Introduction
Otosclerosis is a localized bone disease, which affects only the endochondral bone of the otic capsule in humans. On histology, foci of disordered bone resorption, new bone deposition, vascular proliferation, and/or connective tissue stroma are seen [1]. Otosclerosis may cause a conductive, mixed, or rarely, pure sensorineural hearing loss. Clinical diagnosis is based on history, physical exam findings, and audiometry, and may be supported by imaging studies.
High resolution computed tomography (CT) is the imaging modality of choice for otosclerosis [2], because of the ability to detect pathologic bone lesions in and around the stapes footplate, cochlea, and labyrinth. On CT, otosclerosis appears as a lucent or hypodense focus within the otic capsule, most commonly anterior to the oval window. Other CT findings in otosclerosis include a thickened footplate, narrowed oval window or round window niche, and the double ring sign (a hypodense lesion surrounding the cochlea) [3, 4].
Clinicians may utilize high resolution CT in the diagnostic evaluation of otosclerosis, determination of the extent of disease, or planning prior to medical or surgical treatment. Many authors have evaluated the sensitivity of CT for these purposes over the last several decades [3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13]. Contemporary studies report greater than 90% sensitivity using modern high resolution CT for the diagnosis of otosclerosis [5, 6]. All of these studies rely on comparison of CT findings to clinical data, including history, physical exam, audiometry, and/or surgical findings. There is only one published case report directly comparing CT findings to histology in the same temporal bone, in which a large pericochlear focus of otosclerosis seen on histology was not apparent on CT [14].
Histologic evaluation enables confirmation of the diagnosis of otosclerosis, and is the gold standard for determination of the extent of the disease process. The goal of this study was to evaluate the sensitivity of CT for the diagnosis of otosclerosis by comparison of imaging to pathology on temporal bone specimens. We also evaluated the ability of CT to identify otosclerotic foci in various locations of the otic capsule, to determine involvement of the endosteal layer of the cochlea, and to identify round and oval window obliteration. The goal was to provide clinically relevant information that improves understanding of the uses and limitations of CT in the management of otosclerosis.
Methods
Imaging
High resolution CT imaging was obtained on all temporal bones after extirpation and prior to histologic preparation. The temporal bone was mounted in a custom designed plastic holder to allow for proper orientation and avoid artifact. Previous experiments have shown that the holder did not significantly affect image quality. Images were obtained with a 40-slice multidetector CT scanner (SOMATOM Sensation; Siemens), with 0.6mm collimation, 0.55 pitch, 320 mAs and 120 kVp. From this raw data, images were generated in 0.6 mm slice thickness with 0.1 mm overlap (i.e. 0.5mm increments) with a FOV of 85 and matrix of 512×512. These are the same settings that are used clinically for temporal bone protocol high resolution thin slice multidetector CT imaging. The axial data were then transferred to a separate workstation for postprocessing, with a commercially available 3D reformatting software (Voxar 3D; Barco, Edinburgh, Scotland). Reformatted images were made in an axial plane in the same orientation of the histology sections which had been uploaded to the Radiology PACS system.
Histology
Temporal bones with available CT imaging from the collections at the Massachusetts Eye and Ear Infirmary (MEEI) were examined by light microscopy after standard processing. Standard processing consists of fixation in formalin, CT imaging, and then and decalcification using ethylenediamine tetraacetic acid (EDTA). The specimens are then embedded in celloidin and serial sectioned in the horizontal plane at a section thickness of 20 microns. Every tenth section is stained with hematoxylin and eosin, and mounted on a glass slide [15].
Evaluation of ability to diagnose otosclerosis
In the first part of the study, all temporal bones from the MEEI collections with otosclerosis on histology and available CT imaging were included. The eight temporal bones with evidence of prior stapedectomy were excluded to avoid bias by reviewers, leaving a total of 10 specimens for this portion of the study. Thirty six temporal bones with available CT imaging and no evidence of otosclerosis on histology were included as controls. The CT scans from the temporal bones with and without evidence of otosclerosis on histology were presented to two neuroradiologists in random order. The radiologists were blinded to the histologic evaluations. The radiologists were asked to determine whether the diagnosis of otosclerosis was likely based on CT findings. Comparative densitometry measurements were utilized by the radiologists at their discretion, as would be done in clinical practice. Each radiologist recorded his or her individual opinion on all 46 specimens, and there was agreement in 44 cases. For the two discrepancies, a consensus opinion was reached and used as the recorded outcome in the study.
