Abstract
Purpose
The purpose of this study was to determine whether changes in Medicare reimbursement for punctal plug insertion were associated with a decrease in the incidence of insertion and dry eye diagnosis.
Methods
Incident cases of dry eye syndrome (DES) diagnoses and punctal plug insertions among Medicare beneficiaries were identified from Medicare 5% Part-B from 1994 to 2008, using a 3 year look-back. DES diagnoses and punctal plug insertion codes were ascertained from the International Classification of Diseases and Current Procedural Terminology codes. Medicare payment data were obtained from the Centers for Medicare and Medicaid Services from 1994-2008 for punctal plug insertion. Rates were calculated for both the incidence of DES and the use of punctal plugs.
Results
From 2001-08, inflation-adjusted Medicare reimbursement for punctal plug insertion decreased 55.1% while the Medicare population-adjusted incidence of dry eye diagnosis increased 23.3%. Nine percent of individuals diagnosed with DES between years 1991-2008 underwent punctal plug placement with a mean of 2.0 plugs placed per patient. Total punctal plug placement increased 322.2% between 1994 and 2003 then reached a plateau. First-time punctal plug insertion rates within 365 days of DES diagnosis increased 111.8% from 1994-2002 then declined 47.0% from 2002-08.
Conclusions
Although the frequency of DES diagnosis in the Medicare population has increased over time, first time punctal plug insertion rates, especially within the first year following DES diagnosis, have declined coincident with the increasing presence of a medical alternative and declining Medicare payment. Choice of therapies may have cost and care implications.
Dry eye syndrome (DES) is a common problem with increased frequency in the older population and women.1 DES consists of disorders of the tear film attributable to reduced tear production or excessive tear evaporation. It is associated with ocular discomfort and/or visual symptoms and may lead to disease of the ocular surface.2 The estimated prevalence of DES in the United States population 50 years of age and older in 2003 was 7.8%, or 3.2 million among women,1 and 4.7% or 1.6 million among men.3 In 2004, more than 15% of persons aged 65+ are estimated to have experienced dry eye symptoms.4
DES is responsible for substantial morbidity, affecting vision-related quality of life and impairing perceived abilities to work, drive, read, and perform other tasks of daily living.5 In a time-tradeoff utility analysis, patients with mild DES experienced a reduction in quality of life similar to those with treated symptomatic human immunodeficiency virus infection, and patients with severe DES experienced a loss in quality of life similar to persons on hemodialysis.6 Although most patients (65-89%) with DES have mild dry eye,7 those with moderate to severe dry eye are also at increased risk for further ocular complications.8-10
Management of DES primarily utilizes topical tear replacement.11, 12 Punctal occlusion is a non-pharmacological therapy for dry eye symptoms insufficiently treated by other methods.2, 11, 13 Permanent silicone or temporary collagen punctal plugs are inserted into the lower, upper, or both puncta, occluding the punctum and thus helping to preserve natural tears by decreasing their efflux through the punctum.11 Punctal plugs have relatively few side effects and are generally well tolerated. Randomized controlled trials have demonstrated their efficacy in reducing dry eye symptoms.13 They are recommended by the American Academy of Ophthalmology Preferred Practice Pattern for treatment of moderate DES.2
DES imposes a substantial burden on patients directly affected and on others, such as health insurers and ultimately, premium and tax payers. Using data from 2,171 US survey respondents aged 18+, Yu et al. estimated the economic burden of DES to be $11,302 per patient (2009 dollars), reflecting both direct cost to the insurers and indirect cost, such as productivity loss.14 Patients undergoing punctal plug procedures (15.5-24.2% of persons obtaining care for DES) were more likely to have moderate to severe DES, and for this reason, they incurred higher direct and indirect costs.14
Medicare payment per procedure for punctal plug procedures declined from a peak in 2001. There are conceptual reasons to expect that a reduction in the fee may lead to either an increase or a decrease in utilization15. Prior empirical studies in other medical areas have demonstrated varied physician responses to Medicare fee reductions.16-21 The relationship between punctal plug use and Medicare payment for this procedure has not been evaluated. This study examines changes in punctal plug usage in a nationally representative longitudinal cohort selected from the Medicare population with DES diagnoses over the last decade to ascertain the relationship between DES diagnosis and punctal plug usage during the same time frame.
