Abstract
Objective
This study determined whether high maternal prepregnancy body mass index (BMI) and/or excess gestational weight gain (GWG) is associated with reduced breastfeeding duration and earlier formula supplementation.
Study Design
A prospective longitudinal cohort of postpartum women (n=718), who were a subset of a larger randomized trial, was followed for 6 months postdelivery. We evaluated the relationship between BMI or BMI/GWG groups and timing of breastfeeding cessation and introduction of formula using Kaplan–Meier curves and log-rank tests. Then, we used multivariable Cox proportional hazards models to evaluate the relationship between BMI and BMI/GWG on these breastfeeding outcomes after controlling for potential confounding variables.
Results
The expected relationships between high BMI and high BMI/GWG and poor breastfeeding outcomes were observed in Kaplan–Meier curves. However, after adjusting for relevant maternal and infant covariates in the Cox models, the differences became nonsignificant. Prepregnancy BMI category was not statistically associated with breastfeeding duration (p=0.06) or timing of formula introduction (p=0.15). Similarly, BMI and GWG in combination were not associated with duration (p=0.33) or timing of formula introduction (p=0.18). Mothers' intended breastfeeding duration and rating of the importance of breastfeeding remained the only significant modifiable predictors of breastfeeding outcomes in the final models.
Conclusions
Maternal BMI and GWG were not significantly associated with breastfeeding outcomes after adjusting for confounding variables. Mothers' plans for breastfeeding duration and the importance mothers assign to breastfeeding remain the optimal intervention points for lengthening breastfeeding duration and reducing formula supplementation.
Introduction
According to the latest Centers for Disease Control and Prevention Breastfeeding Report Card, the United States continues to fall short of Healthy People 2020 goals1 for breastfeeding duration and exclusivity.2 One proposed explanation for the failure to achieve these goals is that the recent epidemic of obesity in women of childbearing years3 has had a negative impact on women's ability to initiate and sustain exclusive breastfeeding.4,5 Studies across various populations and countries confirm an association between prepregnancy maternal obesity and shorter duration of breastfeeding.6,7
A related phenomenon is the development of overweight or obesity during pregnancy from excess gestational weight gain (GWG). Considering that overweight and obese women are more likely to exceed the Institute of Medicine's GWG recommendations than are normal weight women8 and that GWG is independently associated with decreased breastfeeding duration,9–11 it is challenging both statistically and biologically to discern the unique and potentially additive contributions of prepregnancy body mass index (BMI) and GWG to breastfeeding outcomes.
The purpose of this study was to determine the contributions of maternal prepregnancy BMI to breastfeeding duration and timing of formula introduction, both with and without consideration of GWG. We followed a midsized prospective cohort of breastfeeding mother–infant dyads from birth to 6 months. Based on prior literature, we hypothesized that mothers with both elevated prepregnancy BMI and excess GWG would breastfeed for a shorter period of time and introduce formula earlier compared with mothers with a recommended (healthy) prepregnancy BMI and appropriate GWG.
Subjects and Methods
Study design and subject recruitment
These data were collected as part of the Nurses for Infants Through Teaching and Assessment after the NurserY (NITTANY) Study, a randomized intervention study to compare the effectiveness of two models of care for reducing unplanned healthcare utilization of “well” mothers and infants in the weeks following delivery.12 The study compared the standard medical model of care (outpatient office model) with a model with a single home nurse visit as the initial outpatient encounter after discharge. The Human Subjects Protection Office of the Penn State College of Medicine approved the study. We registered with www.clinicaltrials.gov prior to the enrollment of the first participants.
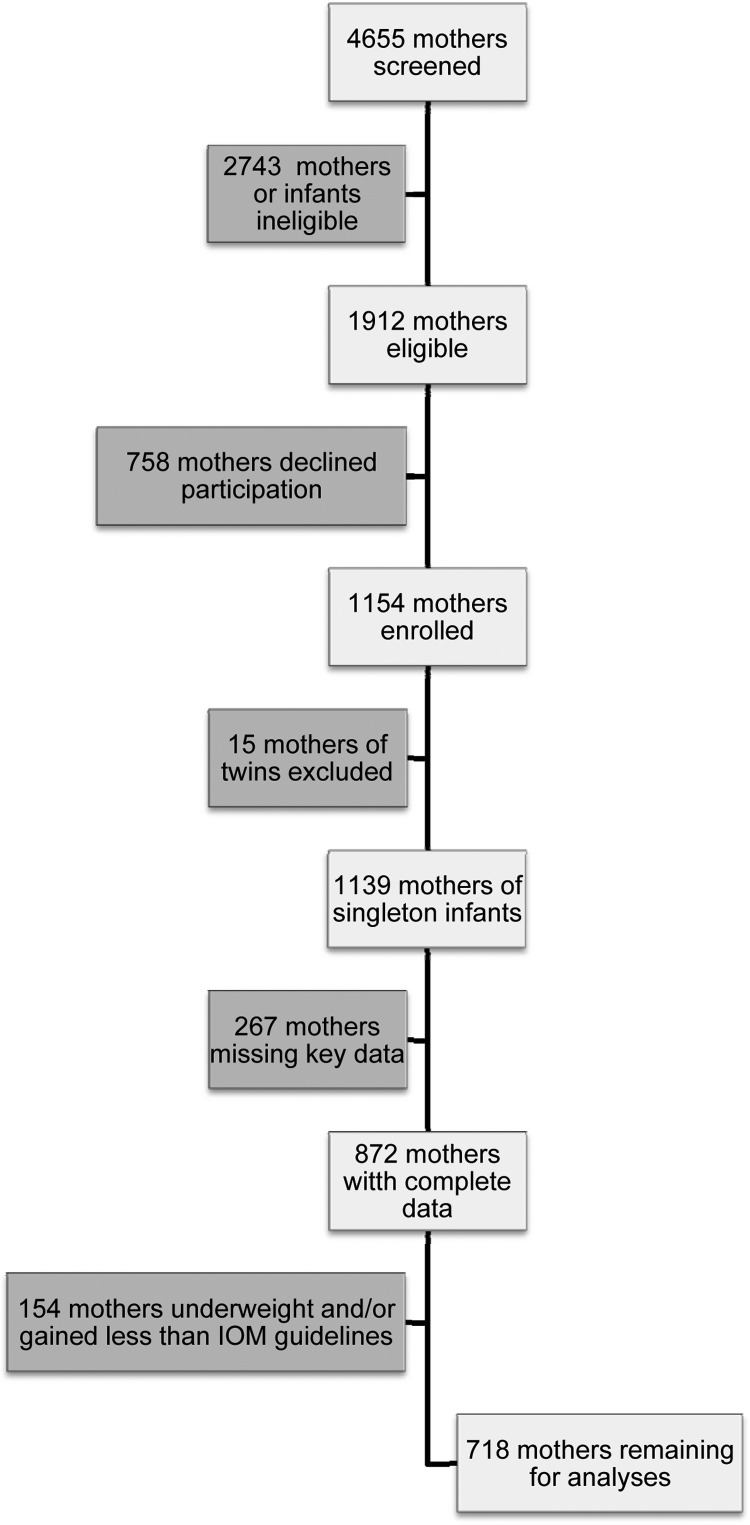
All newborn deliveries at the Penn State Milton S. Hershey Medical Center (Hershey, PA) between September 12, 2006 and August 1, 2009 were screened for study inclusion (n=4,655). As shown in the subject flow diagram (Fig. 1), 2,743 (59%) of mothers were ineligible as they were not breastfeeding, did not speak English, did not expect a regular length of stay after delivery, had higher order multiples, or had a serious, chronic health condition and/or their infant was born at less than 34 weeks of gestation or had health problems that complicated the newborn hospital stay (e.g., severe jaundice). Of the 1,912 eligible subjects, 758 (40%) declined to participate. For this secondary data analysis, 15 twin births were excluded (the Institute of Medicine did not include formal gestational weight gain guidelines for mothers of multiples8), and 267 were missing key data (179 were missing BMI or GWG data, and 88 had no follow-up data beyond baseline), leaving a subsample of 872 mothers for statistical analyses. Prior to starting the study, the research team completed a power analysis based on the ability to detect a difference between a standard medical model of care and a single nurse home visit model of care with a primary outcome of health care utilization in the first 14 days of infant life. For this secondary data analysis, the sample size was predetermined by the number of mothers who met our criteria from the original study pool.
