Abstract
Development of systemic treatment for advanced pancreatic cancer (APC) has been challenging. After fluorouracil, gemcitabine (GEM) became the treatment of choice based on its benefit of symptom relief. Many cytotoxic agents have been combined with GEM in search of regimens with improved survival benefit. However, there were only marginal benefits in people with good performance status. Recently, the combination regimen consisting of oxaliplatin, irinotecan, fluorouracil, and leucovorin (FOLFIRINOX) was found to achieve unprecedented survival benefit and has become the preferred option for patients with good clinical conditions. On the other hand, many biological agents have been combined with GEM, but only erlotinib was found to derive statistically significant survival advantage. However, the effect was too small to be appreciated clinically. The effort in development of targeted therapy in APC continues. This paper summarized key findings in the development of chemotherapy and targeted therapy for APC patients and discussed future directions in management.
1. Introduction
Advanced pancreatic cancer (APC) is a dismal human cancer with median overall survival of merely 6 months. Approaches such as radiation, conventional chemotherapy, or combination of these modalities could not alter the disease course. Previously, fluorouracil (5FU) was given for treatment [1], but it was later taken over by gemcitabine (GEM) due to its effect on alleviation of disease-related symptoms [2]. However, the survival benefit of GEM was small. In desperate need of better treatment, much effort has been put on exploring new treatment regimes. It was once expected that biological agents could bring hope to this deadly cancer just like how they revolutionized the treatment of many other malignancies. When most of these agents seemed to fail, a nongemcitabine-containing combination chemotherapy (FOLFIRINOX) was found to give major improvement in response and survival and set the new standard of the treatment [3].
This paper summarized key development in the treatment of APC and discussed future possibilities in light of our current understanding.
2. Traditional Chemotherapy
The progress in the development of systemic treatment of advanced pancreatic cancer (APC) has been slow (Figure 1). Traditionally, fluorouracil (5FU) was the only treatment option and provided only marginal benefit [1]. In 1997, Burris et al. in a randomized phase III trial showed that GEM was superior to 5FU in alleviation of disease-related symptoms and improving survival [2]. Although the improvement of median survival was merely 1.2 months (from 4.4 months with 5FU to 5.6 months with GEM, P = 0.0025), the 1-year survival rate was 18% for the GEM and 2% for the 5FU arms, respectively. GEM also gave a favorable clinical benefit rate (23.8% versus 4.8%, P = 0.0022). Thereafter, GEM took over to become the standard treatment of APC.
Figure 1.
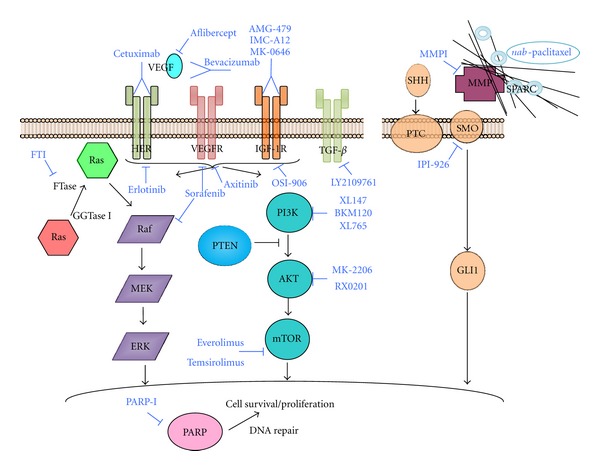
Selected signaling pathways and their targeting in advanced pancreatic cancer.
Much effort was directed to improve the outcome of GEM treatment. GEM-based doublets with either platinum analogues or 5FU were extensively studied (Table 1). When GEM was combined with either cisplatin [4] or oxaliplatin [5] in individual trials, no benefits over single-agent GEM could be shown. Nevertheless, pooled analysis of these two European trials [4, 5] demonstrated that GEM-platinum doublet gave a 25% reduction in risk of progression (P = 0.0030) and 19% reduction in risk of death (P = 0.031) [6]. Yet, these benefits were mainly observed in asymptomatic patients with good performance status. On the other hand, addition of 5FU to GEM did not yield any survival improvement [7, 8]. This finding was further supported by trials where 5FU was substituted by the prodrug capecitabine (CAP) in the GEM doublet [9–11]. In these randomized studies, the GEM-CAP combination improved neither the progression-free survival (PFS), overall survival (OS), nor quality of life (Table 1).
