Abstract
Context
The most intense spenders on health services are considerably less healthy—49% report fair or poor health status compared to 15% of the general adult population— and are elderly. Such findings have important implications for addressing national health-care spending because interventions targeting those people who are in poor health could theoretically generate dramatic cost savings. Although the popularity of complementary and alternative medicine (CAM) in the US is well recognized, little is known about the distribution of out-of-pocket expenditures on CAM services.
Objective
This study examined the distribution of out-of-pocket expenditures on CAM health services in the US.
Design
The research team used data from the 2007 National Health Interview Survey to examine the distribution in the US of out-of-pocket expenditures on CAM services and the characteristics of adult (age ≥ 18 years) CAM users (n = 2972) according to spending.
Outcome Measures
Using complex survey-design methods, the research team generated national estimates of expenditures on CAM services and used linear regression adjusted for covariates to determine whether self-reported health status predicted CAM spending.
Results
According to our estimates, in 2007, over 30 million adults reported out-of-pocket expenditures on CAM services, and of these individuals, 7.2 million were heavy CAM spenders with a mean annual expenditure of $1385. The highest quartile of CAM spenders accounted for $10 billion of the $13.9 billion spent nationally on CAM in 2007. Self-reported health status did not differ among groups with differing levels of CAM spending, β̂ = 1.00 (95% CI, 0.8–1.2).
Conclusions
Out-of-pocket spending on CAM is concentrated. Just a quarter of CAM users account for over 70% of all expenditures on CAM services, and health status does not appear to be associated with level of CAM spending.
Research has shown that a small fraction of the US population accounts for the bulk of expenditures on health services.1–3 Among noninstitutionalized US adults, only 30% of all adults account for 90% of all national health-care expenditures, a percentage that has remained relatively stable for the last several decades.3 The most intense spenders on health services are considerably less healthy—49% report fair or poor health status compared to 15% of the general adult population—and are elderly. Research has demonstrated this highly skewed distribution of spending on health services in many populations, such as those with chronic lower back pain,4 the Medicare population,5 and other groups.6,7 Such findings have important implications for addressing national health-care spending because interventions targeting those people who are in poor health could theoretically generate dramatic cost savings; however, whether these patterns exist among users of complementary and alternative medicine (CAM) is unknown.
CAM is a diverse collection of health services that a substantial number of Americans use and includes acupuncture, massage therapy, chiropractic care, natural products, and self-care therapies—such as yoga and herbal medicines and other natural dietary supplements. Conventionally, the definition of CAM does not include the use of vitamins or prayer therapy.8 In 2007 alone, individuals spent $34 billion out-of-pocket on all forms of CAM, including all professional services as well as self-care measures.9 Of the total out-of-pocket expenditures on CAM, US adults spent approximately $12 billion specifically on CAM professional services.
Despite the popularity of CAM and the numerous studies that have demonstrated high spending on CAM in the Uinted States,10–13 little is known about the distribution of expenditures on CAM. Although a skewed distribution of expenditures on CAM may imply a smaller potential for cost containment through its use, information about this distribution would shed light on the market for CAM services and would be valuable for policymakers and payers to consider in determining whether public or private programs should cover CAM services.
Therefore, the research team used data from the 2007 National Health Interview Survey (NHIS) to examine the distribution of expenditures on CAM services.
METHODS
Design and Data Source
The research team used data from the 2007 National Health Interview Survey (NHIS), which is a nationally representative survey of the civilian, noninstitutionalized US population. In 2007, the NHIS included a supplemental questionnaire about adult respondents’ use of 18 different CAM modalities. The 2007 CAM questionnaire is the most current and complete data source available on CAM use and spending in the United States.
The NHIS Adult Core, Family Core, and CAM questionnaires provided the data for this study. Dartmouth College’s Committee for the Protection of Human Subjects determined the study to be exempt from institutional board review.
