Abstract
Background
Economic disadvantage is associated with depression and suicide. We sought to determine whether economic disadvantage reduces the effectiveness of depression treatments received in primary care.
Methods
We conducted differential-effects analyses of the Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT), a primary care-based randomized, controlled trial for late-life depression and suicidal ideation conducted between 1999 and 2001, which included 514 patients with major depression or clinically significant minor depression.
Results
The intervention effect, defined as change in depressive symptoms from baseline, was stronger among persons reporting financial strain at baseline (differential effect size= −4.5 Hamilton Depression Rating Scale points across the study period; 95% confidence interval = −8.6 to −0.3). We found similar evidence for effect modification by neighborhood poverty, although the intervention effect weakened after the initial 4 months of the trial for participants residing in poor neighborhoods. There was no evidence of substantial differences in the effectiveness of the intervention on suicidal ideation and depression remission by economic disadvantage.
Conclusions
Economic conditions moderated the effectiveness of primary care-based treatment for late-life depression. Financially strained individuals benefitted more from the intervention; we speculate this was because of the enhanced treatment management protocol, which lead to a greater improvement in the care received by these persons. People living in poor neighborhoods experienced only temporary benefit from the intervention. Thus, multiple aspects of economic disadvantage affect depression treatment outcomes; additional work is needed to understand the underlying mechanisms.
Economic disadvantage has been linked with reduced access to, and poorer outcomes of, depression treatments. For example, such disadvantages are associated with prolonged depressive symptoms during the course of depression treatment.1,2 However, it remains unclear whether depression treatments are less effective in the context of social disadvantage. Evidence from observational studies cannot disaggregate the impact of socioeconomic inequalities on the persistence of depressive symptoms from their impact on the effectiveness of depression treatments. For example, community-based studies demonstrate substantial socioeconomic inequalities in the initial onset of depression as well as its prognosis.3-5 Therefore, in any treated sample, there are likely to be socioeconomic differences in depression symptom severity at treatment initiation. The persistence of socioeconomic differences during the course of treatment could therefore arise from differences that existed prior to treatment rather than differences in treatment effectiveness. Additionally, underserved groups (including people with lower incomes) may also be less likely to receive depression treatment or, if treated, they may receive inadequate or lower quality treatment for their depression.6-9
A randomized controlled trial is the most rigorous design for causal inference and the strongest design with which to investigate differential effects of treatments because it removes the confounding effects of differential access to treatment and minimizes variation across participants in treatment regimens, compared with observational designs. We therefore conducted an investigation of the impact of economic disadvantage on the effectiveness of an intervention for late-life depression among attendees of primary care practices - the settings in which a substantial portion of depression treatment is provided and where there is greater risk of receiving inadequate treatment.10-13
Methods
Sample
PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial; Clinicaltrials.gov identifier NCT00279682) was a primary-care-based intervention that reduced depressive symptoms and suicidal ideation throughout its 24-month duration,14-17 and conferred a survival advantage that persisted beyond the study’s end date.18 Twenty primary care practices in the metropolitan areas of New York City, Philadelphia, and Pittsburgh were randomized to intervention or usual-care arms between 1999 and 2001.16 The practices were selected to be diverse with respect to type (e.g., academic vs. non-academic) and patient composition.19 The study was approved by the Institutional Review Boards at participating sites, and all participants gave written informed consent.
Patients aged 60 years and above and who had a Mini-Mental State Examination score≥18 were eligible for enrollment into the study. The trial targeted patients with scores >20 on the Center for Epidemiologic Studies Depression scale, or with a history of depression or depression treatment, and also enrolled patients without depression. The participation rate was 66% of all eligible patients, resulting in a total sample size of 1,226, of whom 599 had major or clinically significant minor depression. 599 participants (320 in intervention practices, and 279 in usual-care practices) were in the target population of the intervention (i.e., those with major or clinically significant minor depression at enrollment) and thus eligible for the current study.17
We excluded 85 (14%) participants due to incomplete data on baseline covariates, and therefore include 514 in the current study (269 in intervention practices and 245 in usual-care practices). These persons provided 2,368 observations obtained at baseline and during five follow-up research visits over the course of the trial: 514 at enrollment, 424 at 4 months, 394 at 8 months, 350 at 12 months, 348 at 18 months, and 338 at 24 months (66% of participants).
The intervention addressed two components of depression care: physician knowledge and treatment management.14,16 In practices randomized to the intervention arm, a depression care manager worked with patients and providers to ensure guideline-based provision of depression treatment (e.g., treatment with citalopram or interpersonal psychotherapy) and follow-up care throughout the study period. The care managers monitored patients’ depressive symptoms, treatment adherence, and side effects, and provided follow-up care as needed. In practices randomized to the usual-care arm, participants’ physicians received educational materials regarding late-life depression, written notices of depression diagnoses made at baseline or during follow-up research visits, and contacts made by the investigators when the study personnel detected a significant suicide risk.
Measures
Depressive symptoms were assessed at each research visit using the Hamilton Depression Rating Scale, with higher scores indicating more severe depressive symptoms.20 In addition to analyzing mean Hamilton Depression Rating Scale scores over the study period, we investigated remission of depressive symptoms, defined as scoring ≤7.21 Suicidal ideation at each visit was assessed using both the Hamilton Depression Rating Scale and the Scale for Suicidal Ideation.22 Suicidal ideation was coded as present based on a score≥1 on either the Scale for Suicidal Ideation or the suicide item of the Hamilton Depression Rating Scale.