Table 1.
Major phase III GEM-based combination chemotherapy.
| Regime | No. pts | ORR (%) | PFS/TTP (mo) | OS (mo) | Reference |
|---|---|---|---|---|---|
| GEM + cisplatin | 195 | 10.2 | 5.3 | 7.5 | Heinemann et al. [4] |
| GEM | 8.2 | 3.1 | 6.0 | ||
| GEM + oxaliplatin | 832 | (P = 0.11) | 2.7 | 5.7 | Poplin et al. [5] |
| GEM | 2.6 | 4.9 | |||
| GEM + 5FU | 322 | 6.9 | 3.4* | 6.7 | Berlin et al. [7] |
| GEM | 5.6 | 2.2 | 5.4 | *P = 0.022 | |
| GEM + capecitabine | 533 | 19.2 | 5.3 | 7.1 | Cunningham et al. [9] |
| GEM | 12.4 | 3.8 | 6.2 | ||
| GEM + capecitabine GEM |
319 | QoL same | n/a | n/a | Bernhard et al. [10] |
| GEM + capecitabine | 319 | 10.0 | 4.3 | 8.4 (10.1*) | Herrmann et al. [11] |
| GEM | 7.8 | 3.9 | 7.2 (7.4) | (*KPS 90–100; P = 0.014) |
Abbreviation: ORR: overall response rate; PFS: progression free survival; TTP: time to progression; OS: overall survival; QoL: quality of life.
As APC is not the most prevalent cancer and most clinical trials contained around 200–300 subjects, it has been criticized that individual study has insufficient statistical power to detect the effect of combination chemotherapy. In view of this, a number of metaanalyses have been conducted (see Table 2). In summary, they primarily showed a significant benefit when GEM was combined with platinum or 5FU, but not with other cytotoxic agents. The maximum survival benefit of GEM-based combination chemotherapy was only marginal and mainly derived from patients with good performance status. Thus, the addition of platinum analogues to GEM was not recommended in general.
Table 2.
Selected metaanalysis of GEM-based combination chemotherapy.
| Reference | No. of pts | HR (all) | HR for platinum | HR for 5FU/capecitabine | HR for other agents |
|---|---|---|---|---|---|
| Heinemann et al. [12] | 4465 | 0.91* | 0.85 | 0.9 | 0.99 |
| Sultana et al. [13] | 9970 | 0.91 | — | — | — |
| Vaccaro et al. [14] | 2422 | 0.87 | 0.94 (cisplatin, P = 0.61) | 0.86 (P = 0.04) | — |
| 0.86 (oxaliplatin, P = 0.04) |
*ECOG PS 0-1: HR 0.76, P < 0.001; ECOG PS 2: HR 1.08, P = 0.40.
Abbreviations: HR: hazard ratio; 5FU: fluorouracil.
Recently, in the French PRODIDGE 4/ACCORD 11 trial, the polychemotherapy regimen FOLFIRINOX (oxaliplatin, irinotecan, fluorouracil, and leucovorin) significantly improved the median OS of metastatic pancreatic cancer patients from 6.8 to 11.1 months when compared with single-agent GEM [3]. Such a magnitude of median OS improvement (4.3 months) was impressive but came with a price. Notably, 45% of the enrolled patients reported grade 3 or 4 adverse events (AEs). The most common AEs were diarrhea, fatigue, and vomiting. About 45% of patients experienced grade 3/4 neutropenia, including febrile neutropenia in 5.4%. In view of significant treatment-related toxicities, FOLFIRINOX is only recommended for patients with good performance status and medical conditions.
3. Biological Therapy in Pancreatic Cancer
Pancreatic cancer is a heterogeneous disease. Although the constitutively active K-rasG12D allele mutation has been reported in 70%–90% of pancreatic cancers [15–17], no single oncogene addiction driving the growth of this cancer has been identified so far. According to the pancreatic cancer genome project, this cancer contains at least 63 genetic alterations on average. Besides K-ras, common mutations include FRAF (20%), AKT2 (20%), p16/CDKN2A (75%–80%), p53 (50%–75%), SMAD4 (50%–60%), and BRCA2 (10%) [17]. A number of cellular signaling pathways have been implicated in the pathogenesis and maintenance of this cancer, including hedgehog signaling, K-ras signaling, and transforming growth factor beta (TGF-β) signaling, to name a few. The following sections will discuss the key findings in the quest of better treatment of APC using biological therapy.