Sample
The research team examined the data from 23 393 adult (age ≥ 18 years) respondents to the Adult Core questionnaire in 2007 (response rate 78%) of whom 22 783 (97%) answered at least one question on the CAM questionnaire. The NHIS offered this questionnaire in both English and Spanish versions. The questionnaire asked respondents whether they had ever used 18 different CAM modalities, which the National Center for Complementary and Alternative Medicine has classified into five domains: (1) alternative medical systems, such as acupuncture, Ayurveda, or homeopathy; (2) biologically- based therapies, such as chelation therapy (removal of heavy metals from the body) herbals and nonvitamin supplements, and special diets; (3) manipulative- and body-based therapies, with the predominate CAM modalities being chiropractic care and massage therapy; (4) mind-body therapies, such as yoga, tai chi, and qigong; and (5) energy healing therapy. And if they had used these modalities, respondents were asked whether they had done so in the previous 12 months. The research team defined a CAM user as a respondent who reported using any CAM modality (excluding prayer and vitamins) in the previous 12 months.8 The team examined the data for 2970 adult NHIS respondents who reported an expenditure on a CAM service (an expenditure on a visit to a CAM practitioner or a CAM class).
Measures
If respondents reported having seen a practitioner for a CAM modality, the NHIS asked them to estimate the number of visits they had made to CAM practitioners and the number of classes for CAM modalities that they had attended in the previous 12 months, as well as the approximate amount paid per visit or class. The research team used these variables to estimate the total out-of-pocket amount spent on CAM among NHIS respondents.9 The survey did not provide information about the amount that health insurance had covered for the few CAM services that are reimbursable in the United States, such as chiropractic care.
For CAM services, the 2007 NHIS collected information on the number of services consumed in the prior year, based on respondents’ reported number of visits to CAM practitioners in the previous 12 months: 2 to 5 times, 6 to 10 times, 11 to 15 times, 16 to 20 times, and >20 times. As a previous report,9 the research team defined usage for each category to be the midpoint of the categories’ intervals: 3.5, 8, 13, and 18 times, respectively, for the first four intervals. The team used an estimate of 21 visits for those respondents who reported visiting a CAM practitioner more than 20 times. For the estimated number of yoga, tai chi, or qi gong classes that a respondent had attended in the previous 12 months, the research team used the midpoint of the related options: 2 to 11 times per year, 2 to 3 times per month, 2 to 3 times per week, and 4 to 6 times per week. The team then converted the daily, weekly, and monthly values to annual estimates.
With regard to the amount paid per visit to a CAM professional or per class, the research team used each respondent’s estimated amounts, from $0 to $499 (as a continuous measure), and used $500 for reports of $500 or more. The team multiplied this amount for each respective service by the number of visits or classes reported for the year to obtain the respondent’s total expenditures on CAM services.
The research team restricted analyses to those respondents who spent between $1 and $10 000 per year on CAM. Twelve NHIS respondents spent more than $10,000. The team separated the CAM-user population into quartiles based on population estimates. Of the 4114 respondents who reported using a CAM service in the previous 12 months, 1142 respondents had $0 out-of-pocket expenditures (ie, they either received a free consultation or a third-party payer covered the service), and therefore the research team did not include them in the study. The expenditure quartiles were: (1) Quartile 1 (the lowest), with spending between $1 and $86; (2) Quartile 2, with spending between $87 and $209; (3) Quartile 3, with spending between $210 and $519; and (4) Quartile 4 (the highest), with spending between $520 and $10 000 on CAM.
Sociodemographic and Health Status Data
To determine whether CAM users differed based on their expenditure quartile, the research team compared the sociodemographic characteristics—age, sex, race/ethnicity, marital status, US region of residence, health-insurance type, education, and employment status—of low versus high CAM spenders. The team did not include personal earnings due to the large number of missing values in the NHIS data. The team aggregated race and ethnicity into the following categories: (1) Hispanic, (2) non-Hispanic white, (3) non-Hispanic black, and (3) other or multiple races.