Methods
We used a 5% sample of Medicare beneficiaries’ Part B claims to identify beneficiaries with DES diagnoses and punctal plug insertion filed between 1991 and 2008. DES and punctal plug insertion codes were ascertained from International Classification of Diseases (ICD) and Current Procedural Terminology procedure codes (Table 1). To ensure that the DES diagnoses were incident cases, we employed a 3 year look-back period which necessitated all individuals be age 68+ and the first year of diagnosis be 1994+. For all subsequent years, we employed a similar look-back strategy. We excluded individuals who reported a plug procedure before first-time DES diagnosis in both DES and plug samples. We also excluded beneficiaries with stenosis of lacrimal punctum (ICD-9 CM 375.52) or stenosis of nasolacrimal duct (ICD-9 CM 375.56) from analysis. These diagnoses are functionally distinct and potentially incompatible with punctal plug insertion. Persons with these diagnoses represented 3.5% of beneficiaries in the sample with DES diagnoses. Sensitivity analysis performed on a sample of persons, which included beneficiaries with the codes from stenosis of lacrimal punctum and nasolacrimal duct, revealed similar results to those reported below.
Table 1.
Study diagnoses
| ICD-9 code | Description |
|---|---|
| 375.15 | Tear film insufficiency (Dry eye syndrome) |
| 370.20 | Superficial keratitis, unspecified |
| 370.21 | Punctate keratitis |
| 370.33 | Keratoconjunctivitis sicca |
| 370.34 | Exposure keratoconjunctivitis |
| 372.53 | Conjunctival xerosis |
| 710.2 | Sicca syndrome (Keratoconjunctivitis sicca, Sjogren’s syndrome) |
| 375.52a | Stenosis of lacrimal punctum |
| 375.56a | Stenosis of nasolacrimal duct |
Used in sensitivity analysis
We calculated annual incidence of DES diagnosis as a percentage of the Medicare 5% base population in a given year (“population-adjusted incidence”). We inflated payments and other reported costs by the Consumer Price Index (all items) to 2009 dollars (“real” dollars).
Results
Real Medicare payments for punctal plug insertion declined 55.1% from 2001 to 2008 (Table 2). The Medicare population-adjusted incidence of dry eye diagnosis increased over this time period by 23.3% (Figure 1). 91,131 total plugs were inserted in 45,582 Medicare beneficiaries from 1994 to 2008, with a mean of 2.0 plugs inserted per beneficiary undergoing plug treatment. Of all beneficiaries with dry eye diagnoses from 1994-2008, numbering 432,068 individuals, 9.2% underwent punctal plug placement from 1994-2008.
Table 2.
Dry eye diagnoses and punctal plug insertion by provider type (number of individuals)
|
Provider type performing plug insertion |
Provider type generating dry eye diagnosis (%)a | |||
| Ophthalmologist | Optometrist | Total | ||
| Ophthalmologist | 30,789 (69.06%) | 1,950 (4.37%) | 32,739 (73.44%) | |
| Optometrist | 1,910 (4.28%) | 9,933 (22.28%) | 11,843 (26.56%) | |
| Total | 32,699 (73.35%) | 11,883 (26.65%) | 44,582 (100.00%) | |
N= 44,582
Ophthalmology providers saw three-fold more patients than optometric providers with dry eye diagnoses. Ophthalmologists placed three-fold as many punctal plugs as optometrists. The majority of punctal plugs were placed by the diagnosing provider.
Figure 1. Incidence of DESa and Punctal Plug Insertion, Persons aged 68+.
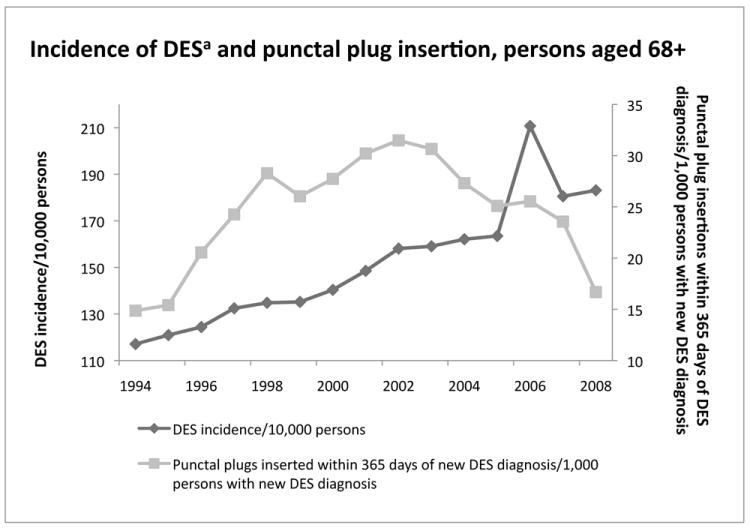
The population-adjusted incidence of DES diagnosis in the Medicare 5% Part-B has increased annually. However, the rate of first-time punctal plug insertion within 365 days of DES diagnosis reached a peak in 2002 and subsequently declined by 47.0% from 2002 to 2008.
