Abstract
This study examines the association between maternal health service utilization and household decision-making in Bangladesh. Most studies of the predictors of reproductive health service use focus on women’s reports; however, men are often involved in these decisions as well. Recently, studies have started to explore the association between health outcomes and reports of household decision-making from both husbands and wives as matched pairs. Many studies of household decision-making emphasize the importance of the wife alone making decisions; however, some have argued that joint decision-making between husbands and wives may yield better reproductive health outcomes than women making decisions without input or agreement from their partners. Husbands’ involvement in decision-making is particularly important in Bangladesh because men often dominate household decisions related to large, health-related purchases. We use matched husband and wife reports about who makes common household decisions to predict use of antenatal and skilled delivery care, using data from the 2007 Bangladesh Demographic and Health Survey. Results from regression analyses suggest that it is important to consider whether husbands and wives give concordant responses about who makes household decisions since discordant reports about who makes these decisions are negatively associated with reproductive health care use. In addition, compared to joint decision-making, husband-only decision-making is negatively associated with antenatal care use and skilled delivery care. Finally, associations between household decision-making arrangements and health service utilization vary depending on whose report is used and the type of health service utilized.
Keywords: Bangladesh, decision-making, husbands/wives, health service utilization, maternal health
INTRODUCTION
The study of reproductive health, including health care utilization, has been primarily individualistic in nature, with a focus on women (Becker, 1996). However, decisions about reproductive health care utilization are not made independent of one’s social context, and are often strongly influenced by spousal relationships (Allendorf, 2010). Although women’s reports often dominate analyses of reproductive health care utilization, an increasing number of “couples studies” examine responses from both husbands and wives as matched pairs. These studies make unique contributions because they reveal discrepancies between men’s and women’s reports of reproductive health attitudes and behaviors. The majority of these studies focus on fertility, family planning, or sexual behavior as the outcome of interest (Bankole & Singh, 1998; Becker, 1999; Gipson & Hindin, 2008; Kulczycki, 2008; McDougall, 2011; Miller et al., 2001; Mullany, 2010).
Recently, couples studies have started to explore the association between health outcomes and couples’ reports of household decision-making (Allendorf, 2007; Becker et al., 2006; Ghuman et al., 2006; Jejeebhoy, 2002). These studies frame their analyses of decision-making as an examination of women’s relative power (Becker et al., 2006) or women’s autonomy (Allendorf, 2007; Ghuman et al., 2006; Jejeebhoy, 2002). It has been suggested that the autonomy paradigm is not adequate for understanding women’s reproductive health in the South Asian context because of the importance of inter-dependence within families (Mumtaz & Salway, 2009). Specifically, women’s independence and autonomy, with respect to health-related decision-making, may be restricted in a society where women are embedded in social relationships and have strong cultural and structural ties to men. Furuta and Salway (2006) argue that focusing on a woman’s independence from her husband and family is inappropriate in South Asia and greater attention should be placed on household decision-making processes that involve multiple people.
Autonomy is not always defined as women’s “full” control over decision-making. In the context of credit programs in rural Bangladesh, Kabeer (2001) suggests that greater equality in a woman’s contribution to household decisions with her spouse has the potential to lead to more positive outcomes compared to independent decision-making. On the other hand, “joint” control over loans has been described as a disguise for male dominance (Montgomery et al., 1996) and insufficient for improving women’s position (Goetz & Sen Gupta, 1996). Others have suggested that couples’ joint decision-making may yield better reproductive health outcomes (Mullany et al., 2005) compared to men making decisions alone or women making decisions without input or agreement from their partners. This could arise because joint decision-making is associated with greater male involvement in health behaviors (Mullany et al., 2005) or because joint decision-making allows the husband and wife to share the responsibility of the decision, especially in cases where there are negative consequences (Carter, 2002). Very few studies explore the ways in which different patterns of household decision-making predict health service utilization (Allendorf, 2007; Becker et al., 2006).
Understanding the decision-making process as a negotiation between husbands and wives is particularly important in Bangladesh. The husband is often involved in decisions about his wife’s health care, especially when it requires her to leave the home. This is ostensibly due to women’s limited mobility and limited educational and economic opportunities in Bangladesh (Paul & Rumsey, 2002; Rozario, 1998). Women’s limited mobility likely arises from the Muslim institution of parda (or purdah), which creates a strict separation between men and women. Since most doctors in Bangladesh are male, women often need their husband’s permission before seeking care. Women’s limited educational and economic opportunities give men more authority in the household, which leads to male involvement in women’s health care needs. These social barriers may, in part, be responsible for the low rates of maternal health service utilization. Currently, only 27% of all births in Bangladesh are assisted by skilled professionals and only 23% of births take place in a health facility. In addition, only 54% of women received at least one antenatal care visit from a medically trained provider and only 23% received four or more antenatal care visits (Bangladesh Maternal Morality and Health Care Survey, 2010). Improvements in the use of adequate antenatal care and professional delivery care have the potential to reduce the high rates of maternal and neonatal mortality in Bangladesh (Campbell & Graham, 2006; Moss et al., 2002); therefore, it is critical to better understand the kinds of relationships that may encourage or inhibit use.
The current literature on antenatal care and delivery care in Bangladesh focuses on socioeconomic, demographic, and geographical barriers to service utilization (Collin et al., 2007). Studies that address interpersonal factors related to maternal health service utilization, such as decision-making and husband’s involvement, tend to focus on specific, non-representative subpopulations (Amin et al., 2010; Choudhury & Ahmed, 2011). Using a nationally representative sample from Bangladesh, this study will make two primary contributions to the existing literature. The first contribution is methodological: we propose a new way to operationalize household decision-making information from surveys that interview both husbands and wives by examining concordant responses (wife and husband agree that the wife alone makes the decision, the husband alone makes the decision, the couple makes the decision together, or someone else is involved in the decision) and discordant responses (wife and husband do not agree about who makes the decision) to each household decision-making question. The second contribution is substantive: using this detailed measure, we describe the association between different household decision-making arrangements and maternal health service utilization from the couple’s perspective.
BACKGROUND
The observed association between couples’ decision-making and reproductive health outcomes may vary for a number of methodological reasons, including the way in which decision-making is measured, the type of respondent (i.e., wife, husband, or both), and the outcome of interest (e.g., utilization of antenatal care or contraceptive use). Four previous studies have examined the association between decision-making and health outcomes along these three dimensions (Allendorf, 2007; Becker et al., 2006; Ghuman et al., 2006; Jejeebhoy, 2002). However, no study has comprehensively examined the predictive power of different types of household decision-making arrangements—using both concordant and discordant responses for each household decision-making item—on maternal health care utilization.
