Abstract
Context/objective
Rehabilitation teams generally are described as consisting of a single representative of 6–8 disciplines, but research suggests that the number of individuals involved may be much larger. This study aimed to determine the size of teams in spinal cord injury (SCI) rehabilitation, and the effect of team size on patients' active participation in their treatment sessions.
Design
Prospective observational study.
Setting
Six SCI rehabilitation centers.
Participants
A total of 1376 patients with traumatic SCI admitted for first rehabilitation.
Interventions
Not applicable.
Outcome measures
Number of treatment sessions, by discipline and overall clinician rating of active participation of the patient; Treatment Concentration Index (TCI) calculated as Σpk2 (where p refers to the proportion of treatment sessions delivered by team member k).
Results
The average patient was treated by 39.3 different clinicians. The numbers were especially high for physical therapy (mean: 8.8), occupational therapy (7.2), and nursing (16.1). TCI was 0.08 overall; it varied by discipline. TCI was negatively correlated with length of stay, except for psychology. Participation ratings were minimally affected by the number of sessions the patient and the therapist had worked together.
Conclusions
In SCI rehabilitation, teams are at least as large as suggested by previous research. However, this may not mean lack of familiarity of patient and therapist with one another, or alternatively, the possibly weak therapeutic alliance does not affect the patients' active participation in their sessions. Further research is needed to determine whether there are negative effects on rehabilitation outcomes.
Keywords: Continuity of patient care, Health services, Patient participation, Rehabilitation, Spinal cord injuries, Outcomes
Introduction
‘Teamwork is the cornerstone of rehabilitation medicine’(ref.1 p. 352). The idea of the “team” has been central to medical (physical) rehabilitation for almost as long as rehabilitation has been a recognized function of the health care system, but certainly since the development of separate rehabilitation units and hospitals after the World War II.2,3 The premise underlying team care always has been that assorted professionals, each contributing their own discipline's expertise and closely cooperating through oral and written communication (team rounds, informal hallway discussions, medical record entries, etc.) are able to achieve outcomes that are superior to those of a lone clinician, or of a number of different clinicians each practicing independently of all others.4 The potential downsides of health care teams (eroding the clinician's autonomy; undermining clinical decision making) are in the main overlooked.5
Even though it is generally accepted that the team is and should be the modus operandi of rehabilitation, we still have limited understanding of how this ‘dominant model of care delivery in the inpatient setting’ (ref.6 p. 537) affects outcomes,2,3,7–11 although some have claimed otherwise.12,13 Much effort has gone into discussions focused on whether the team ought to be or is multidisciplinary (cross functional) or interdisciplinary (interprofessional) or even transdisciplinary.9,11,14–22 Cott23 calls this the ‘preponderance of rhetorical ‘how-to’ literature about teamwork with very little research and theory about health care teams' (p. 848). The team's functioning per se has been investigated from angles such as leadership, social climate (teamness), interprofessional relations, problem solving, conflict management, and a number of other sociopsychological constructs, with a focus on team rounds and little attention to the team members' interactions outside of formal meetings.2,3,6,18,19,22,24–26 Research examining whether the quality and intensity of rehabilitation team functioning make a difference in terms of patient outcomes is limited to a few studies by Strasser et al.,2,27 although there are some earlier investigations, discussed by Halstead,28 which reported ‘few consistent changes or trends across all studies’ (p. 508).
It is worth noting that almost always when the rehabilitation team and its functioning are described, the members of each discipline are listed using the singular. For instance: ‘Teams may differ depending on the individual programs but many include the following health care professionals: physician, nurse, physical therapist, occupational therapist, speech/language pathologist, psychologist and social worker’ (ref.29 p. 182–3). The major issue seems to be whether particular disciplines belong on the team, and thus whether the number of individuals sitting around the table for interdisciplinary conferences, the hallmark of the team approach, is six or seven or a somewhat larger number.2,13 However, studies of rehabilitation teams and team functioning have reported vastly greater numbers: average numbers of 8.6,14 11.5,2 19.0,30 44.0,18 44.3,19 a ‘core team’ of over 40,8 47,22 and up to 50, ‘a number that the teamworking literature would consider too large for the necessary social functions to operate’ (ref.31 p. 246). While patients, family members or students may have been included in some of these counts, it is clear that once one begins counting the multiple representatives of particular disciplines, especially of nursing, the team that takes care of a particular patient is too large to fit around the conference room table.
That also suggests that the team has a challenge: how do so many people exchange information on progress, problems, necessary next steps, etc. to coordinate the treatment of a particular patient and achieve continuity of care? How do they even know everyone,31 or agree on who is part of the team?10 While the proverbial chart rounds meeting may serve to provide communication between the primary clinicians of each discipline,8 how do they communicate the same information to others – the non-primary participants on the team? The medical record as a communication document has been declared to be unsatisfactory for all but the rehabilitation medicine representative; to supplement it there are departmental record notes, shift reports, and informal exchanges in hallways and treatment gyms,8 and probably many other unofficial mechanisms. Still, the question remains: how does a team of 40+ specialists separated by disciplinary and other barriers manage to achieve the advantage that the interdisciplinary team presumably brings?
This study aims to answer two questions related to that issue: (1) How many staff members are involved in an episode of inpatient rehabilitation care for a particular patient, within and across disciplines? and (2) Does team size have an impact on the quality of the interactions between each professional and the patient? With regard to the latter, we hypothesized that the larger the number of clinicians involved, the less chance each has to get to know the patient as an individual, and consequently the poorer performance they would manage to get out of the patient.
Methods
The SCIRehab project is a multi-center collaborative study that is quantifying the interventions provided during spinal cord injury (SCI) rehabilitation, with the goal of relating those treatments to outcomes at discharge and at 1 year after injury.32,33 The study is led by the Rocky Mountain Regional Spinal Injury System at Craig Hospital and involves collaboration with five other specialized SCI rehabilitation programs: Shepherd Center, Rehabilitation Institute of Chicago, Carolinas Rehabilitation, The Mount Sinai Medical Center, and MedStar National Rehabilitation Hospital.