FIG. 1.
Flow diagram for determination of final sample. IOM, Institute of Medicine.
Maternal prepregnancy BMI and GWG were calculated from maternal height, prepregnancy weight, and admission weight, which were extracted from the mother's medical chart. Mothers' prepregnancy BMI was classified according to the Centers for Disease Control and Prevention definitions for underweight (<18.5 kg/m2), normal weight (18.5 to <25 kg/m2), overweight (25 to <30 kg/m2), and obese (≥30 kg/m2).13 Then, their total GWG was compared with the 2009 Institute of Medicine GWG guidelines for underweight (12–18 kg), normal weight (11.5–16 kg), overweight (7–11.5 kg), and obese (5–9 kg) women.8 Mothers were classified as gaining less, more, or within the recommended range for their prepregnancy BMI weight status category. In total, 154 mothers were classified either as underweight and/or gaining less GWG than Institute of Medicine recommendations for their prepregnancy BMI. They were removed from the final data set as our primary research questions related to maternal overweight/obesity and excess GWG, leading to a sample size of 718 mothers for the data presented herein.
After enrollment and during the maternity stay, mothers were randomly assigned to one of the two study arms with stratification for delivery type. Follow-up data were collected via phone interviews at 15–18 days (median, 15 days; range, 8–33 days), 2 months (median, 63 days; range, 55–95 days), and 6 months (median, 183 days; range, 174–224 days) after the baby's birth. As each study arm was randomized, all BMI/GWG groups contained similar numbers of women in each arm (p=0.17), and the two arms were collapsed for these analyses.
Outcome variables
All breastfeeding questions were taken from the Infant Feeding Practices Study II Neonatal Questionnaire (for newborn and day of life 15–18 interviews) and Infant Month 2 Questionnaire (for the 2- and 6-month interviews).14 Breastfeeding duration, defined as the time from birth until the mother completely stopped breastfeeding, was obtained through self-report from mothers during the follow-up phone interviews at 15–18 days, 2 months, and 6 months after the baby's birth. If mothers reported that they had ceased breastfeeding, they were asked the age of the infant in days, weeks, or months when they completely stopped breastfeeding. Breastfeeding duration data were censored at the final study visit (approximately 6 months) or at the last recorded follow-up visit.
Time to formula use was defined as the time from birth until formula was introduced to the infant's diet. This information was obtained through self-report of mothers during the follow-up phone interviews if mothers reported using formula. One exception to this coding was for mothers who provided formula during their hospital stay to address a feeding problem but then reported providing 100% breastmilk at the 2-week follow-up phone call. Of the 278 mothers who introduced formula at the hospital, 39 (14%) reported exclusively breastfeeding at the 2-week follow-up. Their time to formula use was defined as the time from birth until formula was re-introduced to the diet after the 2-week follow-up call. Time to formula use data were censored at the final study visit (approximately 6 months) or at the last recorded follow-up visit.
Covariates
During the postpartum hospital stay, mothers were asked about their intended duration of breastfeeding and their rating of the importance of breastfeeding using questions from the Infant Feeding Practices Study II Neonatal Questionnaire.14 Information on other covariates considered in previous studies such as maternal characteristics (age, race, ethnicity, education, marital status, employment, enrollment in the Women, Infants and Children supplemental nutrition program, number of previous pregnancies, delivery method, smoking during pregnancy) and infant gestational age was gathered during the postpartum hospital stay.
Statistical analysis
The final sample of 718 mothers was stratified two ways. For comparison by prepregnancy BMI, mothers were stratified into three groups: normal BMI (Normal) (n=399), overweight (Overweight) (n=186), or obese (Obese) (n=133). As current Institute of Medicine GWG guidelines are a function of prepregnancy BMI, GWG cannot be interpreted independently from BMI. Hence, we also stratified the sample into five separate groups for each BMI/GWG combination in the analysis, as opposed to a factorial approach in which each factor is independently considered along with their interaction. The five groups included Normal/Recommended (NR) (n=162), Overweight-Obese/Recommended (OOR) (n=58), Normal/More (NM) (n=237), Overweight/More (OWM) (n=156), and Obese/More (OBM) (n=105). Overweight and obese mothers gaining within the recommended GWG guidelines were combined to form one group to obtain an adequate sample size for analysis.