The primary social determinant of differential treatment response was participants’ financial strain at enrollment (defined as participant response of “Can’t make ends meet” to a question about current financial situation). Financial strain reflects a person’s income relative to their needs. In a prior observational analysis of data from this intervention trial, financial strain was the factor that most strongly predicted depressive symptoms and suicidal ideation in the full study sample, irrespective of treatment condition.23 Additionally, we considered neighborhood poverty as a potential determinant of treatment response. It was defined as living in a high- (>40%), medium- (20-40%), or low- (<20%) poverty census tract; the differential-effects analyses combined participants in high- and medium-poverty census tracts.24 We geocoded participants’ address to the United States 2000 decennial census tract codes, from which we were able to determine the poverty rate in each participant’s neighborhood. Baseline control variables included educational attainment (college education vs. less than college), race-ethnicity (white vs. non-white), sex, age (60-75 vs. 75+ years), study site (Pittsburgh, Philadelphia, or New York) and the Charlson Comorbidity Index—a measure of participant medical burden.25
Statistical analysis
Differential treatment outcomes are assessed by conducting tests of statistical interaction between hypothesized moderators of treatment outcomes and intervention status.26,27 Because the intervention effect on change in outcomes during follow-up in this trial is determined by the interaction between intervention status and time,14,16,17 the differential treatment effect is evaluated by the three-way interaction among social factors at baseline, intervention status, and time (e.g., financial strain × intervention × time).
We used mixed-effects regression models to evaluate differential intervention effects on mean levels of depressive symptoms (using linear regression) and the likelihood of suicidal ideation and depression remission (using logistic regression). Analyses of depressive symptoms and suicidal ideation included all 6 research visits, whereas the analyses of remission included post-baseline visits only. Subject-specific intercepts were included to account for within-subject variability in treatment outcomes over the course of the study.16 Random effects for primary care practices were not necessary given that the within-practice correlations of depression and suicidal ideation were negligible (e.g., 0.01-0.02).16 The linear random effects models were fitted using PROC MIXED, and the logistic random effects models were fitted using PROC GLIMMIX (using maximum likelihood estimation with adaptive quadrature), in SAS v9.2 (SAS Institute, Cary, NC).
First, we conducted descriptive analyses of the social determinants of treatment effectiveness. For each endpoint, we calculated treatment outcomes (means for Hamilton Depression Rating Scale scores, proportions for suicidal ideation and depression remission) across visits in the intervention and usual-care arms of the trial separately for participants with and without financial strain at baseline, and again, separately for participants who resided in medium or high vs. low poverty census tracts.
Next we determined the best-fitting model for trends in depressive symptoms over the 2-year study period. The trial was not originally designed to detect differential treatment effects, and therefore we considered it advantageous, in terms of increased statistical power, to use the most parsimonious approach possible. We evaluated a “saturated” model that included terms representing the mean response at each visit in both treatment arms (in addition to baseline control variables), and reduced-form models with fewer parameters. In the saturated model, the (dichotomous) baseline covariate × intervention × time interaction term involves 5 coefficients, requiring 5 degrees of freedom (one for each post-baseline assessment). A reduced model would yield a more powerful test of the baseline covariate × intervention × time interaction.28 For example, if mean Hamilton Depression Rating Scale scores declined in a linear fashion over the course of the trial, then only a linear term for time would be required, and the baseline covariate × intervention × time interaction would reduce to a single coefficient and a more powerful, 1 degree-of-freedom test.
The best-fitting model for Hamilton Depression Rating Scale scores over the course of the trial was a piecewise linear model with a knot at month 4 (eTable 3, http://links.lww.com/EDE/A622). This model divides the study period into two parts and fits a linear trend within each part. This is consistent with descriptive analyses in which levels of depressive symptoms and suicidal ideation declined most sharply in the initial months of the trial, and then declined in a linear, though less steep fashion, during the remaining months. For example, in the analyses involving financial strain, the parameters in the model include two terms for the effects of time in the study (representing the period between baseline and month 4, and the period between months 4 and 24), intervention status, financial strain at baseline, and all two-way and three-way interaction terms between time, intervention status, and financial strain (the parameterization of this model is shown in the eAppendix, http://links.lww.com/EDE/A622). The test for a differential treatment effect is given by a joint test of the significance of the 2 coefficients of the 3-way interactions involving time, intervention status, and financial strain.
Finally, we conducted analyses to determine whether the findings were robust to biases caused by participant attrition. We explored the distributions of baseline covariates among study participants present and missing at each follow-up visit, fitted a logistic mixed-effects model predicting attrition during the study period to assess associations between baseline measures and non-participation, and reanalyzed the data using two statistical techniques to account for participant attrition: inverse-probability weighting and multiple imputation (see eTable 5 for further details, http://links.lww.com/EDE/A622).
Results
The demographic characteristics of participants in the analysis sample at baseline are shown in Table 1, separately for the intervention and usual-care arms of the trial. Overall, 13% of participants (n=66) reported financial strain at enrollment into the study (12% in the intervention arm, 14% in the usual-care arm). Participants reporting financial strain had higher mean Hamilton Depression Rating Scale scores (19.2 [SD = 6.2] vs. 17.7 [5.9]), and a higher likelihood of suicidal ideation (55% vs. 37%). Financial strain was reported by 12% of participants at the conclusion of the study and its distribution was almost the same as at baseline.
Table 1. Baseline sociodemographic characteristics of participants randomized in the Prevention of Suicide in Primary Care Elderly: Collaborative Trial.a.
| Intervention No. (%) |
Usual Care No. (%) |
|
|---|---|---|
| Financial Strain | ||
| Yes | 31 (12) | 35 (14) |
| No | 238 (89) | 210 (86) |
| Census Tract Poverty | ||
| High (>40%) | 15 (6) | 13 (5) |
| Medium (20-40%) | 58 (22) | 72 (29) |
| Low (<20%) | 196 (73) | 160 (65) |
| College Education | ||
| Yes | 95 (35) | 109 (45) |
| No | 174 (65) | 136 (56) |
| Race/ethnicity | ||
| White | 199 (74) | 161 (66) |
| Non-White | 70 (26) | 84 (34) |
| Sex | ||
| Male | 82 (31) | 61 (25) |
| Female | 187 (70) | 184 (75) |
| Age Group | ||
| <75 | 184 (68) | 171 (70) |
| 75+ | 85 (32) | 74 (30) |
Analysis sample includes participants in the trial with clinically significant major or minor depression at enrollment, with complete data on the covariates listed in the table (n=514).