Evaluation of extent of otosclerosis, endosteal margin involvement, and obliteration of the oval and round window niches
In the following parts of the study, all 18 temporal bones from the MEEI collection with otosclerosis on histology and available CT imaging were included. In contrast to the first part of the study, specimens that had undergone stapedectomy in life were included, and radiologists were aware of the histopathologic diagnosis of otosclerosis in these 18 specimens. The radiologists were blinded, however, to the specific questions that were evaluated, as described below.
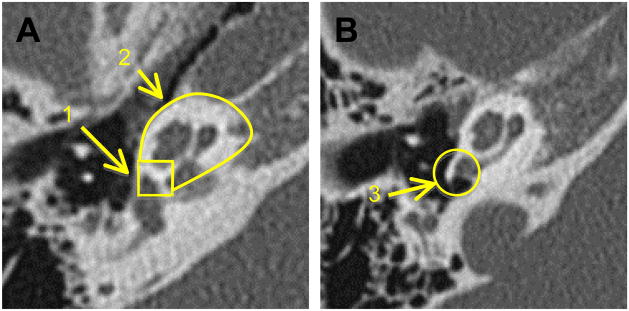
Three anatomic regions, or zones, with clinical relevance were defined in order to simplify the description of the anatomical extent of the disease (Figure 1). Zone 1 was defined as the region anterior to the oval window, including the area of the fissula antefenestra. Disease in this area is often called fenestral otosclerosis on imaging. Zone 2 was defined as the pericochlear region, consisting of otic capsule bone surrounding the cochlea. Zone 3 was defined as the round window niche, including the round window membrane and surrounding otic capsule bone. Zones 2 and 3 are often called retrofenestral otosclerosis on imaging.
Figure 1.
Areas of the otic capsule that are clinically relevant for the study of otosclerosis were divided into 3 zones, as depicted. Zone 1 is the area anterior to the oval window. Zone 2 is the pericochlear area. Zone 3 is the round window niche.
In the second part of the study, histology was compared to imaging in specific regions of the otic capsule. Histologic sections from each temporal bone with otosclerosis were reviewed to determine the extent of otosclerosis, as defined by the three zones. In this second part of the study, radiologists were aware of the diagnosis of otosclerosis based on histology, but were blinded to the extent and locations of foci of otosclerosis determined on histologic evaluation. Two radiologists reviewed the CT scans for each temporal bone, in random order, and reported their consensus opinion on the extent of otosclerosis as defined by the three zones.
In the third part of the study, histologic sections from each temporal bone with otosclerosis were reviewed to determine whether the focus or foci of otosclerosis reached the endosteal margin of the cochlea. The exact location of endosteal margin involvement on histology was also noted. The CT images were then reviewed for endosteal margin involvement and location in a blinded fashion.
In the fourth part of the study, the oval window niche and round window niche were examined on histology, and cases of complete obliteration were noted. Partial obliteration was reported as not obliterated. Temporal bones that had undergone a stapedectomy in life were excluded from the evaluation of oval window obliteration, in order to avoid confusion with post-surgical changes in the oval window. The CT from each temporal bone was reviewed by radiologists who were aware of the diagnosis of otosclerosis, but blinded to the histologic review of oval and round window niche obliteration.
Results
Evaluation of ability to diagnose otosclerosis
There were 10 temporal bones with otosclerosis evident on histology and 36 controls without otosclerosis on histology included in the blinded, randomized review (Table 1). Eight of the 10 temporal bones with otosclerosis (80%) had CT findings consistent with otosclerosis. In these specimens, the presumed focus of otosclerosis identified on an axial CT image was compared to the corresponding histologic section, which confirmed the diagnosis. An example is shown in Figure 2. Two of the 10 temporal bones with otosclerosis (20%) were not given a diagnosis of otosclerosis based on the CT, i.e. had a false negative diagnosis. Three of the 36 control specimens without otosclerosis on histology (8%) had CT findings consistent with a diagnosis of otosclerosis, i.e. had a false positive diagnosis of otosclerosis based on CT alone (Figure 3). The CT images and corresponding histologic slides of each of these three false positive cases were examined. All three false positive radiologic diagnoses were based on a hypodense region anterior to the oval window, thought to be a focus of otosclerosis. On histology, all three temporal bones had an area anterior to the footplate that contained increased amounts of connective tissue and vessels.
Table 1.
