Abstract
Objective
To identify whether, by what means, and the extent to which historically, government health care expenditure growth in Europe has changed following economic crises.
Data Sources
Organization for Economic Cooperation and Development Health Data 2011.
Study Design
Cross-country fixed effects multiple regression analysis is used to determine whether statutory health care expenditure growth in the year after economic crises differs from that which would otherwise be predicted by general economic trends. Better understanding of the mechanisms involved is achieved by distinguishing between policy responses which lead to cost-shifting and all others.
Findings
In the year after an economic downturn, public health care expenditure grows more slowly than would have been expected given the longer term economic climate. Cost-shifting and other policy responses are both associated with these slowdowns. However, while changes in tax-derived expenditure are associated with both cost-shifting and other policy responses following a crisis, changes in expenditure derived from social insurance have been associated only with changes in cost-shifting.
Conclusions
Disproportionate cuts to the health sector, as well as reliance on cost-shifting to slow growth in health care expenditure, serve as a warning in terms of potentially negative effects on equity, efficiency, and quality of health services and, potentially, health outcomes following economic crises.
Keywords: Health economics, health care financing/insurance/premiums, comparative health systems/international health, health care organizations and systems
In the past 4 years, a number of European countries have experienced a sharp reduction in economic activity. This has had immediate implications for national finances as tax revenues, both direct and indirect, fall and some important categories of expenditure, such as unemployment benefits, rise, leading to growing deficits. However, do such changes have implications for expenditure on health care? Clearly, this depends on the political choices made in response to a crisis, but it is important that those choices are informed by what has happened previously in similar circumstances.
In all European countries governments play a substantial, if varying role in paying for health care, either by direct contributions from taxation or, in countries with social insurance, through their involvement in setting contributions as part of their macroeconomic policy, or in paying the contributions of those outside the labor force. However, predicting the consequences of an economic crisis for health expenditure is not straightforward. Some governments may elect to restrict growth in health care expenditure following economic crises, as is now happening in the United Kingdom (Appleby 2011), while others, especially those in receipt of external loans, may be required to cut it (Abel-Smith 1986). Yet others may increase expenditure, seeking to strengthen social safety nets in anticipation of the adverse health effects of unemployment (Stuckler et al. 2009). They may also see the health system as a counter-cyclical instrument to stimulate the economy. These possibilities can be summarized as three broad policy options: (1) to slow the rate of growth, or even cut health spending (2) to increase health spending above trend, or (3) to make no changes.
Should governments decide to slow the rate of growth in health care expenditure, there are several policy tools that they can use. Some policies do not seek to increase the burden of health care expenditure for patients, but rather slow aggregate growth by reducing the volume and/or quality of care through rationing, closing facilities, reducing staff numbers, or delaying capital investments. Governments may also slow growth more directly by reducing staff salaries or overheads. Other policies that can slow public expenditure growth include shifting costs to patients, either directly through user charges or indirectly through policies that encourage patients to seek care in the private sector. The assumption is that increases in out-of-pocket expenditure will slow public expenditure growth through two possible processes. First, increased household expenditure will substitute for lower public spending on health services, as public payers foot less of the bill. Second, the requirement to pay a higher share of publicly funded health care will reduce demand if patients are responsive to changes in prices, further reducing the amount spent by governments (Manning et al. 1987; Ellis and McGuire 1993). Likewise, inaction on the part of governments to reduce user charges to compensate for lower incomes at times of economic crisis may also lead to slower public expenditure growth through a similar mechanism, causing some patients to demand fewer services than previously. However, given that increased user charges are both inequitable and inefficient, policy makers could instead decide to increase the government's share of health expenditure and reduce out-of-pocket payments to preserve or increase financial protection for those affected by an economic downturn (Thomson, Foubister, and Mossialos 2010). Growth in health spending could also be maintained or increased by engaging in fiscal stimuli or by depleting savings.
In this study, we review the recent experiences of European countries. Using data from the Organisation for Economic Cooperation and Development's (OECD) National Health Accounts (NHA), we develop econometric models to estimate the association between economic crises and changes in growth in statutory health care expenditure (from taxes and social insurance schemes), and identify which types of policy tools are most strongly associated with these changes. As the OECD data are disaggregated into tax and social health insurance (SHI) derived expenditure, we also investigate changes in growth from each of these financing schemes. We do not attempt to categorize countries according to their health financing system, as most countries use a mix of tax and SHI financing.