We evaluated the relationship between BMI or BMI/GWG groups and timing of breastfeeding cessation and introduction of formula using Kaplan–Meier curves and log-rank tests. Then, we used multivariable Cox proportional hazards models to evaluate the relationship between BMI and BMI/GWG on these breastfeeding outcomes after controlling for potential confounding variables; only complete cases (n=672 [94%]) were used. Schoenfeld residuals were inspected to verify proportional hazards assumptions.
Results
Stratified samples
Table 1 shows the characteristics of mothers and infants stratified by BMI/GWG group. For the entire sample, there were few missing data; data were missing for three or fewer mothers in all covariates except for employment status (n=13) and planned breastfeeding duration (n=25).
Table 1.
Characteristics of Mothers and Their Infants Grouped by Body Mass Index Category and Gestational Weight Gain
| |
|
Group |
|
||||
|---|---|---|---|---|---|---|---|
| Variable | Total sample (n=718) | NR (n=162) | OOR (n=58) | NM (n=237) | OWM (n=156) | OBM (n=105) | p value |
| Prepregnancy BMI (kg/m2) | 25.9±5.8 | 21.9±1.8 | 32.5±6.7 | 22.1±1.8 | 17.0±1.4 | 35.3±4.2 | <0.01 |
| GWG (kg) | 16.6±6.1 | 13.4±1.3 | 8.0±1.7 | 20.4±4.1 | 17.7±7.2 | 15.9±6.4 | <0.01 |
| Age (years) | 28.7±5.5 | 29.5±5.6 | 29.7±5.5 | 28.3±5.4 | 28.5±5.6 | 28.4±5.6 | 0.14 |
| Parity | 0.10 | ||||||
| 0 | 51.4 | 50.6 | 36.2 | 56.1 | 52.6 | 51.4 | |
| 1 | 32.4 | 32.1 | 41.4 | 32.1 | 26.9 | 26.9 | |
| ≥2 | 16.8 | 17.3 | 22.3 | 11.8 | 20.6 | 19.2 | |
| Vaginal delivery (%) | 67.1 | 77.2 | 60.3 | 68.8 | 65.4 | 54.3 | <0.01 |
| Married (%) | 78.5 | 84.0 | 81.0 | 78.0 | 76.8 | 72.1 | 0.27 |
| Education (%) | <0.01 | ||||||
| <High school | 2.5 | 2.5 | 0 | 1.3 | 3.2 | 5.7 | |
| High school | 15.6 | 8.6 | 15.5 | 20.0 | 14.1 | 19.0 | |
| Some college or more | 81.8 | 88.9 | 84.5 | 78.7 | 82.8 | 75.3 | |
| Race (%) | 0.08 | ||||||
| White | 90.6 | 88.1 | 89.7 | 92.4 | 91.7 | 89.5 | |
| Asian | 3.4 | 7.5 | 1.7 | 1.7 | 3.2 | 1.9 | |
| Black | 5.0 | 3.8 | 3.8 | 3.8 | 4.5 | 8.6 | |
| Other | 1.0 | 0.6 | 0 | 2.1 | 0 | 0 | |
| Hispanic/Latino ethnicity (%) | 5.9 | 6.2 | 8.6 | 5.9 | 5.8 | 3.8 | 0.80 |
| WIC enrolled (%) | 17.0 | 14.2 | 15.5 | 16.0 | 16.0 | 25.7 | 0.14 |
| Smoked during pregnancy (%) | 8.8 | 4.3 | 3.4 | 11.0 | 10.3 | 11.4 | 0.06 |
| Plans to work after delivery (%) | 78.7 | 73.1 | 80.7 | 78.8 | 78.6 | 86.4 | 0.15 |
| Planned breastfeeding duration (months) | 7.9±4.4 | 8.2±4.6 | 8.3±4.1 | 8.0±4.3 | 7.2±4.2 | 8.3±5.0 | 0.28 |
| Maternal rating of breastfeeding importance (%) | 0.14 | ||||||
| Not very important | 0.3 | 0 | 0 | 0.8 | 0 | 0 | |
| Somewhat important | 7.9 | 7.4 | 3.4 | 5.1 | 11.5 | 12.4 | |
| Very important | 43.9 | 43.8 | 55.2 | 43.9 | 39.1 | 44.8 | |
| Extremely important | 47.9 | 48.8 | 41.4 | 50.2 | 49.4 | 42.9 | |
| Infant birth weight (kg) | 3.46±0.48 | 3.33±0.52 | 3.41±0.45 | 3.52±0.48 | 3.53±0.42 | 3.47±0.51 | <0.01 |
| Gestational age (weeks) | 39.3±1.2 | 39.2±1.2 | 38.9±1.4 | 39.5±1.2 | 39.3±1.2 | 39.2±1.3 | <0.01 |
| Using formula prior to hospital discharge (%) | 30.9 | 23.5 | 29.3 | 27.0 | 37.8 | 41.9 | <0.001 |
| Milk came in later than 4 days postdelivery (%) | 16.9 | 13.0 | 10.3 | 16.5 | 17.4 | 26.7 | 0.03 |
| Maternal report of (%) | |||||||
| Milk “took too long to come in” | 21.7 | 21.0 | 17.5 | 21.6 | 22.7 | 23.8 | 0.91 |
| “Pain while breastfeeding in the first 2 weeks” | 63.6 | 73.5 | 60.3 | 65.0 | 59.4 | 53.3 | 0.01 |
| “Baby had trouble sucking or latching on” | 52.5 | 50.6 | 54.4 | 54.7 | 50.0 | 53.3 | 0.88 |
| “Nipples were sore, cracked, or bleeding” | 60.4 | 69.8 | 50.9 | 65.3 | 53.9 | 49.5 | 0.001 |
Groups were named by prepregnancy body mass index (BMI) category (normal, overweight, or obese)/adherence to Institute of Medicine gestational weight gain (GWG) guidelines (recommended weight gain, more), leading to the following group names: Normal/Recommended (NR), Overweight-Obese/Recommended (OOR), Normal/More (NM), Overweight/More (OWM), and Obese/More (OBM).
In univariable Cox proportional hazards models all covariates considered except race and gestational age were significantly associated with breastfeeding duration.
WIC, Women, Infants and Children supplemental nutrition program.