Diagnosis of otosclerosis on radiology and histology, reported as “yes” or “no”.
| Histology | |||
|---|---|---|---|
| Yes | No | ||
| Radiology | Yes | 8 | 3 |
| No | 2 | 33 | |
| Total | 10 | 36 | |
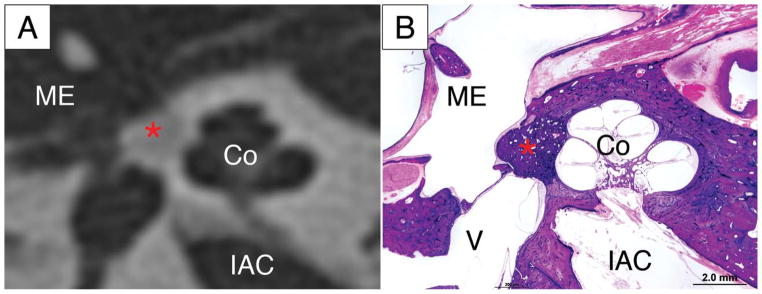
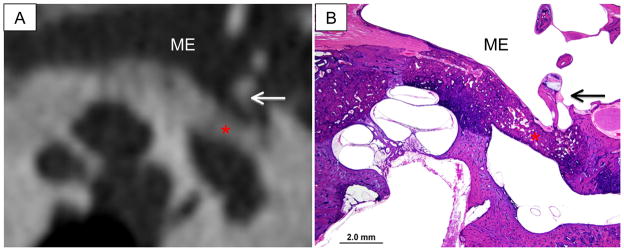
Figure 2.
The radiologic diagnosis of otosclerosis is confirmed on histology. A lucent area anterior to the oval window (*) on high resolution CT (A) matches the focus of otosclerosis (*) seen on the corresponding histologic slide, imaged at low power with light microscopy (B). Co-cochlea, ME-middle ear, IAC – internal auditory canal, V -vestibule
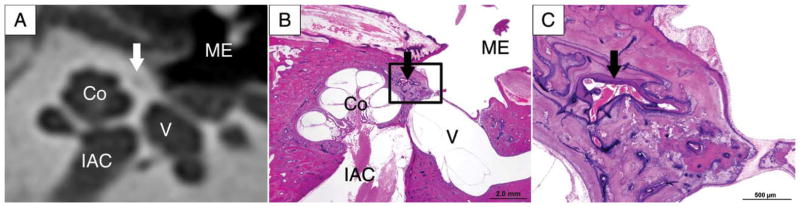
Figure 3.
A false positive CT for diagnosis of otosclerosis is shown in A, with a lucent area seen anterior to the oval window (arrow). The corresponding histology slide is shown in low power (B) and high power (C). There is no otosclerosis, but there is an area (arrow) of connective tissue and vessels at the junction of the endochondral and perichondral bone. Co-cochlea, ME-middle ear, IAC – internal auditory canal, V -vestibule
Evaluation of extent of otosclerosis, endosteal margin involvement, and obliteration of the oval and round window niches
There were 18 temporal bones from 11 patients with available CT imaging and otosclerosis on histology (Table 2). In zone 1, the area anterior to the oval window, 17 out of 18 bones had a focus of otosclerosis on histology. All 17 of these foci were identified on the corresponding CT images. Eleven temporal bones had a focus of otosclerosis in zone 2 (pericochlear region) on histology, and nine (82%) of these foci were apparent on CT. A focus of otosclerosis in zone 3 (round window niche) was apparent on 3 out of 6 (50%) temporal bones with foci seen on corresponding histology. In all three cases when the zone 3 lesion was not identified on CT, the focus of otosclerosis was very small.
Table 2.
Comparison of CT findings and histology for 18 temporal bones with otosclerosis. Evidence of otosclerosis is reported as “yes” or “no”, with radiology (Rad) findings to the left of the slash and histology(Histo)findings to the right of the slash. Discrepancies are highlighted in gray and bold type.