Since research has shown that self-reported health status is a strong predictor of health and mortality,14 the research team used respondents’ self-reports as the primary measure of health status and collapsed this variable into two categories: (1) excellent, very good, or good, and (2) fair or poor. The team also reported the percentage of respondents who had any functional limitation (ie, any physical or cognitive limitation). The team used body mass index (BMI) of NHIS respondents in kg/m2 to characterize respondents as obese (BMI ≥ 30) or nonobese.
OUTCOME MEASURES
To generate national estimates, the research team employed complex survey-design methods using the software Stata version 11.1 (College Station, Texas). These complex survey-design methods account for each respondent’s probability of selection and for the NHIS’ sampling methodology using application sampling strata, primary sampling units (PSUs), and person weight variables. The research team used χ2 for categorical variables and a t-test for continuous variables to compare sociodemographic characteristics among quartiles and calculated the P-values comparing respondents with the lowest and highest expenditures on CAM.
Because differences in health status often explain variations in expenditures for health services, the research team used linear regression—adjusted for age, sex, education, marital status, and race/ethnicity—to determine if self-reported health status predicted CAM spending. The team transformed CAM spending into a logarithmic scale and used health status as a dichotomized variable in the linear regression model.
RESULTS
According to the current study’s national estimates, just over 30 million US adults reported an out-of-pocket expenditure for at least one CAM service in 2007. The current study found that 7.4 million US adults were heavy CAM spenders (Table 1) with a mean annual expenditure of $1385 compared to just $45 for the lowest CAM expenditure quartile.
Table 1.
The Characteristics of US Adults that Used Complementary and Alternative Medicine Services by Out-of-pocket
| CAM Expenditure Quartilea
|
P-value for Difference between Lowest and Highest Quartileb | |||||
|---|---|---|---|---|---|---|
| 1 (Lowest) | 2 | 3 (highest) | 4 | |||
| No. of NHIS Respondents (sample) | 728 | 720 | 756 | 754 | ||
| Projected National Estimates | ||||||
| No. of US adults (millions) | 7.7 | 7.4 | 7.8 | 7.4 | ||
| % of US adult population | 3.5 | 3.3 | 3.5 | 3.3 | ||
| US Region (%) | ||||||
| Northeast | 15.7 | 16.3 | 16.6 | 20.7 |
|
< 0.01 |
| Midwest | 32.1 | 28.7 | 27.6 | 17.9 | ||
| South | 25.3 | 26.8 | 31.0 | 28.1 | ||
| West | 26.9 | 28.1 | 24.9 | 33.3 | ||
| Sociodemographic Characteristics | ||||||
| Age (mean) | 43.4 | 44.3 | 44.9 | 46.4 | 0.02 | |
| % female | 56.4 | 61.1 | 62.7 | 68.1 | < 0.01 | |
| Race/Ethnicity (%) | ||||||
| Hispanic | 9.0 | 8.0 | 4.5 | 5.5 |
|
0.03 |
| Non-Hispanic White | 80.4 | 82.0 | 84.5 | 85.6 | ||
| Non-Hispanic Black | 4.5 | 3.4 | 5.0 | 2.6 | ||
| Other or multiple races | 6.1 | 6.5 | 6.0 | 6.2 | ||
| Marital status (%) | ||||||
| married | 62.9 | 62.4 | 64.5 | 55.2 |
|
0.01 |
| not married | 37.1 | 37.6 | 35.5 | 44.8 | ||
| Employment status (%) | ||||||
| unemployed/retired | 26.1 | 23.7 | 24.1 | 24.1 |
|
0.45 |