Breastfeeding duration
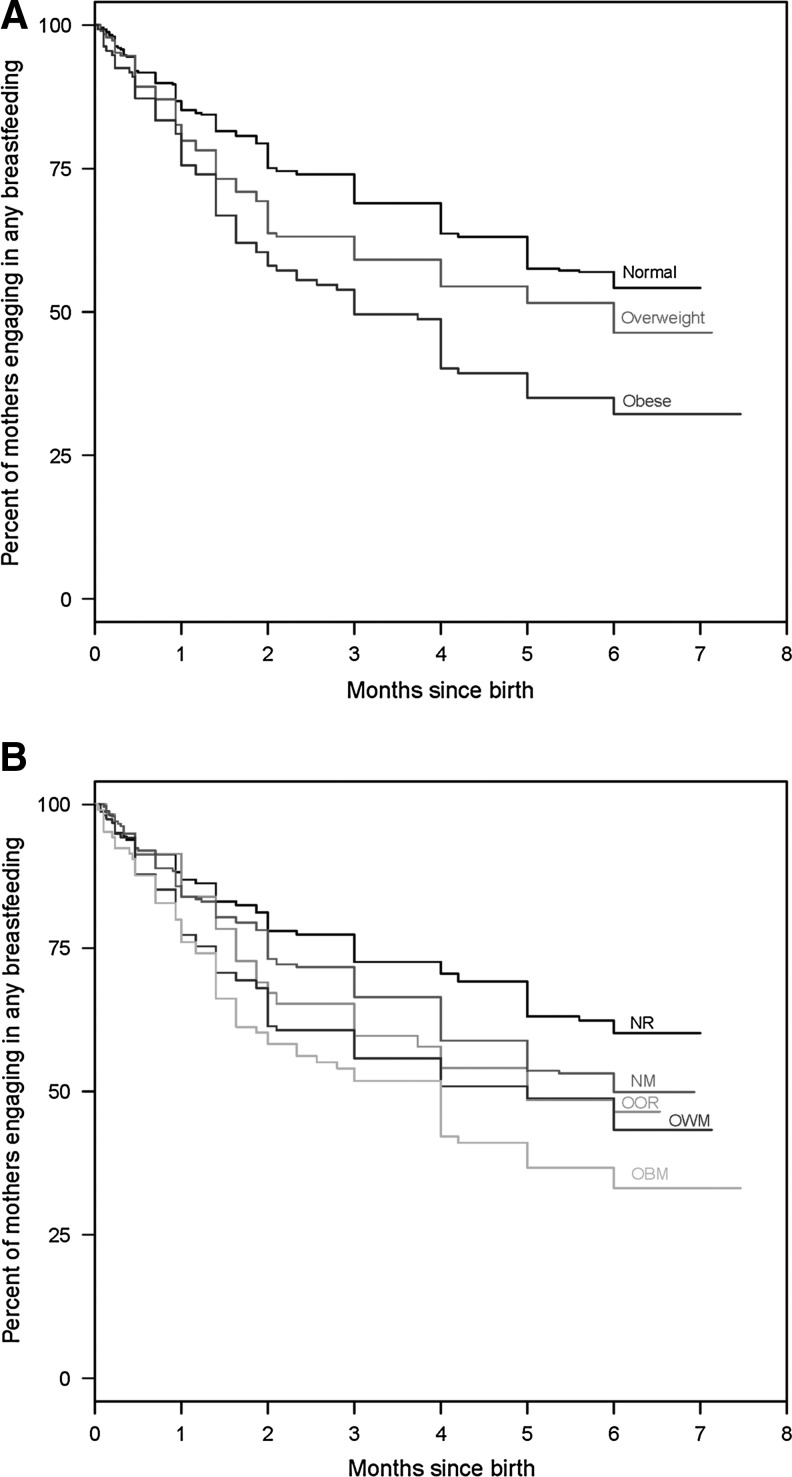
In the total sample, 349 mothers (49%) stopped breastfeeding completely at some point during the 6 months of observation. Figure 2 shows the Kaplan–Meier curves for time to breastfeeding cessation or, alternatively, the percentage of mothers still engaging in any breastfeeding across the 6 months of observation when the groups are stratified by BMI (Fig. 2A) or both BMI and GWG (Fig. 2B). Log-rank test results for between-group differences in breastfeeding duration by BMI and BMI/GWG groups were calculated (see supplementary Tables S1 and S2 at www.liebertpub.com/bfm). In brief, obese mothers engaged in any breastfeeding for a shorter duration than normal BMI mothers (p<0.001) and overweight mothers (p=0.02). When groups were examined by both BMI and GWG, OWM and OBM mothers breastfed for a shorter duration than NR mothers (p=0.002 and p<0.001, respectively), and OBM mothers had shorter breastfeeding duration than NM mothers (p=0.002).
FIG. 2.
Kaplan–Meier curves for breastfeeding duration stratified by (A) body mass index (BMI) or (B) BMI/gestational weight gain (GWG) group. BMI groups include Normal, Overweight, or Obese. BMI/adherence to Institute of Medicine GWG guideline groups include Normal/Recommended (NR), Overweight-Obese/Recommended (OOR), Normal/More (NM), Overweight/More (OWM), and Obese/More (OBM).
The results of the multivariable Cox proportional hazards models for breastfeeding cessation fit separately using BMI or BMI/GWG group are shown in Table 2. In the final multivariate models for both BMI and BMI/GWG, only education, marital status, planned breastfeeding duration, and maternal rating of breastfeeding importance remained significant contributors to the timing of breastfeeding cessation.
Table 2.