| Pt ID | Side | Zone 1: Anterior to the OW? (Rad/Histo) | Zone 2: Pericochlear? (Rad/Histo) | Zone 3: In the RW niche? (Rad/Histo) |
|---|---|---|---|---|
| 1 | R | yes / yes | no / yes | no / no |
| 1 | L | no / no | no / yes | no / no |
| 2 | R | yes / yes | yes / yes | yes / yes |
| 2 | L | yes / yes | yes / yes | yes / yes |
| 3 | R | yes / yes | yes / yes | no / no |
| 3 | L | yes / yes | yes / yes | no / no |
| 4 | R | yes / yes | no / no | no / no |
| 4 | L | yes / yes | no / no | no / no |
| 5 | L | yes / yes | yes / yes | yes / yes |
| 6 | L | yes / yes | no / no | no / yes |
| 7 | R | yes / yes | no / no | no / no |
| 7 | L | yes / yes | no / no | no / no |
| 8 | R | yes / yes | yes / yes | no / no |
| 8 | L | yes / yes | yes / yes | no / yes |
| 9 | R | yes / yes | no / no | no / yes |
| 10 | L | yes / yes | no / no | no / no |
| 11 | R | yes / yes | yes / yes | no / no |
| 11 | L | yes / yes | yes / yes | no / no |
Eight of the 18 temporal bones had a focus of otosclerosis in zone 1 that reached the endosteal margin of the cochlea on one or more histologic sections (Table 3 and Figure 4A,B,C). On CT imaging, 5 of these 8 (63%) temporal bones with endosteal margin involvement were identified, and one of the 8 temporal bones was indeterminant on CT. Two of the 8 (25%) temporal bones with endosteal margin involvement had false negative diagnoses, in which the focus of otosclerosis did not appear to reach the endosteal margin on CT (Figure 4D,E,F).
Table 3.
Temporal bones with both CT and otopathology available were reviewed for the four questions listed below. The answers are reported as “yes” or “no”, with radiology (Rad) findings to the left of the slash and histology(Histo)findings to the right of the slash.
| Pt ID | Side | Does otosclerosis reach the endosteal margin anterior to the OW (Zone 1)? (Rad/Histo) | Does otosclerosis reach the endosteal margin in pericochlear area (Zone 2)? (Rad/Histo) | Is the OW obliterated? (Rad/Histo) | Is the RW obliterated? (Rad/Histo) |
|---|---|---|---|---|---|
| 1 | R | no / no | - / no | no / no | no / no |
| 1 | L | - / - | - / no | N/A | no / no |
| 2 | R | yes / yes | yes /yes | N/A | yes / yes |
| 2 | L | yes / yes | yes / yes | yes / yes | no / no |
| 3 | R | no / yes | no / no | N/A | no / no |
| 3 | L | no / no | no / no | N/A | no / no |
| 4 | R | no / no | - / - | N/A | no / no |
| 4 | L | no / no | - / - | no / no | no / no |
| 5 | L | yes / yes | yes /yes | yes / yes | yes / yes |
| 6 | L | no / no | - / - | N/A | no / no |
| 7 | R | no / no | - / - | N/A | no / no |
| 7 | L | no / no | - / - | no / no | no / no |
| 8 | R | indeter / yes | no / no | no / no | no / no |
| 8 | L | yes / yes | yes / yes | no / no | no / no |
| 9 | R | no / no | - / - | no / no | no / no |
| 10 | L | no / no | - / - | no / no | no / no |
| 11 | R | no / yes | no / no | no / no | no / no |
| 11 | L | yes / yes | no / no | N/A | no / no |
Discrepancies are highlighted in gray and bold type.
“-“ means not applicable because the radiologist or pathologist did not identify any focus of otosclerosis and therefore the question does not apply.
“N/A” (not applicable) is entered for bones that had undergone a stapedectomy during life, and therefore oval window obliteration could not be assessed.
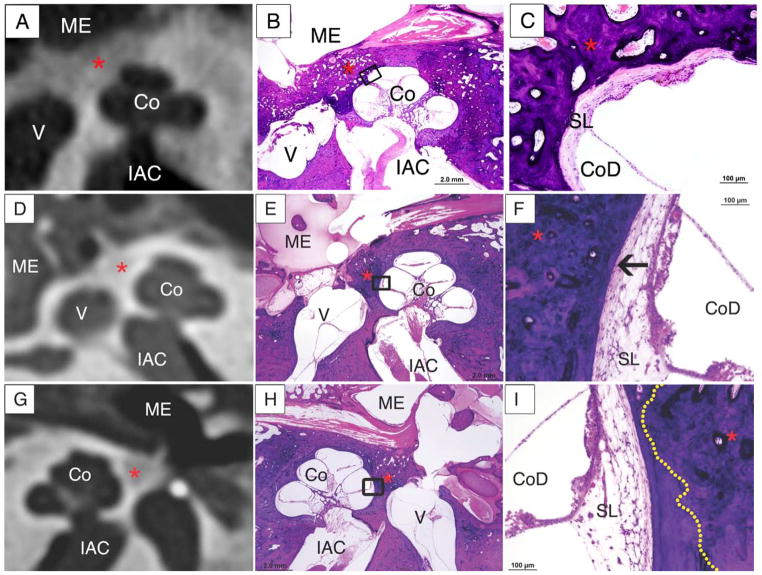
Figure 4.
