Abstract
Endometriosis-related ovarian neoplasms (ERONs) are a unique group of tumors as they are associated with endometriosis, especially endometriosis presenting as an ovarian endometriotic cyst (endometrioma). ERONs include clear cell carcinoma, endometrioid carcinoma, and seromucinous borderline tumor. A growing body of evidence from both clinicopathological and molecular studies suggests that most, if not all, ERONs develop from endometriotic cyst epithelium through different stages of tumor progression. The endometriotic cyst contains abundant iron-induced reactive oxygen species which are thought to be mutagenic, and chronic exposure of cystic epithelium to this microenvironment facilitates the accumulation of somatic mutations that ultimately result in tumor development. Molecular analyses of ERONs, including genome-wide screens, have identified several molecular genetic alterations that lead to aberrant activation or inactivation of pathways involving ARID1A, PI3K, Wnt, and PP2A. Among all molecular genetic changes identified to date, inactivating mutations of the ARID1A tumor suppressor gene are the most common in ERON. Understanding the molecular changes and pathogenesis involved in the development of ERON is fundamental for future translational studies aimed at designing new diagnostic tests for early detection and identifying critical molecular features for targeted therapeutics.
Keywords: endometriosis-related ovarian neoplasms, clear cell carcinoma, endometrioid carcinoma, endometrial carcinoma, ARID1A
Introduction
Ovarian epithelial tumors can be broadly classified into two major types of diseases. Type I ovarian carcinoma is composed of clear cell carcinoma (CCC), endometrioid carcinoma (EC), mucinous carcinoma, and low-grade serous carcinoma, while type II ovarian carcinoma mainly consists of high-grade serous carcinoma, the most common and lethal type of ovarian neoplasm.1 Type I and type II ovarian tumors are characterized by different types of precursor lesions and distinct molecular genetic alterations that account for their unique pathobiological features and clinical behaviors. For example, endometriosis is associated with several type I diseases including ovarian cystic clear cell and endometrioid carcinoma, whereas type II tumors are thought to develop from fallopian tubal epithelium through a putative precursor lesion called “serous tubal intraepithelial carcinoma”.2, 3 Recognition of the role of endometriosis in the development of some ovarian cancers (type I carcinomas) dates back to as early as 1925,4 and subsequent studies have demonstrated that endometriosis, especially when presenting as an ovarian endometriotic cyst (endometrioma), is associated with a risk for developing cystic CCC and EC, collectively known as “endometriosis-related ovarian neoplasms (ERONs)”.5 In fact, ERON is the most serious complication of endometriosis.6 Moreover, clinicopathological, molecular, and epidemiologic studies provide further evidence identifying endometriosis as the tissue of origin for both cystic CCC and EC.3 Historically, morphologic studies have consistently demonstrated an association of CCC and EC with endometriosis, and it is now widely recognized that most of these tumors arise from endometriotic cysts. Furthermore, a morphological continuum of sequential stages during tumor progression can be observed from endometriosis to EC or CCC (Fig. 1). Common molecular genetic alterations in ERON such as PTEN deletion and microsatellite instability can also be detected in the normal-appearing epithelial cells of endometriotic cysts.7, 8 Several reports have further delineated the clonal relationship between endometriosis and ERON.9–12 More recently, gene expression profiling has shown that ovarian CCC and EC are molecularly more similar to normal uterine endometrium than to colonic epithelium, ovarian surface epithelium, or fallopian tube epithelium.13
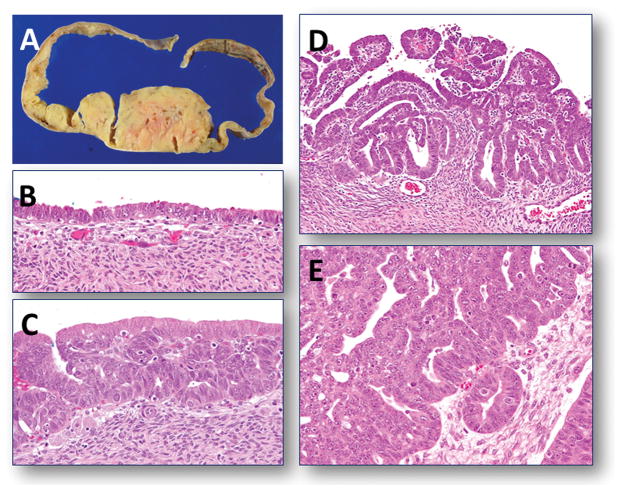
Fig. 1.
Gross appearance and morphological continuum in tumor progression in an endometrioid carcinoma. A. An ovarian endometriotic cyst containing an intracystic polyploid endometrioid carcinoma. B–E. Photomicrographs show a morphological continuum of different stages of tumor progression from normal-appearing endometriotic cyst epithelium to invasive endometrioid carcinoma.
In addition to ovarian cystic CCC and EC, a relatively rare ovarian tumor termed “seromucinous borderline tumor” (SMBT) or “endocervical-like mucinous borderline tumor” is also frequently associated with endometriosis. Like ovarian CCC and EC, SMBT is frequently located within an ovarian endometriotic cyst, an observation providing further evidence for the endometriotic origin for these tumors. Thus, we include SMBT along with CCC and EC as the known ERONs.
Genome-wide analyses have been performed in several types of gynecological neoplasms including ovarian high-grade serous carcinoma,14 ovarian low-grade serous carcinoma,15 ovarian clear cell carcinoma,16 uterine serous carcinoma,17 and uterine endometrioid carcinoma (TCGA, unpublished). These studies come to the conclusion that somatic ARID1A mutations are uniquely associated with ERONs.18 In this review, we briefly summarize the clinicopathological features and discuss the pathophysiology of ERONs with special emphasis on molecular genetic alterations of ARID1A.
Clinicopathological features of ERON
Ovarian clear cell carcinoma
There is a significant racial difference in the incidence of ovarian CCC among ovarian carcinomas. CCC represents approximately 5–10% of ovarian cancers in the United States.19–23 In contrast, CCC incidence among ovarian carcinoma is significantly higher in Japan (approximately 20%),24, 25 and the incidence has risen in the past decade. Similarly, Chan et al. 23 performed an incidence analysis according to racial background among 28,082 U.S. ovarian cancer patients, and found that the incidence of CCC is higher in the Asian American population (11.8%) than in the White American population (4.8%) or African American population (3.1%).
Despite 60–70% of CCCs present in early stages (Stage I or II) with approximately 50% being stage I disease, 21, 23, 24, 26–28 CCC has widely been regarded as a subtype with poor prognosis when presenting at an advanced stage. The prognosis of early stage CCCs are generally much better than advanced stage CCCs. 20, 22, 24, 29, 30 One of the main explanations for the poor prognosis of advanced stage ovarian CCC patients is that their tumors are more resistant to platinum-based chemotherapy. 21,23,24,31,32,33,28 Development of new target-based therapies thus remains an unmet need for these patients.