Methods
Data
The OECD Health Data 2011 contains expenditure data for 24 European countries: Austria, Belgium, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Luxembourg, Netherlands, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, and United Kingdom. The sample includes data from 1960 to 2010, although not all countries report data in every year and only five countries have yet reported health expenditure data for 2010. As a result and as we are incorporating time lags for some explanatory variables, the sample used in our models is from 1972 to the latest available year in each country.
There is no universally agreed measure of an economic crisis and even the commonly used term “recession” is problematic (Suhrcke et al. 2011). The most widely used, and precise, definition, “a decline in the seasonally and calendar adjusted real gross domestic product (GDP) in at least two successive quarters,” is no more than a “rule of thumb” suggested in a 1974 newspaper article (Shiskin 1974). The broader definition, proposed by the National Bureau for Economic Research (NBER), is less precise, “a significant decline in [the] economic activity spread across the country, lasting more than a few months, normally visible in real GDP growth, real personal income, employment, industrial production, and wholesale-retail sales” (National Bureau of Economic Research Undated). However, many of these variables are not reported consistently over time or across countries or can be difficult to interpret. For example, historical unemployment data are subject to definitional problems and potential alternative measures, such as stock market valuations, have converged over the past four decades as global capital markets have become interdependent. As many of the variables required for our analyses are reported annually, we have adopted a pragmatic definition, consistent with that of the NBER, of a crisis existing in any year where real GDP contracted. This is more conservative than the commonly used two-quarter decline. However, it also reflects the reality of annual budget cycles in government spending.
Defining Dependent Variables
We develop econometric models to explain changes in growth for three different health expenditure data series:
total public expenditure,
tax-based public expenditure, and
SHI-based public expenditure.
The majority of health care in Europe is paid for by public sources that are either funded by taxes (e.g., directly via income and capital gains taxes or indirectly via consumption taxes, such as VAT), SHI contributions (e.g., premiums paid by employers and employees), or a mixture of the two (Thomson, Foubister, and Mossialos 2009). For example, the National Health Service of the United Kingdom is funded almost exclusively by taxes, whereas the statutory health insurance system in France is funded by employer and employee contributions, as well as some tax revenues. A limitation of the NHA data is that they classify all revenue channeled through social health insurance funds as social insurance contributions, even though they often include substantial amounts of tax-based allocations; for example, in France some of the funds spent by the SHI scheme are actually generated by taxes and transferred by the government to cover those who, for various reasons, do not pay contributions, but this tax revenue appears as social health insurance revenue in the NHA data (Chevreul et al. 2010).
Total public expenditure (series 1) is the aggregation of series 2 and 3, with our econometric models numbered correspondingly. Each of the dependent variables is expressed as nominal per capita expenditure in $US, adjusted for Purchasing Power Parity ($USPPP) for every country. We decided against using real per capita expenditure that are adjusted to remove the effects of inflation in the main analysis because of the uncertainty surrounding the quality and availability of health-specific price indexes that would otherwise be needed for this adjustment (Schreyögg et al. 2008; OECD 2010). However, we find that using inflation-adjusted expenditure data does not materially affect the analysis.
In our final model (Model 4), we attempt to explain year-to-year changes in:
4. public health care expenditure share of total government outlays.
To examine whether countries alter their rate of health expenditure growth in proportion to changes in other government expenditure following a crisis.
Defining Explanatory Variables
The models contain a combination of four different variables to explain changes in public expenditure growth rates or shares of government outlays. These four explanatory variables are:
3-year moving average of economic growth, lagged 1 year,
a logarithmic time trend,
a dummy variable in the year after an economic crisis, and
cost-shifting to households in the year after an economic crisis (i.e., the change in the out-of-pocket share of total health expenditure).
The first two variables are intended to produce simple, stable models of health expenditure growth, whereas the third and fourth variables are of primary concern for assessing the effects of economic crises.