Evaluation of endosteal margin involvement.
A, B, C: Endosteal margin involvement by otosclerosis (*) is seen on the CT (A), and confirmed on the corresponding histologic slide, shown in low (B) and high (C) magnification. The high power image (C) shows endosteal margin involvment with adjacent spiral ligament hyalinization (arrow).
D,E,F: The CT image (D) fails to demonstrate endosteal margin involvement by the focus of otosclerosis(*). Endosteal margin involvement is seen in the low power (E) and high power (F) photomicrographs of the corresponding histologic slide. In C, an arrow points to hyalinization of the spiral ligament associated with the focus of otosclerosis at the endosteal margin.
G,H,I: The CT image (G) shows absence of endosteal margin involvement, which is confirmed on low (H) and high power (I) photomicrographs. In F, the dotted yellow line represents the border of the focus of otosclerosis, which does not involve the endosteal margin.
Co-cochlea, ME-middle ear, IAC – internal auditory canal, V -vestibule
There were four temporal bones with endosteal margin involvement from a zone 2 (pericochlear) focus of otosclerosis, and notably these were all relatively large foci. CT imaging reported endosteal margin involvement in all four of these bones (Table 3). For all 10 temporal bones without endosteal margin involvement on histology, the CT findings were accurate (Figure 4G,H,I).
Two specimens had oval window obliteration on histology, and these were both identified as cases of obliteration on CT (Figure 5). Two specimens had complete round window obliteration on histology, and both were identified on CT (Table 3).
Figure 5.
Complete obliteration of the oval window by otosclerosis (*) was identified on review of the CT imaging, and is demonstrated by a representative CT image (A). The corresponding histopathology in low power (B) shows a focus of otosclerosis (*)that extends across the entire oval window and has caused marked thickening of the stapes footplate. ME-middle ear, Arrow – stapes suprastructure
Discussion
Many previous studies have examined the sensitivity of CT for the diagnosis of otosclerosis using clinical data for comparison [2, 3, 5, 6, 8, 9, 10, 12, 13]. All of these studies compared CT evaluations to history and physical exam, audiometric data, and/or intraoperative findings. Typical audiometric findings may be absent early in the course of the disease or may not be bothersome enough to the patient to prompt evaluation. Surgical intervention allows the opportunity to confirm stapes fixation and/or gross plaques consistent with otosclerosis. While intraoperative findings are reliable for confirming the diagnosis of otosclerosis, only patients with disease that has progressed enough to merit surgical intervention and patients that elect surgery can be included in such studies. Clinical data has been used for comparison to CT findings in otosclerosis since it is not possible to evaluate histology of the otic capsule during life.
This study compares CT imaging on a series of temporal bone specimens with otosclerosis to histology of the same temporal bones. Histology is the most accurate way to determine the diagnosis of otosclerosis. It allows confirmation of the diagnosis even when the disease has not caused typical audiometric findings, and has not led to surgical intervention. Comparison of CT findings to histology allows evaluation of temporal bones with otosclerosis at all stages in the disease course. The extent of the disease determined on CT and histology can be compared because individual foci of otosclerosis can be specifically examined. Furthermore, direct comparison of the CT image to the corresponding histologic slide provides information on why CT evaluations may differ from histology.
In this study, the sensitivity of CT for the diagnosis of otosclerosis when compared to histology was 80%. Several contemporary studies, that compared CT findings to clinical data, found the sensitivity of CT to be greater than 90% for the diagnosis of otosclerosis [5, 6]. This small difference may be accounted for by the limited number of temporal bones with otosclerosis that met inclusion criteria for the study. Additionally, one missed diagnosis in this study occurred in a patient with a small, subtle focus of otosclerosis in the pericochlear region, and no otosclerosis anterior to the oval window. This patient with early histologic otosclerosis would not have been included in studies comparing radiology to clinical data because she had no associated hearing loss. Regardless, comparison of CT to histology provides the most compelling data as histology is the gold standard for determining the presence or absence of the disease process.