Decision-making is typically measured by using a summative index, which incorporates a variety of decision-making variables. The past studies that examined the association between couples’ decision-making and health outcomes each used different measures of decision-making to create such indices. Two of the four studies measured decision-making by using questions related to the “final say” on specific household decisions (Allendorf, 2007; Becker et al., 2006). Each study created a spouse-specific summary score based on men’s and women’s responses. Ghuman and colleagues (2006) measured autonomy using a set of 11 decision-making questions related to freedom of movement, child care, and household tasks. Lastly, Jejeebhoy (2002) measured three aspects of autonomy using indices for each construct: mobility, access to economic resources, and economic decision-making.
In the final regression models used to predict health outcomes, two of the studies placed a greater value on the wife alone making a decision (Ghuman et al., 2006; Jejeebhoy, 2002), and the other two studies assessed decision-making by the wife alone or together with her husband (Allendorf, 2007; Becker et al., 2006). Each of these prior studies examined the concordance and discordance of wives’ and husbands’ reports about who made each type of decision. Although a large and significant proportion of couples disagreed about who made each of the studied decisions (between 10% and 53% in all four studies), only two of the studies included information about the level of discordance in the final regression models of the association between decision-making and health outcomes (Allendorf, 2007; Ghuman et al., 2006).
Furthermore, all four prior studies reported the estimated association with health outcomes based on women’s and men’s reports about decision-making. Couples’ reports were also included in the final regression models to predict health outcomes in different ways, such as interacting couples’ responses (Allendorf, 2007), combining wives’ and husbands’ responses in a summative score (Becker et al., 2006), and using an item response model to compare women’s and men’s responses (Ghuman et al., 2004). However, no prior study compared the variation in the estimated association between decision-making and the use of health services for each decision-making item and each decision-making arrangement according to wives’ reports, husbands’ reports, and couples’ reports. Lastly, only two of the four studies examined maternal health service utilization as the outcome of interest (Allendorf, 2007; Becker et al., 2006).
STUDY AIMS
This study will contribute to the existing literature on couples’ reports about decision-making and health service utilization by studying the cultural context of Bangladesh. We aim to examine (1) concordance and discordance in husbands’ and wives’ responses to questions about who makes particular decisions in the household, (2) the potential variability in our estimates of the association between decision-making arrangement and the use of maternal health services when we vary whose report is used (wives only, husbands only, or the couple), and (3) the association between decision-making arrangement and the use of maternal health services for two types of health services (antenatal care and delivery care).
METHODS
Data Source and Sampling Strategy
This study involved the secondary analysis of publically available, de-identified data from the 2007 Bangladesh Demographic and Health Survey (BDHS) (NIPORT, 2009), as such, ethics approval was not required. The survey focused on women between the ages of 15 and 49 who had been or were currently married. A survey of men was conducted among a sub-sample of one of every two households selected for the women’s survey. All men between the ages of 15 and 54 and who had ever been married were eligible for the male survey.
A total of 10,996 women age 15–49 (98.4% response rate) and 3,771 men (92.6% response rate) were successfully interviewed. For the purpose of this study, the sample was limited to 3,336 married couples in which both partners were interviewed. Each member of the couple was interviewed at the same time, but separately, so their responses could not influence each other. We created an analytic sample of 1,649 couples with a child under five years old, as only these respondents were asked questions about the use of antenatal and delivery care. Further omitting those couples with item missing data yielded a final analytic sample of 1,623 couples.
Outcome Variables
The binary outcome variables are based on the woman’s report and included (1) whether she received at least one antenatal care visit and (2) whether her last birth was assisted by a skilled health professional—such as a doctor, nurse, or midwife. The use of one visit as the threshold for antenatal care is appropriate because we are interested in assessing women’s access to antenatal care services in Bangladesh—a country where the coverage of such services is low. Additionally, this measure has been used by other studies of couples (Allendorf, 2007). The measure of skilled delivery care is based on the World Health Organization recommendation that deliveries be assisted by someone with midwifery skills, including doctors, nurses and midwives (WHO, 2005). These two indicators were selected because of their positive association with improved maternal and neonatal health outcomes (Campbell & Graham, 2006). They also represent two very different types of decisions: antenatal care use is a planned behavior that can occur multiple times during pregnancy, whereas, in Bangladesh, delivery by a skilled health professional is often an unplanned decision made at a crisis point, such as during a difficult labor (Parkhurst et al., 2006).
Predictor Variables
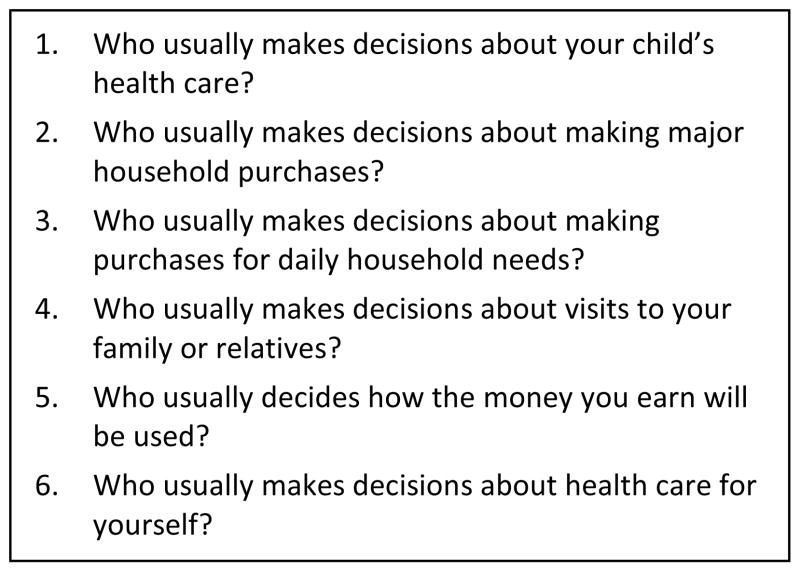
The primary predictor variables for this study are measures of household decision-making. The BDHS includes a total of six questions related to household decision-making (Figure 1). Most other couples studies used the decision-making questions to quantify a theoretical construct (e.g., women’s autonomy) that is not directly measurable. Instead we used these questions directly, to assess who makes decisions within the household. Only four of the items were used in our analysis. The fifth question inquires about the use of money the wife earns and only 18% of the women in our sample had any earnings. The sixth question asks about decisions about health care for “yourself,” which made it impossible to compare men’s and women’s responses because the object of inquiry differed.
Figure 1.