Short-Run Average Economic Growth
Economic growth is a widely cited driver of growth in health care expenditure (Newhouse 1992; Barros 1998), although the association is inconsistent and subject to model specification (Parkin, McGuire, and Yule 1987). In our models, economic growth is estimated as the 3-year moving average of nominal per capita GDP growth in $USPPP, lagged 1 year. This smoothed measure of GDP growth is used instead of annual growth for a number of reasons, the primary reason being that we assume that governments will not substantially alter the rate of growth in health expenditure based on minor year-to-year fluctuations in the economy. Provided there are no major shocks they can use deficit spending to maintain annual income levels. The short-run economic growth term is lagged because spending is assumed to be largely unaffected by contemporaneous changes in the economy, as it takes time to implement health system reforms. Furthermore, by using a moving average we are able to isolate the effect of economic contractions on health spending using the economic crisis variables (i.e., explanatory variables three and four). As a robustness check, we find that using annual GDP growth produces similar results, although the goodness-of-fit in many of the models is slightly worse. The moving average of economic growth is presumed to capture the general economic trends that drive health expenditure growth, but will not reveal large fluctuations like economic crises, allowing differences in the rate of health expenditure growth due to an economic crisis to be detected separately from any statistical relationship between health spending and economic growth. The use of a moving average term is consistent with other studies that examine the relationship between public expenditure and economic growth (Devarajan, Swaroop, and Zou 1996; Centers for Medicare and Medicaid Services 2011). The 3-year period was selected after experimenting with various lag structures.
Logarithmic Time Trend
A time trend variable is included to compensate for any persistent upwards or downwards effect on expenditure growth which may be due to immeasurable or otherwise missing explanatory variables that exist across the entire sample. For example, if the coefficient on the trend variable was positive, it may imply that there is a missing variable driving health expenditure growth persistently upwards; this may be the case, for example, if price growth in the health sector has historically grown faster than GDP price growth (a potential scenario as both GDP and health expenditure are expressed nominally in the models). On the other hand, a negative coefficient implies a slowdown in growth over time, perhaps signaling an opportunity cost associated with continual high growth in health expenditure, recognizing that, ultimately, growth must slow to allow fiscal space for growth in expenditure on other government priorities. After experimenting with linear, quadratic, and logarithmic time trends, a logarithmic trend was selected for its goodness-of-fit and because constant upwards or downwards expenditure growth trends over long-time periods are not realistic. Excluding the logarithmic time trend from the models altogether does not have a significant effect on the magnitudes of the coefficients of interest, although it does reduce the goodness-of-fit (see Appendix).
Dummy Variable in the Year after an Economic Crisis
Because we define an economic crisis as any year where real per capita GDP growth is negative, we identify economic crises using a dummy variable where a crisis year is set equal to 1 and all other years are equal to 0. This dummy variable, lagged by 1 year, is used in the models to determine whether health expenditure growth in the year after an economic crisis is different from that which would otherwise be predicted by each model. Therefore, if statistically significant in the models, it implies that some sort of mechanism exists in our sample that consistently alters the expected rate of expenditure growth in the year after a crisis. If the coefficient on this variable is negative, it means that in the year following a crisis this mechanism exerts downwards pressure on expenditure growth (and vice versa). We make no attempt to distinguish economic crises based on their length or severity.
Cost-Shifting to Households in the Year after an Economic Crisis
Although health care in Europe is largely funded by public sources, in many countries patients pay some portion of health care costs out-of-pocket. Public payers may alter the public/household mix of health expenditure following economic crises. They could (1) do this explicitly by altering user charges, they may (2) introduce other policies that indirectly change the household share of health expenditure, or they may (3) “do nothing,” which may also indirectly change the household share of health expenditure. Using the data available, it is not possible to assess with certainty whether governments have instituted or altered cost-sharing arrangements. However, we attempt to estimate whether and to what degree changes in out-of-pocket expenditure are associated with a change in growth of public health care expenditure in the year after an economic crisis. Therefore, we estimate cost-shifting policy responses as changes in the out-of-pocket share of total health expenditure in the year following an economic crisis, which are thus distinguishable from other methods to control health budgets. Although it is possible to measure whether changes in expenditure growth are associated with an alteration in the public/household mix of health expenditure, it is not possible to attribute causality.
Model Specifications
We construct three models in three stages to estimate statistical relationships between the aforementioned explanatory variables and changes in health expenditure, and a fourth model in two stages to explain changes in the health expenditure share of government outlays. Models 1, 2, and 3 are estimated generalized least-squares (EGLS) fixed effects models using cross-section weights on the countries, whereas Model 4 uses fixed effects panel least-squares method with no cross-section weights. Cross-section weights are used in Models 1, 2, and 3 to address potential heteroscedasticity. The nature of the fixed effects model accounts for some differences between countries by estimating country-specific constant rates of growth which enables us to use the same model specification for countries with vastly different health systems. However, we make no additional attempts to account for any country-specific structural changes to health financing systems or otherwise (such as health sector reforms) across time. All variables that are referred to as growth rates are expressed in the models as log-differenced expenditure levels; variables that are referred to as changes in shares are calculated as year-to-year differences in levels.