An unanticipated finding from this study was the false positive radiologic diagnosis of otosclerosis in three temporal bones due to areas of connective tissue and vessels anterior to the oval window. The findings in these three control temporal bones possibly represent a variant of normal histology. Otologists and radiologists should be aware that a lucency in the antefenestral area is not always due to otosclerosis,.
The sensitivity of CT for identifying otosclerotic foci in various locations around the otic capsule was highest in the area anterior to the oval window (zone 1) and lowest in the round window niche (zone 3). Because, in this phase of the study, radiologists were aware of the diagnosis of otosclerosis (though blinded to the location), they may have been biased toward a positive finding of otosclerosis for zone 1 since this is the most common location for otosclerosis. The higher rate of missed foci in the round window niche is partly due to the extremely small size of foci at that location in three of the temporal bones. These small foci of otosclerosis would not be expected to have any clinical sequelae, and thus failure to identify tiny foci of otosclerosis at the RW niche on the CT would not impact clinical management. Additionally, slight differences in the plane of tissue between a CT slice and the best corresponding histologic slide may lead to discrepancies with identification of very small foci.
When otosclerosis reaches the endosteal margin of the cochlea, deposition of a hyalin material in the spiral ligament may ensue and cause sensorineural hearing loss[1, 16]. Identification of patients with otosclerosis in whom the sensorineural component is due to otosclerosis is important for patient counseling. In the future, identifying these patients may become essential as medical therapies (e.g. bisphosphonate treatment) for otosclerosis-related sensorineural hearing loss are developed. Multiple authors have compared CT findings with audiometry to determine whether endosteal margin involvement is associated with otosclerosis-related sensorineural hearing loss[3, 5, 6, 8, 12, 13]. The average bone conduction threshold among patients with endosteal involvement on CT has been found to be significantly elevated compared to those without endosteal involvement[5, 6]. This implies generally good correlation between positive findings of endosteal involvement on CT and the pathology leading to sensorineural hearing loss. The present study confirms excellent correlation: all temporal bones with endosteal margin involvement on CT demonstrated endosteal margin involvement on histology. Guneri et. al detected radiolucent areas in 45% of patients suspected to have cochlear otosclerosis by history and audiometry[13]. This poor correlation could be attributed to an error in the diagnosis of cochlear otosclerosis or failure of the CT to detect radiolucent foci with endosteal margin involvement. In the present study, the false negative rate for endosteal margin involvement on CT was 37% (3/8), which would help explain the poor correlation in the study by Guneri et al. Thus, CT may be used to confirm endosteal margin involvement, but is not as accurate in ruling out involvement.
Although the protocol used for imaging these temporal bones was as close to clinical standards as possible, technical issues related to imaging of a temporal bone in isolation may have altered the quality of images obtained. The CT images were examined at the orientation which best matched the histological sections but which may not have been the most optimal angle to visualize subtle otosclerotic changes. Additionally, there was some minor artifact related to fixation material. The images were also slightly degraded due to presence of air in soft tissue structures.
Conclusions
High resolution temporal bone CT is highly sensitive and specific for the diagnosis of otosclerosis when compared to histopathology. Most otosclerotic foci can be detected on CT with current technology, but the sensitivity appears to vary by size and quality of the otosclerotic focus. Otologists and radiologists should be aware that not all hypodense lesions in the antefenestral area represent otosclerosis. Positive endosteal margin involvement on CT was confirmed by pathology, but absence of endosteal margin involvement on CT is not as reliable.
Acknowledgments
The authors wish to thank Jon Pack and Garyfallia Pagonis for their assistance in capturing the photomicrographs and creating the figures.
Footnotes
Funding Disclosure: This work was supported by NIH grant U24DC011943 (SNM).