Each site obtained institutional review board approval for this observational study, and tried to enroll all patients who were 12 years of age or older, gave informed consent (or whose parent/guardian gave consent, for minors), and were admitted to the facility's SCI unit for initial rehabilitation following traumatic SCI. Patients requiring transfer to medical/surgical units during their rehabilitation program were retained in the study, no matter how long they spent in acute care before returning to the rehabilitation unit; their acute care days were not counted as part of the rehabilitation length of stay (LOS). Patients who spent more than 2 weeks in another Inpatient Rehabilitation Facility (IRF) prior to admission to the SCIRehab facility were excluded, as were patients who spent more than a week of their rehabilitation stay on a non-SCI rehabilitation unit in the participating SCIRehab facility, because staff of the non-SCI units were not trained in the data collection methods.
Patient and injury data
Most patient and injury data were abstracted from patient medical records. In addition, all sites collected the SCI Model Systems' standardized information on injury through community discharge (Form I).34 The International Standards of Neurological Classification of SCI (ISNCSCI)35 were used to describe the neurologic level and completeness of injury; the Functional Independence Measure (FIM®)36 served to describe a patient's functioning level in motor and cognitive tasks at admission.
Treatment data
The data requirements for the SCIRehab project necessitated the completion of discipline-specific special documentation by each clinician as he/she delivered care. This point-of-care (POC) documentation supplemented medical record entries for Psychology (PS), Physical Therapy (PT), Occupational Therapy (OT), Therapeutic Recreation (TR), Social Work/Case Management (SW), and Speech Therapy (ST). Nursing (NU) decided that their routine nursing record entries were sufficient for routine non-rehabilitative care (washing and dressing patients, medication management, wound care, etc.) but not for patient education and care management, for which supplemental documentation was created. Each discipline developed documentation strategies to capture details of the treatments provided to patients.37 At the core of the documentation was a taxonomy, described in detail previously, of the discipline's treatment activities and interventions.38–44 All staff in the named disciplines used electronic data capture on a handheld personal digital assistant (PDA) to record details about each treatment session. Physicians and respiratory therapists determined that their medical record entries were sufficient to reflect their interventions.
PT, OT, TR, and ST clinicians captured the following session details: date/time of the session, center identity, patient and therapist code, group or individual session, intervention activities performed in the session (complete with activity-specific details), and session-level variables, such as co-treatment with another therapist or discipline, and degree of family participation. PS and SW clinicians recorded interactions with or on behalf of patients that typically occur at multiple times over the course of a day, rather than in scheduled sessions. For each day, these staff recorded in the PDA intervention activities or topic/content areas that had been addressed, with whom, and for how long.38,44 Nursing representatives completed their POC supplementary documentation to record the content and duration of bedside education and of care management activities.41
Each discipline chose to use time (number of minutes) to measure the dosage of their interventions. The clinicians documented the number of minutes spent on every separate activity, rounded to the nearest multiple of 5 minutes; interventions that consumed less than 5 minutes (10 minutes for NU) were not documented. The minutes for the various therapeutic activities combined add to the approximate duration of time spent each session (or each day or shift) by each clinical discipline. These time records are the focus of this analysis, along with the clinicians' ratings of the participation in the session by the patient.
Participation of the patient in the treatment session was rated by PT and OT on the Pittsburgh Rehabilitation Participation Scale (PRPS).45 The characterizations available for the patient's effort and active involvement were on a six-point scale (see Table 1); ‘not applicable’ was available for those situations where the therapist dealt with e.g. a family member but the patient was not present. TR and ST used a variation of the PRPS that used the same labels, but adjusted the description as appropriate to their services. The PS staff used a modification with the categories (5) Engaged, (4) Active, (3) Passive, (2) Resistive, and (1) Refused, while NU used (4) Engaged, (3) Active, (2) Passive and (1) Refused. SW did not complete a participation scale.
Table 1.
Categories of the modified Pittsburgh Rehabilitation Participation Scale as used by PT and OT
|
POC data completeness and reliability
The project team provided clinician training at each of the SCIRehab centers. Clinicians' knowledge of the taxonomy and completion of the POC documentation were tested at regular intervals using written scenarios describing treatment sessions with hypothetical patients. Those clinicians scoring less than a cut-off point of adequacy received additional tutoring by the local coordinator or their lead clinician.
Project local coordinators compared POC entries for each discipline with scheduling, billing, or other clinical records to ensure that all sessions were included in the POC data. If a session had been scheduled or was billed but not documented, the coordinator reported this to the therapist and the lead clinician involved so that it could be added to the database.
Data processing and analysis
A total of 307 452 records were submitted across the seven disciplines. Eliminated were 241 with a missing date or clinician identification number (<0.1%) and 1750 (0.6%) that were apparently duplicate reports (same patient, clinician, date, and start time), possibly due to clinician forgetfulness or equipment malfunction, leaving 305 457 useful records.
To summarize the degree to which the sessions of a particular discipline that a patient received were delivered by a few clinicians, or by many, a Treatment Concentration Index (TCI) was calculated using the formula: Σpk2, where p refers to the proportion of treatment sessions delivered by team member k. When a single therapist delivers all treatments for a particular patient, the TCI takes on its highest value, 1.0. The minimum value is not fixed, but depends on the number of treatment sessions. It becomes indistinguishable from 0.0 as the number of sessions and the number of therapists approach infinity. When the primary therapist delivers 20 out of 29 sessions, and six colleagues divide the other 9, the TCI is around 0.50. When 10 sessions are delivered by 10 different therapists, the value is 0.01, suggesting that values smaller than 0.10 are reached rather easily.
Basic statistical methods are used to describe the data – percentages, means and the corresponding SDs, percentiles, Pearson product moment correlations, and partial correlations based on the zero-order correlations. Partial correlations express the strength of the relationship between two variables after the effect of specific additional variables on the two has been deleted. Regression analysis is used to disentangle the effects of various predictors on PRPS ratings. This was done twice – once with and once without session sequence number as a predictor. Where statistical tests are reported, these are two-sided tests.
Results
Patients
The percentage of eligible patients who consented to be enrolled was 90% overall, and varied from 71 to 97% by SCIRehab center. Demographic and injury information on the 1376 patients admitted during SCIRehab recruitment is provided in Table 2. The group does not appear much different from the typical SCI patient served in the SCI model systems of care. The average rehabilitation stay was 55.5 days (excluding interruptions for returns to acute medical care), but this hides a great variation: the shortest difference between the first and last day on which treatment was provided per the POC documentation was 2, and the longest 323.
