Abstract
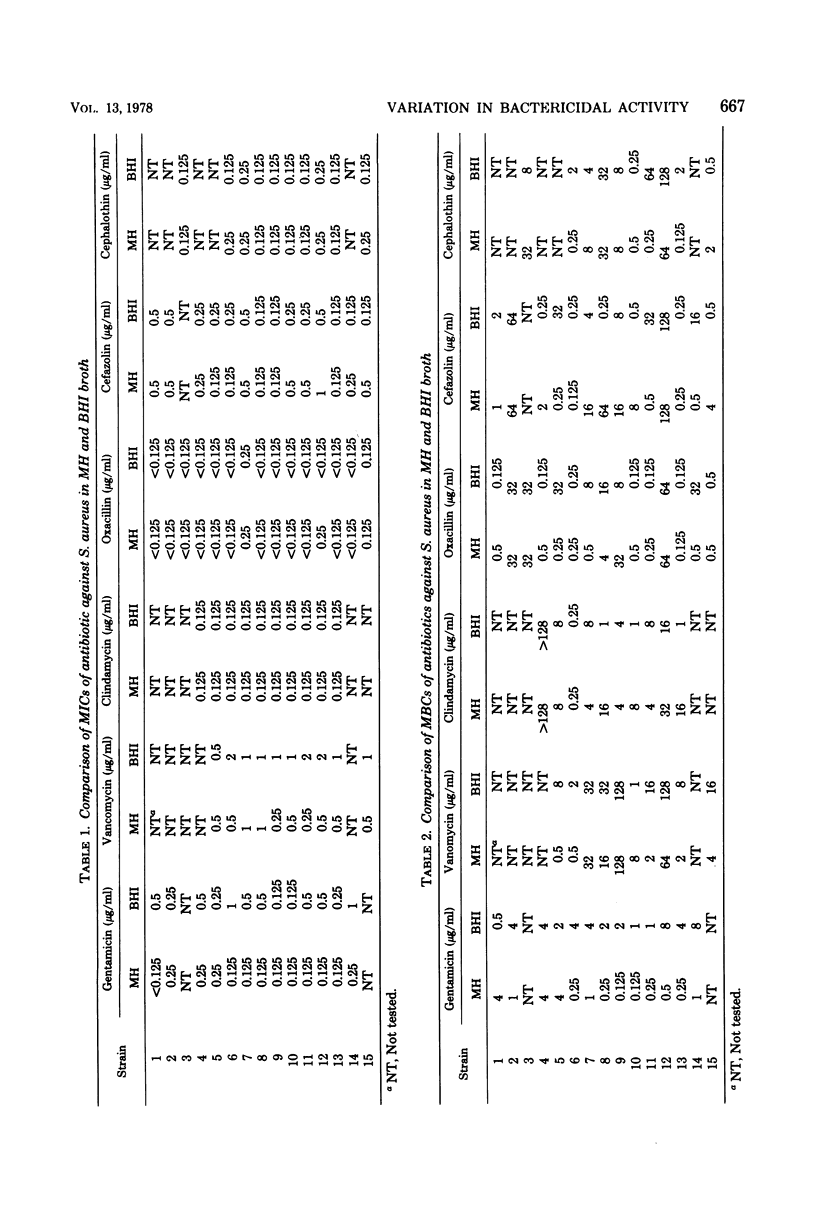
Staphylococcus aureus resistant to bactericidal activity of antibiotics caused sepsis in three patients. Bacteriological and clinical responses were not achieved until serum and tissue fluid levels of administered antibiotics exceeded the minimum bactericidal concentration (MBC) of the infecting organism. Fifteen clinical isolates of S. aureus were tested in brain heart infusion broth and Mueller-Hinton broth for the MBC of gentamicin, vancomycin, clindamycin, oxacillin, cefazolin, and cephalothin. Results showed significant eightfold or greater broth-dependent differences in the MBC of at least one antibiotic against 87% (13/15) of strains tested. The MBC was unpredictable and varied with the strain, antibiotic, and medium used. No controlled studies are available to indicate the clinical significance of the MBC demonstrated in different media. The necessity for treating serious infection with bactericidal drugs has not yet been established; however, in septicemia such as that caused by bacterial endocarditis, bacteriostatic antibiotics have generally failed to eradicate the infection, whereas bactericidal agents have often been curative. Therefore, in patients unresponsive to usual antistaphylococcal therapy, we suggest that MBC testing be performed in at least two media and that treatment be instituted with antibiotics demonstrating the lowest MBC in all media used.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brenner V. C., Sherris J. C. Influence of different media and bloods on results of diffusion antibiotic susceptibility tests. Antimicrob Agents Chemother. 1972 Feb;1(2):116–122. doi: 10.1128/aac.1.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUNLOP S. G. THE SERUM-DILUTION BACTERICIDAL TEST FOR ANTIBIOTIC EFFECTIVENESS. Am J Med Technol. 1965 Jan-Feb;31:69–76. [PubMed] [Google Scholar]
- Fong I. W., Engelking E. R., Kirby W. M. Relative inactivation by Staphylococcus aureus of eight cephalosporin antibiotics. Antimicrob Agents Chemother. 1976 Jun;9(6):939–944. doi: 10.1128/aac.9.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GARROD L. P., WATERWORTH P. M. Methods of testing combined antibiotic bactericidal action and the significance of the results. J Clin Pathol. 1962 Jul;15:328–338. doi: 10.1136/jcp.15.4.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GERACI J. E. Further experiences with short-term (2 weeks) combined penicillinstreptomycin therapy for bacterial endocarditis caused by penicillin-sensitive streptococci. Proc Staff Meet Mayo Clin. 1955 May 4;30(9):192–200. [PubMed] [Google Scholar]
- GERACI J. E., MARTIN W. J. Antibiotic therapy of bacterial endocarditis. VI. Subacute enterococcal endocarditis; clinical, pathologic and therapeutic consideration of 33 cases. Circulation. 1954 Aug;10(2):173–194. doi: 10.1161/01.cir.10.2.173. [DOI] [PubMed] [Google Scholar]
- GERACI J. E. The antibiotic therapy of bacterial endocarditis: therapeutic data on 172 patients seen from 1951 through 1957: additional observations on short-term therapy (two weeks) for penicillin-sensitivie streptococcal endocarditis. Med Clin North Am. 1958 Jul;42(4):1101–1140. doi: 10.1016/s0025-7125(16)34262-6. [DOI] [PubMed] [Google Scholar]