It has been well established that there is strong association between endometriosis and the development of CCC, and women with endometriosis are at a higher risk to develop CCC than those without. Approximately 30–35% of CCCs are associated with endometriosis either in the involved ovary or in other pelvic or peritoneal tissues. By separating CCC into either cystic or adenofibromatous lesions, Veras et al.34 found that endometriosis is more frequently associated with cystic CCC (90%) than with adenofibromatous CCC (44%). A prospective study in Japan, which specifically focused on carcinomas arising from ovarian endometriotic cysts in a cohort of 6398 patients with endometriotic cysts, revealed a significantly increased ovarian cancer incidence in women with ovarian endometriotic cysts (standardized incidence ratio, 8.95), with 39% of cancers being CCC, and 35% being EC.35 Thus, endometriosis, especially endometriotic cysts, should be considered not only as a risk factor for ERONs, but as potential precursors of ERONs.
Histologically, cystic CCC exhibits a unilocular or paucilocular cystic lesion with a solid component that protrudes into the cystic cavity. Stepwise transition from benign-appearing glandular epithelium, to so-called “atypical endometriosis”, to overt CCC can be commonly observed.34,36,37,12,13 The tumor cells of CCC recapitulate endometrial glands during pregnancy (Arias-Stella reaction), and are characterized by clear (glycogen-rich) cytoplasm with hobnail morphology, forming tubulocystic, glandular, solid, and papillary patterns. Several tumors may be morphologically confused with ovarian CCC 38 but ovarian CCC has relatively specific immunostaining pattern including positive HNF-1β staining and negative (or focally positive) ER, PR, WT1 and p53 staining, that helps its differential diagnosis.39
Ovarian endometrioid carcinoma
EC is another subtype of ovarian epithelial cancer that is frequently associated with endometriosis, especially endometriotic cysts. The incidence of ovarian EC in the older literature is about 15–20%. However, if strict criteria are applied, requiring a close morphological resemblance to uterine endometrioid adenocarcinoma and exclusion of high-grade carcinomas, the figure is estimated to be much lower (7.5%). Up to 42% of ECs are associated with ipsilateral ovarian or pelvic endometriosis.40,41,42,36 Similar to CCC, EC is frequently associated with atypical endometriosis (23% of cases).36 Interestingly, 15–20% of ovarian ECs are associated with uterine endometrial carcinoma. 43–47 The favorable outcome in cases exhibiting cancer limited to both organs suggests independent primaries. However, it is sometimes difficult to distinguish metastatic uterine endometrioid carcinoma involving the ovary from independent primary tumors of both organs. Most ERONs are either CCC or EC, but occasionally there are cases exhibiting mixed CCC and EC within the same tumor, suggesting that they share a common precursor arising in the endometriotic cyst, which then differentiates into different histologic types, or that they arise from independent clones that separately evolve into CCC and EC.
On gross examination, most ECs show solid growth in the background of an endometriotic cyst. The tumor nodules may be solitary or multiple with papillary protrusions that contain invasive carcinoma components (Fig. 1A). The common criterion used to diagnose EC is that the glandular component of EC resembles the endometrioid carcinomas of the uterus. As a consequence, almost all ovarian ECs are well-differentiated or low-grade, and are characterized by a confluent or cribriform proliferation of glands lined by tall, stratified columnar epithelium with sharp luminal margins. Occasionally, high-grade endometrioid carcinoma is diagnosed in the ovary, but it is uncertain if high-grade endometrioid carcinoma represents a tumor progression from a low-grade endometrioid carcinoma or if it arises independently.
Seromucinous borderline tumor
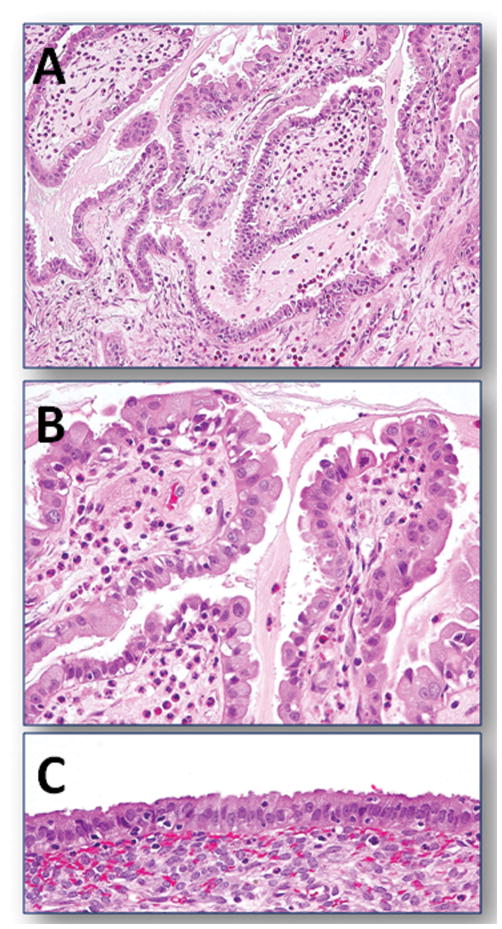
Two types of ovarian mucinous borderline tumors of the ovary have been recognized; they are gastrointestinal-type and nongastrointestinal-type borderline tumors. The former is far more common than the latter, comprising approximately 85% of mucinous borderline tumors of the ovary. Both types of borderline tumors are distinct in their clinical presentation, morphology, immunophenotype, and molecular genetic alterations. The nongastrointestinal-type mucinous borderline tumors have been described as displaying both endocervical and serous differentiation. There are several terms used to describe this tumor entity from time to time; they include “endocervical-like” mucinous borderline tumors, “mixed-epithelial papillary cystadenoma of borderline malignancy of mullerian type,” or “atypical proliferative seromucinous (borderline) tumors,” reflecting the uncertainty about the biological nature of this disease. In this review, we group all of these tumors under the umbrella seromucinous borderline tumor (SMBT). Bilateral ovarian involvement is much more frequent in SMBTs than in gastrointestinal-type borderline tumors. Grossly, SMBTs are almost always unilocular or paucilocular cystic lesions that have numerous intracystic papillae. Approximately 20% of SMBTs are reported to have extraovarian spread at the time of diagnosis.48 However, the malignant counterpart of SMBT, seromucinous adenocarcinoma, is extremely rare. Histologically, SMBTs frequently contain ciliated cells, endometrial-type cells, cells with abundant eosinophilic cytoplasm, and hobnail-shaped cells, all of which can be found in endometrioid tumors (Fig. 2). In addition, a prominent leukocyte infiltration is almost always present, and appears unique to SMBT among all ovarian borderline tumors. Coexistence of endometriosis is observed in 30–70% of SMBTs.48, 49,50 Furthermore, there is accumulating evidence based on immunohistochemical studies to support the Mullerian-type nature of SMBT. Most SMBTs express estrogen receptor, progesterone receptor, CA-125, and vimentin, whereas gastro-intestinal types of mucinous borderline tumors are usually negative for these markers.51, 52 Therefore, it is now widely accepted that SMBT is a tumor with a mixed Mullerian phenotype, and the endometriotic cyst is its likely origin.
Fig. 2.