Table 2.
Demographic, injury, and hospitalization characteristics of patients
| Characteristics | Percentages | Meanand SD |
|---|---|---|
| Age | 37.6 (16.9) | |
| Gender | ||
| Male | 80.7 | |
| Race/ethnicity | ||
| White | 65.1 | |
| Black | 20.7 | |
| Hispanic | 9.1 | |
| Other | 5.0 | |
| Language skill | ||
| English primary language | 94.3 | |
| Understands sufficient English | 2.3 | |
| No English | 3.3 | |
| Primary payer | ||
| Medicare | 7.9 | |
| Medicaid | 18.5 | |
| Private insurance | 60.1 | |
| Worker's compensation | 10.1 | |
| Marital status | ||
| Married | 38.1 | |
| Education | ||
| Less than high school diploma | 19.4 | |
| High school diploma or GED | 47.0 | |
| Mora than high school diploma | 23.8 | |
| Other/unknown | 9.8 | |
| Occupational status | ||
| Working | 64.8 | |
| Student | 15.4 | |
| Other | 19.8 | |
| Injury etiology | ||
| Vehicular | 48.0 | |
| Violence | 10.6 | |
| Sports | 6.1 | |
| Fall or falling object | 24.6 | |
| Other | 10.7 | |
| Neurological injury group | ||
| C1–4, ASIA A, B or C | 28.6 | |
| C5–8, ASIA A, B or C | 19.6 | |
| T1–S5, ASIA A, B or C | 36.3 | |
| ASIA D (any level of injury) | 15.6 | |
| Days from injury to rehabilitation | 30.4 (27.2) | |
| Length of rehabilitation stay* | 55.5 (37.0) | |
| Length of treatment period** | 56.5 (37.9) | |
| Admission Total FIM score | 52.0 (14.1) | |
| Admission Motor FIM score | 23.5 (11.1) | |
| Admission Cognitive FIM score | 28.6 (6.0) | |
*Calculated as the difference between the first and last day in the rehabilitation unit, less all days the patient was off the unit (short-term intermissions).
**Calculated as the difference between the first day any reported treatment took place and the last day any reported treatment took place.
Treatment sessions
Table 3 provides information on the treatment sessions the average patient received. The mean number of sessions was 222.0, or 4.1 per average day of the stay; however, there was a large variation, with the number of sessions over the stay ranging from 8 to 931. Individual sessions (189.5 on average) were more common than group sessions (32.5). Because NU operates two or three shifts, 7 days a week, it is not surprising that nursing treatments make up the largest component (65.9 mean per stay, or 29.7% of the total), while ST, which is ordered for a minority of patients, contributes only 6.2 (2.8%) of the total.
Table 3.
Length of treatment period, total sessions over the stay, and sessions per day, by discipline and overall
| Mean | SD | Range | Minimum | Maximum | 25th percentile | 50th percentile | 75th percentile | |
|---|---|---|---|---|---|---|---|---|
| Length of treatment period* | 56.5 | 37.9 | 321 | 2 | 323 | 30.0 | 45.0 | 73.0 |
| Total sessions | 222.0 | 129.5 | 923 | 8 | 931 | 131.0 | 193.0 | 281.8 |
| Total individual sessions | 189.5 | 113.4 | 843 | 8 | 851 | 115.0 | 165.0 | 239.8 |
| Total group sessions | 32.5 | 32.3 | 215 | 0 | 215 | 12.0 | 21.0 | 43.0 |
| Total sessions per day | 4.1 | 0.8 | 6.3 | 0.5 | 6.8 | 3.7 | 4.2 | 4.6 |
| Individual sessions per day | 3.6 | 0.9 | 6.2 | 0.4 | 6.6 | 3.0 | 3.6 | 4.1 |
| Group sessions per day | 0.6 | 0.4 | 2.1 | 0.0 | 2.1 | 0.3 | 0.5 | 0.8 |
| Total PT sessions | 59.8 | 42.9 | 326 | 2 | 328 | 29.0 | 45.0 | 80.8 |
| Total OT sessions | 53.7 | 38.6 | 290 | 0 | 290 | 28.0 | 41.5 | 69.8 |
| Total ST sessions | 6.2 | 14.0 | 163 | 0 | 163 | 0.0 | 0.0 | 6.0 |
| Total TR sessions | 11.8 | 8.8 | 49 | 0 | 49 | 5.0 | 11.0 | 18.0 |
| Total PS sessions | 13.1 | 13.7 | 129 | 0 | 129 | 5.0 | 9.0 | 16.0 |
| Total SW sessions | 11.5 | 13.3 | 107 | 0 | 107 | 3.0 | 7.0 | 15.0 |
| Total NU sessions | 65.9 | 38.7 | 332 | 0 | 332 | 41.0 | 60.0 | 83.0 |
*Calculated as the days elapsed between the first and last recorded treatment session, which not necessarily coincides with the dates of rehabilitation admission and discharge.
Clinicians
Over the duration of their stay, patients typically get treatment from more than one clinician, except for ST, SW, and PS. (Table 4). Depending on circumstances, especially LOS, the number easily is as high as 10 for PT (the 75th percentile was 11), 8 for OT, and 20 for NU. Not surprisingly, the disciplines of which the typical IRF has more representatives on staff (OT, PT, and NU) have the higher median scores.
Table 4.