Household decision-making questions from the 2007 Bangladesh Demographic and Health Survey
The four remaining decision-making questions were used separately in our analysis in order to retain the ability to directly compare husbands’ and wives’ responses. Four categories were created for each question in which wives and husbands gave concordant responses: (1) Wife only made the decision, (2) Husband only, (3) Jointly, and (4) Other. The “Other” category combined two additional responses: “Someone else” and “You and someone else.” When analyzing couples data, each of these four categories represented concordant responses by the wife and husband. A fifth category—Disagree—was included in the analysis of couple data to represent wives’ and husbands’ discordant reports. We classified all discordant reports together, though they could be comprised of many different combinations of men’s and women’s reports about who made decisions. “Jointly” was used as the reference group in the regression models because it is associated with better reproductive health outcomes (Carter, 2002; Mullany et al., 2005) and it had an adequate number of observations for comparison purposes.
Predictor variables were selected based on their previously reported association with antenatal and delivery care in Bangladesh (Chakraborty et al., 2003). These variables were divided into three categories: previous use of health services, demographic characteristics, and socioeconomic characteristics. Previous use of health services refers to a woman’s experience with antenatal care, prior complication during childbirth, and experience in childbearing. Antenatal care is self-reported and was a binary variable coded as 1 if the wife reported attending at least one antenatal care check-up and 0 otherwise. Previous complications during pregnancy were assessed by asking the woman whether or not she had any miscarriages, abortions, stillbirths or menstrual regulations (any treatment administered within 14 days of a menstrual period to ensure that a woman either is not pregnant or does not remain pregnant) that ended before 2002. Previous complications were coded as 1 if the woman responded in the affirmative and 0 if not. Previous experience with childbirth is measured by the woman’s number of births. A high value is often placed on the first pregnancy and, in some settings, a woman’s family will help her to access the best care possible for the first birth. Additionally, women of higher parity may not feel the need to receive professional care if previous deliveries were uncomplicated (Gabrysch & Campbell, 2009). Parity is self-reported and divided into four distinct categories: first birth (omitted category), second birth, third birth, and fourth or higher order birth.
Demographic characteristics included wife’s age and place of residence. Age is self-reported and used as a continuous variable in this study. A quadratic term for age and age splines were both considered when specifying the model; however, neither transformation of age improved the model fit. Place of residence is measured by the cluster from which the household is selected (clusters were either all urban or all rural) and was coded as 1 for urban and 0 for rural. Socioeconomic characteristics included wife’s education, wife’s employment, and household wealth. Education is self-reported and divided into four distinct categories: no schooling, primary education, secondary education, and college or above. Employment is also self-reported and divided into three distinct categories: unemployed, employed without earnings, and employed with earnings. No schooling and unemployment were used as the reference categories in the regression models. Wealth is measured using the wealth index in the BDHS. This index used information on household ownership of consumer items and dwelling characteristics. Each asset was assigned a weight generated through principal components analysis. Each household was then assigned a score for each asset, and the scores were summed for each household. Couples were ranked according to the total wealth score of the household in which they resided. The wealth index was used as a continuous variable in the regression models.
We conducted several sensitivity analyses using men’s characteristics, including age, education and employment. When we added these covariates to our regression models (with and without women’s age, education level, and employment), there were no meaningful differences in our results. Therefore, we decided to use the age, education level, and employment for women only to avoid multicollinearity in our models.
Analytic Strategy
Descriptive statistics are presented for each outcome and predictor variable. Cross-tabulations and kappa-statistics show concordance and discordance between wives’ and husbands’ reports on each decision-making item. Bivariate analyses compared the association between decision-making arrangements and the use of maternal health services, varying the respondent from whom the report of decision-making was obtained (women, men, and couples). Multivariate logistic regression models were used to determine the association between decision-making arrangement and the use of antenatal care and skilled delivery care, controlling for other factors. Four models were estimated, one for each decision-making item. The criterion for statistical significance was p<0.05. Survey estimation procedures adjusted for the multi-stage sample design, including clustering of the primary sampling units. Men’s sampling weights were used since the male subpopulation was a sufficient approximation of the couples included in our study. All statistical analyses were conducted using Stata 11.1.
RESULTS
Fifty-eight percent of the women received at least one antenatal care visit and 17% had a doctor, nurse, or midwife assist with the delivery of their youngest child (Table 1). Twenty-eight percent of the women reported that their most recent delivery was their first birth and only 17% of women had a previous complication during pregnancy. Nearly 80% of the households in our sample were rural and the average age of the women was 25.9 years. Over one quarter (26%) of the women in our sample had no formal education and 68% were unemployed.
Table 1.
Summary statistics for couples in the 2007 Bangladesh Demographic and Health Survey
| n | % | |
|---|---|---|
| Outcome variables | ||
| Antenatal care | ||
| No visits | 640 | 42 |
| One or more visits | 983 | 58 |
| Assistance at delivery | ||
| Untrained attendant | 1,291 | 83 |
| Skilled professional | 332 | 17 |
| Previous use of health services | ||
| Previous complication | ||
| No previous complication | 1,326 | 83 |
| Previous complication | 297 | 17 |
| Parity | ||
| First birth | 460 | 28 |
| Second birth | 435 | 27 |
| Third birth | 298 | 19 |
| Four or higher order birth | 430 | 26 |
| Demographic characteristics | ||
| Wife’s age (Mean) | 1,623 | 25.85a |
| Place of residence | ||
| Rural | 1,037 | 79 |
| Urban | 586 | 21 |
| Socioeconomic characteristics | ||
| Wife’s Education | ||
| No Education | 414 | 26 |
| Primary | 533 | 33 |
| Secondary | 545 | 34 |
| Higher | 131 | 7 |
| Wife’s employment | ||
| Unemployed | 1161 | 68 |
| Employed without earnings | 63 | 6 |
| Employed with earnings | 399 | 26 |
| Wealth | ||
| Poorest | 320 | 23 |
| Poorer | 337 | 22 |
| Middle | 322 | 20 |
| Richer | 301 | 19 |
| Richest | 343 | 16 |
Std. dev. = 0.18
Notes: All variables are reported at the couple-level unless otherwise specified. All percentages are weighted to account for sampling design. There were 1,623 total observations.
Study Aim 1: Concordance and Discordance about Decision-Making
In order to better understand the patterns of concordance and discordance among couples, wives’ and husbands’ responses to each of the decision-making questions were cross-tabulated (Table 2). The highest level of concordance was related to decisions about major household purchases (50.2%) and the lowest was related to purchases for daily household needs (38.6%). Across all four decision-making questions, the most typical concordant response was that couples made the decision together (range: 16.0% to 30.9%). Concordant reports that the wife made the decision alone were generally the least frequent arrangement (range: 0.4% to 3.8%). Concordance between couples’ reports of decision-making was significantly greater than that predicted by chance alone, with all kappa statistics positive and significant at the 0.01 level.
Table 2.