3.1. Ras Signaling
As K-ras mutation is the commonest mutation in pancreatic cancer, it was one of the earliest targets for drug development. The functional sites of this protein are difficult to access, so scientists have attempted to target the enzyme taking part in modification/activation of Ras called farnesyltransferase. Examples of farnesyltransferase inhibitors (FTIs) include tipifarnib and SCH66336. These agents as single agents or when combined with GEM showed no appreciable activity in clinical trials [18–21], and the failure of FTIs was suspected to be due to recruitment of alternative pathways for Ras activation. Nowadays, people are still developing novel methods such as antisense and RNA interference and inhibitors of its key effector MEK kinase to target the Ras protein or its signaling.
3.2. Epidermal Growth Factor Receptor (EGFR)
EGFR is overexpressed in human pancreatic cancer and is suspected to play an important role in metastasis [22]. Both small molecule tyrosine kinase inhibitors (TKIs) and monoclonal antibodies are well-known strategies in targeting the EGFRs. Erlotinib is a TKI of this class and has gained attention in the treatment of APC. In the PA.3 study, which is a multicentre, randomized, double-blind, and placebo-controlled clinical study of erlotinib in combination with GEM in APC, the erlotinib-GEM combination compared with single-agent GEM showed a statistically improvement in PFS (HR 0.77 (95% CI, 0.64 to 0.92; P = 0.004)) and 1-year survival (23% versus 17%; P = 0.023) [23]. The median OS was also increased, but the improvement was small (6.24 versus 5.91 months, HR 0.82 (95% CI, 0.69 to 0.99; P = 0.038)). This combination is not considered a clinically meaningful option or a cost-effective choice by many physicians.
Cetuximab is a chimeric monoclonal antibody against ErbB-1 receptors with high specificity.
In a phase II study combining cetuximab and GEM in untreated APC patients, there appeared to be encouraging results [24]. But this combination did not show superiority to single-agent GEM when tested in a randomized phase III study (6.3 versus 5.9 months, HR 1.06; (95% CI, 0.91 to 1.23; P = 0.23)) [25]. In order to “intensify” the anti-EGFR activity, people have attempted to combine another anti-EGFR antibody, panitumumab, with erlotinib and GEM [26]. Nevertheless, excessive toxicities shown in the phase II study precluded further pursuit using this combination. These research studies suggest that EGFR expression, though correlating with tumor aggressiveness, does not necessarily predict response to anti-EGFR therapy. The role of this class of treatment remains to be defined.
3.3. Angiogenesis
Tumor growth is sustained by angiogenesis. Vascular endothelial growth factor (VEGF) expression was found to be associated with liver metastasis and poor prognosis in pancreatic cancer [27]. However, trials on anti-VEGF therapy in APC have been disappointing.
Bevacizumab is the most widely used anti-VEGF antibody and has been shown to enhance the effect of chemotherapy in many other cancers. In the Cancer and Leukemia Group B (CALGB) 80303 trial, patients with APC were randomized to receive GEM with or without bevacizumab [28]. The addition of bevacizumab, however, did not extend overall survival. Similarly, in the phase III AVITA trial, patients were given GEM with erlotinib plus either bevacizumab or placebo. Despite improved PFS (median: 4.6 months versus 3.6 months, HR 0.73, P = 0.0002), it did not translate into improved overall survival [29]. Attempts of other oral inhibitors of VEGF receptor, such as axitinib [30] or aflibercept [31], or multikinase inhibitor like sorafenib [32], also failed to improve survival.