Number of therapists and nurses providing services over a patient's stay, by discipline and overall
| Discipline | Patients | Mean | SD | Range | Minimum | Maximum | 25th percentile | 50th percentile | 75th percentile |
|---|---|---|---|---|---|---|---|---|---|
| PT | 1376 | 8.8 | 5.0 | 25 | 1 | 26 | 5 | 7 | 11 |
| OT | 1375 | 7.2 | 3.5 | 20 | 1 | 21 | 5 | 7 | 9 |
| ST | 594 | 1.6 | 1.0 | 5 | 1 | 6 | 1 | 1 | 2 |
| TR | 1259 | 4.3 | 2.6 | 11 | 1 | 12 | 2 | 4 | 6 |
| PS | 1342 | 1.7 | 0.8 | 4 | 1 | 5 | 1 | 1 | 2 |
| SW | 1197 | 1.2 | 0.5 | 3 | 1 | 4 | 1 | 1 | 1 |
| NU | 1371 | 16.1 | 6.8 | 44 | 1 | 45 | 12 | 16 | 20 |
| All | 1376 | 39.3 | 13.5 | 77 | 5 | 82 | 30 | 38 | 48 |
Treatment concentration
Table 5 summarizes information on the distribution of the TCI, for each of the disciplines separately and combined. For disciplines that offer group sessions, the TCI based on the individual treatment sessions only is also provided. The lowest mean TCI value is observed for NU. The highest mean values were found for SW, PS, and ST, at least 0.87. TR, OT, and PT occupied an intermediate position, with TCI values in the 0.45–0.50 range. For disciplines that offered group treatment, the TCI based on individual sessions only in all instances was higher than the all-sessions index, by a value of 0.08 or more. It should be noted that there is for all disciplines great variability among patients: with a few exceptions, the TCI value for the 75th percentile is at least 0.20 or even 0.30 higher than that for the 25th percentile. The maximum TCI value of 1.00 (all sessions delivered by a single clinician) is actually found for all disciplines; this generally occurs when patients had an abbreviated stay, but is not uncommon for ST, TR individual sessions, SW and PS, where 75th percentile values of 1.00 are found. For SW and PS individual sessions, 1.00 is the 25th percentile value, suggesting that the greater part of patients interact with one clinician only.
Table 5.
Treatment concentration index (TCI) for various disciplines and overall, based on all treatment sessions, and on individual (rather than group and individual combined) treatment sessions
| Discipline and format |
Patients | Mean | SD | Range | Minimum | Maximum | 25th % | 50th % | 75th % | |
|---|---|---|---|---|---|---|---|---|---|---|
| PT | All | 1376 | 0.45 | 0.21 | 0.93 | 0.07 | 1.00 | 0.27 | 0.42 | 0.60 |
| PT | Individual | 1375 | 0.53 | 0.22 | 0.90 | 0.10 | 1.00 | 0.34 | 0.52 | 0.70 |
| OT | All | 1375 | 0.50 | 0.21 | 0.90 | 0.10 | 1.00 | 0.32 | 0.47 | 0.65 |
| OT | Individual | 1374 | 0.60 | 0.20 | 0.85 | 0.15 | 1.00 | 0.44 | 0.59 | 0.75 |
| ST* | All | 594 | 0.87 | 0.20 | 0.74 | 0.26 | 1.00 | 0.78 | 1.00 | 1.00 |
| TR | All | 1259 | 0.51 | 0.30 | 0.88 | 0.12 | 1.00 | 0.27 | 0.39 | 0.72 |
| TR | Individual | 1216 | 0.63 | 0.28 | 0.85 | 0.15 | 1.00 | 0.38 | 0.55 | 1.00 |
| PS | All | 1342 | 0.82 | 0.22 | 0.75 | 0.25 | 1.00 | 0.63 | 1.00 | 1.00 |
| PS | Individual | 1331 | 0.95 | 0.13 | 0.64 | 0.36 | 1.00 | 1.00 | 1.00 | 1.00 |
| SW* | All | 1197 | 0.95 | 0.13 | 0.67 | 0.33 | 1.00 | 1.00 | 1.00 | 1.00 |
| NU* | All | 1371 | 0.16 | 0.13 | 0.96 | 0.04 | 1.00 | 0.11 | 0.13 | 0.16 |
| All | All | 1376 | 0.08 | 0.03 | 0.35 | 0.03 | 0.39 | 0.07 | 0.08 | 0.09 |
| All | Individual | 1376 | 0.10 | 0.04 | 0.72 | 0.04 | 0.77 | 0.08 | 0.09 | 0.11 |
*There were no ST, SW, or NU group sessions.
Determinants of treatment concentration
In addition to discipline, LOS determines TCI, as reflected in Table 6. Generally, the longer a patient's stay, the more likely it is he or she will see care delivered by more than a few therapists (as indicated by the negative correlations). However, there is no such relationship for SW and PS – suggesting that the same clinician is likely to be involved in the case whatever the duration of treatment.
Table 6.
Correlation of TCI with length of stay, and with average patient participation rating, by discipline and overall
| Discipline | Correlation with LOS | N | Correlation with participation rating | Partial correlation with participation rating* |
|---|---|---|---|---|
| PT | −0.24*** | 1376 | −0.09*** | −0.12*** |
| OT | −0.33*** | 1375 | 0.09*** | 0.02 |
| ST | −0.17*** | 594 | 0.07 | 0.06 |
| TR | −0.13*** | 1259 | −0.31*** | −0.33*** |
| PS | 0.26*** | 1342 | −0.02 | −0.05 |
| SW | 0.04 | 1197 | – | – |
| NU | −0.09*** | 1371 | 0.35*** | 0.36*** |
| All | −0.15*** | 1376 | – | – |
*Controlling for length of stay.
***Significant at P < 0.001.
The effects of treatment concentration
The ratings of patient participation across all sessions are shown, by discipline, in Fig. 1. (SW did not rate patient participation). Most ratings are in the high-positive range: active or engaged for PS and NU, excellent or very good for TR, ST, PT, and OT. It seems that different processes linking treatment concentration to participation ratings are at work in the disciplines (Table 6): while there essentially is no effect for PS, both NU and OT give higher average ratings when TCI is high (treatment delivered by relatively few clinicians), but the reverse is true for TR and PT. When the relationship is controlled (using partial correlation coefficients) for LOS or for total number of treatments delivered by all clinicians in the discipline combined, the negative correlation for TR remains, but so does the positive correlation for NU.
Multiple regression was used to further investigate this phenomenon. (Table 7) Because exploratory investigation had suggested that participation ratings increased over the duration of a patient's stay, but then started to decrease again as discharge neared, these analyses incorporated days from admission and days until discharge, in raw format and squared to take into account simple non-linear effects. Also controlled were the patient's tendency to get high participation scores from all therapists in a particular discipline who dealt with him/her (presumably reflecting his or her effort and motivation whoever the therapist was), and the therapist's tendency to give out high or low participation grades, across all of his or her patients. The session sequence number (counting only sessions of this particular patient being treated by this particular therapist) still had an effect on participation rating: the more the therapist had worked with the patient, the higher that patient's participation was rated. There was a weaker contrary effect for session sequence number squared, suggesting that the relationship is not linear.