Hazard Ratios from Cox Models for Breastfeeding Duration (Cessation) Fit Separately Using Body Mass Index or Body Mass Index/Gestational Weight Gain and Other Covariates
|
Breastfeeding cessation model including | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
BMI group |
BMI/GWG group |
||||||||
| Variable | HR | (95% CI) | p value | Overall p value | Variable | HR | (95% CI) | p value | Overall p value |
| BMI group | 0.06 | BMI/GWG group | 0.33 | ||||||
| Healthy | Ref | NR | Ref | ||||||
| Overweight | 1.15 | (0.88–1.51) | 0.30 | OOR | 1.40 | (0.88–2.22) | 0.16 | ||
| Obese | 1.43 | (1.06–1.93) | 0.02 | NM | 1.06 | (0.76–1.48) | 0.74 | ||
| OWM | 1.22 | (0.86–1.74) | 0.27 | ||||||
| OBM | 1.40 | (0.94–2.08) | 0.09 | ||||||
| Age, 1 year increase | 1.02 | (0.98–1.03) | 0.87 | 1.00 | (0.98–1.03) | 0.86 | |||
| Parity, 1 child increase | 0.91 | (0.79–1.05) | 0.20 | 0.91 | (0.79–1.06) | 0.22 | |||
| Delivery | |||||||||
| Cesarean | 1.23 | (0.96–1.57) | 0.10 | 1.23 | (0.96–1.58) | 0.10 | |||
| Vaginal | Ref | Ref | |||||||
| Marital status | <0.001 | <0.001 | |||||||
| Single | 1.73 | (1.20–2.50) | 0.004 | 1.71 | (1.19–2.47) | 0.004 | |||
| Other | 2.41 | (1.65–3.53) | <0.001 | 2.34 | (1.61–3.42) | <0.001 | |||
| Married | Ref | Ref | |||||||
| Education | <0.001 | <0.001 | |||||||
| <High school graduate | 3.35 | (1.49–7.54) | 0.003 | 3.52 | (1.57–7.93) | 0.002 | |||
| High school graduate | 3.08 | (1.93–4.92) | <0.001 | 3.11 | (1.95–4.97) | <0.001 | |||
| Some college | 2.43 | (1.64–3.59) | <0.001 | 2.47 | (1.67–3.65) | <0.001 | |||
| College graduate | 1.27 | (0.89–1.81) | 0.19 | 1.27 | (0.89–1.82) | 0.19 | |||
| Postgraduate training | Ref | Ref | |||||||
| Race | |||||||||
| White | 1.39 | (0.91–2.13) | 0.13 | 1.39 | (0.90–2.13) | 0.14 | |||
| Other | Ref | Ref | |||||||
| Ethnicity | |||||||||
| Hispanic | 1.21 | (0.79–1.86) | 0.39 | 1.22 | (0.79–1.87) | 0.37 | |||
| Non-Hispanic | Ref | Ref | |||||||
| Enrolled in WIC | |||||||||
| Yes | 1.14 | (0.82–1.59) | 0.44 | 1.15 | (0.82–1.60) | 0.41 | |||
| No | Ref | Ref | |||||||
| Smoked during pregnancy | |||||||||
| Yes | 0.78 | (0.53–1.14) | 0.20 | 0.78 | (0.53–1.14) | 0.20 | |||
| No | Ref | Ref | |||||||
| Plan to work after delivery | |||||||||
| Yes | 0.96 | (0.70–1.32) | 0.80 | 0.97 | (0.70–1.33) | 0.83 | |||
| No | Ref | Ref | |||||||
| Planned breastfeeding duration, 1 month increase | 0.89 | (0.86–0.92) | <0.001 | 0.89 | (0.86–0.92) | <0.001 | |||
| Breastfeeding importance | <0.001 | <0.001 | |||||||
| Somewhat important | 2.20 | (1.49–3.24) | <0.001 | 2.23 | (1.51–3.29) | <0.001 | |||
| Very important | 1.45 | (1.14–1.86) | 0.003 | 1.46 | (1.14–1.88) | 0.003 | |||
| Extremely important | Ref | Ref | |||||||
| Gestational age, 1 week increase | 0.98 | (0.89–1.07) | 0.58 | 0.98 | (0.89–1.07) | 0.58 | |||
Groups were named by prepregnancy body mass index (BMI) category (normal, overweight, or obese)/adherence to Institute of Medicine gestational weight gain (GWG) guidelines (recommended weight gain, more), leading to the following group names: Normal/Recommended (NR), Overweight-Obese/Recommended (OOR), Normal/More (NM), Overweight/More (OWM), and Obese/More (OBM).
In univariable Cox models for time to formula use, all covariates were significant predictors.
CI, confidence interval; HR, hazard ratio; Ref, reference; WIC, Women, Infants and Children supplemental nutrition program.
Time to formula use
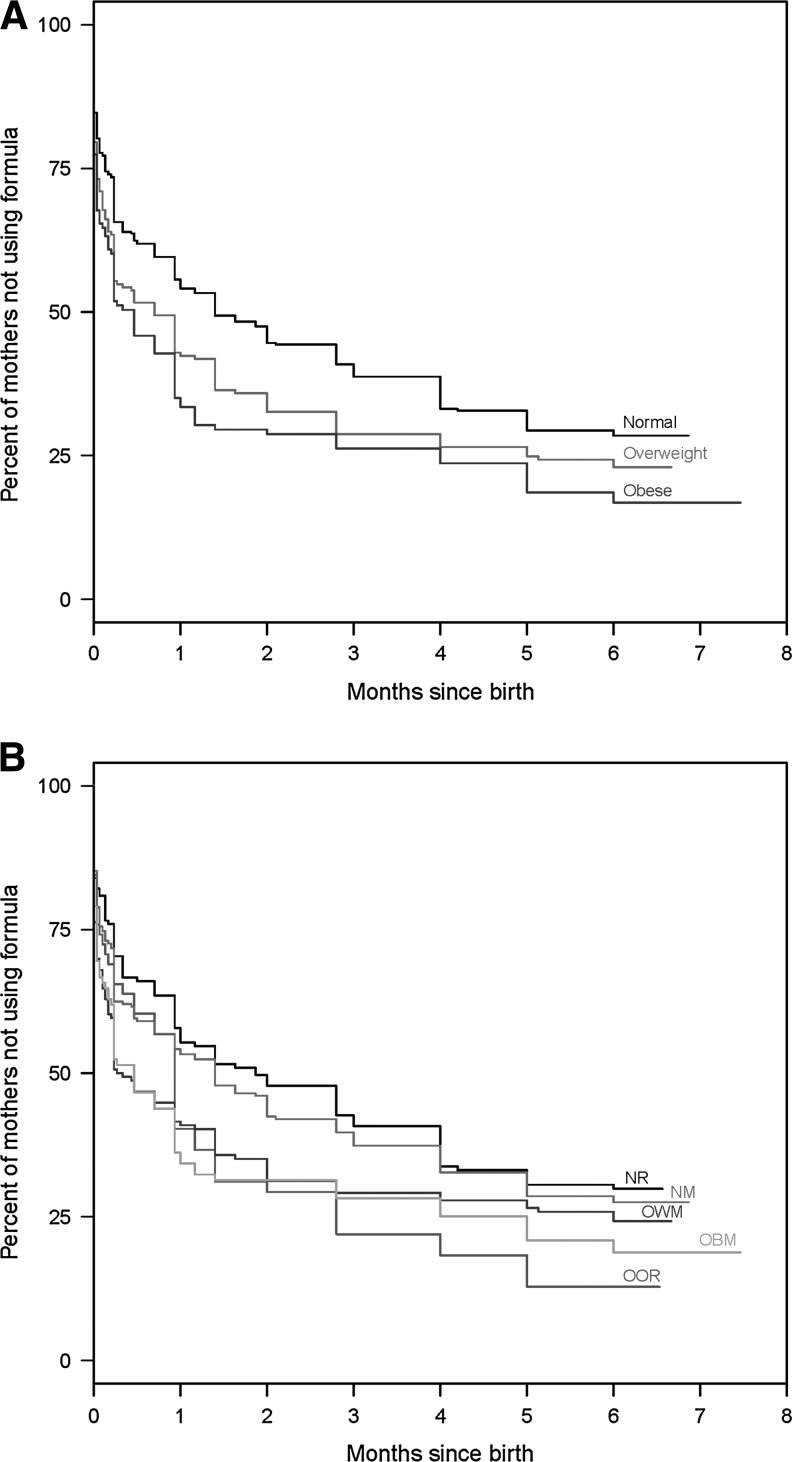
In the total sample, 222 mothers (31%) introduced formula prior to discharge from the hospital, and only 32 (14% of those introducing formula) returned to 100% breastmilk feeding by 2 weeks. Of the total sample, 44% had introduced formula by week 2 and 62% by month 6. From the Kaplan–Meier estimate, the median time to formula use for mothers who introduced formula during the 6-month study was 3–4 weeks. Figure 3 shows the Kaplan–Meier curves for the percentage of mothers who were not using formula when the groups are stratified by BMI (Fig. 3A) or both BMI and GWG (Fig. 3B). Log-rank test results for between-group differences in breastfeeding duration by BMI and BMI/GWG groups were calculated (see supplementary Tables S1 and S2 at www.liebertpub.com/bfm). Compared with normal BMI mothers, obese mothers introduced formula earlier (p=0.02). In addition, mothers in the OOR (p=0.01), OWM (p=0.02), and OBM (p=0.005) groups introduced formula earlier than mothers with normal BMI who stayed within GWG guidelines.