Cross-tabulation of couples’ responses to all four decision-making questions, Bangladesh, 2007a
|
Who usually makes decisions about your child’s health care?
| |||||
|---|---|---|---|---|---|
| Wife’s response | Husband’s response
|
Total | |||
| Wife | Husband | Both jointly | Other | ||
| Wife | 3.8 | 1.5 | 7.2 | 0.3 | 12.8 |
| Husband | 4.4 | 4.8 | 13.9 | 1.5 | 24.6 |
| Both jointly | 10.5 | 8.7 | 30.9 | 2.3 | 52.4 |
| Other | 1.6 | 1.2 | 4.9 | 2.5 | 10.2 |
| Total | 20.3 | 16.2 | 56.9 | 6.6 | 100.0 |
|
| |||||
| Spousal agreement = 42.0% k=0.08** | |||||
|
Who usually makes decisions about making major household purchases?
| |||||
|---|---|---|---|---|---|
| Wife’s response | Husband’s response
|
Total | |||
| Wife | Husband | Both jointly | Other | ||
| Wife | 0.4 | 1.9 | 3.1 | 0.6 | 6.0 |
| Husband | 1.1 | 10.8 | 15.0 | 3.7 | 30.6 |
| Both jointly | 1.2 | 12.5 | 30.4 | 4.3 | 48.4 |
| Other | 0.1 | 2.9 | 3.4 | 8.6 | 15.0 |
| Total | 2.8 | 28.1 | 51.9 | 17.2 | 100.0 |
|
| |||||
| Spousal agreement = 50.2% k=0.22** | |||||
|
Who usually makes decisions about making purchases for daily household needs?
| |||||
|---|---|---|---|---|---|
| Wife’s response | Husband’s response
|
Total | |||
| Wife | Husband | Both jointly | Other | ||
| Wife | 3.5 | 9.4 | 11.5 | 1.6 | 26.0 |
| Husband | 2.4 | 11.2 | 10.0 | 1.9 | 25.5 |
| Both jointly | 3.2 | 12.6 | 16.0 | 1.8 | 33.6 |
| Other | 0.6 | 3.9 | 2.5 | 7.9 | 14.9 |
| Total | 9.7 | 37.1 | 40.0 | 13.2 | 100.0 |
|
| |||||
| Spousal agreement = 38.6% k=0.15** | |||||
|
Who usually makes decisions about visits to your family or relatives?
| |||||
|---|---|---|---|---|---|
| Wife’s response | Husband’s response
|
Total | |||
| Wife | Husband | Both jointly | Other | ||
| Wife | 0.6 | 2.0 | 4.9 | 0.3 | 7.8 |
| Husband | 1.6 | 10.1 | 16.3 | 3.6 | 31.6 |
| Both jointly | 1.1 | 13.1 | 30.1 | 2.9 | 47.2 |
| Other | 0.2 | 2.7 | 4.4 | 6.1 | 13.4 |
| Total | 3.5 | 27.9 | 55.7 | 12.9 | 100.0 |
|
| |||||
| Spousal agreement = 46.9% k=0.15** | |||||
All proportions are unweighted.
p<0.01
Nonetheless, there was substantial discordance in couples’ reports on each decision-making item. Although there were variations across the four decision-making items, there were some observable patterns. The marginal totals revealed that wives were more likely than husbands to report that the wife alone made decisions for three of the four decision-making items. For example, 26.0% of wives reported that they alone usually made decisions about daily household purchases, whereas only 9.7% of husbands reported that their wives alone made these decisions. Wives were also more likely than husbands to report that the husband alone made decisions for three of the four decision-making items. Lastly, husbands were more likely than wives to report that they made decisions together. For example, 55.7% of husbands reported that they made the decision to visit family together, whereas only 47.2% of wives reported that they made this decision jointly.
Study Aim 2: Decision-Making and the Type of Respondent
The bivariate analyses in Tables 3 and 4 show that the strength of the association between decision-making arrangement and maternal health care utilization depended on whose report was used. According to wives’ reports, compared to the odds of antenatal care use when spouses made household decisions together, the estimated odds of antenatal care use were lower when the husband alone made decisions (range: 0.51 to 0.63). The odds ratios were statistically significant for each of the four decision-making questions. According to husbands’ reports, compared to when spouses made decisions together, the estimated odds of antenatal care use were also lower when the husband alone made decisions (range: 0.60 to 0.93). The magnitude of the association was slightly weaker (closer to 1) when using women’s reports and the odds ratios were statistically significant for only two of the four decision-making questions. According to couples’ reports, the trend in the estimated odds of antenatal care use when the husband alone made decisions continues (range: 0.32 to 0.63). The magnitude of the association was slightly stronger than when using women’s reports and the odds ratios were statistically significant for three of the four decision-making questions. The same patterns were observed for skilled delivery care; however, fewer odds ratios were statistically significant (Table 4). In summary, using husbands’ reports alone yields associations that were significantly weaker than when using women’s reports or couples’ reports.
Table 3.
Bivariate logistic regression analysis of the association between decision-making arrangement and having at least one antenatal check-up by respondent.
| Variables | Wives | Husbands | Couples |
|---|---|---|---|
| Decision-making | |||
| Who decides about your child’s health care? | |||
| Jointly | 1.00 | 1.00 | 1.00 |
| Wife only | 0.80 | 1.31 | 0.89 |
| Husband only | 0.51** | 0.60** | 0.32** |
| Other | 0.96 | 1.21 | 1.14 |
| Disagree | -- | -- | 0.86 |
| Who decides about making major household purchases? | |||
| Jointly | 1.00 | 1.00 | 1.00 |
| Wife only | 0.68 | 1.22 | 0.71 |
| Husband only | 0.63** | 0.74* | 0.50** |
| Other | 1.27 | 1.17 | 1.08 |
| Disagree | -- | -- | 0.72* |
| Who decides about making daily household purchases? | |||
| Jointly | 1.00 | 1.00 | 1.00 |
| Wife only | 0.74* | 1.41 | 1.64 |
| Husband only | 0.61** | 0.93 | 0.63 |
| Other | 1.12 | 1.46 | 1.10 |
| Disagree | -- | -- | 0.68* |
| Who decides about visits to your family or relatives? | |||
| Jointly | 1.00 | 1.00 | 1.00 |
| Wife only | 0.83 | 1.21 | 1.57 |
| Husband only | 0.63** | 0.81 | 0.51** |
| Other | 0.96 | 1.12 | 1.24 |
| Disagree | -- | -- | 0.75* |
Notes: All data are presented as odds ratios.
p< 0.05.
p< 0.01.
-- Not applicable. There were 1,623 observations.
Table 4.