- Gopal V., Bisno A. L., Silverblatt F. J. Failure of vancomycin treatment in Staphylococcus aureus endocarditis. In vivo and in vitro observations. JAMA. 1976 Oct 4;236(14):1604–1606. [PubMed] [Google Scholar]
- JAWETZ E., BRAINERD H. D. Staphylococcal endocarditis. Results of combined antibiotic therapy in fourteen consecutive cases (1956-1959). Am J Med. 1962 Jan;32:17–24. doi: 10.1016/0002-9343(62)90178-x. [DOI] [PubMed] [Google Scholar]
- JAWETZ E. Combined antibiotic therapy in serious infections caused by drug-resistant staphylococci (1956-1957). AMA Arch Intern Med. 1959 Feb;103(2):289–307. doi: 10.1001/archinte.1959.00270020117014. [DOI] [PubMed] [Google Scholar]
- JAWETZ E., GUNNISON J. B., COLEMAN V. R., KEMPE H. C. A laboratory test for bacterial sensitivity to combinations of antibiotics. Am J Clin Pathol. 1955 Sep;25(9):1016–1031. doi: 10.1093/ajcp/25.9.1016. [DOI] [PubMed] [Google Scholar]
- JAWETZ E. The "tough case" of bacterial endocarditis. Circulation. 1959 Sep;20:430–437. doi: 10.1161/01.cir.20.3.430. [DOI] [PubMed] [Google Scholar]
- Klastersky J., Daneau D., Swings G., Weerts D. Antibacterial activity in serum and urine as a therapeutic guide in bacterial infections. J Infect Dis. 1974 Feb;129(2):187–193. doi: 10.1093/infdis/129.2.187. [DOI] [PubMed] [Google Scholar]
- Marcoux J. A., Washington J. A., 2nd Pitfalls in identification of methicillin-resistant Staphylococcus aureus. Appl Microbiol. 1969 Oct;18(4):699–700. doi: 10.1128/am.18.4.699-700.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayhall C. G., Medoff G., Marr J. J. Variation in the susceptibility of strains of Staphylococcus aureus to oxacillin, cephalothin, and gentamicin. Antimicrob Agents Chemother. 1976 Oct;10(4):707–712. doi: 10.1128/aac.10.4.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pursiano T. A., Misiek M., Leitner F., Price K. E. Effect of assay medium on the antibacterial activity of certain penicillins and cephalosporins. Antimicrob Agents Chemother. 1973 Jan;3(1):33–39. doi: 10.1128/aac.3.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan K. J., Sherris J. C. Antimicrobial susceptibility testing. Hum Pathol. 1976 May;7(3):277–286. doi: 10.1016/s0046-8177(76)80038-x. [DOI] [PubMed] [Google Scholar]
- Sabath L. D., Wheeler N., Laverdiere M., Blazevic D., Wilkinson B. J. A new type of penicillin resistance of Staphylococcus aureus. Lancet. 1977 Feb 26;1(8009):443–447. doi: 10.1016/s0140-6736(77)91941-9. [DOI] [PubMed] [Google Scholar]
- TUMULTY P. A. The management of bacterial endocarditis. Arch Intern Med. 1960 Jan;105:126–142. doi: 10.1001/archinte.1960.00270130142019. [DOI] [PubMed] [Google Scholar]
- Washington J. A., 2nd, Hermans P. E., Martin W. J. In vitro susceptibility of staphylococci and streptococci and influence of agar media on minimum inhibitory concentration. Mayo Clin Proc. 1970 Jul;45(7):527–535. [PubMed] [Google Scholar]