| employed | 73.9 | 76.3 | 75.9 | 75.9 | ||
| Education (%) | ||||||
| less than high school | 7.8 | 7.7 | 5.9 | 2.3 |
|
< 0.01 |
| high school graduate | 23.8 | 21.5 | 15.4 | 14.9 | ||
| some college or associate’s degree | 35.5 | 34.5 | 30.6 | 31.4 | ||
| bachelor’s or graduate degree | 32.9 | 36.3 | 48.1 | 51.4 | ||
| Health Insurance (%) | ||||||
| private | 37.8 | 32.4 | 32.4 | 35.2 |
|
0.57 |
| public | 44.95 | 1.5 | 50.7 | 48.0 | ||
| uninsured | 17.2 | 16.1 | 16.9 | 16.9 | ||
| Health Status and Health Behaviors | ||||||
| % Fair or Poor Self-reported Health Status | 11.6 | 8.9 | 11.6 | 10.2 | 0.42 | |
| % Obese (body mass index ≥ 30.0kg/m2 | 25.3 | 25.5 | 25.6 | 23.2 | 0.39 | |
| % Any Functional or Cognitive Limitation | 32.5 | 36.4 | 36.2 | 36.9 | 0.14 | |
| % Smokers | 15.7 | 16.6 | 16.1 | 14.7 | 0.65 | |
| % Drinker | 74.6 | 76.7 | 76.8 | 81.1 | 0.01 | |
Total annual expenditures on complementary and alternative medicine (CAM) by quartile: > $0 Q1 < $87; ≥ $87 Q2 < $210; ≥ $210 Q3 < $520; ≥ $520 Q4 ≤ $10 000
t-test used in comparison of means and #2 statistic used in comparison of proportions
The total amount spent on all US CAM services was $13.9 billion: (1) 60% of expenditures on manipulative and body-based therapies, (2) 24% on mind-body therapies, (3) 10% on alternative medical systems, and (4 and 5) 6.4% on biologically-based therapies and energy healing therapy.
Concentration of Expenditures
The research team found spending on CAM to be concentrated (Table 2). The highest expenditure quartile accounted for 72% of the nation’s out-of-pocket expenditures on CAM ($10 billion of the $13.9 billion spent on CAM), while the lowest CAM expenditure quartile accounted for only 2.5%. Examining the distribution of CAM spending more closely, the research team found that the top 10% of CAM spenders accounted for nearly half of all CAM expenditures ($6.6 billion of $13.9 billion) and had a mean annual expenditure of $2392 on CAM. The bottom 50% of CAM spenders accounted for only 10% of CAM expenditures ($1.4 billion of $13.9 billion) and had a mean annual expenditure of $92 on CAM.
Table 2.
The Concentration of Out-of-pocket Expenditures on Complementary and Alternative Medicine (CAM)
| Percentile of CAM User Population | Total Expenditures on CAM (billions of USD) | Percentage of National Expenditures on CAM | Mean Annual Expenditures on CAM (USD) |
|---|---|---|---|
| Top 1% | 1.6 | 11 | 6685 |
| Top 2% | 3.5 | 25 | 5193 |
| Top 5% | 4.6 | 32 | 3432 |
| Top 10% | 6.6 | 48 | 2392 |
| Top 25% | 10.0 | 72 | 1385 |
| Top 50% | 12.5 | 90 | 839 |
| Bottom 50% | 1.4 | 10 | 92 |
Spending Patterns by Expenditure Quartile
The highest quartile spent $10 billion while the lowest spent $348 million on CAM services (Table 3). Across all quartiles, over 50% of expenditures were on manipulative and body-based therapies ($8.3 billion out of $13.9 billion) with virtually all expenditures being on chiropractic or osteopathic manipulation and massage therapy, while biologically-based therapies comprised only 1% to 6% of CAM expenditures across quartiles. The highest quartile spent significantly more on mind-body therapies, with 29% of expenditures in the highest quartile devoted to mind-body therapies compared to only 6% to 11% in the other three quartiles.
Table 3.