FIG. 3.
Kaplan–Meier curves for time to formula use stratified by (A) BMI or (B) BMI/GWG group. BMI groups include Normal, Overweight, or Obese. BMI/adherence to Institute of Medicine GWG guideline groups include Normal/Recommended (NR), Overweight-Obese/Recommended (OOR), Normal/More (NM), Overweight/More (OWM), and Obese/More (OBM).
Table 3 contains the results of multivariable Cox proportional hazards models for formula introduction fit separately using BMI or BMI/GWG group. In the final multivariate models for both BMI and BMI/GWG, only education, race, plans to return to work, planned breastfeeding duration, and maternal rating of breastfeeding importance remained significant contributors to the timing of formula introduction.
Table 3.
Hazard Ratios from Cox Models for Time to Formula Use Fit Separately Using Body Mass Index or Body Mass Index/Gestational Weight Gain and Other Covariates
|
Formula introduction model including | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| |
BMI group |
|
BMI/GWG group |
||||||
| Variable | HR | 95% CI | p value | Overall p value | Variable | HR | 95% CI | p value | Overall p value |
| BMI | 0.15 | BMI/GWG | 0.18 | ||||||
| Healthy | Ref | NR | Ref | ||||||
| Overweight | 1.19 | (0.96–1.47) | 0.11 | OOR | 1.36 | (0.96–1.93) | 0.09 | ||
| Obese | 1.22 | (0.95–1.55) | 0.12 | NM | 0.91 | (0.71–1.18) | 0.48 | ||
| OWM | 1.11 | (0.85–1.47) | 0.44 | ||||||
| OBM | 1.04 | (0.76–1.43) | 0.79 | ||||||
| Age, 1 year increase | 1.01 | (0.99–1.03) | 0.29 | 1.01 | (0.99–1.03) | 0.31 | |||
| Parity, 1 child increase | 0.95 | (0.84–1.07) | 0.40 | 0.95 | (0.84–1.07) | 0.41 | |||
| Delivery | |||||||||
| Cesarean | 1.12 | (0.93–1.37) | 0.24 | 1.14 | (0.94–1.39) | 0.18 | |||
| Vaginal | Ref | Ref | |||||||
| Marital status | 0.11 | 0.11 | |||||||
| Single | 1.28 | (0.91–1.81) | 0.15 | 1.29 | (0.92–1.82) | 0.15 | |||
| Other | 1.40 | (1.00–1.96) | 0.05 | 1.38 | (0.99–1.94) | 0.06 | |||
| Married | Ref | Ref | |||||||
| Education | 0.04 | 0.03 | |||||||
| <High school graduate | 1.82 | (0.91–3.64) | 0.09 | 1.90 | (0.95–3.80) | 0.07 | |||
| High school graduate | 1.66 | (1.16–2.39) | 0.006 | 1.69 | (1.17–2.43) | 0.005 | |||
| Some college | 1.36 | (1.01–1.85) | 0.04 | 1.39 | (1.03–1.88) | 0.03 | |||
| College graduate | 1.05 | (1.05–1.34) | 0.72 | 1.04 | (0.81–1.34) | 0.76 | |||
| Postgraduate training | Ref | Ref | |||||||
| Race | |||||||||
| White | 0.69 | (0.51–0.94) | 0.02 | 0.69 | (0.51–0.94) | 0.02 | |||
| Other | Ref | Ref | |||||||
| Ethnicity | |||||||||
| Hispanic | 1.15 | (0.79–1.67) | 0.46 | 1.11 | (0.77–1.62) | 0.57 | |||
| Non-Hispanic | Ref | Ref | |||||||
| Enrolled in WIC | |||||||||
| Yes | 1.33 | (0.99–1.79) | 0.05 | 1.33 | (0.99-1.78) | 0.06 | |||
| No | Ref | Ref | |||||||
| Smoked during pregnancy | |||||||||
| Yes | 1.00 | (0.71–1.40) | 0.99 | 1.02 | (0.73–1.42) | 0.93 | |||
| No | Ref | Ref | |||||||
| Plan to work after delivery | |||||||||
| Yes | 1.31 | (1.01–1.69) | 0.04 | 1.32 | (1.02–1.71) | 0.03 | |||
| No | Ref | Ref | |||||||
| Planned breastfeeding duration, 1 month increase | 0.91 | (0.89–0.94) | <0.001 | 0.91 | (0.89–0.94) | <0.001 | |||
| Breastfeeding importance | <0.001 | <0.001 | |||||||
| Somewhat important | 2.56 | (1.79–3.65) | <0.001 | 2.61 | (1.83–3.74) | <0.001 | |||
| Very important | 1.33 | (1.09–1.61) | 0.005 | 1.33 | (1.09-1.61) | 0.005 | |||
| Extremely important | Ref | Ref | |||||||
| Gestational age, 1 week increase | 0.96 | (0.90–1.04) | 0.31 | 0.97 | (0.90–1.04) | 0.38 | |||
Groups were named by prepregnancy body mass index (BMI) category (normal, overweight, or obese)/adherence to Institute of Medicine gestational weight gain (GWG) guidelines (recommended weight gain, more), leading to the following group names: Normal/Recommended (NR), Overweight-Obese/Recommended (OOR), Normal/More (NM), Overweight/More (OWM), and Obese/More (OBM).