aDry Eye Syndrome, bMultiple Ordinate Axes
Total punctal plug placement rates per beneficiary diagnosed with DES including repeat procedures increased annually until 2002 after which rates declined slightly (Figure 2). Specifically, use of this procedure increased 322% from 1994 to 2003, and subsequently declined by 7.7% from 2003-2008. First-time punctal plug insertion rates in individuals with DES diagnosis increased 203.7% from 1994 to a peak in 2003 and then declined by 15.3% (Figure 2). First-time punctal plug insertion rates within 365 days of first-time DES diagnosis as a proportion of individuals with DES diagnosed during that period increased 111.8% from 1994-2002 and then declined 47.0% from 2002 to 2008 (Figure 1).
Figure 2. Number of Punctal Plug Insertions by Year, Persons aged 68+.
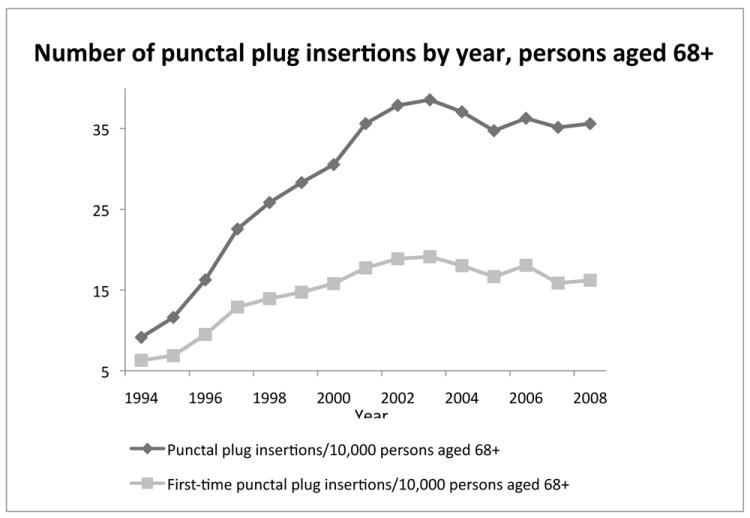
In Medicare 5% Part-B, total punctal plug placement including repeat procedures increased annually until 2002-2003, after which time rates remained relatively constant. First-time punctal plug insertion rates in individuals with dry eye syndrome diagnoses increased 203.7% from 1994 to a peak in 2003, then declined by 15.3% from 2003-2008.
In the population of Medicare beneficiaries diagnosed with DES that subsequently underwent first-time punctal plug insertion, ophthalmologists diagnosed and performed plug placement in 69%, while optometrists diagnosed and inserted in 23% of beneficiaries; 4% of individuals were diagnosed by optometrists with insertion performed by an ophthalmologist and conversely, 4% of beneficiaries received a diagnosis from a ophthalmologist with insertion by an optometrist (Table 3).
Table 3.
Annual Medicare payment for punctal plug insertion and Cyclosporine A (Restasis®, Allergan, Irvine, CA) sales
| Year | Medicare payment for CPT 68761a | Restasis® sales (106 dollars)a, 23 |
|---|---|---|
| 1994 | b | c |
| 1995 | b | c |
| 1996 | b | c |
| 1997 | b | c |
| 1998 | 112.36 | c |
| 1999 | 138.00 | c |
| 2000 | 219.68 | c |
| 2001 | 295.81 | c |
| 2002 | 194.28 | c |
| 2003 | 190.23 | 44.81 |
| 2004 | 206.44 | 113.77 |
| 2005 | 154.24 | 210.00 |
| 2006 | 141.89 | 286.41 |
| 2007 | 133.80 | 354.84 |
| 2008 | 132.92 | 440.00 |
| 2009 | 134.22 | 522.90 |
in 2009 real dollars
not available
Restasis® introduced April 2003
Coincident with the increase in diagnosis of DES, rates of punctal plug treatment for DES also increased to a peak in the early 2000s, which coincided with the highest Medicare payment levels for this procedure reached between 2000 and 2004. Payment per procedure was at least 30% higher than in other years, inflation-adjusted (Figure 2). Subsequent to 2004, overall rates of punctal plug treatment plateaued.