Table 7.
Regression of participation rating on various patient and therapist characteristics: percent of variance explained and predictor beta coefficients
| Discipline |
||||||
|---|---|---|---|---|---|---|
| PT | OT | ST | TR | PS | NU | |
| Adjusted R2 without session sequence number | 0.42 | 0.41 | 0.42 | 0.41 | 0.60 | 0.35 |
| Adjusted R2 with session sequence number | 0.42 | 0.41 | 0.42 | 0.41 | 0.60 | 0.35 |
| Beta coefficient (for models with session number) | ||||||
| Days from admission | 0.02* | 0.08*** | 0.11*** | 0.10*** | 0.08*** | |
| Days from admission-squared | −0.03*** | −0.07* | −0.05** | −0.06*** | ||
| Days until discharge | 0.05*** | 0.03*** | 0.05* | 0.06*** | 0.15*** | |
| Days until discharge-squared | −0.06*** | 0.07*** | ||||
| Session sequence number | 0.10*** | 0.05*** | 0.05*** | 0.09*** | 0.04*** | |
| Session sequence number-squared | −0.06*** | −0.03*** | −0.07*** | −0.04*** | ||
| Patient average participation | 0.46*** | 0.51*** | 0.60*** | 0.45*** | 0.75*** | 0.30*** |
| Therapist average participation | 0.29*** | 0.23*** | 0.11*** | 0.30*** | 0.03*** | 0.41*** |
*Significant at P < 0.05; **significant at P < 0.01; ***significant at P < 0.001.
Figure 1.
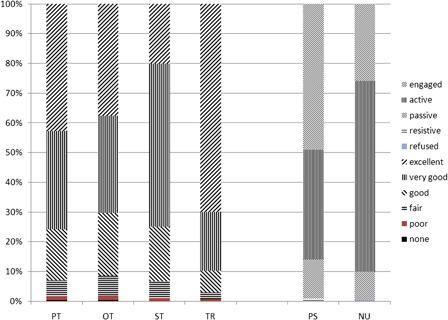
Ratings on the (modified) Pittsburgh Rehabilitation Participation Scale, by discipline.
Discussion
Continuity of care, whether it involves transfers between shifts in a hospital, coordination between phases of care (e.g. inpatient acute rehabilitation and subacute rehabilitation or home care), or collaboration between various care providers with the same or different specialty, is an important issue in health services research, because poor coordination has the potential to bring about inferior patient outcomes. The concern in (inpatient) rehabilitation ought to be higher, to the degree that the rehabilitation team has been the cornerstone of rehabilitation, and much ideological writing (and a little research) has addressed the issue of team functioning. Team size and its impact on care coordination to date have not been addressed systematically.
These data confirm what has been suggested by studies enumerating the membership of rehabilitation teams: the actual number of clinicians delivering care to a patient over his/her LOS is well in excess of the 6–10 implied by discussions of the make-up of the clinical team. A number as high as 48 is not unusual, and this still excludes students doing rotations, aides and assistants in NU, PT, and OT, as well as representatives from medicine, respiratory care, and other disciplines. Some use of multiple clinicians is unavoidable, especially given the relatively long stays of patients with SCI. Nursing, which has round-the-clock coverage, needs at least six persons with 12-hour shifts, nine with 8-hour shifts, and more to accommodate time-off. Specialization within disciplines may call for having more than one representative of a discipline treat the patient. This typically is the case where the IRF has ‘clinics’ (for seating, for woundcare, etc.) where patients get specialist care. In SCIRehab, POC documentation was completed by the clinicians staffing such clinics, just as they did for their own ‘caseload’ of patients. However, it would seem that the typical patient has to deal with an ever-changing parade of clinicians. These clinicians, in turn, are confronted by the challenge of communicating patient information to a very large team; likely, coordination suffers.
It would seem that how an SCI unit is organized has the potential to contribute to the diffusion of care responsibilities over therapists, and the nature and quality of communication between them. In almost all inpatient rehabilitation programs a patient is assigned to a particular therapist, and he or she is responsible for this patient until the patient is discharged. In instances of therapist illness, vacation or attendance at professional meetings – not uncommon events – care is delivered by a colleague, who may use medical record entries and ‘cover notes’ to become aware of the status and progress of patients. In most programs, the therapies that deliver the most care (in terms of minutes per day), PT and OT, all treat their patients in close proximity in a single gym, and all therapists get to know all patients to some degree, the same as all patients get to know all therapists. If therapist A has expertise that therapist B's patient needs, the two may arrange to co-treat, both to offer continuity to the patient and as an opportunity for therapist B to improve her skill set.