CI, confidence interval; HR, hazard ratio; Ref, reference; WIC, Women, Infants and Children supplemental nutrition program.
Discussion
In our study, we observed that prepregnancy BMI, alone and in combination with GWG, was associated with reduced breastfeeding duration and earlier introduction of formula. However, these relationships disappeared after we adjusted for important covariates. After controlling for confounding variables in multivariate models, the only statistically significant predictors of breastfeeding duration included education, marital status, planned breastfeeding duration, and rating of breastfeeding importance. Similarly, the only significant predictors of time to formula supplementation were education, race, plans to return to work, planned breastfeeding duration, and rating of breastfeeding importance. Thus, while overweight and obese women remain an important population to target for breastfeeding education, important modifiable risk factors for deleterious breastfeeding outcomes—the mother's own plans for how long she will breastfeed and her perceptions of the importance of breastfeeding to her parenting goals—apply to all women.
Although high prepregnancy BMI and excess GWG clearly present a variety of health risks to both mother and infant, their effects on breastfeeding outcomes remain unclear. Some, but not all, studies to date reported a deleterious effect of maternal prepregnancy overweight or obesity6,7 and GWG9–11,15 on duration of breastfeeding. Of note is that studies from Denmark, Russia, and Greece, as well as studies of specific racial groups in the United States, have not reported associations between breastfeeding duration and maternal overweight and obesity.10,15,16 Researchers have hypothesized that one source of the inconsistent findings may be the number and type of confounders that are controlled for when performing statistical analyses.10,11 Our multivariable Cox models indicated that planned breastfeeding duration and importance of breastfeeding, evaluated while mothers were still in the hospital, were among the statistically important factors in determining breastfeeding outcomes. These findings are consistent with those of Hilson et al.,17 who first documented that the relationship between maternal prepregnancy weight status and poor breastfeeding outcomes is modified by psychosocial factors such as planned duration and importance of breastfeeding. Thus, some of the inconsistency in this area of research may be due to whether women's breastfeeding plans and intentions are considered.6,7
This study extends the current literature by evaluating the impact of BMI and BMI/GWG groups on timing of formula introduction. Although the U.S. National Immunization Survey18 has monitored introduction of formula before 2 days, 3 months, and 6 months of life since 2003, we are not aware of any published studies that have evaluated the impact of maternal prepregnancy BMI and/or GWG on formula introduction. Human and animal studies suggest that maternal overweight and obesity may result in delays in lactogenesis II (onset of copious milk production),6,19 anatomical differences that contribute to problems latching and transferring milk,17 and problems with milk production.20,21 Thus, it is reasonable to suspect that a high prepregnancy BMI and/or excess GWG would be associated with earlier introduction of formula. Although that hypothesis was not supported by our data, future studies should test this hypothesis in other populations.
Given the mixed findings in the area, it is important to outline the limitations of this study and the extent to which the results can be extrapolated. This study is the result of secondary data analysis of an intervention study from Central Pennsylvania. The initial sample size was determined based on power analysis for the primary outcome (healthcare utilization); for this secondary data analysis, the sample size was predetermined by the number of mothers who met our criteria from the original study pool. The original eligible subject pool consisted of only “well” newborns and mothers who were intending to breastfeed. Thus, the results will not necessarily apply to mothers or babies who were screened out of our study—those who had unexpected medical complications during their hospital stay (e.g., uterine hemorrhaging, endometritis, hyperbilirubinemia requiring phototherapy, etc.), mothers with serious chronic illnesses affecting medical care, or families with characteristics that interfered with the primary study objectives (e.g., non–English-speaking family, living outside of the nurse home visit coverage area, baby placed for adoption). Approximately 40% of eligible mothers declined to participate. We cannot rule out the possibility that inclusion of these mothers in the study would have altered the results. We also have not accounted for every possible covariate that may affect breastfeeding outcomes, such as time to first feeding following delivery or prior lactation experiences.
The pool of subjects selected for this analysis included only mothers classified as normal, overweight, or obese prior to pregnancy and those with GWG within or above the Institute of Medicine guidelines. Our decision to eliminate underweight and low GWG mothers from the analyses was based on a belief that these mothers could be fundamentally different in other psychological or physiological variables that were not measured in the study but could potentially impact lactation success (e.g., high rates of physical activity or food insecurity). We also only included mothers of singleton infants; thus, the study results may not apply to mothers of multiples. Our subject pool was largely composed of non-Hispanic white, well-educated mothers who intended to work at some point following delivery. About half of the mothers were delivering their first child. More than 30% of mothers were using formula prior to discharge, which is higher than the Centers for Disease Control and Prevention's Breastfeeding Report Card rates of formula introduction before 2 days2 for Pennsylvania (18%) and the nation (25%), but considerably better than national average for in-hospital supplementation (56%) reported in the Ross Mothers Survey.22 The rate of formula use in this sample, especially the rate of formula use prior to discharge from the hospital stay, could mask any effects of maternal weight patterns on formula introduction. In contrast, about 51% of our mothers were still breastfeeding at 6 months, which is higher than the rates for Pennsylvania (38%) and the United States (45%). Our results, in part, may differ from other similar studies in the United States because of the participant pool. Future studies should systematically investigate the impact of participant pool characteristics and covariates included in statistical models on both breastfeeding duration and formula introduction across all levels of prepregnancy BMI and GWG.