In April of 2003, Cyclosporine A (Cs A), a novel dry eye treatment, became commercially available.22 Distributed as Restasis® (0.05% cyclosporine ophthalmic emulsion [Allergan Inc., Irvine, CA]), Cs A is the first and only prescription topical eye drop with a Food and Drug Administration-approved indication for ocular inflammation associated with dry eye.11, 22, 23 Annual sales revenue of Restasis® increased 1067% from 2003 to 2009, reaching annual sales of 523 million 2009 real dollars in 2009 (Table 3).24
Discussion
DES occurs frequently, adversely affects vision-related quality of life, and has increased prevalence with age.1, 3-5 The rate of DES diagnosis increased over a recent 15-year period. Whether this increase demonstrates greater awareness of the condition by both providers and patients or growth in the underlying disease prevalence is unclear. Given the growth of marketing associated with the introduction of a prescription dry eye drug in 2003 and the likely greater market “savvy” by eye care providers regarding billable services during the 1990s, at least part of the increase is probably attributable to greater rates of diagnosis of previously uncoded or unrecognized DES. Additionally, as longevity of the Medicare population increases, DES rates may be expected to increase for this reason as well.
Between 2004 and 2008, the rate of plug use remained stable and the rate at which plugs were utilized for the first time decreased somewhat. The rise in payment for the punctal plug procedure was associated with a contemporaneous increase in the use of plugs, but subsequent reductions in Medicare payment since 2004 have not been associated with a change in punctal plug use. In contrast, reductions in Medicare fees for cataract procedures coincided with reduced numbers of cataract procedures in earlier studies.20, 21 Our analysis does not allow us to establish a causal relationship between changes in Medicare fees and punctual plug use.
Use of punctal plug within the first year of DES has changed. In particular, the proportion of first-time punctal plug insertion within a year of DES diagnosis as a proportion of individuals with DES diagnosed increased dramatically from 1994 to 2002, and then declined about half as much from 2002 to 2008. This finding suggests that the time interval between DES diagnosis and first-time punctal plug placement increased.
Given the stability in rates of overall use of punctal plugs in the Medicare population as measured by incidence of overall punctal plug insertions (Figure 1), it is likely that the delay in usage reflects another factor in the DES care environment. The 2003 introduction of CsA may well have contributed to the decline in the rate of first-time plug insertion within 365 days after DES diagnosis, since an additional therapeutic option was now available that did not require a procedure to be performed.
Choice of therapies for DES may have cost and care implications. Tear replacement by topical artificial tears and lubricants remains the most widely employed DES therapy, with estimated global sales of artificial tears exceeding 643 million real dollars in 2002.23 Cs A is also a topical therapy with a continuous monthly cost both to the patient and the insurers. By contrast, punctal plug insertion is theoretically a single treatment, with rates of punctal plug retention reported at 69.5% after one year,25 which may translate to cost savings for DES treatment. A recent study found similar increases in tear volume after six months of treatment with CsA or punctal plugs although variations in certain outcomes were observed.26
In a recent study of a large sample of commercial health plan enrollees, Fiscella et al. estimated the yearly health plan cost of topical Cs A at $376 per patient in 2009 dollars, and the yearly health plan cost of punctal plug occlusion to be $420 in 2009 dollars in the 365 day period following plug insertion with a mean of 2.85 punctal plug procedures per patient undergoing plug insertion within a 365 day period.27 In contrast, we found a mean of 2.0 punctal plug procedures per patient undergoing plug insertion over a 15 year period, which may indicate potential cost savings of punctal plug placement relative to chronic topical CsA therapy.