An example of a seromucinous borderline tumor of the ovary arising from an endometriotic cyst. A. A lower magnification view shows the typical papillary growth of the tumor with abundant mucinous material in the lumen. B. A higher magnification reveals the mixed histologic features of the tumor cells exhibiting serous, mucinous, and hobnail-shaped differentiation. A prominent leukocyte infiltration is also present. C. portion of endometriotic cyst adjacent to the ovarian tumor.
Pathogenesis of ERON
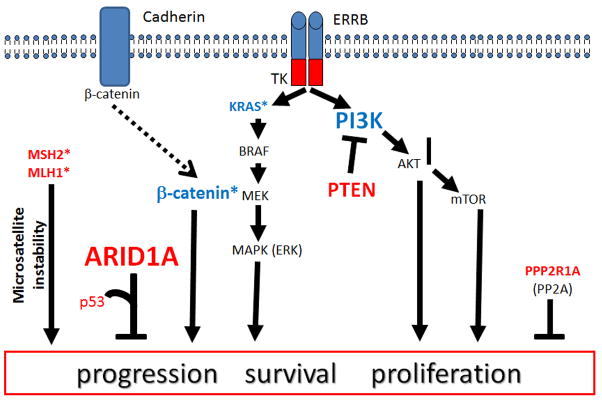
The carcinogenic steps contributing to the development of ERONs from endometriotic cystic epithelium are unclear. “Incessant menstruation” and longstanding estrogen stimulation are likely contributing factors, as repeated epithelial damage and repair in an inflammatory tissue microenvironment (cyst content) rich in iron-induced oxygen free radicals facilitate the accumulation of DNA damage that predispose endometriotic cyst epithelial cells to neoplastic transformation.53, 54 It has been thought that DNA damage is the underlying driving force propelling tumor development through creating molecular genetic alterations in several cancer-related genes and the pathways they control. We summarize the most common molecular genetic alterations in ERONs with special emphasis on ARID1A mutations in the next section (Fig. 3).
Fig 3. Molecular genetic alterations and pathway aberrations in ERON.
The common molecular genetic changes shared by clear cell and endometrioid carcinomas include ARID1A mutation, PIK3CA/PTEN mutation, and PP2R1A mutation. Mutations in CTNNB1 and mismatch repair genes such as MHL1 and MSH2 leading to microsatellite instability are almost always detected in endometrioid carcinoma but not in clear cell carcinoma. Genes in red indicate inactivating (loss of function) mutations, and genes in blue represent activating (gain of function) mutations. The larger the font, the greater the observed frequency of mutation of the gene. Asterisks indicate molecular changes that are predominantly found in ovarian endometrioid carcinoma.
In ovarian CCC, somatic activating mutations of PIK3CA 55 are detected in nearly half of the affinity-purified fresh tumors and cell lines. Moreover, Yamamoto et al. report that mutations of PIK3CA occur not only in CCCs but also in the concurrent endometriotic epithelium. Since the mutation is detected even in the associated endometriosis, which lacks cytological atypia, it has been suggested that these mutations occur during the early stage of tumorigenesis in ovarian CCC, i.e., during malignant transformation of endometriosis.11, 56 The relatively high frequency of PIK3CA mutations in ovarian CCC contrasts with rare PIK3CA mutations in ovarian high-grade serous carcinoma, the most common and aggressive type of ovarian cancer. Interestingly, expression of PTEN, a tumor suppressor gene involved in the PI3K signaling pathway (Fig. 3), decreases in approximately one third of CCCs,57 supporting a role of an aberrant PI3K pathway in the development of CCC (Fig. 2). Loss of heterozygosity at the PTEN locus is reported in both the carcinoma and associated endometriotic cyst epithelium in some cases, suggesting that inactivation of the PTEN tumor suppressor, like mutation of PIK3CA, is a relatively early molecular event in the development of ovarian CCC.12 Mutations that are commonly detected in other types of ovarian cancer such as KRAS, BRAF, and TP53 have been found in only a few CCCs.58 Although studies to date are rather limited, CCCs do not appear to share many other changes with ECs, as canonical Wnt signaling pathway defects and microsatellite instability have been rarely observed in CCC (Fig. 3).58
In addition to molecular genetic changes, ovarian CCC is characterized by a unique gene expression pattern as compared to other histological types of ovarian carcinomas.58 Compared to normal tissues including colon, endometrium, and fallopian tube, the overall gene expression profile of CCC is most similar to that of normal endometrium, supporting the view that the cell of origin of CCC likely arises from endometriosis.13 An increasing number of genes have been reported to be preferentially expressed in CCC as compared to other types of ovarian carcinoma. Based on a comprehensive gene expression analysis, Yamaguchi et al. proposed a “signature” of ovarian CCC that consists of HNF-1β, versican (VCAN), and several genes involved in oxidative stress.59 Interestingly, expression of these CCC signature genes is induced by treatment of immortalized ovarian surface epithelial cells with the contents of endometriotic cysts, suggesting that the CCC signature may be dependent on the tumor microenvironment, and suggesting that CCC pathogenesis is related to endometriosis. In fact, several researchers hypothesize that the iron in endometriosis participates in the pathogenesis of CCC via generation of reactive oxygen species.54, 60
In ovarian EC, several molecular genetic alterations have been reported including CTNNB1 and PTEN mutations along with microsatellite instability, of which alterations are also detected in uterine endometrioid carcinoma (Fig. 3).58 CTNNB1 encodes β-catenin, which plays a pivotal role in the Wnt/β-catenin signaling pathway. Dysregulation of Wnt/β-catenin signaling occurs in 16–38% of ovarian ECs, most often as a result of activating mutations of CTNNB1. Interestingly, CTNNB1 mutation is highly characteristic of ECs, as CTNNB1 mutation is not found in other types of ovarian carcinoma. On the other hand, PTEN is mutated in 14–20% of ovarian ECs and in 46% of those with loss of heterozygosity (LOH) of 10q23. Similar to CTNNB1, PTEN mutation is uncommon in other types of ovarian carcinomas. It has been reported that 10q23 LOH and PTEN mutations occurred in both endometrioid cysts and adjacent EC,12 a result supporting a possible precursor role of endometriosis in the carcinogenesis of ovarian ECs. Experimentally, Wnt and PI3K/PTEN pathway alterations are sufficient to induce ovarian EC development as evidenced by an engineered mouse model.61 The frequency of microsatellite instability (13–20%) in ovarian ECs is less frequent than in uterine endometrial carcinoma, and is usually associated with low levels of expression of proteins associated with mismatch repair, such as hMLH1 and hMSH2.62, 63
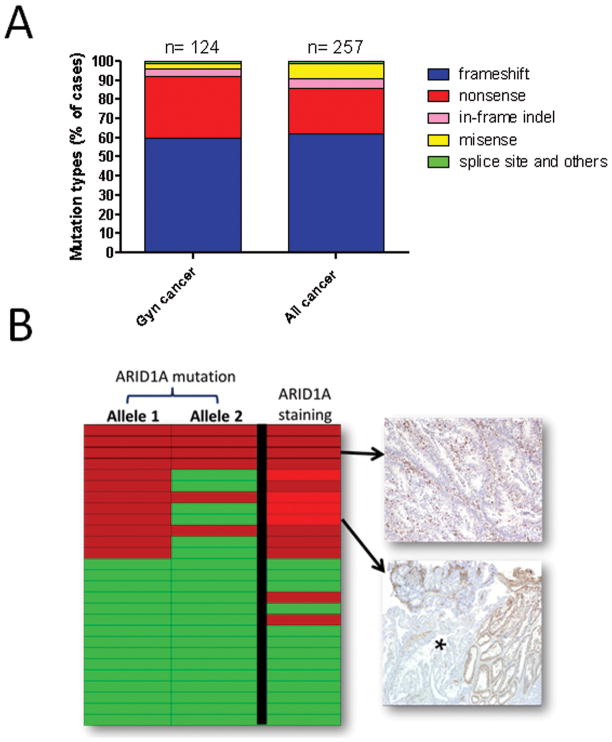
ARID1A is a new ERON-associated gene