3.4. Other Potential Treatment Strategies in the Near Future
The chemotherapy-resistant nature of APC and failure of antiangiogenesis therapy have prompted revision on the existing model of tumor microarchitecture. Increasing evidence suggests that pancreatic cancer is characterized by “tumor desmoplasia,” the presence of dense stromal tissue with decreased vascular density that penetrates and envelopes the tumor [33]. It is now believed that this stromal tissue impairs drug delivery, leading to treatment resistance. nab-paclitaxel is an albumin-bound formulation of paclitaxel with enhanced affinity to a stromal protein called secreted protein acidic and rich in cysteine (SPARC), which is overexpressed in the stroma of APC. As a result, nab-paclitaxel is concentrated around the tumor. Early phase I/II trial demonstrated promising result when nab-paclitaxel was combined with GEM in untreated APC patients. The reported response rate was 48%, 1-year overall survival rate was 48%, and the median OS was 12.2 months [34]. Phase III trial of this combination is underway. Novel technological advance such as nanotechnology might help develop drug therapy that can overcome the barrier imposed by the dense stromal microenvironment. Other ongoing pieces of research aiming at manipulating the signaling or function of microenvironment include hedgehog pathway inhibitors and hyaluronidase which breaks down the hyaluronan in the extracellular matrix.
Pancreatic cancer is a complicated disease. Increasing understanding of the molecular pathways to pathogenesis and growth of pancreatic cancer showed that a number of other signaling pathways are also implicated. For instance, insulin-like growth factor receptor (IGFR-1) mRNA in pancreatic cancer was more than 30 times that in normal pancreatic tissue, and abnormal regulation of IGF-1 autocrine loop was associated with increased tumorigenicity [35, 36]. Another signaling pathway, transforming growth factor beta (TGF-β), has both the effects of regulation of cell growth and mediation of cancer cell proliferation and metastasis [37]. Drug development that targets these pathways is still preliminary.
In the era of personalized medicine, there is an unmet need for development of biomarkers to guide management. Carbohydrate antigen 19.9 (CA 19.9) is a widely accepted surrogate marker for treatment response, although it has only modest sensitivity and specificity [38]. Furthermore, K-ras wild type status appeared to derive better survival from erlotinib than K-ras mutant tumor, and so did patients who developed rash during erlotinib treatment. Pharmacogenetics also plays a role. Depressed level of GEM metabolism gene products such as deoxycytidine kinase (dCK) and ribonucleoside reductases M1 and M2 (RRM1, RRM2) has been correlated with treatment resistance to GEM [39–41]. Low expressers of the nucleoside transporter-1 (hENT1) reduced uptake of GEM in cell and were found to have poorer prognosis [40]. In the future, we wish to identify biomarker that can predict response of treatment and stratify patients accordingly to enhance the treatment effect.
4. Conclusion
The development of treatment for APC has been challenging. Although many biological agents were tested, recent advances in clinically significant treatment are dominated by chemotherapy. The FOLFIRINOX regimen has gained increased acceptance, and the effect of nab-paclitaxel-GEM combination is awaited from phase III study. The future prospective depends on further understanding in the tumor biology, targeting various growth factor signaling pathways, and development of new technologies, including identification of biomarkers that predict treatment response.
Abbreviations
- FTI:
Farnesyltransferase inhibitor
- GGTase I:
Geranylgeranyltransferase I
- IGF-1R:
Insulin-like growth factor 1 receptor
- HER:
Human epidermal growth factor receptor
- MEK:
Mitogen-activated protein kinase/ERK kinase
- MMP:
Matrix metalloproteinases
- PTC:
Patched-1 receptor
- PTEN:
Phosphatase and tensin homologue deleted on chromosome ten
- SHH:
Sonic hedgehog
- SMO:
Smoothened
- SPARC:
Secreted protein acidic and rich in cysteine
- TGF-β:
Transforming growth factor β
- VEGF:
Vascular endothelial growth factor
- VEGFR:
VEGF receptor.