Fiscella et al. also reported a substantial number of patients received combination treatment with Cs A and punctal plugs, with 21.1% of punctal plug patients proceeding to Cs A use, and 11.4% of Cs A patients later undergoing punctal plug insertion.27 Initial studies suggest that a combination of punctal occlusion by plug with topical Cs A may have an additive effect in the treatment of DES,26 and providers are likely utilizing both therapies in practice. Combination therapies may obviate any cost savings from punctal plug insertion, particularly if future investigations confirm a greater crossover from punctal plug treatment to Cs A as compared to Cs A treatment progressing to punctal plug insertion. Dissemination of results of such studies may affect frequency of punctal plug insertion and Cs A prescription behavior in the future, as well as shape algorithms of treatment for optimal efficacy and cost-savings. In addition, while Fiscella et al. assumed a fixed price of Cs A and punctal plug insertion,27 future pricing changes including patent expiration for Cs A and continued fee reductions in punctal plug insertions would affect results of future analyses.
We found that most procedures were performed by the diagnosing provider. Since ophthalmologists cared for three times as many patients with DES diagnoses as optometrists, it is not surprising that they placed three-fold more punctal plugs than optometrists did. Comparing rates, however, does not allow us to risk-adjust for severity of disease in patients seen.
A strength of our study is the large national and longitudinal sample used in the analysis. Furthermore, the observational data allowed monitoring of trends as they applied in actual practice rather than in a controlled setting.
We acknowledge several study limitations. First, a deficiency of insurance claims is that data are collected for billing purposes and do not contain clinical findings other than those reflected in diagnosis codes. We examined only dry eye diagnoses, and not diagnoses also associated with dry eye symptoms, such as blepharitis. Also, the Medicare claims lacked information on prescription drug use such as of topical cyclosporine A, or over the counter treatments such as fish oil. We could not determine whether the observed decrease in first-time punctal plug insertion rates within the first year after DES diagnosis was accompanied by an increase in Cs A utilization. We also could not determine if repeat plug insertions were in the same or contralateral eye. Third, the Medicare sample was limited to persons aged 68+. Although DES is more common among elderly persons, our results do not necessarily generalize to the entire US population with DES.
In sum, although the frequency of DES diagnosis in the Medicare population has increased over time, first time punctal plug insertion rates, especially within the first year following DES diagnosis, have declined coincident with the increasing presence of a medical alternative and declining Medicare payment. The decline in punctal plug insertion coupled with an increase in utilization of potentially more costly alternative treatments could represent an increased burden to the health care system. Additional studies are needed to examine the comparative efficacy of punctal plug insertion and ocular anti-inflammatory therapy for the treatment of dry eye in order to fully describe DES treatments of optimal efficacy and cost savings.
Acknowledgments
Disclosure
Funding/Support: Partial support for this research came from the National Institute of Health grant RO1 AG-017473-09A2 and an Alcon Research Institute Award (PPL). The sponsors had no role in the design or conduct of this study.
References
- 1.Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136(2):318–26. doi: 10.1016/s0002-9394(03)00218-6. [DOI] [PubMed] [Google Scholar]
- 2.Opthalmology AAo. Dry Eye Syndrome - Preferred Practice Pattern. 2008 Sep; [Google Scholar]
- 3.Schaumberg DA, Dana R, Buring JE, Sullivan DA. Prevalence of dry eye disease among US men: estimates from the Physicians’ Health Studies. Arch Ophthalmol. 2009;127(6):763–8. doi: 10.1001/archophthalmol.2009.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schein OD, Munoz B, Tielsch JM, et al. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997;124(6):723–8. doi: 10.1016/s0002-9394(14)71688-5. [DOI] [PubMed] [Google Scholar]