In a small unit, communication between therapists is also easier, with nurses and psychotherapists just a few yards from one another and other team members. Modern communications technology also plays a role; many units now use ‘communications badges’ for an instant wireless spoken connection to each team member. The key clinical and administrative leaders of the team (physician, nurse manager, and therapy manager) generally are available by pager when they are removed from the hospital grounds where the hands-free communication system is effective. Thus, a group of 15 or 20 persons, all of whom have one or more treatment sessions with a particular patient, still can be a ‘team’ provided there is extensive, intensive, and high-quality communication. The data available in the present study only reflected the numbers of individuals within and across disciplines that were involved with a particular patient, and did not reveal any aspect of their communication. A future study might investigate aspects of the communication between team members (frequency, quality, and topics) and whether good communication can overcome whatever disadvantage is posed by a large team size. Potential models for conceptualizing the ‘handoff’ situation and instruments for a detailed analysis of handoff exist.46,47 There is much research in family practice and other primary care to offer support for a link between continuity of care and patient satisfaction, presumably an outcome or indicator of the quality of the bond between clinician and patient.48,49 There also is evidence for a link with other outcomes, including emergency department use, hospitalizations, and improved receipt of preventive services.50
Studies of the development of a therapeutic relationship and how that development may be affected by aspects of the continuity of care (duration, density, dispersion, and sequence)51 appear to be rare, in all health care fields. In rehabilitation, there is one study showing that longitudinal continuity of care (in outpatient PT treatment) is linked to patient satisfaction.52 A small number of studies in (outpatient) rehabilitation have shown that the therapeutic alliance between therapist and patient has positive effects on outcomes such as pain and function.53
However, there is an extensive literature in psychotherapy and related fields showing that the therapeutic alliance between clinician and patient makes a modest but fairly consistent contribution to therapy outcomes, however those may be defined.54 While there are a number of conceptualizations of the therapeutic bond or alliance in psychotherapy research,54,55 most center on three components of the patient–therapist relationship that are postulated to be required for an effective therapeutic process: a collaborative relationship; an affective bond; and agreement on treatment goals and tasks. It is unclear to what degree the relationship between a rehabilitation therapist and a patient requires the same elements to be effective. The few rehabilitation studies that have been published on the link between the patient–therapist relationship and patient outcomes just adopted one of the existing instruments developed for psychotherapy (most often the Working Alliance Inventory) rather than investigating which one of the three main elements in the therapeutic alliance are necessary ingredients. However, it is reasonable to assume that in inpatient SCI rehabilitation an affective bond, collaboration between patient and therapist, and agreement on treatment goals and methods are important, and that continuity in the patient–clinician relationship allows these three to be increased to an optimal level. The discontinuity of care reported in this paper as characteristic of the care process for many SCI patients cannot but detract from the development of a productive therapeutic bond.
Future research should focus on the patient–therapist relationship and its three main components, and determine its importance in various disciplines. It is possible that a therapeutic alliance is of less importance in, for instance, PT than in psychology treatment. The data presented here indicate a much higher TCI for the latter (0.82 average for all treatment sessions; 0.95 for individual sessions) than for the former (0.45 and 0.53, respectively). (Table 5) Because traditionally in SCI rehabilitation the emphasis has been on physical restoration rather than psychological adjustment, and because Medicare counts PT and OT hours but not PS ones toward its 3-hour rule, the typical treatment program has 3–4 times as many PTs as psychologists. As a consequence, there is more opportunity to have a colleague cover when the treating therapist is absent. But it is also likely that the high TCI values for psychology (and SW) are the result of a need for a much stronger alliance in order for treatment to be effective.
This analysis presented data on the presumed reflection of or effect of such a therapeutic bond, the therapist's rating of patient participation in the treatment session. There is no claim that the Participation Scale is a replacement for one of the many instruments that have been developed for measuring the working alliance in psychotherapy;54,55 more likely, it reflects the outcome of such a relationship as it affects the implementation of the treatment session in question. Other analyses of SCIRehab data indicate that participation of the patient in treatment sessions is a strong predictor of rehabilitation outcomes, whether at discharge from inpatient rehabilitation or after a number of months living in the community, whether the ratings are mode by Nursing,56 OT,57 PT,58 or TR.59
Limitations
Only a very small percentage of the variance in participation ratings was explained by continuity of care; however, it should be noted that some of the other predictors used, especially the typical ratings patients receive, and potentially typical ratings therapists give out, already reflect to some degree strength of the therapeutic alliance, thus leaving limited room for a pure continuity index to explain additional variance. As suggested above, good communication within the rehabilitation team may counter the presumed negative effect of a large team on lack of familiarity of patients with therapists and vice versa. This may be an additional reason for the small percentage of the variance in Participation scores explained by TCI.
Another limitation of this study is the omission of the treatment sessions a minority of patients may have had during their admission to a non-SCI unit of the participating SCIRehab facilities; counting the sessions they had on those units would have decreased their TCI, most likely. On the other hand, included in the TCI were some sessions where there was no patient–therapist interaction, but the therapist dealt with other team members, the patient's family or outside agencies on the patient's behalf. While such sessions are not likely to contribute to the growth of the therapeutic alliance, to the degree that continuity of care is important in optimal communication of the patient's strengths and needs, inclusion of these sessions is justifiable. Other limitations are the narrow assessment of participation (a one-item scale, completed by the therapist only), and the absence of information on some members of the rehabilitation team (technicians and assistants in nursing and other disciplines, physicians, respiratory therapists, etc.). Missing documentation may also have an impact, although there is no information on its frequency, or whether primary or secondary clinicians were more likely to fail to complete a POC report.
Conclusion
In SCI rehabilitation, teams are at least as large as suggested by previous research. The large size of the rehabilitation team should be reason for concern about continuity of care, unless it can be shown that formal and informal mechanisms of communication between staff members are available that counteract the problems inherent in conveying information on a patient's status, progress, and needs to a team numbering in the dozens. Treatment of a single patient by dozens of clinicians may not mean lack of familiarity of patient and therapist with one another; alternatively, the possibly weak therapeutic alliance does not affect the patients' active participation in their sessions. The nature and impact of the therapeutic relationships SCI rehabilitation inpatients may develop with their nurses and therapists deserve further study.
Acknowledgements
Thanks are due to the participating clinicians and researchers at Craig Hospital (Denver, CO, USA), Shepherd Center (Atlanta, GA, USA), Rehabilitation Institute of Chicago (Chicago, IL, USA), Carolinas Rehabilitation (Charlotte, NC, USA), the Mount Sinai Medical Center (New York, NY, USA), and National Rehabilitation Hospital (Washington, DC, USA), as well as researchers at the Institute for Clinical Outcomes Research (Salt Lake City, UT, USA). This research was funded by grants from the National Institute on Disability and Rehabilitation Research (NIDRR), Office of Special Education and Rehabilitative Services, U.S. Department of Education, numbers H133A060103 to Craig Hospital and H133N060027 to Mount Sinai School of Medicine.