Bivariate logistic regression analysis of the association between decision-making arrangement and skilled delivery care by respondent.
| Variables | Wives | Husbands | Couples |
|---|---|---|---|
| Decision-making | |||
| Who decides about your child’s health care? | |||
| Jointly | 1.00 | 1.00 | 1.00 |
| Wife only | 0.87 | 1.23 | 1.23 |
| Husband only | 0.57** | 0.84 | 0.61 |
| Other | 0.97 | 1.23 | 1.33 |
| Disagree | -- | -- | 0.88 |
| Who decides about making major household purchases? | |||
| Jointly | 1.00 | 1.00 | 1.00 |
| Wife only | 0.78 | 0.47 | Omitted |
| Husband only | 0.63* | 0.84 | 0.59 |
| Other | 1.48 | 1.28 | 1.49 |
| Disagree | -- | -- | 0.65** |
| Who decides about making daily household purchases? | |||
| Jointly | 1.00 | 1.00 | 1.00 |
| Wife only | 0.76 | 1.34 | 1.16 |
| Husband only | 0.60* | 0.92 | 0.45* |
| Other | 1.22 | 1.90** | 1.34 |
| Disagree | -- | -- | 0.76 |
| Who decides about visits to your family or relatives? | |||
| Jointly | 1.00 | 1.00 | 1.00 |
| Wife only | 1.47 | 0.82 | 1.06 |
| Husband only | 0.52** | 0.83 | 0.58 |
| Other | 1.32 | 1.53* | 1.87* |
| Disagree | -- | -- | 0.75 |
Notes: All data are presented as odds ratios.
p < 0.05
p < 0.01.
-- = Not applicable. There were 1,623 observations.
Study Aim 3: Decision-Making and the Type of Maternal Health Service
Compared to joint decision-making, decision-making of any other type was associated with less antenatal care (Table 5), while the associations with skilled delivery care were less clear (Table 6). For example, compared to the odds of antenatal care use when spouses make household decisions together, the estimated odds of antenatal care use were smaller when the husband alone made decisions (range: 0.32 to 0.82), when someone else was involved in the decision (range: 0.45 to 0.59), and when couples give discordant reports about who made decisions (range: 0.65 to 0.84). Each of these odds ratios was statistically significant for at least two of the four decision-making questions. This pattern of association was similar for skilled delivery care; however, none of the odds ratios were statistically significant.
Table 5.
Multivariate logistic regression analysis of the association between decision-making arrangement and having at least one antenatal check-up controlling for confounders.
| Variables | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Decision-making | ||||
| Who decides about your child’s health care? | ||||
| Agree – Jointly | 1.00 | -- | -- | -- |
| Agree – Wife only | 0.81 | -- | -- | -- |
| Agree – Husband only | 0.32** | -- | -- | -- |
| Agree – Other | 0.53 | -- | -- | -- |
| Disagree | 0.84 | -- | -- | -- |
| Who decides about making major household purchases? | ||||
| Agree – Jointly | -- | 1.00 | -- | -- |
| Agree – Wife only | -- | 1.30 | -- | -- |
| Agree – Husband only | -- | 0.57* | -- | -- |
| Agree – Other | -- | 0.45** | -- | -- |
| Disagree | -- | 0.74 | -- | -- |
| Who decides about making daily household purchases? | ||||
| Agree – Jointly | -- | -- | 1.00 | -- |
| Agree – Wife only | -- | -- | 1.61 | -- |
| Agree – Husband only | -- | -- | 0.82 | -- |
| Agree – Other | -- | -- | 0.50* | -- |
| Disagree | -- | -- | 0.65* | -- |
| Who decides about visits to your family or relatives? | ||||
| Agree – Jointly | -- | -- | -- | 1.00 |
| Agree – Wife only | -- | -- | -- | 1.73 |
| Agree – Husband only | -- | -- | -- | 0.57* |
| Agree – Other | -- | -- | -- | 0.59 |
| Disagree | -- | -- | -- | 0.70* |
| Previous use of health services | ||||
| Previous complication | ||||
| No previous complication | 1.00 | 1.00 | 1.00 | 1.00 |
| Previous complication | 1.12 | 1.13 | 1.11 | 1.12 |
| Parity | ||||
| First birth | 1.00 | 1.00 | 1.00 | 1.00 |
| Second birth | 0.55** | 0.55** | 0.56** | 0.56** |
| Third birth | 0.50** | 0.51** | 0.50** | 0.50** |
| Fourth or higher order birth | 0.34** | 0.34** | 0.34** | 0.34** |
| Demographic characteristics | ||||
| Wife’s age | 1.019 | 1.014 | 1.016 | 1.016 |
| Place of residence | ||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 |
| Urban | 1.37 | 1.32 | 1.27 | 1.34 |
| Socioeconomic characteristics | ||||
| Wife’s Education | ||||
| No education | 1.00 | 1.00 | 1.00 | 1.00 |
| Primary | 1.47* | 1.48* | 1.52* | 1.61** |
| Secondary | 2.75** | 2.78** | 2.79** | 2.76** |
| Higher | 4.90** | 5.34** | 5.10** | 5.37** |
| Wife’s employment | ||||
| Unemployed | 1.00 | 1.00 | 1.00 | 1.00 |
| Employed without earnings | 0.80 | 0.79 | 0.81 | 0.79 |
| Employed with earnings | 1.00 | 1.00 | 1.04 | 1.00 |
| Wealth | 1.00** | 1.00** | 1.00** | 1.00** |
Notes: All results are reported as odds ratios. All variables are reported at the couple-level unless otherwise specified.
p< 0.05
p< 0.01.
-- = Not applicable. There were 1,623 observations.
Table 6.
Multivariate logistic regression analysis of the association between decision-making arrangement and skilled delivery care controlling for confounders.