The three-stage process for estimating Model 1 serves as the basis for Models 2 and 3, where hi,t represents per capita health expenditure for country i in year t, c is a constant, GDPi,t−1 is per capita GDP lagged 1 year, trend is the time trend, xt−1 is the lagged economic crisis dummy variable, st is the out-of-pocket share of total health expenditure, μi is the country-specific fixed effect, and εi,t is the error term:
Model 1 Stage 1 equation:
Model 1 Stage 2 equation:
Model 1 Stage 3 equation:
The first stage of Model 1 regresses total public health care expenditure growth on a constant term, 3-year moving average economic growth, and the logged time trend, to demonstrate a stable, statistical relationship absent an economic crisis. In stage 2, the lagged crisis dummy variable is added to the model to determine whether there is a statistically significant difference in the model predicted rate of growth in the year after an economic crisis. Including both the 3-year moving average of economic growth and the lagged crisis dummy variable does not present a collinearity issue because although the variables are conceptually related, they are not highly correlated (r = −0.2005).1 The third stage adds the cost-shifting variable to estimate whether changes in the household burden of health expenditure are associated with changes in total public health care expenditure growth.
When the cost-shifting and economic crisis dummy variables are both used in stage 3, the interpretation of the dummy variable changes. In this case, if both variables are statistically significant, the coefficient on the cost-shifting variable will estimate the change in total public expenditure growth that is associated with a change in the out-of-pocket share; the dummy variable will capture any remaining slowdown in health spending growth in the year after a crisis. Therefore, in stage 3 the dummy variable is assumed to capture any efforts to control health budgets that do not lead to changes in the out-of-pocket share of total health expenditures. These will include policy actions on the part of the payer or supplier of health care that do not directly necessitate behavioral responses by patients (e.g., changes in salaries, delaying investment, etc.), as they do not result in a change in the household portion of health care expenditure.
To test whether the Model 1 specifications are consistent for both types of statutory financing sources, Models 2 and 3 employ the identical three-stage process with the dependent variables in these models being tax-based expenditure growth and SHI expenditure growth, respectively.
Finally, to test whether economic crises are associated with changes in the overall public health care expenditure share of government budgets, we construct Model 4 in two stages, where gi,t is the public health care expenditure share of total government outlays for country i in year t, c is a constant, trend is the time trend, germ92 is a dummy variable for Germany in 1992, xt-1 is the lagged economic crisis dummy variable, μi is the country-specific fixed effect, and εi,t is the error term:
Model 4 Stage 1 equation:
Model 4 Stage 2 equation:
The first stage regresses changes in public health expenditure as a share of total government outlays on a constant term, a logged trend, and a dummy variable for Germany in 1992; the second stage introduces the lagged economic crisis dummy variable. The change in health expenditure as a share of government outlays for Germany in 1992 is an extreme outlier; controlling for this single observation drastically improves the model goodness-of-fit. The funder played no role in the analysis, interpretation, or presentation of the findings.
Results
Using the OECD data, we identify 139 economic crisis years across all countries of 816 available observations, although corresponding data on health expenditure are not available for all of those observations. In the year after an economic crisis, public health care expenditure growth has slowed 62 times (65 percent of available observations); in 14 of those years health expenditure growth contracted (Table 1).
Table 1.
Summary Statistics, 1972–2010
| Number of economic crises | 139 |
| Number of real per capita GDP growth rates | 816 |
| Percentage of years with a crisis | 17.0% |
| Number of years where public health expenditure per capita growth has slowed in the year after a crisis | 62 |
| Number of years where public health expenditure per capita growth has increased in the year after a crisis | 33 |
| Number of years where public health expenditure per capita growth has contracted (negative) in the year after a crisis | 14 |
| Number of years where public health expenditure per capita growth has been positive in the year after a crisis | 81 |
| Number of years where the out-of-pocket share of total health expenditures has increased in the year after a crisis | 38 |
| Number of years where the out-of-pocket share of total health expenditures has decreased in the year after a crisis | 19 |
Note. The share of economic crises that resulted in altered health expenditure growth cannot be directly calculated because some countries have GDP data available but not health expenditure data for all years.
