Biliary reconstruction was long considered the Achilles heel of the liver transplant operation. The refinement in the techniques described by various authors1 has dramatically reduced the incidence of biliary complications. These complications still occur, however, and carry a disproportionately high penalty in terms of morbidity and mortality.2 The obstructive type of these complications sometimes has a very insidious presentation and course that requires a high index of suspicion for a correct diagnosis. Our group favors the end-to-end choledochocholedochostomy (CC) repair whenever feasible.3 Over the past few years, a certain complication of this type of repair, heretofore unreported, has emerged: the diffuse dilatation (DD) of both donor and recipient common bile ducts (CBDs) without any obvious mechanical obstruction.
MATERIALS AND METHODS
During the period from March 1, 1980, to June 30, 1987, 886 patients underwent orthotopic liver transplantation (OLTX) at the University of Pittsburgh Health Center; there were 557 adults (age over 18) and 329 children (aged 18 or under). The biliary reconstruction was performed with a CC in 441 patients (46%) and with a Roux-en-Y choledochojejunostomy (RY) or some other method in 475 patients (54%).
RESULTS
Of the patients who underwent reconstruction by CC, 65 (15.8%) had some significant complication: 23 (35.4%) DD of the CBD without any apparent stricture (ST), 22 (33.8%) bile leaks, and 20 (30.8%) ST.
The time of onset of DD was an average of 34.6 weeks after OLTX (range. 1 to 330 weeks).
The presentation was usually with an elevation of the bilirubin and liver enzyme levels. Some patients had been already treated for presumed rejection with several pulses of intravenous steroids before the bile duct problem was finally diagnosed.
DISCUSSION
In our experience, it appears that the most frequent complication of the CC is DD of the CBD, without any obvious physical obstruction (ST) (Fig 1). The DD develops gradually in the majority of the patients and causes a rather insidious elevation of the levels of serum bilirubin and liver enzymes. Frequently, these changes are interpreted as bouts of rejection and treated with pulses of steroids with variable (but usually incomplete) results. Even the histological presentation, on biopsy specimens, can be misleading because it may mimic rejection or early chronic active hepatitis. The direct study of the CBD by a percutaneous transhepatic cholangiogram (PTC) or endoscopic retrograde cholangiopancreatogram is the best way to diagnose the condition (Fig 2).
Fig 1.
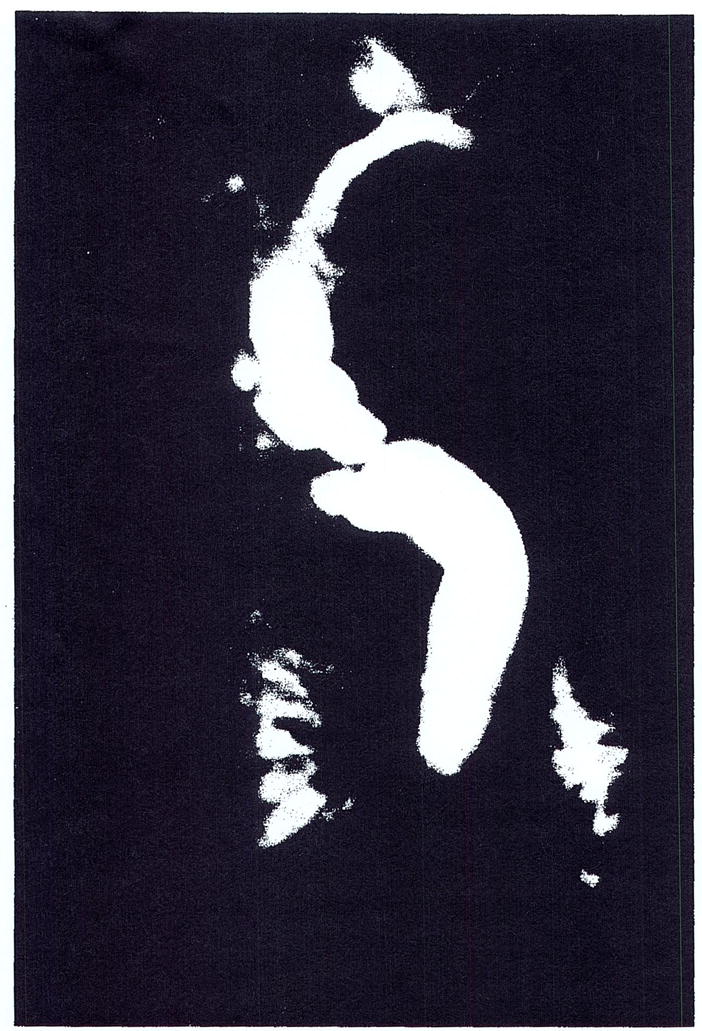
Diffusa dilatation of the CBD. diagnosed by PTC. No obvious stricture of the papilla is apparent.