Table 2 presents the intervention effect on mean Hamilton Depression Rating Scale scores for those with and without financial strain, and for those residing in medium/high- and low-poverty census tracts. The intervention effect is given by the difference between the change from baseline in the intervention arm and the change from baseline in the usual-care arm. The final column of Table 2 presents the differential effect of the intervention (i.e., the intervention effect for those with financial strain minus the intervention effect for those without financial strain).
Table 2. Mean Hamilton Depression Rating Scale scores according to study arm (intervention or usual care) and baseline financial strain or census-tract poverty.
| Study Arm |
Intervention effect (Group Difference in Mean Change from Baseline)a Mean (SE) |
Study Arm |
Intervention effect (Group Difference in Mean Change from Baseline)a Mean (SE) |
Differential Effect of the trial interventionb Mean (95% CI) |
|||
|---|---|---|---|---|---|---|---|
| Intervention Mean (SE) |
Usual Care Mean (SE) |
Intervention Mean (SE) |
Usual Care Mean (SE) |
||||
| Financial Strain | |||||||
|
| |||||||
|
Baseline Financial Strain
|
No Baseline Financial Strain
|
||||||
| Baseline | 22.0 (1.3) | 16.7 (1.2) | 18.0 (0.5) | 17.4 (0.5) | |||
| 4 months | 14.5 (1.4) | 15.2 (1.3) | −5.9 (2.6) | 10.5 (0.5) | 12.8 (0.5) | −2.9 (1.0) | −3.1 (−8.5, 2.4) |
| 8 months | 11.7 (1.4) | 12.1 (1.3) | −5.7 (2.6) | 10.1 (0.5) | 11.0 (0.5) | −1.4 (1.0) | −4.3 (−9.8, 1.2) |
| 12 months | 10.2 (1.5) | 12.1 (1.6) | −7.2 (2.8) | 9.6 (0.6) | 10.3 (0.6) | −1.3 (1.0) | −6.0 (−11.8, −0.2) |
| 18 months | 10.0 (1.5) | 11.5 (1.5) | −6.7 (2.7) | 9.2 (0.6) | 9.3 (0.6) | −0.7 (1.0) | −6.1 (−11.8, −0.3) |
| 24 months | 11.9 (1.5) | 10.4 (1.5) | −3.8 (2.8) | 8.7 (0.6) | 9.1 (0.6) | −0.9 (1.1) | −2.9 (−8.7, 2.9) |
| Census Tract Poverty | |||||||
|
Medium or High Census Tract Poverty
|
Low Census Tract Poverty
|
||||||
| Baseline | 18.8 (0.8) | 17.9 (0.8) | 18.3 (0.5) | 17.0 (0.6) | |||
| 4 months | 11.8 (0.9) | 14.3 (0.8) | −3.5 (1.7) | 10.7 (0.6) | 12.6 (0.6) | −3.2 (1.1) | −0.3 (−4.3, 3.6) |
| 8 months | 10.0 (1.0) | 11.7 (0.9) | −2.6 (1.7) | 10.4 (0.6) | 10.8 (0.6) | −1.7 (1.1) | −0.9 (−5.0, 3.1) |
| 12 months | 9.4 (1.0) | 10.3 (0.9) | −1.8 (1.8) | 9.7 (0.6) | 10.6 (0.7) | −2.1 (1.2) | 0.3 (−3.9, 4.5) |
| 18 months | 10.4 (1.0) | 9.5 (0.8) | −0.1 (1.8) | 8.9 (0.6) | 9.6 (0.7) | −2.0 (1.2) | 1.9 (−2.3, 6.0) |
| 24 months | 11.3 (1.1) | 9.0 (0.9) | 1.3 (1.8) | 8.4 (0.6) | 9.4 (0.7) | −2.3 (1.2) | 3.6 (−0.6, 7.8) |
The intervention effect is defined as the intervention minus usual care difference in the change in score from baseline.
Differential effect defined as the intervention effect in the less advantaged group minus the intervention effect in the more advantaged group. Differential effects<0 indicate greater reductions (from baseline) in scores in the less advantaged group than in the more advantaged group.
The unadjusted patterns of mean Hamilton Depression Rating Scale scores during the trial suggest that the intervention was more effective among participants entering the trial under conditions of financial strain. This is shown by differential effects <0, indicating more pronounced changes from baseline in the group with financial strain. For example, between baseline and 4 months, the intervention was associated with a mean reduction of 5.9 points in score among those with financial strain (95% confidence interval [CI]= −11.0 to −0.8), compared with a mean reduction of 2.9 points among those without financial strain (−4.8 to −0.9). The difference between these two estimates (last column of Table 2) is −3.1 (95% CI= −8.5 to 2.4). At months 8, 12, 18, and 24, the differential effects were −4.3, −6.0, −6.1, and −2.9, respectively. Averaged across post-baseline visits, the differential intervention effect at baseline was −4.5 Hamilton Depression Rating Scale points (95% CI= −8.6 to −0.3).