For example, between 1995 and 2010 Italy and Switzerland each experienced four economic crises, more than any other country that also has corresponding expenditure data for all years (Figure 1). Italy has predominantly tax-based funding, whereas Switzerland has predominantly a mix of statutory mandated health insurance (classified as SHI in the NHA data) and tax-based funding (Leu et al. 2009). Slowdowns in expenditure growth are directly observable in the year following four of the eight economic crisis years.
Figure 1.
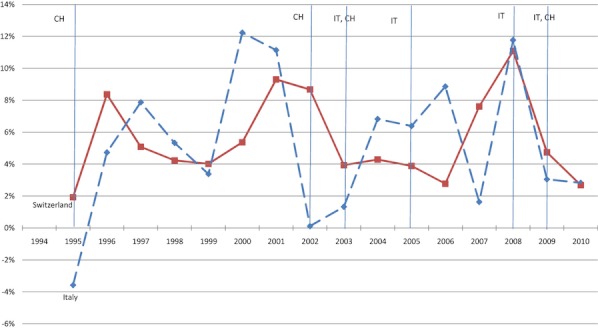
Italy (IT) and Switzerland (CH) Health Expenditure Growth and Economic Downturns, 1995–2010
Note. Vertical lines represent economic crisis years; the countries that experienced the downturn are listed accordingly to the left of the line.
Our econometric models enable us to assess whether expenditure growth differs from that which would have otherwise been expected absent an economic crisis. Model 1, Stage 1 suggests that growth in statutory health care expenditure is positively driven by economic growth (0.78 percent acceleration in health expenditure growth for every 1 percent increase in average economic growth) which is within the likely range of income elasticity of demand for health care found in other studies (Table 2) (Costa-i-Font, Marin, and Rubert 2011). The logged trend coefficient is negative, indicating an overall slowdown in expenditure growth over time across the sample. In Model 1, Stage 2, the economic crisis dummy variable is negative (−2.2 percent), revealing that on average, statutory health care expenditure growth in European countries is slower than that which would otherwise be predicted by general economic trends in the year following an economic crisis. This slowdown is estimated at 95% confidence between −1.3 and −3.2 percent across countries (Figure 2). Likewise, in Model 1, Stage 3, both the economic crisis dummy variable and the cost-shifting variable are negative (−1.9 percent and −2.4 percent slowdown in expenditure growth for every 1 percentage point increase in the out-of-pocket share of total expenditure, respectively). Again, cost-shifting in the year after an economic crisis is associated with −1.5 to −3.4 percentage points slowdown in public expenditure growth for every 1 percentage point increase in the out-of-pocket share of total expenditure, and all other policy tools are on average associated with −0.9 to −2.9 percentage point slowdowns in public expenditure growth (Figure 2).
Table 2.
Coefficients from Fixed Effects Regression Analysis for Models 1, 2, and 3
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Public Health Care Expenditure Per Capita ($US PPP) Growth | Tax-Based Public Health Care Expenditure Per Capita ($US PPP) Growth | SHI-based Public Health Care Expenditure Per Capita ($US PPP) Growth | |||||||
| Stage 1 | Stage 2 | Stage 3 | Stage 1 | Stage 2 | Stage 3 | Stage 1 | Stage 2 | Stage 3 | |
| 3-Year moving average of nominal economic growth lagged 1 year | 0.782*** | 0.726*** | 0.725*** | 0.816*** | 0.765*** | 0.807*** | 0.404*** | 0.373*** | 0.308*** |
| Logged time trend | −0.035*** | −0.038*** | −0.029*** | −0.030*** | −0.031*** | −0.030*** | −0.051*** | −0.052*** | −0.046*** |
| crisis dummy variable lagged 1 year | −0.022*** | −0.019*** | −0.024*** | −0.021*** | −0.001 | −0.001 | |||
| Cost-shifting in the year after a crisis | −0.024*** | −0.024*** | −0.020*** | ||||||
| n | 643 | 643 | 397 | 520 | 520 | 391 | 358 | 358 | 324 |
| R-squared | 0.337 | 0.363 | 0.382 | 0.293 | 0.313 | 0.351 | 0.244 | 0.246 | 0.242 |
| DW statistic | 1.622 | 1.662 | 1.742 | 1.646 | 1.673 | 1.842 | 1.908 | 1.911 | 1.986 |
Source. Authors' calculations.
Statistical significance at 99%.
**Statistical significance at 95%.
*Statistical significance at 90%.
Figure 2.