References
- 1.Glimelius B, Hoffman K, Sjödén PO, et al. Chemotherapy improves survival and quality of life in advanced pancreatic and biliary cancer. Annals of Oncology. 1996;7(6):593–600. doi: 10.1093/oxfordjournals.annonc.a010676. [DOI] [PubMed] [Google Scholar]
- 2.Burris HA, III, Moore MJ, Andersen J, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. Journal of Clinical Oncology. 1997;15(6):2403–2413. doi: 10.1200/JCO.1997.15.6.2403. [DOI] [PubMed] [Google Scholar]
- 3.Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. The New England Journal of Medicine. 2011;364(19):1817–1825. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 4.Heinemann V, Quietzsch D, Gieseler F, et al. Randomized phase III trial of gemcitabine plus cisplatin compared with gemcitabine alone in advanced pancreatic cancer. Journal of Clinical Oncology. 2006;24(24):3946–3952. doi: 10.1200/JCO.2005.05.1490. [DOI] [PubMed] [Google Scholar]
- 5.Poplin E, Feng Y, Berlin J, et al. Phase III, randomized study of gemcitabine and oxaliplatin versus gemcitabine (fixed-dose rate infusion) compared with gemcitabine (30-minute infusion) in patients with pancreatic carcinoma E6201: a trial of the Eastern cooperative oncology group. Journal of Clinical Oncology. 2009;27(23):3778–3785. doi: 10.1200/JCO.2008.20.9007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heinemann V, Labianca R, Hinke A, Louvet C. Increased survival using platinum analog combined with gemcitabine as compared to single-agent gemcitabine in advanced pancreatic cancer: pooled analysis of two randomized trials, the GERCOR/GISCAD intergroup study and a German multicenter study. Annals of Oncology. 2007;18(10):1652–1659. doi: 10.1093/annonc/mdm283. [DOI] [PubMed] [Google Scholar]
- 7.Berlin JD, Catalano P, Thomas JP, Kugler JW, Haller DG, Benson AB. Phase III study of gemcitabine in combination with fluorouracil versus gemcitabine alone in patients with advanced pancreatic carcinoma: Eastern cooperative oncology group trial E2297. Journal of Clinical Oncology. 2002;20(15):3270–3275. doi: 10.1200/JCO.2002.11.149. [DOI] [PubMed] [Google Scholar]
- 8.Sultana A, Smith CT, Cunningham D, Starling N, Neoptolemos JP, Ghaneh P. Meta-analyses of chemotherapy for locally advanced and metastatic pancreatic cancer: results of secondary end points analyses. British Journal of Cancer. 2008;99(1):6–13. doi: 10.1038/sj.bjc.6604436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cunningham D, Chau I, Stocken DD, et al. Phase III randomized comparison of gemcitabine versus gemcitabine plus capecitabine in patients with advanced pancreatic cancer. Journal of Clinical Oncology. 2009;27(33):5513–5518. doi: 10.1200/JCO.2009.24.2446. [DOI] [PubMed] [Google Scholar]
- 10.Bernhard J, Dietrich D, Scheithauer W, et al. Clinical benefit and quality of life in patients with advanced pancreatic cancer receiving gemcitabine plus capecitabine versus gemcitabine alone: a randomized multicenter phase III clinical trial—SAKK 44/00-CECOG/PAN.1.3.001. Journal of Clinical Oncology. 2008;26(22):3695–3701. doi: 10.1200/JCO.2007.15.6240. [DOI] [PubMed] [Google Scholar]
- 11.Herrmann R, Bodoky G, Ruhstaller T, et al. Gemcitabine plus capecitabine compared with gemcitabine alone in advanced pancreatic cancer: a randomized, multicenter, phase III trial of the Swiss group for clinical cancer research and the central European cooperative oncology group. Journal of Clinical Oncology. 2007;25(16):2212–2217. doi: 10.1200/JCO.2006.09.0886. [DOI] [PubMed] [Google Scholar]
- 12.Heinemann V, Boeck S, Hinke A, Labianca R, Louvet C. Meta-analysis of randomized trials: evaluation of benefit from gemcitabine-based combination chemotherapy applied in advanced pancreatic cancer. BMC Cancer. 2008;8, article 82 doi: 10.1186/1471-2407-8-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sultana A, Smith CT, Cunningham D, Starling N, Neoptolemos JP, Ghaneh P. Meta-analyses of chemotherapy for locally advanced and metastatic pancreatic cancer. Journal of Clinical Oncology. 2007;25(18):2607–2615. doi: 10.1200/JCO.2006.09.2551. [DOI] [PubMed] [Google Scholar]