References
- 1.Eldar R, Marincek C, Kullmann L. Need for rehabilitation teamwork training in Europe. Croat Med J 2008;49(3):352–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strasser DC, Falconer JA, Herrin JS, Bowen SE, Stevens AB, Uomoto J. Team functioning and patient outcomes in stroke rehabilitation. Arch Phys Med Rehabil 2005;86(3):403–9 [DOI] [PubMed] [Google Scholar]
- 3.Strasser DC, Uomoto JM, Smits SJ. The interdisciplinary team and polytrauma rehabilitation: prescription for partnership. Arch Phys Med Rehabil 2008;89(1):179–81 [DOI] [PubMed] [Google Scholar]
- 4.Keith RA. The comprehensive treatment team in rehabilitation. Arch Phys Med Rehabil 1991;72(5):269–74 [PubMed] [Google Scholar]
- 5.Bakheit AM. Effective teamwork in rehabilitation. Int J Rehabil Res 1996;19(4):301–6 [DOI] [PubMed] [Google Scholar]
- 6.Stevens AB, Strasser DC, Uomoto J, Bowen SE, Falconer JA. Utility of treatment implementation methods in clinical trial with rehabilitation teams. J Rehabil Res Dev 2007;44(4):537–46 [DOI] [PubMed] [Google Scholar]
- 7.Kane RL. Assessing the effectiveness of postacute care rehabilitation. Arch Phys Med Rehabil 2007;88(11):1500–4 [DOI] [PubMed] [Google Scholar]
- 8.Sinclair LB, Lingard LA, Mohabeer RN. What's so great about rehabilitation teams? An ethnographic study of interprofessional collaboration in a rehabilitation unit. Arch Phys Med Rehabil 2009;90(7):1196–201 [DOI] [PubMed] [Google Scholar]
- 9.Vyt A. Interprofessional and transdisciplinary teamwork in health care. Diabetes Metab Res Rev 2008;24(Suppl. 1):S106–9 [DOI] [PubMed] [Google Scholar]
- 10.Suddick KM, De Souza L. Therapists' experiences and perceptions of teamwork in neurological rehabilitation: Reasoning behind the team approach, structure and composition of the team and teamworking processes. Physiother Res Int 2006;11(2):72–83 [DOI] [PubMed] [Google Scholar]
- 11.Mullins LL, Balderson BHK, Chaney JM. Implementing team approaches in primary and tertiary care settings: Applications from the rehabilitation context. Fam Syst Health 1999;17(4):413–26 [Google Scholar]
- 12.Petersson IF. Evolution of team care and evaluation of effectiveness. Curr Opin Rheumatol 2005;17(2):160–3 [DOI] [PubMed] [Google Scholar]
- 13.Neumann V, Gutenbrunner C, Fialka-Moser V, Christodoulou N, Varela E, Giustini A, et al Interdisciplinary team working in physical and rehabilitation medicine. J Rehabil Med 2010;42(1):4–8 [DOI] [PubMed] [Google Scholar]
- 14.Nair KP, Wade DT. Satisfaction of members of interdisciplinary rehabilitation teams with goal planning meetings. Arch Phys Med Rehabil 2003;84(11):1710–3 [DOI] [PubMed] [Google Scholar]
- 15.Norrefalk JR. How do we define multidisciplinary rehabilitation? J Rehabil Med 2003;35(2):100–1 [DOI] [PubMed] [Google Scholar]
- 16.Long AF, Kneafsey R, Ryan J. Rehabilitation practice: challenges to effective team working. Int J Nurs Stud 2003;40(6):663–73 [DOI] [PubMed] [Google Scholar]
- 17.Jelles F, van Bennekom CA, Lankhorst GJ. The interdisciplinary team conference in rehabilitation medicine. Am J Phys Med Rehabil 1995;74(6):464–5 [DOI] [PubMed] [Google Scholar]
- 18.Korner M. Analysis and development of multiprofessional teams in medical rehabilitation. Psychosoc Med. 2008;v.5:pDoc01. [PMC free article] [PubMed] [Google Scholar]
- 19.Korner M, Bengel J. Teamwork and team success in multi- and interdisciplinary teams in medical rehabilitation. Rehabilitation (Stuttg) 2004;43(6):348–57 [DOI] [PubMed] [Google Scholar]
- 20.Alexander JA, Lichtenstein R, Jinnett K, Wells R, Zazzali J, Liu D. Cross-functional team processes and patient functional improvement. Health Serv Res 2005;40(5 Pt 1):1335–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mullins LL, Balderson BHK, Sanders N, Chaney JM, Whatley PR. Therapists' perceptions of team functioning in rehabilitation contexts. Int J Rehabil Health 1997;3(4):281–8 [Google Scholar]
- 22.Korner M. Interprofessional teamwork in medical rehabilitation: a comparison of multidisciplinary and interdisciplinary team approach. Clin Rehabil 2010;24:745–55 [DOI] [PubMed] [Google Scholar]
- 23.Cott C. Structure and meaning in multidisciplinary teamwork. Sociol Health Illn 1998;20(6):848–73 [Google Scholar]
- 24.Nijhuis BJ, Reinders-Messelink HA, de Blecourt AC, Olijve WG, Groothoff JW, Nakken H, et al A review of salient elements defining team collaboration in paediatric rehabilitation. Clin Rehabil 2007;21(3):195–211 [DOI] [PubMed] [Google Scholar]
- 25.Strasser DC, Smits SJ, Falconer JA, Herrin JS, Bowen SE. The influence of hospital culture on rehabilitation team functioning in VA hospitals. J Rehabil Res Dev 2002;39(1):115–25 [PubMed] [Google Scholar]
- 26.Strasser DC, Falconer JA, Martino-Saltzmann D. The rehabilitation team: staff perceptions of the hospital environment, the interdisciplinary team environment, and interprofessional relations. Arch Phys Med Rehabil 1994;75(2):177–82 [PubMed] [Google Scholar]
- 27.Strasser DC, Falconer JA, Stevens AB, Uomoto JM, Herrin J, Bowen SE, et al Team training and stroke rehabilitation outcomes: a cluster randomized trial. Arch Phys Med Rehabil 2008;89(1):10–5 [DOI] [PubMed] [Google Scholar]
- 28.Halstead LS. Team care in chronic illness: a critical review of the literature of the past 25 years. Arch Phys Med Rehabil 1976;57(11):507–11 [PubMed] [Google Scholar]
- 29.Cobble NBJ. Introduction to principles of rehabilitation. J Neurol Rehabil 1990;4(4):181–5 [Google Scholar]
- 30.Smits SJ, Falconer JA, Herrin J, Bowen SE, Strasser DC. Patient-focused rehabilitation team cohesiveness in veterans administration hospitals. Arch Phys Med Rehabil 2003;84(9):1332–8 [DOI] [PubMed] [Google Scholar]
- 31.Baxter SK, Brumfitt SM. Once a week is not enough: evaluating current measures of teamworking in stroke. J Eval Clin Pract 2008;14(2):241–7 [DOI] [PubMed] [Google Scholar]