Analyses involving census-tract poverty (lower part of Table 2), reveal a different pattern. Differential effects were essentially zero in the initial follow-up visits, indicating equal effectiveness of the intervention across groups irrespective of the level of census-tract poverty, whereas effects trended toward positive values by the end of the trial. The estimate of the differential intervention effect at month 24 was 3.6 points (95% CI= −0.6 to 7.8). The differential effect averaged across all post-baseline assessments was small (0.9 [-2.1 to 3.9]).
Patterns of differences in the effectiveness of the intervention on the likelihood of suicidal ideation according to financial strain were generally consistent with the patterns for Hamilton Depression Rating Scale scores; however, the confidence intervals surrounding these estimates were very wide, limiting the conclusions that could be drawn (eTable 1, http://links.lww.com/EDE/A622). There were no discernable patterns of differences in the effectiveness of the intervention on the likelihood of suicidal ideation according to census-tract poverty (eTable 1, http://links.lww.com/EDE/A622), or on the likelihood of depression remission according to financial strain or census-tract poverty (eTable 2, http://links.lww.com/EDE/A622).
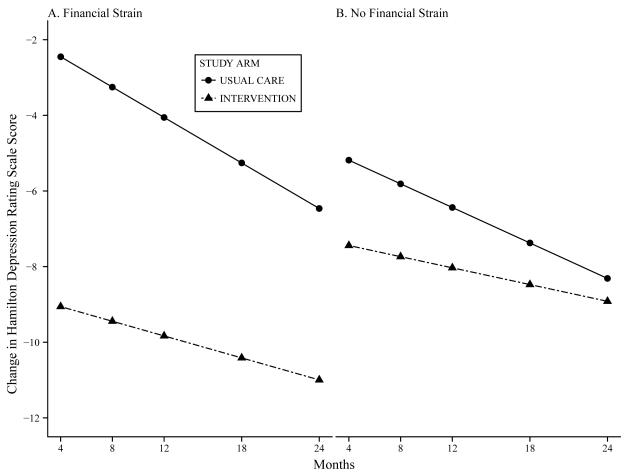
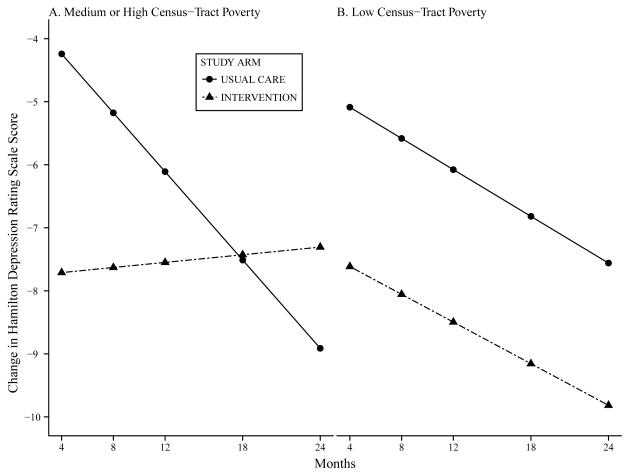
There were two statistically significant differential effects at the α=0.05 level, both in the analyses of mean Hamilton Depression Rating Scale scores: financial strain (P=0.022) and census-tract poverty (P=0.003) (eTable 6, http://links.lww.com/EDE/A622). The latter test would also meet a more stringent significance threshold accounting for the 6 interaction tests conducted (0.05/6=0.008). To interpret the interactions, we used the coefficients from the regression models to generate plots of mean changes in Hamilton Depression Rating Scale scores from baseline, according to study arm and financial strain (Figure 1) or census-tract poverty (Figure 2) (see eTable 5 for the coefficients and 95% CI’s of the 3-way interaction terms, http://links.lww.com/EDE/A622). The results for financial strain demonstrate more pronounced effects of the intervention on Hamilton Depression Rating Scale scores in the financial strain group (Figure 1). This is seen by the larger separation between the lines for the intervention and usual-care arms of the trial among participants reporting financial strain at baseline.
Figure 1.
Estimated changes from baseline in Hamilton Depression Rating Scale scores according to study arm (intervention or usual-care) and financial strain, adjusting for census-tract poverty, educational attainment, race, sex, age, study site, and baseline medical burden.
Figure 2.
Estimated changes from baseline in Hamilton Depression Rating Scale scores according to study arm (intervention or usual-care) and census-tract poverty, adjusting for financial strain, educational attainment, race, sex, age, study site, and baseline medical burden.
The results of the differential-effects analysis involving census-tract poverty, presented in Figure 2, are different from those involving financial strain. Viewing just the results at 4 months, there were no differences in the intervention effects between participants according to their level of census-tract poverty. For participants residing in medium- or high-poverty census tracts, the intervention effect did not persist beyond 4 months. In contrast, the trial led to a continued reduction of depressive symptoms among participants residing in low-poverty census tracts.
We used sensitivity analyses to assess whether the findings were robust to missing data at baseline and non-participation in the follow-up assessments. eFigure 1 (http://links.lww.com/EDE/A622) depicts the distribution of 9 baseline covariates among participants present and absent at each visit. In general the distributions of baseline covariates did not differ by participants’ presence or absence at each visit. In a logistic mixed-effects model predicting missingness during the study period, there were no detectable effects of baseline covariates (eTable 4, http://links.lww.com/EDE/A622). Finally, we refitted the models for differential effects involving financial strain and census-tract poverty in Hamilton Depression Rating Scale scores using inverse-probability weighting and multiple imputation (eTable 5, http://links.lww.com/EDE/A622). The regression coefficients for the 3-way interaction terms from the analyses using all available data presented above and from the two sets of sensitivity analyses were similar, with confidence intervals that covered a similar range.