- 14.Vaccaro V, Sperduti I, Milella M. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. The New England Journal of Medicine. 2011;365(8):768–769. doi: 10.1056/NEJMc1107627. [DOI] [PubMed] [Google Scholar]
- 15.Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, Perucho M. Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell. 1988;53(4):549–554. doi: 10.1016/0092-8674(88)90571-5. [DOI] [PubMed] [Google Scholar]
- 16.Hezel AF, Kimmelman AC, Stanger BZ, Bardeesy N, DePinho RA. Genetics and biology of pancreatic ductal adenocarcinoma. Genes and Development. 2006;20(10):1218–1249. doi: 10.1101/gad.1415606. [DOI] [PubMed] [Google Scholar]
- 17.Jones S, Zhang X, Parsons DW, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;321(5897):1801–1806. doi: 10.1126/science.1164368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen SJ, Ho L, Ranganathan S, et al. Phase II and pharmacodynamic study of the farnesyltransferase inhibitor R115777 as initial therapy in patients with metastatic pancreatic adenocarcinoma. Journal of Clinical Oncology. 2003;21(7):1301–1306. doi: 10.1200/JCO.2003.08.040. [DOI] [PubMed] [Google Scholar]
- 19.Macdonald JS, McCoy S, Whitehead RP, et al. A phase II study of farnesyl transferase inhibitor R115777 in pancreatic cancer: a Southwest oncology group (SWOG 9924) study. Investigational New Drugs. 2005;23(5):485–487. doi: 10.1007/s10637-005-2908-y. [DOI] [PubMed] [Google Scholar]
- 20.van Cutsem E, van de Velde H, Karasek P, et al. Phase III trial of gemcitabine plus tipifarnib compared with gemcitabine plus placebo in advanced pancreatic cancer. Journal of Clinical Oncology. 2004;22(8):1430–1438. doi: 10.1200/JCO.2004.10.112. [DOI] [PubMed] [Google Scholar]
- 21.Lersch C, van Cutsem E, Amado R, et al. Randomized phase II study of SCH, 66336 and gemcitabine in the treatment of metastatic adenocarcinoma of the pancreas. Proceedings—American Society of Clinical Oncology. 2001;20(abstract no. 608) [Google Scholar]
- 22.Tobita K, Kijima H, Dowaki S, et al. Epidermal growth factor receptor expression in human pancreatic cancer: significance for liver metastasis. International Journal of Molecular Medicine. 2003;11(3):305–309. [PubMed] [Google Scholar]
- 23.Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the national cancer institute of Canada clinical trials group. Journal of Clinical Oncology. 2007;25(15):1960–1966. doi: 10.1200/JCO.2006.07.9525. [DOI] [PubMed] [Google Scholar]
- 24.Xiong HQ, Rosenberg A, LoBuglio A, et al. Cetuximab, a monoclonal antibody targeting the epidermal growth factor receptor, in combination with gemcitabine for advanced pancreatic cancer: a multicenter phase II trial. Journal of Clinical Oncology. 2004;22(13):2610–2616. doi: 10.1200/JCO.2004.12.040. [DOI] [PubMed] [Google Scholar]
- 25.Philip PA, Benedetti J, Corless CL, et al. Phase III study comparing gemcitabine plus cetuximab versus gemcitabine in patients with advanced pancreatic adenocarcinoma: Southwest oncology group-directed intergroup trial S0205. Journal of Clinical Oncology. 2010;28(22):3605–3610. doi: 10.1200/JCO.2009.25.7550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim GP, Foster NR, Salim M, et al. Randomized phase II trial of panitumumab, erlotinib, and gemcitabine (PGE) versus erlotinib-gemcitabine (GE) in patients with untreated, metastatic pancreatic adenocarcinoma. Journal of Clinical Oncology. 2011;29(supplement, abstract no. 4030) [Google Scholar]
- 27.Seo Y, Baba H, Fukuda T, Takashima M, Sugimachi K. High expression of vascular endothelial growth factor is associated with liver metastasis and a poor prognosis for patients with ductal pancreatic adenocarcinoma. Cancer. 2000;88(10):2239–2245. doi: 10.1002/(sici)1097-0142(20000515)88:10<2239::aid-cncr6>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 28.Kindler HL, Niedzwiecki D, Hollis D, et al. Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: phase III trial of the cancer and leukemia group B (CALGB 80303) Journal of Clinical Oncology. 2010;28(22):3617–3622. doi: 10.1200/JCO.2010.28.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Cutsem E, Vervenne WL, Bennouna J, et al. Phase III trial of bevacizumab in combination with gemcitabine and erlotinib in patients with metastatic pancreatic cancer. Journal of Clinical Oncology. 2009;27(13):2231–2237. doi: 10.1200/JCO.2008.20.0238. [DOI] [PubMed] [Google Scholar]