| Variables | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Decision-making | ||||
| Who decides about your child’s health care? | ||||
| Agree – Jointly | 1.00 | -- | -- | -- |
| Agree – Wife only | 1.48 | -- | -- | -- |
| Agree – Husband only | 0.89 | -- | -- | -- |
| Agree – Other | 0.73 | -- | -- | -- |
| Disagree | 1.07 | -- | -- | -- |
| Who decides about making major household purchases? | ||||
| Agree – Jointly | -- | 1.00 | -- | -- |
| Agree – Wife only | -- | Omitted | -- | -- |
| Agree – Husband only | -- | 0.78 | -- | -- |
| Agree – Other | -- | 0.77 | -- | -- |
| Disagree | -- | 0.73 | -- | -- |
| Who decides about making daily household purchases? | ||||
| Agree – Jointly | -- | -- | 1.00 | -- |
| Agree – Wife only | -- | -- | 0.81 | -- |
| Agree – Husband only | -- | -- | 0.71 | -- |
| Agree – Other | -- | -- | 0.78 | -- |
| Disagree | -- | -- | 0.93 | -- |
| Who decides about visits to your family or relatives? | ||||
| Agree – Jointly | -- | -- | -- | 1.00 |
| Agree – Wife only | -- | -- | -- | 1.65 |
| Agree – Husband only | -- | -- | -- | 0.92 |
| Agree – Other | -- | -- | -- | 1.11 |
| Disagree | -- | -- | -- | 0.76 |
| Previous use of health services | ||||
| Antenatal care | ||||
| No visits | 1.00 | 1.00 | 1.00 | 1.00 |
| One or more visits | 3.61** | 3.59** | 3.63** | 3.60** |
| Previous complication | ||||
| No previous complication | 1.00 | 1.00 | 1.00 | 1.00 |
| Previous complication | 1.88** | 1.91** | 1.90** | 1.90** |
| Parity | ||||
| First birth | 1.00 | 1.00 | 1.00 | 1.00 |
| Second birth | 0.49** | 0.49** | 0.49** | 0.49** |
| Third birth | 0.30** | 0.30** | 0.30** | 0.30** |
| Fourth or higher order birth | 0.23** | 0.24** | 0.23** | 0.23** |
| Demographic characteristics | ||||
| Wife’s age | 1.058 | 1.056 | 1.057 | 1.060 |
| Place of residence | ||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 |
| Urban | 1.81** | 1.80** | 1.79** | 1.83** |
| Socioeconomic characteristics | ||||
| Wife’s Education | ||||
| No education | 1.00 | 1.00 | 1.00 | 1.00 |
| Primary | 0.78 | 0.78 | 0.79 | 0.81 |
| Secondary | 1.56 | 1.59 | 1.57 | 1.58 |
| Higher | 3.09** | 3.09** | 3.06** | 3.16** |
| Wife’s employment | ||||
| Unemployed | 1.00 | 1.00 | 1.00 | 1.00 |
| Employed without earnings | 1.85 | 1.80 | 1.88 | 1.78 |
| Employed with earnings | 0.51** | 0.51** | 0.51** | 0.51** |
| Wealth | 1.00** | 1.00** | 1.00** | 1.00** |
Notes: All results are reported as odds ratios. All variables are reported at the couple-level unless otherwise specified.
p< 0.05,
p< 0.01.
-- = Not applicable. There were 1,623 observations.
DISCUSSION
In this study we make both methodological and substantive contributions to the literature on couples’ decision-making and maternal health care use. Methodologically, we propose a new operationalization of household decision-making variables, by comparing spouse’s responses to common household decision-making questions. We create a more detailed typology of responses than is typically used by retaining information about spousal discordance. Using this new measure, we uncover four important findings. First, there are substantial levels of discordance in responses to each household decision-making item. Second, household decision-making by husbands alone, involvement of others in household decisions, and discordant reports about who makes household decisions result in lower maternal health care utilization compared to joint decision making. Third, associations between household decision-making arrangements and health service utilization are stronger for antenatal care than for skilled delivery care. Finally, compared to using women’s or couples’ reports, using only the husband’s reports yields significantly weaker associations between household decision-making arrangements and maternal health care utilization.
The level of discordance presented in our study (between 49.8% and 61.4%) is consistently high, which is similar to previous studies that reported discordance about common household decisions between 10% and 53% (Allendorf, 2007; Becker et al., 2006; Ghuman et al., 2006; Jejeebhoy, 2002). As shown in Table 2, the most common pattern of discordance is when one spouse says that the decision is made by the husband alone and the other spouse says that they make the decision together. This type of discordance may be due to a number of factors, such as poor communication between spouses about common household decisions (Mullany, 2010), gender-based differences in the understanding of each decision-making question (Ghuman et al., 2006; Miller et al., 2001), or a lack of clarity about the gender norms related to each decision (Allendorf, 2007).
Discordance among couples is not a neutral finding. By examining each member of a couple’s response to each decision-making question, our study shows that, compared to couples who agree that they make household decisions jointly, use of maternal health services is lower among couples who give discordant reports about household decisions. If discordance indicates a lack of communication between the husband and wife (Mullany, 2010), then this may point to the importance of improving spousal communication in order to increase maternal health care utilization. However, it is difficult to interpret why couples that give discordant reports about household decision-making use less maternal health care.
In order to better understand the association between discordance among couples and health care use, discordant responses for each decision-making item were disaggregated into meaningful categories: (1) Wife says wife alone made decision/husband says something else, (2) Husband says wife alone made decision/wife says something else, (3) Wife says decision was made jointly/husband says something else, (4) Husband says decision was made jointly/wife says something else, and (5) Some other form of disagreement. All disaggregated reports by couples (the original concordant categories and these new discordant categories) were compared to the concordant report of joint decision-making. For each decision-making item, different categories of discordance were significantly associated with antenatal care use and no discordance categories were significantly associated with skilled delivery care (data not shown). Since there is no clear pattern for any of these categories of discordant reports, all discordant responses remain in one category for our main analysis.
There is a need to further explore the patterns of discordance across all four items about common household decisions in order to better understand their relationship with reproductive health care decisions. Specifically, it is important to examine whether discordance is related to poor spousal communication (Mullany et al., 2005), is a product of gendered responses to decision-making questions (Ghuman et al., 2006; Miller et al., 2001), or is related to actual (or expected) gender roles within the household. Future couples studies should find new and innovative ways to disaggregate household decision-making questions in order to assess the impact of discordant spousal reports on health care utilization.
We also found that concordant reports of household decision-making by husbands alone is associated with less maternal health care utilization compared to joint decision-making. Although previous studies included decision-making by husbands alone as an informative category, it is difficult to identify the association between decision-making by husbands and health care utilization. The multivariate models used to predict health care use in the other studies of couples either combined decision-making by the husband alone with other patterns of decision-making, such as making the decision jointly with someone else (Allendorf, 2007; Becker et al., 2006), or the survey instrument used to measure women’s autonomy emphasized women making decisions alone (Ghuman et al., 2006; Jejeebhoy, 2002). Consequently it is difficult to discern the control that men may or may not have in household decision-making.
The few studies that have examined male involvement in reproductive health decisions show mixed results. In Pakistan, men’s participation in household decision-making is not necessarily associated with their involvement in reproductive health decisions (Mumtaz & Salway, 2009). Male control over household decisions is seen as a cultural expectation and a wife’s failure to acknowledge his authority is perceived as “an erosion of their husband’s masculinity” (Mumtaz & Salway, 2009, p. 1352). However, although he may have the final say, there is an expectation that the husband and wife will discuss and negotiate the decision at hand. This expectation emphasizes the importance placed on joint decision-making in the Pakistani context. In Nepal, husbands’ domination of household decision-making is associated with less male involvement during pregnancy and childbirth, whereas joint decision-making is associated with higher levels of male involvement (Mullany et al., 2005). In Guatemala, the more power husbands are reported to have in household decision-making, the more likely women are to report that their husbands provided advice or care during pregnancy (Carter, 2002). The Guatemala study also suggests that there is a positive association between husbands’ involvement during pregnancy and reproductive health care use; however, this may not be true in all social contexts.