Although the elucidation of the molecular changes discussed above has significantly advance our understanding of the pathogenesis of ERON, revelation of a comprehensive molecular landscape of ERON has only been made possible by genome-wide analyses. To this end, whole exome sequencing and RNA sequencing have been recently applied to detect genome-wide somatic mutations in ovarian CCC.16, 64 The two studies not only confirmed previously known molecular genetic changes as discussed above, but also identified novel alterations. Among them, somatic ARID1A mutation was independently shown by both studies to be the major molecular genetic change in ERONs.16, 64 ARID1A encodes BAF250a, which belongs to the SWI/SNF chromatin remodeling family. The BAF250a containing chromatin remodeling complex is responsible for several nuclear activities involving transcription, DNA methylation, and DNA synthesis and damage repair. BAF250a interacts with Brg1 (encoded by SMARCA4), an ATPase, which serves as the motor to move the chromatin remodeling complex along the DNA strand. ARID1A mutation occurs in approximately 50% of ovarian CCC and 40% of ovarian EC, as well as in 30% of uterine endometrioid carcinomas.16, 18, 64, 65 Although SMARCA4 mutations are not detected in CCC, it has been recently shown that lung adenocarcinomas harboring ARID1A mutations usually do not have SMARCA4 mutations and vice versa,66 indicating the ARID1A/Brg1 complex is important for tumor suppression. ARID1A mutations occur randomly in the coding regions, the great majority being frameshift and nonsense, leading to lost expression of ARID1A, suggesting that ARID1A is a tumor suppressor gene (Fig. 4). Indeed, a recent functional study has elucidated a tumor suppressor role of ARID1A, by which ARID1A protein interacts with p53 and suppresses cellular proliferation through p53-dependent transcriptional regulation of several tumor suppressors including CDKN1A (encoding p21) and SMAD3.67 As expected, inactivating mutations of ARID1A and TP53 are functionally synonymous, as mutations in either TP53 or ARID1A abolish the transcription of their target tumor suppressors such as CDKN1A, allowing uncontrolled cellular proliferation in ERONs.67 Of note, co-occurrence of ARID1A and TP53 mutations can be found in other cancer types 66 and thus the mutual exclusive nature of ARID1A and TP53 mutations may be tumor type dependent.
Fig. 4.
Types of ARID1A mutations and correlation of mutation and protein expression. A. Analysis of reported ARID1A mutations demonstrates that most of the mutation types belong to frameshift, nonsense, and in-frame mutations that are associated with loss of the tumor suppressor functions of ARID1A. B. ARID1A mutational status in 27 uterine endometrioid carcinomas. All the tumors with ARID1A mutation (in one or both alleles) have lost ARID1A immunoreactivity, and interestingly, two of 15 ARID1A wildtype cases also lost ARID1A staining probably due to epigenetic inactivation. Occasionally, clonal loss of ARID1A expression, as defined by undetectable ARID1A immunoreactivity contiguous to ARID1A positive tumor areas, is found in tumors harboring ARID1A mutations, probably as a result of intra-tumoral heterogeneity. Red boxes denote ARID1A mutation in both alleles (allele 1 and allele 2). Red boxes in the column of ARID1A staining indicate a complete loss (dark red) or clonal loss (light red) of ARID1A expression. Examples of ARID1A staining from two tumors are shown. Asterisk: the tumor area showing clonal loss of ARID1A staining.
The fact that frameshift and non-sense mutations result in loss of ARID1A expression is clear, as those mutants produce truncated mRNAs that are readily degraded. However, whether in-frame insert/deletion mutations also lose their tumor suppressor function is intriguing. A very recent study using biochemical assays demonstrates that, like frameshift mutations, the in-frame mutations that have been analyzed also lose their ability to inhibit cellular proliferation or to activate transcription of p21, a downstream effector of ARID1A.68
Given that ARID1A mutation is associated with loss of its expression,18, 64 undetectable ARID1A immunoreactivity has been proposed as a surrogate marker for the presence of inactivating ARID1A mutations in tissues. This is important because mutational analysis from formalin-fixed and paraffin-embedded tissues is technically challenging, as ARID1A contains many exons. However, we have correlated ARID1A mutational status and immunoreactivity in a series of cases and show that all tumors harboring ARID1A mutations in one or both alleles lose ARID1A immunoreactivity either completely or clonally (Fig. 4B). Several reports have analyzed ARID1A staining patterns in a variety of human cancers and normal tissues, and have demonstrated that loss of ARID1A expression, like its mutation, occurs most frequently in ERONs as well as uterine endometrioid carcinomas.18, 69–71 There is no correlation between ARID1A expression and clinical outcome in patients with ovarian CCC.56, 69, 72 The role of ARID1A inactivation in early molecular pathogenesis of CCC is illustrated in two recent reports. Yamomoto et al. report that loss of ARID1A protein expression occurs in early stages in endometriotic cyst epithelium, and frequently coexists with PIK3CA mutations 56. Similarly, another recent study compared ARID1A expression in endometriotic cysts and associated contiguous ovarian CCCs and well-differentiated ovarian ECs.73, 74 The results demonstrated that ARID1A loss occurred in two thirds of carcinomas (therefore those cases were informative), but in the remaining one third of cases, ARID1A immunoreactivity was retained in both the endometriotic cyst and in the concurrent carcinoma, and thus these cases were not informative.74 Importantly, all informative cases demonstrated loss of ARID1A immunoreactivity in both endometriotic cyst (including those termed “atypical endometriosis”) and associated carcinoma. Based on our experience (Shih, unpublished), loss of ARID1A staining is rarely seen in endometriotic cysts without associated ERON. However, some reports document a loss of ARID1A expression in 15%–20% of such cases.74, 75 Taken together, similarly to mutations in PTEN and PIK3CA, the evidence indicates that loss of ARID1A expression, presumably due to mutations, is an early molecular event in the development of the majority of ERONs.11, 56
In light of the important role of ARID1A in ERONs, Wu et al. analyzed ARID1A expression in different histological subtypes of ovarian borderline tumors including serous, gastrointestinal-type mucinous, seromucinous, and endometrioid borderline tumors using immunohistochemistry, and performed mutational analysis of ARID1A in selected cases.74 Loss of ARID1A staining was observed in 33% of SMBTs. In contrast, ARID1A staining was retained in all other borderline tumors with the exception of a single endometrioid tumor. Moreover, somatic ARID1A mutations were detected in 2 representative SMBTs, which showed complete loss of ARID1A. The loss of expression of ARID1A and the presence of inactivating mutations of ARID1A further link this tumor to CCC and EC, and provide molecular evidence that SMBT is a member of ERON.