- 32.Whiteneck G, Gassaway J, Dijkers M, Jha A. New approach to study the contents and outcomes of spinal cord injury rehabilitation: the SCIRehab project. J Spinal Cord Med 2009;32(3):251–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whiteneck G, Dijkers M, Gassaway J, Lammertse DP. The SCIRehab project: classification and quantification of spinal cord injury rehabilitation treatments. Preface . J Spinal Cord Med 2009;32(3):249–50 [PMC free article] [PubMed] [Google Scholar]
- 34.Lammertse DP, Jackson AB, Sipski ML. Research from the model spinal cord injury systems: findings from the current 5-year grant cycle. Arch Phys Med Rehabil 2004;85(11):1737–9 [DOI] [PubMed] [Google Scholar]
- 35.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011;34(6):535–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Granger CV, Hamilton BB, Keith RA, Zielesny M, Sherwin FS. Advances in functional assessment for medical rehabilitation. Top Geriatr Rehabil 1986;1:59–74 [Google Scholar]
- 37.Gassaway J, Whiteneck G, Dijkers M. Clinical taxonomy development and application in spinal cord injury rehabilitation research: the SCIRehab project. J Spinal Cord Med 2009;32(3):260–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abeyta N, Freeman ES, Primack D, Hammond M, Dragon C, Harmon A, et al. SCIRehab project series: the social work/case management taxonomy. J Spinal Cord Med 2009;32(3):336–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cahow C, Skolnick S, Joyce J, Jug J, Dragon C, Gassaway J. SCIRehab project series: the therapeutic recreation taxonomy. J Spinal Cord Med 2009;32(3):298–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gordan W, Spivak-David D, Adornato V, Dale B, Brougham R, Georgeadis AC, et al. SCIRehab project series: the speech language pathology taxonomy. J Spinal Cord Med 2009;32(3):307–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johnson K, Bailey J, Rundquist J, Dimond P, McDonald CA, Reyes IA, et al. SCIRehab project series: the supplemental nursing taxonomy. J Spinal Cord Med 2009;32(3):329–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Natale A, Taylor S, LaBarbera J, Bensimon L, McDowell S, Mumma SL, et al. SCIRehab project series: the physical therapy taxonomy. J Spinal Cord Med 2009;32(3):270–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ozelie R, Sipple C, Foy T, Cantoni K, Kellogg K, Lookingbill J, et al. SCIRehab project series: the occupational therapy taxonomy. J Spinal Cord Med 2009;32(3):283–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson C, Huston T, Koval J, Gordon SA, Schwebel A, Gassaway J. SCIRehab project series: the psychology taxonomy. J Spinal Cord Med 2009;32(3):319–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lenze EJ, Munin MC, Quear T, Dew MA, Rogers JC, Begley AE, et al The Pittsburgh Rehabilitation Participation Scale: reliability and validity of a clinician-rated measure of participation in acute rehabilitation. Arch Phys Med Rehabil 2004;85(3):380–4 [DOI] [PubMed] [Google Scholar]
- 46.Apker J, Mallak LA, Applegate EB, III, Gibson SC, Ham JJ, Johnson NA, et al Exploring emergency physician-hospitalist handoff interactions: development of the handoff communication assessment. Ann Emerg Med 2010;55(2):161–70 [DOI] [PubMed] [Google Scholar]
- 47.Riesenberg LA, Leisch J, Cunningham JM. Nursing handoffs: a systematic review of the literature. Am J Nurs 2010;110(4):24–34 [DOI] [PubMed] [Google Scholar]
- 48.Adler R, Vasiliadis A, Bickell N. The relationship between continuity and patient satisfaction: a systematic review. Fam Pract 2010;27(2):171–8 [DOI] [PubMed] [Google Scholar]
- 49.Schers H, van den Hoogen H, Bor H, Grol R, van den Bosch W. Familiarity with a GP and patients' evaluations of care. A cross-sectional study. Fam Pract 2005;22(1):15–9 [DOI] [PubMed] [Google Scholar]
- 50.Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract 2004;53(12):974–80 [PubMed] [Google Scholar]
- 51.Jee SH, Cabana MD. Indices for continuity of care: a systematic review of the literature. Med Care Res Rev 2006;63(2):158–88 [DOI] [PubMed] [Google Scholar]
- 52.Beattie P, Dowda M, Turner C, Michener L, Nelson R. Longitudinal continuity of care is associated with high patient satisfaction with physical therapy. Phys Ther 2005;85(10):1046–52 [PubMed] [Google Scholar]
- 53.Hall AM, Ferreira PH, Maher CG, Latimer J, Ferreira ML. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther 2010;90(8):1099–110 [DOI] [PubMed] [Google Scholar]
- 54.Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. J Consult Clin Psychol 2000;68(3):438–50 [PubMed] [Google Scholar]
- 55.Elvins R, Green J. The conceptualization and measurement of therapeutic alliance: an empirical review. Clin Psychol Rev 2008;28(7):1167–87 [DOI] [PubMed] [Google Scholar]
- 56.Bailey J, Dijkers MP, Thomas J, Lingefelt P, Kreider SED, Whiteneck G. Relationship of nursing education and care management inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med 2012;35(6):593–610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ozelie R, Gassaway J, Buchman E, Thimmaiah D, Heisler L, Cantoni K, et al. Relationship of occupational therapy inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCI Rehab Project. J Spinal Cord Med 2012;35(6):527–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Teeter L, Gassaway J, Taylor S, LaBarbera J, McDowell S, Backus B, et al. Relationship of physical therapy inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCI Rehab Project. J Spinal Cord Med 2012;35(6):503–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cahow C, Rider C, Bogenshutz A, Joyce J, Edens K, Kreider SED, et al. Relationship of therapeutic recreation inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med 2012;35(6):547–64 [DOI] [PMC free article] [PubMed] [Google Scholar]