Although our study was not designed to explain the relationship between husbands’ authority and health outcomes, we posit three potential mechanisms that may account for the negative association between husbands’ control over household decision-making and use of maternal health services. First, a common explanation in the literature on women’s decision-making power is that women with greater agency are more likely to obtain maternal health care. This is attributed to women’s power to realize their preferences, which includes a stronger preference for ensuring their own health, compared with their husband’s (Allendorf, 2010). Therefore, as a husband begins to share control of household decisions, it is possible that his wife’s health care will become a higher priority. Second, husbands’ control over household decisions may be correlated with more conservative gender norms, which may be associated with conventional reproductive behaviors, that is, reliance on informal, untrained birth attendants. Third, husbands’ control over household decisions may limit women’s mobility outside the home, inhibiting uptake of antenatal care and access to resources for skilled delivery care. Further research is necessary in order to elucidate these and other possible mechanisms through which husbands’ power in household decision-making affects maternal health care utilization, including qualitative inquiry into the relationship between domestic decision-making and reproductive health decisions (Story et al., 2012).
The strength of the association between health care use and husbands’ control over decision-making differs by the type of health outcome. Specifically, compared to joint decision-making, couples in which the husband makes decisions alone use less antenatal care. Although the pattern of association is similar for skilled delivery care, none of the odds ratios are statistically significant. This finding is also consistent with prior studies on maternal health service utilization (Becker et al., 2006). Since the decisions to use different kinds of maternal health services are made under varying circumstances (e.g., planning for the initiation of antenatal care at some point over several months versus deciding to use professional delivery care in emergency situations), the association between decision-making patterns and maternal health care use should be examined across multiple services in which voluntary decision making is more or less likely to have an influence.
Another major methodological finding is that the strength and magnitude of the association between household decision-making and maternal health care utilization depends on who responds to the question. Three of the four prior studies show substantive differences in the association between decision-making and health outcomes when comparing husbands’ and wives’ reports (Becker et al., 2006; Ghuman et al., 2006; Jejeebhoy, 2002). Although Allendorf (2007) did not report any substantive differences between husbands’ and wives’ reports, couples’ reports (concordant reports only) increased the strength of the association between decision-making and health care utilization. Our study also found an increase in the magnitude of the association between decision-making and health care use when using couples’ reports compared to using husbands’ or wives’ reports alone. The increased strength of the association may be due to the creation of a new response category denoting those husbands and wives who give discordant reports about who makes household decisions. Separating discordant responses, allows us to study patterns of concordance among the other response categories. Assessing the association between health outcomes and the concordant response categories may more accurately represent the “true” response or may account for an unmeasured mediating factor, such as good spousal communication. Future research should triangulate across husbands’ and wives’ self-reports about decision-making in order to improve measurement accuracy.
While this study provides a comparative picture of household decision-making and maternal health care utilization, it was not designed to infer a causal association due to the retrospective, cross-sectional nature of the data. Since reports about decision-making relate to the time of the survey and the maternal health care questions relate to a time in the past 12 months, it is difficult to determine whether husbands’ and wives’ decision-making patterns changed since the birth of their youngest child. Another limitation to our analysis was the use of women’s reports for the outcome variables, which did not account for discordant reports among couples on these measures. However, men’s reports of the outcome variables were strongly correlated with women’s reports. Finally, our analysis did not allow us to incorporate specific information about other family members frequently involved in reproductive health decisions, such as wife’s mother and mother-in-law.
Our results have implications for future maternal health interventions and survey work. Although instances of husbands’ unilateral decision-making appear to reduce the use of maternal health services, husbands must not be viewed as the “problem” and should not be ignored by maternal health outreach efforts. The husband is an important part of the decision-making process and male involvement in reproductive health decisions has the potential to positively impact maternal health care utilization (Carter, 2002; Mullany et al., 2005; Mumtaz & Salway, 2009). In addition, given the results of our study, it is important to consider whether future maternal health surveys should interview both husbands and wives. According to Mullany (2010), women are often considered the “gold standard” for knowledge and practices related to maternal health, but men often dominate the decision-making related to large, health-related purchases in the household. We found the same to be true in Bangladesh; therefore, if survey organization resources are available to collect data from both men and women, it is important to consider the variation in responses when both partners are interviewed, especially the valuable information available in the patterns of concordance and discordance. Finally, the complexity of the decision-making process makes it difficult to quantify decision-making patterns, especially when decisions are made together. We recommend exploring new ways to quantify decision-making using a Likert-type scale to measure which partner has the most say in each decision or using ethnographic methods, such as participant observation, to better understand the cultural nuances of household decision-making.
Research Highlights.
Discordant reports about who makes household decisions resulted in lower health care use compared to joint decision-making.
Associations between decision-making arrangements and health service use were stronger for antenatal than delivery care.
The associations increase in magnitude when using couples’ reports compared to using husbands’ or wives’ reports alone.
Interviewing both men and women provides valuable information available in concordant and discordant reports.
Acknowledgments
During the development of this manuscript, W. Story received financial support from the Agency for Healthcare Research and Quality Predoctoral Training Grant. This study was also supported by core funding from Eunice Kennedy Shriver National Institute of Child Health and Human Development grant R24 HD041028 to the Population Studies Center, University of Michigan. We would like to thank Apoorva Aekka for excellent research assistance; and Caroline Hartnett, Anna West, and the three anonymous reviewers for helpful feedback.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allendorf K. Couples’ reports of women’s autonomy and health-care use in Nepal. Studies in Family Planning. 2007;38(1):35–46. doi: 10.1111/j.1728-4465.2007.00114.x. [DOI] [PubMed] [Google Scholar]
- Allendorf K. The quality of family relationships and use of maternal health-care services in India. Studies in Family Planning. 2010;41(4):263–276. doi: 10.1111/j.1728-4465.2010.00252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amin R, Shah NM, Becker S. Socioeconomic factors differentiating maternal and child health-seeking behavior in rural Bangladesh: A cross-sectional analysis. International Journal for Equity in Health. 2010;9:9. doi: 10.1186/1475-9276-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangladesh Maternal Morality and Health Care Survey. Summary of key findings and implications. [Accessed on September 21, 2011];2010 Retrieved from http://www.dghs.gov.bd/dmdocuments/BMMS_2010.pdf.