Out-of-pocket Expenditures on Specific Complementary and Alternative Medicine (CAM) Modalities by Expenditure Quartile
| Total Out-of-Pocket Expenditures (millions of USD) by CAM Expenditure Quartilea
|
Total | ||||
|---|---|---|---|---|---|
| 1 (Lowest) | 2 | 3 | 4 (Highest) | ||
| Alternatve Medical Systems | 21.4 | 70.1 | 199.0 | 1090.0 | 1380.5 |
| Acupuncture | 11.9 | 48.3 | 132.0 | 631.0 | 823.2 |
| Ayurveda | 0.0 | 0.5 | 3.0 | 15.1 | 18.6 |
| Homeopathy | 1.9 | 4.0 | 19.1 | 140.0 | 165.0 |
| Naturopathy | 0.9 | 3.8 | 29.8 | 236.0 | 270.6 |
| Tradition Healers | 6.7 | 13.4 | 14.6 | 68.3 | 103.0 |
| Biologically-Based Therapies | 10.2 | 20.2 | 24.2 | 576.0 | 630.6 |
| Chelation Therapy | 0.3 | 0.7 | 4.2 | 26.7 | 32.0 |
| Herbals and Non-vitamin Supplements | 8.4 | 19.2 | 15.0 | 524.0 | 566.6 |
| Special Diets | 1.5 | 0.4 | 5.0 | 25.1 | 32.0 |
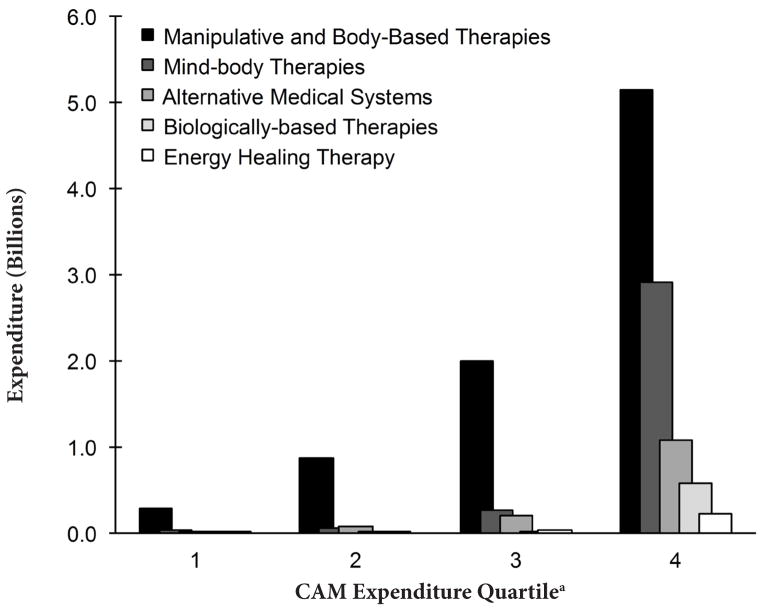
The lowest quartile spent $283 million on manipulative- and body-based therapies, $31.4 million on mind-body therapies, $21.4 million on alternative medical systems, $10.2 million on biologically-based therapies, and only $2.8 million on energy healing therapy. The highest quartile spent $5.2 billion on manipulative and body-based therapies, $2.9 billion on mind-body therapies, $1.1 billion on alternative medical systems, $576 million on biologically-based therapies, and $224 million on energy healing therapy (Figure 1 and Table 3). Expenditures on all specific CAM modalities increased from Quartile 1 to Quartile 4, except for special diets, biofeedback, and hypnosis, which decreased from Quartile 1 (lowest) to Quartile 2.
Figure 1.
Out-of-pocket Expenditures on Complementary and Alternative Medicine Domains by Expenditure Quartile
a>$0 Q1 <$87; ≥$87 Q2 <$210; ≥$210 Q3 <$520; ≥$520 Q4 ≤$10 000
Characteristics of CAM Users by Quartile
Adults in the highest quartile were more likely to reside in the Northeast or the West and less likely to reside in the Midwest as compared to those in the other three quartiles, P-value < .01 (Table 1). Those in the highest quartile were more likely to be older, female, non-Hispanic white, unmarried, and more educated. The research team did not find statistically significant differences in employment status or health insurance across quartiles.