Discussion
We hypothesized that a primary-care-based intervention for late-life depression would be less effective among economically disadvantaged people. This hypothesis was based on evidence from observational studies indicating substantial social inequalities in treatment outcomes for major depression.2 Our results support this hypothesis in part—in the analyses involving census-tract poverty. We found that the intervention effect attenuated after the initial 4 months of the trial among participants residing in poor neighborhoods. In contrast, in the analyses involving financial strain, the intervention effect was larger in the more socially disadvantaged group. These results are based on tests of the statistical interactions between hypothesized moderators of treatment and intervention status.26,29
Limitations
The trial was not designed to detect subgroup differences.30 In particular, the wide confidence intervals surrounding the estimates of differential treatment effects on suicidal ideation and depression remission limit our ability to draw inferences regarding those outcomes. Due to sample-size limitations our study was also unable to test interactions involving financial strain and census-tract poverty simultaneously. Attrition over the course of the trial may have affected our analyses in several respects. Diminishing numbers of participants over the study period could have biased the results if dropout was non-random. The longitudinal mixed-effects models utilized all observed data, but cannot overcome the problem of systematic differences in dropout rates that are due to unobserved factors. In supplemental analyses, neither financial strain nor census-tract poverty was an important predictor of participation in follow-up assessments (eTable 4, http://links.lww.com/EDE/A622). Accounting for attrition using inverse-probability weights and using multiple imputation did not change our results. However, these methods do not address biases due to attrition caused by unmeasured factors.
Our analyses of differential intervention effects involving financial strain were based on participants’ subjective valuations of their economic circumstances rather than actual financial resources. Prior studies have demonstrated robust associations between perceptions of financial strain and both mental and physical health among older adults.31,32 Additional work is needed to establish the validity of self-reported financial strain, and in particular to examine whether such reports are influenced by mental-health problems. Related to this, work is needed to understand what mechanisms operate at the neighborhood level to underlie associations between neighborhood socioeconomic indicators (here, census-tract poverty) and mental health.33
Lastly, while the intervention effects reported in the full study sample can be interpreted as causal effects, interpretation of interactions with intervention status merit caution. Our results suggest that financial strain and census-tract poverty may indicate subgroups that vary in their responsiveness to a primary care-based intervention for depression. However, the extent to which our results can sustain inferences regarding interventions targeting financial strain or census-tract poverty in addition to depression are contingent on our ability to control for potential confounders.34 Our analyses controlled for baseline demographic variables and baseline medical burden, but cannot exclude confounding by other factors.
Consistency with existing evidence
There is substantial evidence that the social determinants of depression observed in epidemiologic samples are associated with worse depression outcomes among people in treatment. However, much of this evidence does not separate pre-existing depression severity from differential treatment outcomes. For example, Cohen and colleagues have reported a relatively unfavorable course of depression treatment outcomes among older adults residing in lower-income census tracts,1,35,36 and data from primary-care clinics demonstrate social inequalities in the receipt of depression treatment, adequacy of depression treatment, and outcomes of depression treatment.10,12,37-40 Friedman et al. reported that lower educational attainment and minority race/ethnicity were associated with worsened depression during the course of antidepressant treatment.2 And, as discussed above, evidence based on data from primary care clinics demonstrates social disparities in the receipt of depression treatment, adequacy of depression treatment, and outcomes of depression treatment.10,12,37-40
Bao et al. previously investigated education and race differences associated with outcomes of the PROSPECT intervention.41 They reported that less educated people benefitted more from the intervention at the final 2-year assessment. Our analyses, controlling for both of these factors, identified economic conditions as significant modifiers of the intervention, consistent with the demonstrated importance of economic conditions to the mental health of older adults.42 Aside from this trial, there are few studies that have addressed the issue of inqualities in treatment outcomes in the context of a randomized controlled trial,43-45 which provides the strongest design for determining whether treatments for depression work equally well for all groups. For example, Arean et al. investigated the relative effectiveness of a primary care-based intervention for late-life depression according to income, and reported that all income groups benefited equally from the intervention.46 They also reported similar intervention effects for all racial/ethnic groups.47 Their study was of a shorter duration than this one (12 months versus 24 months), and randomized individual patients rather than primary-care practices. The summary of existing evidence is therefore that observational studies demonstrate marked disparities in depression treatment outcomes, whereas results from experimental studies are less consistent. In the current study, the PROSPECT intervention was associated with reduced depressive symptoms for all groups, but to a somewhat weaker degree and for a shorter duration among persons experiencing neighborhood-level economic disadvantage.
Importance of investigating differential treatment outcomes
We endorse arguments for investigating which groups are most (and least) likely to benefit from treatment.27,48 Even though this clinical trial was not designed to detect differential treatment effects, it provided a unique opportunity in which to investigate such differences, given its diverse sample and primary care setting. To be sure, waiting until the analysis stage to initiate such investigations is not the optimal strategy for investigating moderators of treatment.26 Randomizing participants within social strata, and enrolling a sufficient number of participants within each stratum to detect differences between them, would yield more definitive results. In addition, enhanced procedures tailored to the populations under study might be needed to maintain participation throughout the trial across groups.49
The use of stratified designs in randomized trials of psychiatric treatments is challenging, in that prognostic factors for treatment outcomes are not as well established as in other specialties (e.g., cardiovascular disease50,51). For stratification to improve power, the stratification factors should have strong effects on treatment outcomes.52 Approaches adopted in other areas of medicine, such as multivariable risk stratification,50 may be particularly useful for identifying groups of people who vary in their expected benefit from treatment on the basis of a wide range of potential prognostic factors (e.g., multiple aspects of social disadvantage).