- Bankole A, Singh S. Couples’ fertility and contraceptive decision-making in developing countries: Hearing the man’s voice. International Family Planning Perspectives. 1998;24:15–24. [Google Scholar]
- Becker S. Couples and reproductive health: A review of couple studies. Studies in Family Planning. 1996;27(6):291–306. [PubMed] [Google Scholar]
- Becker S. Measuring unmet need: Wives, husbands, or couples? International Family Planning Perspectives. 1999;25:172–180. [Google Scholar]
- Becker S, Fonseca-Becker F, Schenck-Yglesias C. Husbands’ and wives’ reports of women’s decision-making power in Western Guatemala and their effects on preventive health behaviors. Social Science & Medicine. 2006;62:2313–2326. doi: 10.1016/j.socscimed.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Campbell OMR, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–1299. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- Carter M. Husbands and maternal health matters in rural Guatemala: Wives’ reports on their spouses’ involvement in pregnancy and birth. Social Science & Medicine. 2002;55:437–450. doi: 10.1016/s0277-9536(01)00175-7. [DOI] [PubMed] [Google Scholar]
- Chakraborty N, Islam MA, Chowdhury RI, Bari W, Akhter HH. Determinants of the use of maternal health services in rural Bangladesh. Health Promotion International. 2003;18 (4):327–337. doi: 10.1093/heapro/dag414. [DOI] [PubMed] [Google Scholar]
- Choudhury N, Ahmed SM. Maternal care practices among the ultra poor households in rural Bangladesh: A qualitative exploratory study. BMC Pregnancy and Childbirth. 2011;11:15. doi: 10.1186/1471-2393-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collin SM, Anwar I, Ronsmans C. A decade of inequality in maternity care: antenatal care, professional attendance at delivery, and caesarean section in Bangladesh (1991–2004) International Journal for Equity in Health. 2007;6:9. doi: 10.1186/1475-9276-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuta M, Salway S. Women’s position within the household as a determinant of maternal health care use in Nepal. International Family Planning Perspectives. 2006;32(1):17–27. doi: 10.1363/3201706. [DOI] [PubMed] [Google Scholar]
- Gabrysch S, Campbell OM. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy and Childbirth. 2009;9:34. doi: 10.1186/1471-2393-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghuman SJ, Leeb HJ, Smith HL. Measurement of women’s autonomy according to women and their husbands: Results from five Asian countries. Social Science Research. 2006;35:1–28. [Google Scholar]
- Gipson JD, Hindin MJ. “Having another child would be a life or death situation for her”: Understanding pregnancy termination among couples in rural Bangladesh. American Journal of Public Health. 2008;98:1827–1832. doi: 10.2105/AJPH.2007.129262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetz AM, Sen Gupta R. Who takes the credit? Gender, power, and control over loan use in rural credit programs in Bangladesh. World Development. 1996;24(1):45–63. [Google Scholar]
- Jejeebhoy SJ. Convergence and divergence in spouses’ perspectives on women’s autonomy in rural India. Studies in Family Planning. 2002;33(4):299–308. doi: 10.1111/j.1728-4465.2002.00299.x. [DOI] [PubMed] [Google Scholar]
- Kabeer N. Conflicts over credit: Re-evaluating the empowerment potential of loans to women in rural Bangladesh. World Development. 2001;29(1):63–84. [Google Scholar]
- Kulczycki A. Husband-wife agreement, power relations and contraceptive use in Turkey. International Family Planning Perspectives. 2008;34:127–137. doi: 10.1363/ifpp.34.127.08. [DOI] [PubMed] [Google Scholar]
- McDougall J, Edmeades J, Krishnan S. (Not) talking about sex: couple reports of sexual discussion and expression in Bangalore, India. Culture, Health & Sexuality. 2011;13:141–156. doi: 10.1080/13691058.2010.520740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K, Zulu EM, Watkins SC. Husband-wife survey responses on Malawi. Studies in Family Planning. 2001;32:161–174. doi: 10.1111/j.1728-4465.2001.00161.x. [DOI] [PubMed] [Google Scholar]
- Montgomery R, Bhattacharya D, Hulme D. Credit for the poor in Bangladesh. In: Hulme D, Mosley P, editors. Finance against poverty. London: Routledge; 1996. [Google Scholar]
- Moss W, Darmstadt GL, Marsh DR, Black RE, Santosham M. Research priorities for the reduction of perinatal and neonatal morbidity and mortality in developing country communities. Journal of Perinatology. 2002;22:484–495. doi: 10.1038/sj.jp.7210743. [DOI] [PubMed] [Google Scholar]
- Mullany BS, Hindin MJ, Becker S. Can women’s autonomy impede male involvement in pregnancy health in Katmandu, Nepal? Social Science & Medicine. 2005;61(9):1993–2006. doi: 10.1016/j.socscimed.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Mullany BC. Spousal agreement on maternal health practices in Kathmandu, Nepal. Journal of Biosocial Science. 2010;42:689–693. doi: 10.1017/s0021932010000222. [DOI] [PubMed] [Google Scholar]
- Mumtaz Z, Salway S. Understanding gendered influences on women’s reproductive health in Pakistan: Moving beyond the autonomy paradigm. Social Science & Medicine. 2009;68:1349–1356. doi: 10.1016/j.socscimed.2009.01.025. [DOI] [PubMed] [Google Scholar]
- NIPORT. Bangladesh Demographic and Health Survey 2007. Dhaka, Bangladesh and Calverton, Maryland, USA: National Institute of Population Research and Training, Mitra and Associates, and Macro International; 2009. [Google Scholar]
- Parkhurst JO, Rahman SA, Ssengooba F. Overcoming access barriers for facility-based delivery in low-income settings: Insights from Bangladesh and Uganda. Journal of Health, Population and Nutrition. 2006;24(4):438–445. [PMC free article] [PubMed] [Google Scholar]
- Paul BK, Rumsey DJ. Utilization of health facilities and trained birth attendants for childbirth in rural Bangladesh: An empirical study. Social Science & Medicine. 2002;54(12):1755–1765. doi: 10.1016/s0277-9536(01)00148-4. [DOI] [PubMed] [Google Scholar]
- Rozario S. The dai and the doctor: Discourses in women’s reproductive health in rural Bangladesh. In: Ram K, Jolly M, editors. Maternities and modernities: Colonial and postcolonial experiences in Asia and the Pacific. Cambridge: Cambridge University Press; 1998. pp. 144–176. [Google Scholar]
- Story WT, Burgard SA, Lori JL, Ali NA, Taleb F, Hoque DM. Husbands’ involvement in delivery care utilization in rural Bangladesh: A qualitative study. BMC Pregnancy and Childbirth. 2012;12:28. doi: 10.1186/1471-2393-12-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) World Health Report 2005: Make every mother and child count. Geneva: WHO; 2005. [Google Scholar]