Conclusion
It has become clear that certain types of ovarian neoplasms are associated with endometriosis, and they most likely arise from a pre-existing endometriotic cyst of the ovary. These tumors, collectively known as ERONs, include ovarian CCC, ovarian EC, and ovarian SMBT. ERONs are characterized by common molecular genetic changes that involve ARID1A, PI3K, and PP2A pathways, but they also have unique molecular changes such as microsatellite instability and CTNNB1 mutations, which occur in ovarian EC, and overexpression of HNF-1β, which is found in CCC. It would be of considerable interest to determine the molecular switch that dictates the development of different types of ERON, and to determine how those early molecular alterations including ARID1A, PTEN, and PIK3CA mutations collaborate in driving neoplastic transformation from an endometriotic cyst to an ERON. Given the availability of PI3K inhibitors, future clinical studies should determine if targeting the PI3K signaling pathway together with other therapeutic interventions has clinical benefit in advanced stage patients with ERON.
Acknowledgments
This study was supported by an NIH/NCI grant, CA165807.
Funding for this work received by NIH/NCI grant, CA165807.
Footnotes
Conflict of interest
None declared.
References
- 1.Kurman RJ, Shih IM. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol. 2010;34:433–443. doi: 10.1097/PAS.0b013e3181cf3d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurman RJ, Shih Ie M. Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer--shifting the paradigm. Hum Pathol. 2011;42:918–931. doi: 10.1016/j.humpath.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuhn E, Kurman RJ, Shih IM. Ovarian cancer is an imprted disease: fact or fiction? Curr Obstet Gynecol Rep. 2012;1:1–9. doi: 10.1007/s13669-011-0004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sampson JA. Endometrial carcinoma of the ovary, arising in endometrial tissue in that organ. Arch Surg. 1925;10:1–72. [Google Scholar]
- 5.Pearce CL, Templeman C, Rossing MA, Lee A, Near AM, Webb PM, Nagle CM, Doherty JA, Cushing-Haugen KL, Wicklund KG, Chang-Claude J, Hein R, Lurie G, Wilkens LR, Carney ME, Goodman MT, Moysich K, Kjaer SK, Hogdall E, Jensen A, Goode EL, Fridley BL, Larson MC, Schildkraut JM, Palmieri RT, Cramer DW, Terry KL, Vitonis AF, Titus LJ, Ziogas A, Brewster W, Anton-Culver H, Gentry-Maharaj A, Ramus SJ, Anderson AR, Brueggmann D, Fasching PA, Gayther SA, Huntsman DG, Menon U, Ness RB, Pike MC, Risch H, Wu AH, Berchuck A. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 2012;13:385–394. doi: 10.1016/S1470-2045(11)70404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mandai M, Suzuki A, Matsumura N, Baba T, Yamaguchi K, Hamanishi J, Yoshioka Y, Kosaka K, Konishi I. Clinical management of ovarian endometriotic cyst (chocolate cyst): diagnosis, medical treatment, and minimally invasive surgery. Curr Obstet Gynecol Rep. 2012;1:16–24. [Google Scholar]
- 7.Ali-Fehmi R, Khalifeh I, Bandyopadhyay S, Lawrence WD, Silva E, Liao D, Sarkar FH, Munkarah AR. Patterns of loss of heterozygosity at 10q23.3 and microsatellite instability in endometriosis, atypical endometriosis, and ovarian carcinoma arising in association with endometriosis. International journal of gynecological pathology : official journal of the International Society of Gynecological Pathologists. 2006;25:223–229. doi: 10.1097/01.pgp.0000192274.44061.36. [DOI] [PubMed] [Google Scholar]
- 8.Munksgaard PS, Blaakaer J. The association between endometriosis and ovarian cancer: a review of histological, genetic and molecular alterations. Gynecologic Oncology. 2012;124:164–169. doi: 10.1016/j.ygyno.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Jiang X, Morland SJ, Hitchcock A, Thomas EJ, Campbell IG. Allelotyping of endometriosis with adjacent ovarian carcinoma reveals evidence of a common lineage. Cancer research. 1998;58:1707–1712. [PubMed] [Google Scholar]
- 10.Prowse AH, Manek S, Varma R, Liu J, Godwin AK, Maher ER, Tomlinson IP, Kennedy SH. Molecular genetic evidence that endometriosis is a precursor of ovarian cancer. International journal of cancer Journal international du cancer. 2006;119:556–562. doi: 10.1002/ijc.21845. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto S, Tsuda H, Takano M, Iwaya K, Tamai S, Matsubara O. PIK3CA mutation is an early event in the development of endometriosis-associated ovarian clear cell adenocarcinoma. J Pathol. 2011;225:189–194. doi: 10.1002/path.2940. [DOI] [PubMed] [Google Scholar]
- 12.Sato N, Tsunoda H, Nishida M, Morishita Y, Takimoto Y, Kubo T, Noguchi M. Loss of heterozygosity on 10q23.3 and mutation of the tumor suppressor gene PTEN in benign endometrial cyst of the ovary: possible sequence progression from benign endometrial cyst to endometrioid carcinoma and clear cell carcinoma of the ovary. Cancer Res. 2000;60:7052–7056. [PubMed] [Google Scholar]
- 13.Marquez RT, Baggerly KA, Patterson AP, Liu J, Broaddus R, Frumovitz M, Atkinson EN, Smith DI, Hartmann L, Fishman D, Berchuck A, Whitaker R, Gershenson DM, Mills GB, Bast RC, Jr, Lu KH. Patterns of gene expression in different histotypes of epithelial ovarian cancer correlate with those in normal fallopian tube, endometrium, and colon. Clin Cancer Res. 2005;11:6116–6126. doi: 10.1158/1078-0432.CCR-04-2509. [DOI] [PubMed] [Google Scholar]