Conclusions
The nature of the differential intervention effects varied between the two economic factors studied. The PROSPECT intervention was more effective among participants reporting financial strain at baseline. The magnitude of this differential effect was clinically important—approximately 5 points on the Hamilton Depression Rating Scale (e.g., approximately twice the size of the effect considered clinically significant, and usually observed, in treatment studies53). We speculate that financially strained people might have benefited more from the intervention because the study provided them with the kind of high-quality depression treatments not previously available from their primary care providers. Thus, the observed differential effects may reflect the positive impact of ongoing treatment management that entails aiding clinicians in following treatment guidelines, monitoring patients’ side effects, and enhancing adherence to depression treatments. At the same time, we observed that for people residing in medium- and high-poverty census tracts, the intervention effect weakened over time. This finding could reflect the effects of neighborhood-level stressors on depressive symptoms that, in the long run, outweighed initial gains in mood brought on by antidepressant therapies.33
The public health, and particularly mental health, impact of adverse economic conditions is increasingly recognized.54 Here we have shown that this impact potentially extends to the effectiveness of clinical interventions for depression. We identified financial strain and neighborhood poverty as two economic factors that had contrasting effects on depression treatment outcomes. More work is needed to understand the mechanisms by which these and other aspects of social and economic disadvantage moderate treatment outcomes, and to determine the viability of directly intervening on these factors in future treatment studies.
Supplementary Material
Acknowledgments
We sincerely appreciate the contributions of Kathleen McGaffigan to data management and statistical programming.
Sources of Funding: This work was supported by National Institute of Mental Health grants MH83335, MH085943, and MH059366. Forest Pharmaceuticals provided free citalopram for the PROSPECT study. The funders had no role in the design or conduct of the present study.
Footnotes
Conflicts of Interest: George S. Alexopoulos receives research support from Forest; he serves on the speakers’ bureau for Forest, Lilly, Bristol Meyers Squibb, Astra Zeneca, Merck; and is a stockholder in Johnson & Johnson. Martha L. Bruce has received financial compensation for consulting to Medispin, Inc., a medical education company. Benoit H. Mulsant has received financial support during the past 36 months from the US National Institute of Mental Health and the Canadian Institutes for Health Research and pharmaceutical supplies from Bristol-Myers Squibb, Eli Lilly, and Pfizer for his NIH sponsored research. He has also received reimbursement for travel expenses from Roche. Benoit H. Mulsant has received pharmaceutical supplies from Bristol-Myers Squibb, Eli Lilly, and Pfizer for his NIH sponsored research. He has also received reimbursement for travel expenses from Roche. Charles F. Reynolds III receives pharmaceutical supplies from Forest Laboratories, BMS, Pfizer, and Lilly for his NIH sponsored research.
SDC Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com). This content is peer-reviewed but not copy-edited; it is the sole responsibility of the author.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Stephen E. Gilman, Department of Society, Human Development and Health, and Department of Epidemiology, Harvard School of Public Health, and Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts, USA
Garrett M. Fitzmaurice, Department of Psychiatry, Harvard Medical School; Department of Biostatistics, Harvard School of Public Health, Boston, Massachusetts, USA
Martha L. Bruce, Department of Psychiatry, Weill-Cornell Medical College, White Plains, New York, USA
Thomas Ten Have, Department of Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania, USA.
M. Maria Glymour, Department of Society, Human Development, and Health, Harvard School of Public Health; Boston, Massachusetts, USA.
Hannah Carliner, Department of Society, Human Development, and Health, Harvard School of Public Health; Boston, Massachusetts, USA.
George S. Alexopoulos, Department of Psychiatry, Weill-Cornell Medical College, White Plains, New York, USA
Benoit H. Mulsant, Center for Addiction and Mental Health, and Department of Psychiatry, University of Toronto, Toronto, Ontario, Canada
Charles F. Reynolds, III, Department of Psychiatry, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Alex Cohen, Faculty of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, London, United Kingdom.
References
- 1.Cohen A, Houck PR, Szanto K, Dew MA, Gilman SE, Reynolds CF., 3rd Social inequalities in response to antidepressant treatment in older adults. Arch Gen Psychiatry. 2006;63(1):50–6. doi: 10.1001/archpsyc.63.1.50. [DOI] [PubMed] [Google Scholar]
- 2.Friedman ES, Wisniewski SR, Gilmer W, Nierenberg AA, Rush AJ, Fava M, Zisook S, Balasubramani GK, Trivedi MH. Sociodemographic, clinical, and treatment characteristics associated with worsened depression during treatment with citalopram: results of the NIMH STAR(*)D trial. Depress Anxiety. 2009;26(7):612–21. doi: 10.1002/da.20568. [DOI] [PubMed] [Google Scholar]
- 3.Gilman SE, Trinh NH, Smoller JW, Fava M, Murphy JM, Breslau J. Psychosocial stressors and the prognosis of major depression: a test of Axis IV. Psychological Medicine. 2012:1–14. doi: 10.1017/S0033291712001080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilman SE, Carliner H, Cohen A. The social determinants of depression in older adulthood. In: Reynolds CF, H L, M S, editors. Late-Life Mood Disorders. Oxford University Press; In Press. [Google Scholar]
