autonomic nervous system. The hallmark manifestation is symptomatic orthostatic tachycardia, with lightheadedness and presyncope. While it is not primarily a syncopal disorder, a minority of patients can also have VVS. POTS is associated with substantial functional disability among otherwise healthy people. Patients with POTS demonstrate a heart rate increase of >30 bpm with standing (within 10 minutes), often have high levels of upright plasma norepinephrine, and many patients have a low blood volume. Exercise training has been found to be highly effective at improving the physiology and symptoms in POTS patients. Pharmacological therapies aimed at correcting the hypovolemia and the excess sympathetic tone may also help improve the symptoms.
Key Points.
Most patients who present to a cardiologist with syncope have vasovagal (reflex) syncope.
A common confounder of vasovagal syncope and presyncope is postural tachycardia syndrome (POTS), a multisystem disorder of the autonomic nervous system.
The hallmark manifestation of POTS is symptomatic orthostatic tachycardia, with lightheadedness and presyncope.
Patients with POTS demonstrate a heart rate increase of >30 bpm with standing (within 10 minutes), often have high levels of upright plasma norepinephrine, and often have a low blood volume.
Postural tachycardia syndrome can often be differentiated from vasovagal syncope by its hemodynamic pattern during tilt table test and differing clinical characteristics.
Exercise training has been found to be highly effective at improving the physiology and symptoms in POTS patients. Pharmacological therapies aimed at correcting the hypovolemia and the excess sympathetic tone may also help improve the symptoms.
ACKNOWLEDGEMENTS
We thank Dr. David Robertson for his leadership in the field of Autonomic Disorders, and his training numerous investigators in the field of autonomic physiology. We also thank Dr. Emily M Garland for her thoughtful review of this manuscript.
Research Funding - Supported in part by NIH grants R01 HL102387, P01 HL56693, and UL1 TR000445 (Clinical and Translational Science Award).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest - None
Reference List
- (1).Raj SR. The Postural Tachycardia Syndrome (POTS): pathophysiology, diagnosis & management. Indian Pacing Electrophysiol J. 2006;6:84–99. [PMC free article] [PubMed] [Google Scholar]
- (2).Schondorf R, Low PA. Idiopathic postural orthostatic tachycardia syndrome: an attenuated form of acute pandysautonomia? Neurology. 1993;43:132–7. doi: 10.1212/wnl.43.1_part_1.132. [DOI] [PubMed] [Google Scholar]
- (3).Robertson D. The epidemic of orthostatic tachycardia and orthostatic intolerance. Am J Med Sci. 1999;317:75–7. doi: 10.1097/00000441-199902000-00001. [DOI] [PubMed] [Google Scholar]
- (4).Raj SR, Biaggioni I, Yamhure PC, Black BK, Paranjape SY, Byrne DW, Robertson D. Renin-aldosterone paradox and perturbed blood volume regulation underlying postural tachycardia syndrome. Circulation. 2005;111:1574–82. doi: 10.1161/01.CIR.0000160356.97313.5D. [DOI] [PubMed] [Google Scholar]
- (5).Raj SR, Black BK, Biaggioni I, Paranjape SY, Ramirez M, Dupont WD, Robertson D. Propranolol decreases tachycardia and improves symptoms in the postural tachycardia syndrome: less is more. Circulation. 2009;120:725–34. doi: 10.1161/CIRCULATIONAHA.108.846501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Garland EM, Raj SR, Black BK, Harris PA, Robertson D. The hemodynamic and neurohumoral phenotype of postural tachycardia syndrome. Neurology. 2007;69:790–8. doi: 10.1212/01.wnl.0000267663.05398.40. [DOI] [PubMed] [Google Scholar]
- (7).Okamoto LE, Raj SR, Peltier A, Gamboa A, Shibao C, Diedrich A, Black BK, Robertson D, Biaggioni I. Neurohumoral and haemodynamic profile in postural tachycardia and chronic fatigue syndromes. Clin Sci (Lond) 2012;122:183–92. doi: 10.1042/CS20110200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Brewster JA, Garland EM, Biaggioni I, Black BK, Ling JF, Shibao CA, Robertson D, Raj SR. Diurnal variability in orthostatic tachycardia: implications for the postural tachycardia syndrome. Clin Sci (Lond) 2012;122:25–31. doi: 10.1042/CS20110077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Streeten DH. Pathogenesis of hyperadrenergic orthostatic hypotension. Evidence of disordered venous innervation exclusively in the lower limbs. J Clin Invest. 1990;86:1582–8. doi: 10.1172/JCI114878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Jacob G, Costa F, Shannon JR, Robertson RM, Wathen M, Stein M, Biaggioni I, Ertl A, Black B, Robertson D. The neuropathic postural tachycardia syndrome. N Engl J Med. 2000;343:1008–14. doi: 10.1056/NEJM200010053431404. [DOI] [PubMed] [Google Scholar]