The team found little difference in health status and behavior measures across quartiles; for instance, 10.2% of the highest quartile reported a fair or poor health status compared to 11.6% in the lowest quartile (P-value = .42). Similarly, the research team found little difference in obesity status, in number of individuals with limitations, and in smoking status when comparing lowest and highest quartiles as well; however, those in the highest quartile were more likely to report consuming alcohol (P-value = .01).
In the team’s multiple linear regression model, self-reported health status was not associated with CAM spending (β̂ = 1.00 (95% CI, 0.8–1.2) after adjustment for age, gender, education, marital status, and race/ethnicity.
DISCUSSION
The research team found that individuals in the highest quartile spent considerably more on CAM services than those in the lowest quartile: 72% of all out-of-pocket CAM expenditures were by the highest spenders, while the lowest CAM spenders accounted for just 2.5% of national expenditures. Considering that the 7.2 million adults in the highest quartile spent $10 billion out-of-pocket on CAM, the team anticipated that these individuals might differ in health status when compared to lower spenders. Specifically, the team hypothesized that a lower health status might explain the larger consumption of CAM health services. The finding that health status did not differ based on CAM spending was unanticipated.
The team’s finding that differences in health status did not account for a high concentration of expenditures on CAM services is somewhat divergent from previous studies of the distribution of spending on conventional medical services, such as studies that found that a poorer health status explained the larger expenditures of the high-spending groups.1–3 Therefore, consumer behaviors other than illness management, such as health promotion and illness prevention, may explain the very high CAM expenditures of a few individuals.15,16 Of course, another factor to consider is differences in access to CAM services, which likely vary geographically.
Many CAM users prefer CAM and some evidence exists that patient treatment preference alone may improve health outcomes.17,18 In addition, the current study suggests that CAM users, as one collective group, are relatively homogenous, at least when it comes to health measures. Research has shown that CAM users, as compared to nonusers, are healthier and more active overall, and the current study adds the information by demonstrating that little variation in health status exists among CAM users according to level of spending. 15
It is apparent that a sizeable group of Americans use these services, and the public demand for CAM continues to be strong. Although total expenditures on CAM are small when compared to the $2.6 trillion spent on traditional medicine,19 it is impressive since these expenditures are out-of-pocket. The research team estimates that over 30 million US adults in 2007 had an out-of-pocket expenditure on a CAM service; this amount is lower than Nahin et al’s previous report,9 because the current study’s analyses did not include users with $0 out-of-pocket expenditures; for example, free consultations or CAM services that third-party payers covered.
Limitations
This study has several limitations. First, the NHIS data are self-reported and collected retrospectively; these limitations are inherent to survey-based work. Therefore, errors may exist, especially in cases where the questionnaires asked respondents to recall their use of health-care services up to 12 months ago. The health-status measures were also self-reported, and therefore, medical or psychological conditions may affect them. Second, nonresponse is a potential limitation of the data that the current study used; however, in 2007, the adult response rate was excellent (78% for the Adult Core), and of these adult respondents, 97% completed the CAM supplemental questionnaire. Lastly, the research team based its estimates of CAM spending on the amount spent out-of-pocket on CAM services and neglects expenditures on CAM by private and governmental sources; nevertheless, with the exception of chiropractic care20 and osteopathic medicine, most spending on CAM is out-of-pocket.9
CONCLUSION
As US health-care reform proceeds, important health-policy decisions pertaining to cost containment reside on the horizon. In light of the strong demand for US CAM services, the field needs to develop a better understanding of spending patterns on CAM services to inform policymakers’ decisions in their consideration of CAM services during reform efforts regarding national health care. The current study has demonstrated that out-of-pocket expenditures on CAM are concentrated and that, among CAM spenders, expenditures are not associated with differences in health status. The field needs future studies to understand better the potential long-term impacts of CAM expenditures on population health.