- 14.network Cgar. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–615. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones S, Wang TL, Kurman RJ, Nakayama K, Velculescu VE, Vogelstein B, Kinzler KW, Papadopoulos N, Shih Ie M. Low-grade serous carcinomas of the ovary contain very few point mutations. The Journal of pathology. 2012;226:413–420. doi: 10.1002/path.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones S, Wang TL, Shih Ie M, Mao TL, Nakayama K, Roden R, Glas R, Slamon D, Diaz LA, Jr, Vogelstein B, Kinzler KW, Velculescu VE, Papadopoulos N. Frequent mutations of chromatin remodeling gene ARID1A in ovarian clear cell carcinoma. Science. 2010;330:228–231. doi: 10.1126/science.1196333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuhn E, Wu RC, Wu G, Guan B, Zhang J, Wang Y, Song L, Yuan X, Wei L, Roden RBS, kUO kT, Nakayama K, Clarke B, Shaw P, Olvera N, levine DA, Kurman RJ, Wang TL, Shih IM. Genome-wide analyses of uterine serous carcinoma identify pathway aberrations involving cyclin E-Fbxw7, PI3K and p53. J Natl Cancer Inst. 2012 doi: 10.1093/jnci/djs345. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guan B, Mao TL, Panuganti PK, Kuhn E, Kurman RJ, Maeda D, Chen E, Jeng YM, Wang TL, Shih Ie M. Mutation and loss of expression of ARID1A in uterine low-grade endometrioid carcinoma. The American journal of surgical pathology. 2011;35:625–632. doi: 10.1097/PAS.0b013e318212782a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McGuire V, Jesser CA, Whittemore AS. Survival among U. S women with invasive epithelial ovarian cancer. Gynecologic Oncology. 2002;84:399–403. doi: 10.1006/gyno.2001.6536. [DOI] [PubMed] [Google Scholar]
- 20.Crozier MA, Copeland LJ, Silva EG, Gershenson DM, Stringer CA. Clear cell carcinoma of the ovary: a study of 59 cases. Gynecologic Oncology. 1989;35:199–203. doi: 10.1016/0090-8258(89)90043-7. [DOI] [PubMed] [Google Scholar]
- 21.Jenison EL, Montag AG, Griffiths CT, Welch WR, Lavin PT, Greer J, Knapp RC. Clear cell adenocarcinoma of the ovary: a clinical analysis and comparison with serous carcinoma. Gynecologic Oncology. 1989;32:65–71. doi: 10.1016/0090-8258(89)90852-4. [DOI] [PubMed] [Google Scholar]
- 22.Kennedy AW, Biscotti CV, Hart WR, Webster KD. Ovarian clear cell adenocarcinoma. Gynecologic Oncology. 1989;32:342–349. doi: 10.1016/0090-8258(89)90637-9. [DOI] [PubMed] [Google Scholar]
- 23.Chan JK, Teoh D, Hu JM, Shin JY, Osann K, Kapp DS. Do clear cell ovarian carcinomas have poorer prognosis compared to other epithelial cell types? A study of 1411 clear cell ovarian cancers. Gynecol Oncol. 2008;109:370–376. doi: 10.1016/j.ygyno.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Sugiyama T, Kamura T, Kigawa J, Terakawa N, Kikuchi Y, Kita T, Suzuki M, Sato I, Taguchi K. Clinical characteristics of clear cell carcinoma of the ovary: a distinct histologic type with poor prognosis and resistance to platinum-based chemotherapy. Cancer. 2000;88:2584–2589. [PubMed] [Google Scholar]
- 25.Ushijima K. Current status of gynecologic cancer in Japan. Journal of gynecologic oncology. 2009;20:67–71. doi: 10.3802/jgo.2009.20.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goncalves FP, Rodrigues AC. Phacoemulsification using clear cornea incision in steepest meridian. Arq Bras Oftalmol. 2007;70:225–228. [PubMed] [Google Scholar]
- 27.Takano M, Kikuchi Y, Yaegashi N, Kuzuya K, Ueki M, Tsuda H, Suzuki M, Kigawa J, Takeuchi S, Tsuda H, Moriya T, Sugiyama T. Clear cell carcinoma of the ovary: a retrospective multicentre experience of 254 patients with complete surgical staging. Br J Cancer. 2006;94:1369–1374. doi: 10.1038/sj.bjc.6603116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mizuno M, Kikkawa F, Shibata K, Kajiyama H, Ino K, Kawai M, Nagasaka T, Nomura S. Long-term follow-up and prognostic factor analysis in clear cell adenocarcinoma of the ovary. J Surg Oncol. 2006;94:138–143. doi: 10.1002/jso.20251. [DOI] [PubMed] [Google Scholar]
- 29.Behbakht K, Randall TC, Benjamin I, Morgan MA, King S, Rubin SC. Clinical characteristics of clear cell carcinoma of the ovary. Gynecologic Oncology. 1998;70:255–258. doi: 10.1006/gyno.1998.5071. [DOI] [PubMed] [Google Scholar]
- 30.Maeda D, Ota S, Takazawa Y, Aburatani H, Nakagawa S, Yano T, Taketani Y, Kodama T, Fukayama M. Glypican-3 expression in clear cell adenocarcinoma of the ovary. Mod Pathol. 2009;22:824–832. doi: 10.1038/modpathol.2009.40. [DOI] [PubMed] [Google Scholar]
- 31.Winter WE, 3rd, Maxwell GL, Tian C, Carlson JW, Ozols RF, Rose PG, Markman M, Armstrong DK, Muggia F, McGuire WP. Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007;25:3621–3627. doi: 10.1200/JCO.2006.10.2517. [DOI] [PubMed] [Google Scholar]
- 32.Goff BA, Sainz de la Cuesta R, Muntz HG, Fleischhacker D, Ek M, Rice LW, Nikrui N, Tamimi HK, Cain JM, Greer BE, Fuller AF., Jr Clear cell carcinoma of the ovary: a distinct histologic type with poor prognosis and resistance to platinum-based chemotherapy in stage III disease. Gynecol Oncol. 1996;60:412–417. doi: 10.1006/gyno.1996.0065. [DOI] [PubMed] [Google Scholar]
- 33.Pectasides D, Fountzilas G, Aravantinos G, Kalofonos C, Efstathiou H, Farmakis D, Skarlos D, Pavlidis N, Economopoulos T, Dimopoulos MA. Advanced stage clear-cell epithelial ovarian cancer: the Hellenic Cooperative Oncology Group experience. Gynecol Oncol. 2006;102:285–291. doi: 10.1016/j.ygyno.2005.12.038. [DOI] [PubMed] [Google Scholar]
- 34.Veras E, Mao TL, Ayhan A, Ueda S, Lai H, Hayran M, Shih Ie M, Kurman RJ. Cystic and adenofibromatous clear cell carcinomas of the ovary: distinctive tumors that differ in their pathogenesis and behavior: a clinicopathologic analysis of 122 cases. Am J Surg Pathol. 2009;33:844–853. doi: 10.1097/PAS.0b013e31819c4271. [DOI] [PubMed] [Google Scholar]
- 35.Kobayashi H, Sumimoto K, Kitanaka T, Yamada Y, Sado T, Sakata M, Yoshida S, Kawaguchi R, Kanayama S, Shigetomi H, Haruta S, Tsuji Y, Ueda S, Terao T. Ovarian endometrioma--risks factors of ovarian cancer development. European journal of obstetrics, gynecology and reproductive biology. 2008;138:187–193. doi: 10.1016/j.ejogrb.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 36.Fukunaga M, Nomura K, Ishikawa E, Ushigome S. Ovarian atypical endometriosis: its close association with malignant epithelial tumours. Histopathology. 1997;30:249–255. doi: 10.1046/j.1365-2559.1997.d01-592.x. [DOI] [PubMed] [Google Scholar]
- 37.Erzen M, Rakar S, Klancnik B, Syrjanen K. Endometriosis-associated ovarian carcinoma (EAOC): an entity distinct from other ovarian carcinomas as suggested by a nested case-control study. Gynecol Oncol. 2001;83:100–108. doi: 10.1006/gyno.2001.6382. [DOI] [PubMed] [Google Scholar]