Fig 2.
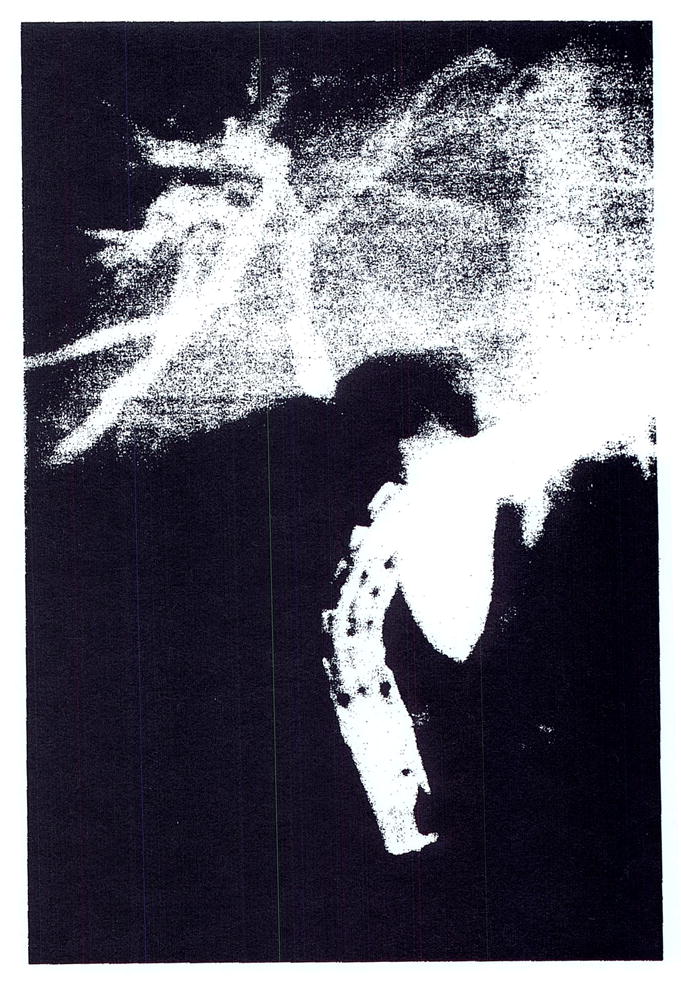
Diffusely dilated CBD by ERCP (the recipient’s duct is more dilated than the donor’s) 6 years after OLTX.
We postulate that the DD is the result of a papillary dyskinesia that is caused by either devascularization or denervation of the papilla of Vater during the recipient hepatectomy. To us, the denervation mechanism seems both more likely and more logical. In this latter case, the result is an outlet obstruction-type of syndrome.
If this holds true, treatment must consist of a decompression procedure; we favor a reconstruction by means of an RY, which we find technically rather simple as well as safe and effective. Only two patients (8.7%) of the ones converted to RY anastomosis had any complication, and this was easily corrected surgically or percutaneously. There was no death in this group. An attempt at balloon dilation after PTC may be helpful in avoiding open surgery. Although endoscopic papillotomy could be advocated by some, it does not appear to be aviable alternative because the length of the involved segment (3 to 4 cm) seems too big for the efficient and safe use of this method.
Finally, if a study could be devised that would permit the identification of those patients who would suffer a denervation of their papillary mechanism during hepatectomy, a primary RY could be directly performed, even in the absence of any other contraindications to CC, in this way avoiding the development of DD at a later time.
References
- 1.Starzl TE, Iwatsuki S, VanThiel D, et al. Hepatology. 1982;2:614. [Google Scholar]
- 2.Lerut J, Gordon RD, Iwatsuki S, et al. Transplantation. 1987;43:47. doi: 10.1097/00007890-198701000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calne RY. In: Liver Transplantation. Calne RY, editor. Philadelphia: Grune & Stratton; 1985. p. 169. [Google Scholar]