- 30.Kindler HL, Ioka T, Richel DJ, et al. Axitinib plus gemcitabine versus placebo plus gemcitabine in patients with advanced pancreatic adenocarcinoma: a double-blind randomised phase 3 study. The Lancet Oncology. 2011;12(3):256–262. doi: 10.1016/S1470-2045(11)70004-3. [DOI] [PubMed] [Google Scholar]
- 31.Riess H, et al. Double-blind, placebo-controlled randomized phase III trial of aflibercept (A) plus gemcitabine (G) versus placebo (P) plus gemcitabine (G) in patients with metastatic pancreatic cancer: final results. Proceedings of the European Society for Medical Oncology's 12th World Congress on Gastrointestinal Cancer; 2010; Barcelona, Spain. [Google Scholar]
- 32.Goncalves A, Gilabert M, François E, et al. BAYPAN study: a double-blind phase III randomized trial comparing gemcitabine plus sorafenib and gemcitabine plus placebo in patients with advanced pancreatic cancer. Annals of Oncology. 2012;23(11):2799–2805. doi: 10.1093/annonc/mds135. [DOI] [PubMed] [Google Scholar]
- 33.Erkan M, Reiser-Erkan C, Michalski CW, Kleeff J. Tumor microenvironment and progression of pancreatic cancer. Experimental Oncology. 2010;32(3):128–131. [PubMed] [Google Scholar]
- 34.Von Hoff DD, Ramanathan RK, Borad MJ, et al. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: a phase I/II trial. Journal of Clinical Oncology. 2011;29(34):4548–4554. doi: 10.1200/JCO.2011.36.5742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bergmann U, Funatomi H, Yokoyama M, Beger HG, Korc M. Insulin-like growth factor I overexpression in human pancreatic cancer: evidence for autocrine and paracrine roles. Cancer Research. 1995;55(10):2007–2011. [PubMed] [Google Scholar]
- 36.Freeman JW, Mattingly CA, Strodel WE. Increased tumorigenicity in the human pancreatic cell line MIA PaCa-2 is associated with an aberrant regulation of an IGF-1 autocrine loop and lack of expression of the TGF-β type RII receptor. Journal of Cellular Physiology. 1995;165(1):155–163. doi: 10.1002/jcp.1041650118. [DOI] [PubMed] [Google Scholar]
- 37.Hanks BA, Holtzhausen A, Gimpel P, et al. Effect of the loss of the type III TGFβ receptor during tumor progression on tumor microenvironment: preclinical development of TGFβ inhibition and TGFβ-related biomarkers to enhance immunotherapy efficacy. Journal of Clinical Oncology. 2012;30(supplement, abstract no. 10563) [Google Scholar]
- 38.Wasan HS, Springett GM, Chodkiewicz C, et al. CA 19-9 as a biomarker in advanced pancreatic cancer patients randomised to gemcitabine plus axitinib or gemcitabine alone. British Journal of Cancer. 2009;101(7):1162–1167. doi: 10.1038/sj.bjc.6605243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.García-Manteiga J, Molina-Arcas M, Casado FJ, Mazo A, Pastor-Anglada M. Nucleoside transporter profiles in human pancreatic cancer cells: role of hCNT1 in 2′,2′-difluorodeoxycytidine-induced cytotoxicity. Clinical Cancer Research. 2003;9(13):5000–5008. [PubMed] [Google Scholar]
- 40.Giovannetti E, del Tacca M, Mey V, et al. Transcription analysis of human equilibrative nucleoside transporter-1 predicts survival in pancreas cancer patients treated with gemcitabine. Cancer Research. 2006;66(7):3928–3935. doi: 10.1158/0008-5472.CAN-05-4203. [DOI] [PubMed] [Google Scholar]
- 41.Nakano Y, Tanno S, Koizumi K, et al. Gemcitabine chemoresistance and molecular markers associated with gemcitabine transport and metabolism in human pancreatic cancer cells. British Journal of Cancer. 2007;96(3):457–463. doi: 10.1038/sj.bjc.6603559. [DOI] [PMC free article] [PubMed] [Google Scholar]