- 38.Offman SL, Longacre TA. Clear Cell Carcinoma of the Female Genital Tract (Not Everything Is as Clear as it Seems) Advances in anatomic pathology. 2012;19:296–312. doi: 10.1097/PAP.0b013e31826663b1. [DOI] [PubMed] [Google Scholar]
- 39.DeLair D, Oliva E, Kobel M, Macias A, Gilks CB, Soslow RA. Morphologic spectrum of immunohistochemically characterized clear cell carcinoma of the ovary: a study of 155 cases. The American journal of surgical pathology. 2011;35:36–44. doi: 10.1097/PAS.0b013e3181ff400e. [DOI] [PubMed] [Google Scholar]
- 40.Mostoufizadeh M, Scully RE. Malignant tumors arising in endometriosis. Clin Obstet Gynecol. 1980;23:951–963. [PubMed] [Google Scholar]
- 41.Heaps JM, Nieberg RK, Berek JS. Malignant neoplasms arising in endometriosis. Obstetrics and gynecology. 1990;75:1023–1028. [PubMed] [Google Scholar]
- 42.DePriest PD, Banks ER, Powell DE, van Nagell JR, Jr, Gallion HH, Puls LE, Hunter JE, Kryscio RJ, Royalty MB. Endometrioid carcinoma of the ovary and endometriosis: the association in postmenopausal women. Gynecologic Oncology. 1992;47:71–75. doi: 10.1016/0090-8258(92)90079-x. [DOI] [PubMed] [Google Scholar]
- 43.Eifel P, Hendrickson M, Ross J, Ballon S, Martinez A, Kempson R. Simultaneous presentation of carcinoma involving the ovary and the uterine corpus. Cancer. 1982;50:163–170. doi: 10.1002/1097-0142(19820701)50:1<163::aid-cncr2820500131>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 44.Zaino RJ, Unger ER, Whitney C. Synchronous carcinomas of the uterine corpus and ovary. Gynecologic Oncology. 1984;19:329–335. doi: 10.1016/0090-8258(84)90200-2. [DOI] [PubMed] [Google Scholar]
- 45.Ulbright TM, Roth LM. Metastatic and independent cancers of the endometrium and ovary: a clinicopathologic study of 34 cases. Hum Pathol. 1985;16:28–34. doi: 10.1016/s0046-8177(85)80210-0. [DOI] [PubMed] [Google Scholar]
- 46.Kline RC, Wharton JT, Atkinson EN, Burke TW, Gershenson DM, Edwards CL. Endometrioid carcinoma of the ovary: retrospective review of 145 cases. Gynecologic Oncology. 1990;39:337–346. doi: 10.1016/0090-8258(90)90263-k. [DOI] [PubMed] [Google Scholar]
- 47.Falkenberry SS, Steinhoff MM, Gordinier M, Rappoport S, Gajewski W, Granai CO. Synchronous endometrioid tumors of the ovary and endometrium. A clinicopathologic study of 22 cases. J Reprod Med. 1996;41:713–718. [PubMed] [Google Scholar]
- 48.Rutgers JL, Scully RE. Ovarian mullerian mucinous papillary cystadenomas of borderline malignancy. A clinicopathologic analysis. Cancer. 1988;61:340–348. doi: 10.1002/1097-0142(19880115)61:2<340::aid-cncr2820610225>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 49.Kim KR, Choi J, Hwang JE, Baik YA, Shim JY, Kim YM, Robboy SJ. Endocervical-like (Mullerian) mucinous borderline tumours of the ovary are frequently associated with the KRAS mutation. Histopathology. 2010;57:587–596. doi: 10.1111/j.1365-2559.2010.03673.x. [DOI] [PubMed] [Google Scholar]
- 50.Fukunaga M, Ushigome S. Epithelial metaplastic changes in ovarian endometriosis. Modern pathology : an official journal of the United States and Canadian Academy of Pathology Inc. 1998;11:784–788. [PubMed] [Google Scholar]
- 51.Yasunaga M, Ohishi Y, Oda Y, Misumi M, Iwasa A, Kurihara S, Nishimura I, Okuma E, Kobayashi H, Wake N, Tsuneyoshi M. Immunohistochemical characterization of mullerian mucinous borderline tumors: possible histogenetic link with serous borderline tumors and low-grade endometrioid tumors. Hum Pathol. 2009;40:965–974. doi: 10.1016/j.humpath.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 52.Vang R, Gown AM, Barry TS, Wheeler DT, Ronnett BM. Ovarian atypical proliferative (borderline) mucinous tumors: gastrointestinal and seromucinous (endocervical-like) types are immunophenotypically distinctive. International journal of gynecological pathology : official journal of the International Society of Gynecological Pathologists. 2006;25:83–89. doi: 10.1097/01.pgp.0000177125.31046.fd. [DOI] [PubMed] [Google Scholar]
- 53.Vercellini P, Crosignani P, Somigliana E, Vigano P, Buggio L, Bolis G, Fedele L. The ‘incessant menstruation’ hypothesis: a mechanistic ovarian cancer model with implications for prevention. Hum Reprod. 2011;26:2262–2273. doi: 10.1093/humrep/der211. [DOI] [PubMed] [Google Scholar]
- 54.Yamaguchi K, Mandai M, Toyokuni S, Hamanishi J, Higuchi T, Takakura K, Fujii S. Contents of endometriotic cysts, especially the high concentration of free iron, are a possible cause of carcinogenesis in the cysts through the iron-induced persistent oxidative stress. Clinical cancer research : an official journal of the American Association for Cancer Research. 2008;14:32–40. doi: 10.1158/1078-0432.CCR-07-1614. [DOI] [PubMed] [Google Scholar]
- 55.Kuo KT, Mao TL, Jones S, Veras E, Ayhan A, Wang TL, Glas R, Slamon D, Velculescu VE, Kuman RJ, Shih Ie M. Frequent activating mutations of PIK3CA in ovarian clear cell carcinoma. Am J Pathol. 2009;174:1597–1601. doi: 10.2353/ajpath.2009.081000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yamamoto S, Tsuda H, Takano M, Tamai S, Matsubara O. PIK3CA mutations and loss of ARID1A protein expression are early events in the development of cystic ovarian clear cell adenocarcinoma. Virchows Archiv : an international journal of pathology. 2012;460:77–87. doi: 10.1007/s00428-011-1169-8. [DOI] [PubMed] [Google Scholar]
- 57.Ho CM, Lin MC, Huang SH, Huang CJ, Lai HC, Chien TY, Chang SF. PTEN promoter methylation and LOH of 10q22–23 locus in PTEN expression of ovarian clear cell adenocarcinomas. Gynecol Oncol. 2009;112:307–313. doi: 10.1016/j.ygyno.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 58.Cho KR, Shih IM. Ovarian cancer. Annu Rev Pathol Mech Dis. 2009;4:287–313. doi: 10.1146/annurev.pathol.4.110807.092246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yamaguchi K, Mandai M, Oura T, Matsumura N, Hamanishi J, Baba T, Matsui S, Murphy SK, Konishi I. Identification of an ovarian clear cell carcinoma gene signature that reflects inherent disease biology and the carcinogenic processes. Oncogene. doi: 10.1038/onc.2009.470. [DOI] [PubMed] [Google Scholar]