Conclusions
Although high prepregnancy BMI and excess GWG present a variety of health risks to both the mother and infant, they are not independent risk factors for breastfeeding cessation or introduction of formula in populations similar to the ones studied here. Overweight and obese mothers may have special needs for assistance with breastfeeding,4 but healthcare providers should address women's plans for breastfeeding and the importance they assign to it during prenatal and postpartum visits regardless of maternal BMI or GWG. The final multivariable models suggest that the potentially modifiable factors of mothers' plans for breastfeeding duration and the importance mothers assign to breastfeeding remain the optimal intervention points for improving breastfeeding duration and reducing formula supplementation.
Supplementary Material
Acknowledgments
This project was supported by grant R40 MC 06630 from the Maternal Child Health Bureau (Title V, Social Security Act), Health Resources and Services Administration, Department of Health and Human Services.
Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Disease Control and Prevention. Healthy People 2020 Objectives for the Nation. 2012. www.cdc.gov/breastfeeding/policy/hp2010.htm?topicId=26. [Jan 20;2012 ]. www.cdc.gov/breastfeeding/policy/hp2010.htm?topicId=26
- 2.Centers for Disease Control and Prevention. Breastfeeding Report Card 2011, United States: Outcome Indicators. 2012. www.cdc.gov/breastfeeding/data/reportcard2.htm. [Jan 20;2012 ]. www.cdc.gov/breastfeeding/data/reportcard2.htm
- 3.Flegal KM. Carroll MD. Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 4.Jevitt C. Hernandez I. Groer M. Lactation complicated by overweight and obesity: Supporting the mother and newborn. J Midwifery Womens Health. 2007;52:606–613. doi: 10.1016/j.jmwh.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Lovelady CA. Is maternal obesity a cause of poor lactation performance? Nutr Rev. 2005;63:352–355. doi: 10.1111/j.1753-4887.2005.tb00113.x. [DOI] [PubMed] [Google Scholar]
- 6.Amir LH. Donath S. A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy Childbirth. 2007;7:9. doi: 10.1186/1471-2393-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wojcicki JM. Maternal prepregnancy body mass index and initiation and duration of breastfeeding: A review of the literature. J Womens Health. 2011;20:341–347. doi: 10.1089/jwh.2010.2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institute of Medicine, National Research Council. Weight Gain During Pregnancy: Reexamining the Guidelines. National Academies Press; Washington, DC: 2009. National Research Council. [PubMed] [Google Scholar]
- 9.Hilson JA. Rasmussen KM. Kjolhede CL. Excessive weight gain during pregnancy is associated with earlier termination of breast-feeding among white women. J Nutr. 2006;136:140–146. doi: 10.1093/jn/136.1.140. [DOI] [PubMed] [Google Scholar]
- 10.Manios Y. Grammatikaki E. Kondaki K, et al. The effect of maternal obesity on initiation and duration of breast-feeding in Greece: The GENESIS study. Public Health Nutr. 2009;12:517–524. doi: 10.1017/S1368980008002838. [DOI] [PubMed] [Google Scholar]
- 11.Li R. Jewell S. Grummer-Strawn L. Maternal obesity and breast-feeding practices. Am J Clin Nutr. 2003;77:931–936. doi: 10.1093/ajcn/77.4.931. [DOI] [PubMed] [Google Scholar]
- 12.Paul IM. Beiler JS. Schaefer EW, et al. A randomized trial of single home nursing visits vs office-based care after nursery/maternity discharge: The Nurses for Infants Through Teaching and Assessment After the NurserY (NITTANY) Study. Arch Pediatr Adolesc Med. 2012;166:263–270. doi: 10.1001/archpediatrics.2011.198. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Defining Overweight and Obesity. 2010. www.cdc.gov/obesity/defining.html. [Oct 5;2010 ]. www.cdc.gov/obesity/defining.html
- 14.Centers for Disease Control and Prevention. Infant Feeding Practices Study II Questionnaires. www.cdc.gov/ifps/questionnaires.htm. [Oct 25;2010 ]. www.cdc.gov/ifps/questionnaires.htm
- 15.Baker JL. Michaelsen KF. Sorensen TI, et al. High prepregnant body mass index is associated with early termination of full and any breastfeeding in Danish women. Am J Clin Nutr. 2007;86:404–411. doi: 10.1093/ajcn/86.2.404. [DOI] [PubMed] [Google Scholar]
- 16.Grjibovski AM. Yngve A. Bygren LO, et al. Socio-demographic determinants of initiation and duration of breastfeeding in northwest Russia. Acta Paediatr. 2005;94:588–594. doi: 10.1111/j.1651-2227.2005.tb01944.x. [DOI] [PubMed] [Google Scholar]
- 17.Hilson JA. Rasmussen KM. Kjolhede CL. High prepregnant body mass index is associated with poor lactation outcomes among white, rural women independent of psychosocial and demographic correlates. J Hum Lact. 2004;20:18–29. doi: 10.1177/0890334403261345. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Breastfeeding Among U.S. Children Born 2000–2008, CDC National Immunization Survey. 2012. www.cdc.gov/breastfeeding/data/NIS_data/index.htm. [Jan 20;2012 ]. www.cdc.gov/breastfeeding/data/NIS_data/index.htm
- 19.Nommsen-Rivers LA. Chantry CJ. Peerson JM, et al. Delayed onset of lactogenesis among first-time mothers is related to maternal obesity and factors associated with ineffective breastfeeding. Am J Clin Nutr. 2010;92:574–584. doi: 10.3945/ajcn.2010.29192. [DOI] [PubMed] [Google Scholar]
- 20.Rolls BJ. Rowe EA. Fahrbach SE, et al. Obesity and high energy diets reduce survival and growth rates of rat pups [abstract] Proc Nutr Soc. 1980;39:51A. [PubMed] [Google Scholar]
- 21.Shaw MA. Rasmussen KM. Myers TR. Consumption of a high fat diet impairs reproductive performance in Sprague-Dawley rats. J Nutr. 1997;127:64–69. doi: 10.1093/jn/127.1.64. [DOI] [PubMed] [Google Scholar]
- 22.Ross Products Division. Mothers Survey. Abbott Laboratories; Columbus, OH: 2003. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.