- 5.Gilman SE, Kawachi I, Fitzmaurice GM, Buka SL. Socioeconomic status in childhood and the lifetime risk of major depression. International Journal of Epidemiology. 2002;31(2):359–67. [PubMed] [Google Scholar]
- 6.Roy-Byrne PP, Joesch JM, Wang PS, Kessler RC. Low socioeconomic status and mental health care use among respondents with anxiety and depression in the NCS-R. Psychiatr Serv. 2009;60(9):1190–7. doi: 10.1176/ps.2009.60.9.1190. [DOI] [PubMed] [Google Scholar]
- 7.Harman JS, Edlund MJ, Fortney JC. Disparities in the Adequacy of Depression Treatment in the United States. Psychiatr Serv. 2004;55(12):1379–1385. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- 8.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–40. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 9.Houle J, Beaulieu MD, Lesperance F, Frasure-Smith N, Lambert J. Inequities in medical follow-up for depression: a population-based study in Montreal. Psychiatr Serv. 2010;61(3):258–63. doi: 10.1176/ps.2010.61.3.258. [DOI] [PubMed] [Google Scholar]
- 10.Stockdale SE, Lagomasino IT, Siddique J, McGuire T, Miranda J. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995-2005. Medical Care. 2008;46(7):668–77. doi: 10.1097/MLR.0b013e3181789496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harman JS, Veazie PJ, Lyness JM. Primary care physician office visits for depression by older Americans. Journal of General Internal Medicine. 2006;21(9):926–30. doi: 10.1111/j.1525-1497.2006.00497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stafford RS, Ausiello JC, Misra B, Saglam D. National Patterns of Depression Treatment in Primary Care. Prim Care Companion J Clin Psychiatry. 2000;2(6):211–216. doi: 10.4088/pcc.v02n0603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) Jama. 2003;289(23):3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 14.Alexopoulos GS, Katz IR, Bruce ML, Heo M, Ten Have T, Raue P, Bogner HR, Schulberg HC, Mulsant BH, Reynolds CF., 3rd Remission in depressed geriatric primary care patients: a report from the PROSPECT study. American Journal of Psychiatry. 2005;162(4):718–24. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bogner HR, Cary MS, Bruce ML, Reynolds CF, 3rd, Mulsant B, Ten Have T, Alexopoulos GS. The role of medical comorbidity in outcome of major depression in primary care: the PROSPECT study. American Journal of Geriatric Psychiatry. 2005;13(10):861–8. doi: 10.1176/appi.ajgp.13.10.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bruce ML, Ten Have TR, Reynolds CF, 3rd, Katz II, Schulberg HC, Mulsant BH, Brown GK, McAvay GJ, Pearson JL, Alexopoulos GS. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291(9):1081–91. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 17.Alexopoulos GS, Reynolds CF, 3rd, Bruce ML, Katz IR, Raue PJ, Mulsant BH, Oslin DW, Ten Have T. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. American Journal of Psychiatry. 2009;166(8):882–90. doi: 10.1176/appi.ajp.2009.08121779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gallo JJ, Bogner HR, Morales KH, Post EP, Lin JY, Bruce ML. The effect of a primary care practice-based depression intervention on mortality in older adults: a randomized trial. Annals of Internal Medicine. 2007;146(10):689–98. doi: 10.7326/0003-4819-146-10-200705150-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bruce ML, Pearson JL. Designing an intervention to prevent suicide: PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial) Dialogues Clin Neurosci. 1999;1(2):100–12. doi: 10.31887/DCNS.1999.1.2/mbruce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, Rush AJ, Weissman MM. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Archives of General Psychiatry. 1991;48(9):851–5. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Brown GK, Steer RA. Psychometric characteristics of the Scale for Suicide Ideation with psychiatric outpatients. Behav Res Ther. 1997;35(11):1039–46. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- 23.Gilman S, Bruce M, Have T, Alexopoulos G, Mulsant B, Reynolds C, Cohen A. Social inequalities in depression and suicidal ideation among older primary care patients. Social Psychiatry and Psychiatric Epidemiology. doi: 10.1007/s00127-012-0575-9. DOI: 10.1007/s00127-012-0575-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bishaw A, United States. Bureau of the Census . Censr. U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau; Washington, D.C.: 2005. Areas with concentrated poverty, 1999: Census 2000 special reports. [Google Scholar]
- 25.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 26.Rothwell PM. Treating individuals 2. Subgroup analysis in randomised controlled trials: importance, indications, and interpretation. Lancet. 2005;365(9454):176–86. doi: 10.1016/S0140-6736(05)17709-5. [DOI] [PubMed] [Google Scholar]
- 27.Kraemer HC, Frank E, Kupfer DJ. Moderators of treatment outcomes: clinical, research, and policy importance. Jama. 2006;296(10):1286–9. doi: 10.1001/jama.296.10.1286. [DOI] [PubMed] [Google Scholar]
- 28.Fitzmaurice GM, Laird NM, Ware JH. Wiley series in probability and statistics. Wiley-Interscience; Hoboken, N.J.: 2004. Applied longitudinal analysis. [Google Scholar]
- 29.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59(10):877–83. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 30.Brookes ST, Whitely E, Egger M, Smith GD, Mulheran PA, Peters TJ. Subgroup analyses in randomized trials: risks of subgroup-specific analyses; power and sample size for the interaction test. Journal of clinical epidemiology. 2004;57(3):229–36. doi: 10.1016/j.jclinepi.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 31.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. Journal of Health and Social Behavior. 2006;47(1):17–31. doi: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 32.Zimmerman FJ, Katon W. Socioeconomic status, depression disparities, and financial strain: what lies behind the income-depression relationship? Health Econ. 2005;14(12):1197–215. doi: 10.1002/hec.1011. [DOI] [PubMed] [Google Scholar]