- 60.Mandai M, Yamaguchi K, Matsumura N, Baba T, Konishi I. Ovarian cancer in endometriosis: molecular biology, pathology, and clinical management. International journal of clinical oncology / Japan Society of Clinical Oncology. 2009;14:383–391. doi: 10.1007/s10147-009-0935-y. [DOI] [PubMed] [Google Scholar]
- 61.Wu R, Hendrix-Lucas N, Kuick R, Zhai Y, Schwartz DR, Akyol A, Hanash S, Misek DE, Katabuchi H, Williams BO, Fearon ER, Cho KR. Mouse model of human ovarian endometrioid adenocarcinoma based on somatic defects in the Wnt/beta-catenin and PI3K/Pten signaling pathways. Cancer Cell. 2007;11:321–333. doi: 10.1016/j.ccr.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 62.Catasus L, Bussaglia E, Rodrguez I, Gallardo A, Pons C, Irving JA, Prat J. Molecular genetic alterations in endometrioid carcinomas of the ovary: similar frequency of beta-catenin abnormalities but lower rate of microsatellite instability and PTEN alterations than in uterine endometrioid carcinomas. Hum Pathol. 2004;35:1360–1368. doi: 10.1016/j.humpath.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 63.Liu J, Albarracin CT, Chang KH, Thompson-Lanza JA, Zheng W, Gershenson DM, Broaddus R, Luthra R. Microsatellite instability and expression of hMLH1 and hMSH2 proteins in ovarian endometrioid cancer, Modern pathology : an official journal of the United States and Canadian Academy of Pathology. Inc. 2004;17:75–80. doi: 10.1038/modpathol.3800017. [DOI] [PubMed] [Google Scholar]
- 64.Wiegand KC, Shah SP, Al-Agha OM, Zhao Y, Tse K, Zeng T, Senz J, McConechy MK, Anglesio MS, Kalloger SE, Yang W, Heravi-Moussavi A, Giuliany R, Chow C, Fee J, Zayed A, Prentice L, Melnyk N, Turashvili G, Delaney AD, Madore J, Yip S, McPherson AW, Ha G, Bell L, Fereday S, Tam A, Galletta L, Tonin PN, Provencher D, Miller D, Jones SJ, Moore RA, Morin GB, Oloumi A, Boyd N, Aparicio SA, Shih Ie M, Mes-Masson AM, Bowtell DD, Hirst M, Gilks B, Marra MA, Huntsman DG. ARID1A mutations in endometriosis-associated ovarian carcinomas. The New England journal of medicine. 2010;363:1532–1543. doi: 10.1056/NEJMoa1008433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jones S, Li M, Parsons DW, Zhang X, Wesseling J, Kristel P, Schmidt MK, Markowitz S, Yan H, Bigner D, Hruban RH, Eshleman JR, Iacobuzio-Donahue CA, Goggins M, Maitra A, Malek SN, Powell S, Vogelstein B, Kinzler KW, Velculescu VE, Papadopoulos N. Somatic mutations in the chromatin remodeling gene ARID1A occur in several tumor types. Hum Mutat. 2012;33:100–103. doi: 10.1002/humu.21633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Imielinski M, Berger AH, Hammerman PS, Hernandez B, Pugh TJ, Hodis E, Cho J, Suh J, Capelletti M, Sivachenko A, Sougnez C, Auclair D, Lawrence MS, Stojanov P, Cibulskis K, Choi K, de Waal L, Sharifnia T, Brooks A, Greulich H, Banerji S, Zander T, Seidel D, Leenders F, Ansen S, Ludwig C, Engel-Riedel W, Stoelben E, Wolf J, Goparju C, Thompson K, Winckler W, Kwiatkowski D, Johnson BE, Janne PA, Miller VA, Pao W, Travis WD, Pass HI, Gabriel SB, Lander ES, Thomas RK, Garraway LA, Getz G, Meyerson M. Mapping the hallmarks of lung adenocarcinoma with massively parallel sequencing. Cell. 2012;150:1107–1120. doi: 10.1016/j.cell.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Guan B, Wang TL, Shih Ie M. ARID1A, a factor that promotes formation of SWI/SNF-mediated chromatin remodeling, is a tumor suppressor in gynecologic cancers. Cancer research. 2011;71:6718–6727. doi: 10.1158/0008-5472.CAN-11-1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Guan B, Gao M, Wu CS, Wang TL, Shih Ie M. Functional analysis of in-frame indel ARID1A mutations reveals new regulatory mechanisms of its tumor suppressor functions. Noplasia. 2012 doi: 10.1593/neo.121218. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lowery WJ, Schildkraut JM, Akushevich L, Bentley R, Marks JR, Huntsman D, Berchuck A. Loss of ARID1A-associated protein expression is a frequent event in clear cell and endometrioid ovarian cancers. International journal of gynecological cancer : official journal of the International Gynecological Cancer Society. 2012;22:9–14. doi: 10.1097/IGC.0b013e318231f140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wu CH, Mao TL, Vang R, Ayhan A, Wang TL, Kurman RJ, Shih IM. Endocervical-type mucinous borderline tumors are related to endometrioid tumors based on mutation and loss of expression of ARID1A. Int J Gyn Pathol. 2012;31:297–303. doi: 10.1097/PGP.0b013e31823f8482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wiegand KC, Lee AF, Al-Agha OM, Chow C, Kalloger SE, Scott DW, Steidl C, Wiseman SM, Gascoyne RD, Gilks B, Huntsman DG. Loss of BAF250a (ARID1A) is frequent in high-grade endometrial carcinomas. The Journal of pathology. 2011;224:328–333. doi: 10.1002/path.2911. [DOI] [PubMed] [Google Scholar]
- 72.Maeda D, Mao TL, Fukayama M, Nakagawa S, Yano T, Taketani Y, Shih Ie M. Clinicopathological Significance of Loss of ARID1A Immunoreactivity in Ovarian Clear Cell Carcinoma. Int J Mol Sci. 2010;11:5120–5128. doi: 10.3390/ijms11125120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yamamoto S, Tsuda H, Takano M, Tamai S, Matsubara O. Loss of ARID1A protein expression occurs as an early event in ovarian clear-cell carcinoma development and frequently coexists with PIK3CA mutations. Mod Pathol. 2012;25:615–624. doi: 10.1038/modpathol.2011.189. [DOI] [PubMed] [Google Scholar]
- 74.Ayhan A, Mao TL, Seckin T, Wu CH, Guan B, Ogawa H, Futagami M, Mizukami H, Yokoyama Y, Kurman RJ, Shih IM. Loss of ARID1A Expression Is an Early Molecular Event in Tumor Progression From Ovarian Endometriotic Cyst to Clear Cell and Endometrioid Carcinoma. International journal of gynecological cancer : official journal of the International Gynecological Cancer Society. 2012 doi: 10.1097/IGC.0b013e31826b5dcc. [DOI] [PMC free article] [PubMed] [Google Scholar]