- 5.Miljanovic B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143(3):409–15. doi: 10.1016/j.ajo.2006.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schiffman RM, Walt JG, Jacobsen G, et al. Utility assessment among patients with dry eye disease. Ophthalmology. 2003;110(7):1412–9. doi: 10.1016/S0161-6420(03)00462-7. [DOI] [PubMed] [Google Scholar]
- 7.Doughty MJ, Fonn D, Richter D, et al. A patient questionnaire approach to estimating the prevalence of dry eye symptoms in patients presenting to optometric practices across Canada. Optom Vis Sci. 1997;74(8):624–31. doi: 10.1097/00006324-199708000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Goto E, Yagi Y, Matsumoto Y, Tsubota K. Impaired functional visual acuity of dry eye patients. Am J Ophthalmol. 2002;133(2):181–6. doi: 10.1016/s0002-9394(01)01365-4. [DOI] [PubMed] [Google Scholar]
- 9.Liu Z, Pflugfelder SC. Corneal thickness is reduced in dry eye. Cornea. 1999;18(4):403–7. doi: 10.1097/00003226-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Rolando M, Iester M, Macri A, Calabria G. Low spatial-contrast sensitivity in dry eyes. Cornea. 1998;17(4):376–9. doi: 10.1097/00003226-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Calonge M. The treatment of dry eye. Surv Ophthalmol. 2001;45(Suppl 2):S227–39. doi: 10.1016/s0039-6257(00)00205-8. [DOI] [PubMed] [Google Scholar]
- 12.Pflugfelder SC, Solomon A, Stern ME. The diagnosis and management of dry eye: a twenty-five-year review. Cornea. 2000;19(5):644–9. doi: 10.1097/00003226-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Ervin AM, Wojciechowski R, Schein O. Punctal occlusion for dry eye syndrome. Cochrane Database Syst Rev. (9) doi: 10.1002/14651858.CD006775.pub2. CD006775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu J, Asche CV, Fairchild CJ. The Economic Burden of Dry Eye Disease in the United States: A Decision Tree Analysis. Cornea. doi: 10.1097/ICO.0b013e3181f7f363. [DOI] [PubMed] [Google Scholar]
- 15.McGuire TG, Pauly MV. Physician response to fee changes with multiple payers. J Health Econ. 1991;10(4):385–410. doi: 10.1016/0167-6296(91)90022-f. [DOI] [PubMed] [Google Scholar]
- 16.Chang SL, Liao JC, Shinghal R. Decreasing use of luteinizing hormone-releasing hormone agonists in the United States is Independent of Reimbursement Changes: A Medicare and Veterans Health Administration claims analysis. J Urol. 2009;182(1):255–60. doi: 10.1016/j.juro.2009.02.141. discussion 61. [DOI] [PubMed] [Google Scholar]
- 17.Gross CP, Andersen MS, Krumholz HM, et al. Relation between Medicare screening reimbursement and stage at diagnosis for older patients with colon cancer. JAMA. 2006;296(23):2815–22. doi: 10.1001/jama.296.23.2815. [DOI] [PubMed] [Google Scholar]
- 18.Jacobson M, O’Malley AJ, Earle CC, et al. Does reimbursement influence chemotherapy treatment for cancer patients? Health Aff (Millwood) 2006;25(2):437–43. doi: 10.1377/hlthaff.25.2.437. [DOI] [PubMed] [Google Scholar]
- 19.Lee AJ, Mitchell JB. Physician reaction to price changes: an episode-of-care analysis. Health Care Financ Rev. 1994;16(2):65–83. [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell JM, Hadley J, Gaskin DJ. Physicians’ responses to Medicare fee schedule reductions. Med Care. 2000;38(10):1029–39. doi: 10.1097/00005650-200010000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell JM, Hadley J, Gaskin DJ. Spillover effects of Medicare fee reductions: evidence from ophthalmology. Int J Health Care Finance Econ. 2002;2(3):171–88. doi: 10.1023/a:1020436509217. [DOI] [PubMed] [Google Scholar]
- 22.Donnenfeld E, Pflugfelder SC. Topical ophthalmic cyclosporine: pharmacology and clinical uses. Surv Ophthalmol. 2009;54(3):321–38. doi: 10.1016/j.survophthal.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Kymionis GD, Bouzoukis DI, Diakonis VF, Siganos C. Treatment of chronic dry eye: focus on cyclosporine. Clin Ophthalmol. 2008;2(4):829–36. doi: 10.2147/opth.s1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allergan. Earnings Release. 2003-2009 [Google Scholar]
- 25.Horwath-Winter J, Thaci A, Gruber A, Boldin I. Long-term retention rates and complications of silicone punctal plugs in dry eye. Am J Ophthalmol. 2007;144(3):441–4. doi: 10.1016/j.ajo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 26.Roberts CW, Carniglia PE, Brazzo BG. Comparison of topical cyclosporine, punctal occlusion, and a combination for the treatment of dry eye. Cornea. 2007;26(7):805–9. doi: 10.1097/ICO.0b013e318074e460. [DOI] [PubMed] [Google Scholar]
- 27.Fiscella RG, Lee JT, Walt JG, Killian TD. Utilization characteristics of topical cycolsporine and punctal plugs in a managed care database. Am J Manag Care. 2008;14(3 Suppl):S107–12. [PubMed] [Google Scholar]