Footnotes
Author Disclosure Statement: Award Number 1K01AT006162 from the National Center for Complementary and Alternative Medicine supported Matthew Davis’s work on this study. The views expressed herein do not necessarily represent the official views of the National Center for Complementary and Alternative Medicine or the National Institutes of Health.
References
- 1.Berk ML, Monheit AC, Hagan MN. How the U.S. spent its health care dollar: 1929–1980. Health Aff (Millwood) 1988;7(4):46–60. doi: 10.1377/hlthaff.7.4.46. [DOI] [PubMed] [Google Scholar]
- 2.Berk ML, Monheit AC. The concentration of health expenditures: an update. Health Aff (Millwood) 1992;11(4):145–149. doi: 10.1377/hlthaff.11.4.145. [DOI] [PubMed] [Google Scholar]
- 3.Berk ML, Monheit AC. The concentration of health care expenditures, revisited. Health Aff (Millwood) 2001;20(2):9–18. doi: 10.1377/hlthaff.20.2.9. [DOI] [PubMed] [Google Scholar]
- 4.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976) 2004;29(1):79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 5.Riley GF. Long-term trends in the concentration of Medicare spending. Health Aff (Millwood) 2007;26(3):808–816. doi: 10.1377/hlthaff.26.3.808. [DOI] [PubMed] [Google Scholar]
- 6.Lin PJ, Biddle AK, Ganguly R, Kaufer DI, Maciejewski ML. The concentration and persistence of health care expenditures and prescription drug expenditures in Medicare beneficiaries with Alzheimer disease and related dementias. Med Care. 2009;47(11):1174–1179. doi: 10.1097/MLR.0b013e3181b69fc1. [DOI] [PubMed] [Google Scholar]
- 7.Bitton R. The economic burden of osteoarthritis. Am J Manag Care. 2009;15(8 suppl):S230–S235. [PubMed] [Google Scholar]
- 8.Kaptchuk TJ, Eisenberg DM. Varieties of healing, II: a taxonomy of unconventional healing practices. Ann Intern Med. 2001;135(3):196–204. doi: 10.7326/0003-4819-135-3-200108070-00012. [DOI] [PubMed] [Google Scholar]
- 9.Nahin RL, Barnes PM, Stussman BJ, Bloom B. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. Natl Health Stat Report. 2009;(18):1–14. [PubMed] [Google Scholar]
- 10.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;(12):1–23. [PubMed] [Google Scholar]
- 11.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;(343):1–19. [PubMed] [Google Scholar]
- 12.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280(18):1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 13.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States: prevalence, costs, and patterns of use. N Engl J Med. 1993;328(4):246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 14.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question: a meta-analysis. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis MA, West AN, Weeks WB, Sirovich BE. Health behaviors and utilization among users of complementary and alternative medicine for treatment versus health promotion. Health Serv Res. 2011;46(5):1402–1416. doi: 10.1111/j.1475-6773.2011.01270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279(19):1548–1553. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 17.Moffett JK, Torgerson D, Bell-Syer S, et al. Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. BMJ. 1999;319(7205):279–283. doi: 10.1136/bmj.319.7205.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sherman KJ, Cherkin DC, Ichikawa L, et al. Treatment expectations and preferences as predictors of outcome of acupuncture for chronic back pain. Spine (Phila Pa 1976) 2010;35(15):1471–1477. doi: 10.1097/BRS.0b013e3181c2a8d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin AB, Lassman D, Washington B, Catlin A National Health Expenditure Accounts Team. Growth in US health spending remained slow in 2010; health share of gross domestic product was unchanged from 2009. Health Aff (Millwood) 2012;31(1):208–219. doi: 10.1377/hlthaff.2011.1135. [DOI] [PubMed] [Google Scholar]
- 20.Davis MA, Sirovich BE, Weeks WB. Utilization and expenditures on chiropractic care in the United States from 1997 to 2006. Health Serv Res. 2010;45(3):748–761. doi: 10.1111/j.1475-6773.2009.01067.x. [DOI] [PMC free article] [PubMed] [Google Scholar]