- 33.Paczkowski MM, Galea S. Sociodemographic characteristics of the neighborhood and depressive symptoms. Curr Opin Psychiatry. 2010;23(4):337–41. doi: 10.1097/YCO.0b013e32833ad70b. [DOI] [PubMed] [Google Scholar]
- 34.VanderWeele TJ, Knol MJ. Interpretation of subgroup analyses in randomized trials: heterogeneity versus secondary interventions. Annals of Internal Medicine. 2011;154(10):680–3. doi: 10.7326/0003-4819-154-10-201105170-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen A, Chapman BP, Gilman SE, Delmerico AM, Wieczorek W, Duberstein PR, Lyness JM. Social inequalities in the occurrence of suicidal ideation among older primary care patients. American Journal of Geriatric Psychiatry. 2010;18(12):1146–1154. doi: 10.1097/JGP.0b013e3181dd1e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen A, Gilman SE, Houck PR, Szanto K, Reynolds CF., 3rd Socioeconomic status and anxiety as predictors of antidepressant treatment response and suicidal ideation in older adults. Social Psychiatry and Psychiatric Epidemiology. 2009;44(4):272–7. doi: 10.1007/s00127-008-0436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Olfson M, Shea S, Feder A, Fuentes M, Nomura Y, Gameroff M, Weissman MM. Prevalence of anxiety, depression, and substance use disorders in an urban general medicine practice. Archives of Family Medicine. 2000;9(9):876–83. doi: 10.1001/archfami.9.9.876. [DOI] [PubMed] [Google Scholar]
- 38.Stafford RS, Saglam D, Causino N, Starfield B, Culpepper L, Marder WD, Blumenthal D. Trends in adult visits to primary care physicians in the United States. Archives of Family Medicine. 1999;8(1):26–32. doi: 10.1001/archfami.8.1.26. [DOI] [PubMed] [Google Scholar]
- 39.Strothers HS, 3rd, Rust G, Minor P, Fresh E, Druss B, Satcher D. Disparities in antidepressant treatment in Medicaid elderly diagnosed with depression. Journal of the American Geriatrics Society. 2005;53(3):456–61. doi: 10.1111/j.1532-5415.2005.53164.x. [DOI] [PubMed] [Google Scholar]
- 40.Varkey AB, Manwell LB, Williams ES, Ibrahim SA, Brown RL, Bobula JA, Horner-Ibler BA, Schwartz MD, Konrad TR, Wiltshire JC, Linzer M. Separate and unequal: clinics where minority and nonminority patients receive primary care. Archives of Internal Medicine. 2009;169(3):243–50. doi: 10.1001/archinternmed.2008.559. [DOI] [PubMed] [Google Scholar]
- 41.Bao Y, Alexopoulos GS, Casalino LP, Ten Have TR, Donohue JM, Post EP, Schackman BR, Bruce ML. Collaborative depression care management and disparities in depression treatment and outcomes. Archives of General Psychiatry. 2011;68(6):627–36. doi: 10.1001/archgenpsychiatry.2011.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annual review of clinical psychology. 2009;5:363–89. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lesser IM, Myers HF, Lin KM, Bingham Mira C, Joseph NT, Olmos NT, Schettino J, Poland RE. Ethnic differences in antidepressant response: a prospective multi-site clinical trial. Depress Anxiety. 2010;27(1):56–62. doi: 10.1002/da.20619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miranda J, Schoenbaum M, Sherbourne C, Duan N, Wells K. Effects of Primary Care Depression Treatment on Minority Patients’ Clinical Status and Employment. Arch Gen Psychiatry. 2004;61(8):827–834. doi: 10.1001/archpsyc.61.8.827. [DOI] [PubMed] [Google Scholar]
- 45.Roy-Byrne PP, Perera P, Pitts CD, Christi JA. Paroxetine response and tolerability among ethnic minority patients with mood or anxiety disorders: a pooled analysis. J Clin Psychiatry. 2005;66(10):1228–33. doi: 10.4088/jcp.v66n1004. [DOI] [PubMed] [Google Scholar]
- 46.Arean PA, Gum AM, Tang L, Unutzer J. Service Use and Outcomes Among Elderly Persons With Low Incomes Being Treated for Depression. Psychiatr Serv. 2007;58(8):1057–1064. doi: 10.1176/ps.2007.58.8.1057. [DOI] [PubMed] [Google Scholar]
- 47.Areán PA, Ayalon L, Hunkeler E, Lin EHB, Tang L, Harpole L, Hendrie H, Williams JWJ, Unützer J. Improving Depression Care for Older, Minority Patients in Primary Care. Medical Care. 2005;43(4):381–390. doi: 10.1097/01.mlr.0000156852.09920.b1. [DOI] [PubMed] [Google Scholar]
- 48.Rothwell PM. Can overall results of clinical trials be applied to all patients? Lancet. 1995;345(8965):1616–9. doi: 10.1016/s0140-6736(95)90120-5. [DOI] [PubMed] [Google Scholar]
- 49.Warden D, Rush AJ, Wisniewski SR, Lesser IM, Thase ME, Balasubramani GK, Shores-Wilson K, Nierenberg AA, Trivedi MH. Income and attrition in the treatment of depression: a STAR*D report. Depress Anxiety. 2009;26(7):622–33. doi: 10.1002/da.20541. [DOI] [PubMed] [Google Scholar]
- 50.Hayward RA, Kent DM, Vijan S, Hofer TP. Multivariable risk prediction can greatly enhance the statistical power of clinical trial subgroup analysis. BMC medical research methodology. 2006;6:18. doi: 10.1186/1471-2288-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rothwell PM, Mehta Z, Howard SC, Gutnikov SA, Warlow CP. From subgroups to individuals: general principles and the example of carotid endarterectomy. The Lancet. 2005;365(9455):256–265. doi: 10.1016/S0140-6736(05)17746-0. [DOI] [PubMed] [Google Scholar]
- 52.Kernan WN, Viscoli CM, Makuch RW, Brass LM, Horwitz RI. Stratified randomization for clinical trials. Journal of Clinical Epidemiology. 1999;52(1):19–26. doi: 10.1016/s0895-4356(98)00138-3. [DOI] [PubMed] [Google Scholar]
- 53.Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS Med. 2008;5(2):e45. doi: 10.1371/journal.pmed.0050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cooper B. Economic recession and mental health: an overview. Neuropsychiatr. 2011;25(3):113–7. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.