References
- 1.McKenna MJ, Merchant SN. Disorders of Bone. In: Merchant SN, Nadol JB, editors. Schuknecht’s Pathology of the Ear. Shelton, CT: People’s Medical Pub. House-USA Inc; 2010. pp. 716–9. [Google Scholar]
- 2.Berrettini S, Ravecca F, Volterrani D, Neri E, Forli F. Imaging evaluation in otosclerosis: single photon emission computed tomography and computed tomography. Ann Otol Rhinol Laryngol. 2010 Apr;119(4):215–24. doi: 10.1177/000348941011900402. [DOI] [PubMed] [Google Scholar]
- 3.Mafee MF, Valvassori GE, Deitch RL, Norouzi P, Henrikson GC, Capek V, et al. Use of CT in the evaluation of cochlear otosclerosis. Radiology. 1985 Sep;156(3):703–8. doi: 10.1148/radiology.156.3.4023229. [DOI] [PubMed] [Google Scholar]
- 4.Sakai O, Curtin HD, Fujita A, Kakoi H, Kitamura K. Otosclerosis: computed tomography and magnetic resonance findings. Am J Otolaryngol. 2000 Mar-Apr;21(2):116–8. doi: 10.1016/s0196-0709(00)85008-5. [DOI] [PubMed] [Google Scholar]
- 5.Lagleyre S, Sorrentino T, Calmels MN, Shin YJ, Escude B, Deguine O, et al. Reliability of high-resolution CT scan in diagnosis of otosclerosis. Otol Neurotol. 2009 Dec;30(8):1152–9. doi: 10.1097/MAO.0b013e3181c2a084. [DOI] [PubMed] [Google Scholar]
- 6.Shin YJ, Fraysse B, Deguine O, Cognard C, Charlet JP, Sevely A. Sensorineural hearing loss and otosclerosis: a clinical and radiologic survey of 437 cases. Acta Otolaryngol. 2001 Jan;121(2):200–4. doi: 10.1080/000164801300043505. [DOI] [PubMed] [Google Scholar]
- 7.Valvassori GE. Imaging of otosclerosis. Otolaryngol Clin North Am. 1993 Jun;26(3):359–71. [PubMed] [Google Scholar]
- 8.Vartiainen E, Saari T. Value of computed tomography (CT) in the diagnosis of cochlear otosclerosis. Clin Otolaryngol Allied Sci. 1993 Dec;18(6):462–4. doi: 10.1111/j.1365-2273.1993.tb00614.x. [DOI] [PubMed] [Google Scholar]
- 9.Harcourt JP, Lennox P, Phelps PD, Brookes GB. CT screening for temporal bone abnormalities in idiopathic bilateral sensorineural hearing loss. J Laryngol Otol. 1997 Feb;111(2):117–21. doi: 10.1017/s002221510013662x. [DOI] [PubMed] [Google Scholar]
- 10.Mafee MF, Henrikson GC, Deitch RL, Norouzi P, Kumar A, Kriz R, et al. Use of CT in stapedial otosclerosis. Radiology. 1985 Sep;156(3):709–14. doi: 10.1148/radiology.156.3.4023230. [DOI] [PubMed] [Google Scholar]
- 11.Swartz JD, Faerber EN, Wolfson RJ, Marlowe FI. Fenestral otosclerosis: significance of preoperative CT evaluation. Radiology. 1984 Jun;151(3):703–7. doi: 10.1148/radiology.151.3.6718730. [DOI] [PubMed] [Google Scholar]
- 12.Kawase S, Naganawa S, Sone M, Ikeda M, Ishigaki T. Relationship between CT densitometry with a slice thickness of 0.5 mm and audiometry in otosclerosis. Eur Radiol. 2006 Jun;16(6):1367–73. doi: 10.1007/s00330-005-0128-7. [DOI] [PubMed] [Google Scholar]
- 13.Guneri EA, Ada E, Ceryan K, Guneri A. High-resolution computed tomographic evaluation of the cochlear capsule in otosclerosis: relationship between densitometry and sensorineural hearing loss. Ann Otol Rhinol Laryngol. 1996 Aug;105(8):659–64. doi: 10.1177/000348949610500813. [DOI] [PubMed] [Google Scholar]
- 14.Thiers FA, Valvassori GE, Nadol JB., Jr Pathology case of the month: otosclerosis of the cochlear capsule: correlation of computerized tomography and histopathology. Am J Otol. 1999 Jan;20(1):93–5. [PubMed] [Google Scholar]
- 15.Merchant SN. Methods of Removal, Preparation and Study. In: Merchant SN, Nadol JB, editors. Schuknecht’s Pathology of the Ear. Shelton, CT: People’s Medical Pub. House-USA Inc; 2010. pp. 3–51. [Google Scholar]
- 16.Parahy C, Linthicum FH., Jr Otosclerosis and otospongiosis: clinical and histological comparisons. Laryngoscope. 1984 Apr;94(4):508–12. doi: 10.1288/00005537-198404000-00015. [DOI] [PubMed] [Google Scholar]