- (11).Fouad FM, Tadena-Thome L, Bravo EL, Tarazi RC. Idiopathic hypovolemia. Ann Intern Med. 1986;104:298–303. doi: 10.7326/0003-4819-104-3-298. [DOI] [PubMed] [Google Scholar]
- (12).Streeten DH, Thomas D, Bell DS. The roles of orthostatic hypotension, orthostatic tachycardia, and subnormal erythrocyte volume in the pathogenesis of the chronic fatigue syndrome. Am J Med Sci. 2000;320:1–8. doi: 10.1097/00000441-200007000-00001. [DOI] [PubMed] [Google Scholar]
- (13).Mustafa HI, Garland EM, Biaggioni I, Black BK, Dupont WD, Robertson D, Raj SR. Abnormalities of angiotensin regulation in postural tachycardia syndrome. Heart Rhythm. 2011;8:422–8. doi: 10.1016/j.hrthm.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (14).Fu Q, Vangundy TB, Shibata S, Auchus RJ, Williams GH, Levine BD. Exercise training versus propranolol in the treatment of the postural orthostatic tachycardia syndrome. Hypertension. 2011;58:167–75. doi: 10.1161/HYPERTENSIONAHA.111.172262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Shannon JR, Flattem NL, Jordan J, Jacob G, Black BK, Biaggioni I, Blakely RD, Robertson D. Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency. N Engl J Med. 2000;342:541–9. doi: 10.1056/NEJM200002243420803. [DOI] [PubMed] [Google Scholar]
- (16).Vincent S, Bieck PR, Garland EM, Loghin C, Bymaster FP, Black BK, Gonzales C, Potter WZ, Robertson D. Clinical assessment of norepinephrine transporter blockade through biochemical and pharmacological profiles. Circulation. 2004;109:3202–7. doi: 10.1161/01.CIR.0000130847.18666.39. [DOI] [PubMed] [Google Scholar]
- (17).Schroeder C, Tank J, Boschmann M, Diedrich A, Sharma AM, Biaggioni I, Luft FC, Jordan J. Selective norepinephrine reuptake inhibition as a human model of orthostatic intolerance. Circulation. 2002;105:347–53. doi: 10.1161/hc0302.102597. [DOI] [PubMed] [Google Scholar]
- (18).Shibao C, Arzubiaga C, Roberts LJ, Raj S, Black B, Harris P, Biaggioni I. Hyperadrenergic postural tachycardia syndrome in mast cell activation disorders. Hypertension. 2005;45:385–90. doi: 10.1161/01.HYP.0000158259.68614.40. [DOI] [PubMed] [Google Scholar]
- (19).Plash WB, Diedrich A, Biaggioni I, Garland EM, Paranjape SY, Black BK, Dupont WD, Raj SR. Diagnosing Postural Tachycardia Syndrome: Comparison of Tilt Test versus Standing Hemodynamics. Clin Sci (Lond) 2012 doi: 10.1042/CS20120276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Jacob G, Shannon JR, Black B, Biaggioni I, Mosqueda-Garcia R, Robertson RM, Robertson D. Effects of volume loading and pressor agents in idiopathic orthostatic tachycardia. Circulation. 1997;96:575–80. doi: 10.1161/01.cir.96.2.575. [DOI] [PubMed] [Google Scholar]
- (21).Fu Q, Vangundy TB, Galbreath MM, Shibata S, Jain M, Hastings JL, Bhella PS, Levine BD. Cardiac origins of the postural orthostatic tachycardia syndrome. J Am Coll Cardiol. 2010;55:2858–68. doi: 10.1016/j.jacc.2010.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Coffin ST, Black BK, Biaggioni I, Paranjape SY, Orozco C, Black PW, Dupont WD, Robertson D, Raj SR. Desmopressin acutely decreases tachycardia and improves symptoms in the postural tachycardia syndrome. Heart Rhythm. 2012;9:1484–90. doi: 10.1016/j.hrthm.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Grubb BP, Karas B, Kosinski D, Boehm K. Preliminary observations on the use of midodrine hydrochloride in the treatment of refractory neurocardiogenic syncope. J Interv Card Electrophysiol. 1999;3:139–43. doi: 10.1023/a:1009813312936. [DOI] [PubMed] [Google Scholar]
- (24).Raj SR, Black BK, Biaggioni I, Harris PA, Robertson D. Acetylcholinesterase inhibition improves tachycardia in postural tachycardia syndrome. Circulation. 2005;111:2734–40. doi: 10.1161/CIRCULATIONAHA.104.497594. [DOI] [PubMed] [Google Scholar]
- (25).Singer W, Opfer-Gehrking TL, Nickander KK, Hines SM, Low PA. Acetylcholinesterase inhibition in patients with orthostatic intolerance. J Clin Neurophysiol. 2006;23:476–81. doi: 10.1097/01.wnp.0000229946.01494.4c. [DOI] [PubMed] [Google Scholar]
- (26).Kanjwal K, Karabin B, Sheikh M, Elmer L, Kanjwal Y, Saeed B, Grubb BP. Pyridostigmine in the treatment of postural orthostatic tachycardia: a single-center experience. Pacing Clin Electrophysiol. 2011;34:750–5. doi: 10.1111/j.1540-8159.2011.03047.x. [DOI] [PubMed] [Google Scholar]
- (27).Raj SR, Sheldon RS. Head-up tilt-table test. In: Saksena S, Camm AJ, editors. Electrophysiological Disorders of the Heart. 2nd ed Saunders; New York: 2012. pp. 73-1–73-11. [Google Scholar]