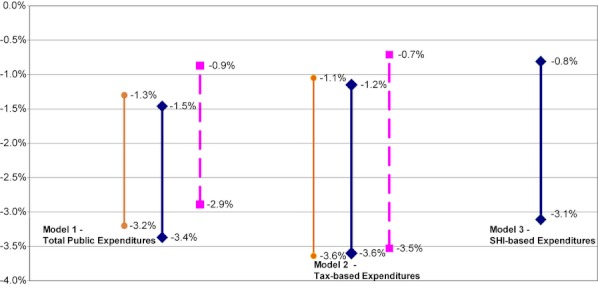
95% Confidence Intervals of Explanatory Variable Associations with Changes in Health Expenditure Growth in the Year after a Crisis (in %)
Notes. The line ending in circles is the overall association between the lagged economic crisis dummy variable and health expenditure growth in Stage 2 of each model. The line ending in diamonds is the relationship between a 1 percent increase in the out-of-pocket share of total health expenditures in the year after a crisis and health expenditure growth in Stage 3 of each model. The dotted line is the relationship between the lagged economic crisis dummy variable and health expenditure growth in Stage 3 of each model. The economic crisis dummy variable in Model 3 lacked statistical significance in Stages 2 and 3.
The results are similar in terms of magnitude, direction, and statistical significance in Model 2 for all variables, implying that for tax-based health expenditure, growth has slowed in the year after an economic crisis and that both cost-shifting and other policy tools are associated with these slowdowns (Figure 2 and Table 2). However, for Model 3, Stage 2 the economic crisis dummy variable, while still negative, was no longer statistically significant. This implies that although economic crises may be associated with slowdowns in SHI expenditure, any association is not strong.
Despite the lack of statistical significance for the dummy variable in Stage 2, Model 3 Stage 3 includes both the economic crisis dummy variable and the cost-shifting variable. Although the economic crisis variable is negative, it is still not statistically significant. The cost-shifting variable, however, is both negative and statistically significant. This indicates that although we cannot say with certainty that SHI expenditure growth is consistently altered in the year after an economic crisis, increases in the out-of-pocket share of total health expenditure following economic crises are associated with slowdowns in SHI expenditure growth (and vice versa); historically, European countries do not seem to have slowed growth in SHI expenditure after economic crises using other non-cost-shifting policy tools.
Figure 3 compares the actual and predicted 2010 health expenditure growth rates for the current economic crisis in Italy and Switzerland as well as 2009 real GDP growth. Tax-based expenditure in Italy (which comprises nearly all of Italian public health care spending) is correctly predicted to slow by the model, although in actuality growth only slowed from 2.9 to 2.8 percent. Likewise, SHI-based expenditure in Switzerland (which comprises around two-thirds of public health care spending) was predicted to increase from 3.3 to 3.5 percent growth in 2010; 2010 SHI spending actually grew by a slightly higher 3.7 percent.
Figure 3.
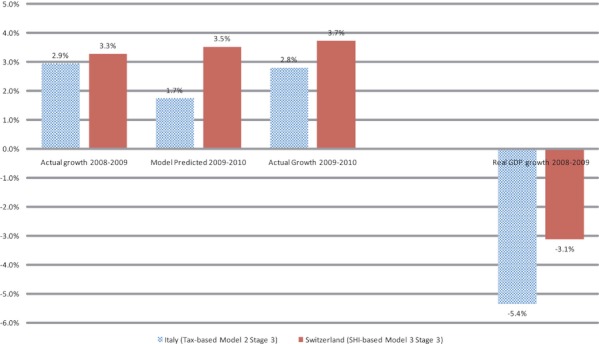
Actual versus Model Predicted Expenditure Growth in Italy and Switzerland, 2009–2010
Model 4 is intended to determine whether governments reduce the size of their health budgets relative to total government outlays in the context of crises. In Model 4, Stage 1 we found the coefficient on the logarithmic time trend to be slightly positive and statistically significant, indicating that statutory health care expenditure consumes a growing share of government resources over time. The coefficient on the economic crisis dummy variable in Model 4, Stage 2 is, however, found to be statistically significant and negative (−0.2 percent) which indicates that in the year after an economic crisis, on average, health expenditure comprises a smaller percentage of total government outlays than would otherwise be expected (Appendix S1). At 95 percent confidence, in the year after an economic crisis, the health expenditure share of government outlays is found to decrease by −0.1 to −0.4 percentage points.
Discussion
These analyses are subject to a number of limitations. First, there are missing observations in the data series, particularly in earlier years. To verify that missing data do not materially affect comparison between the models, we reran all models using a restricted dataset that only includes observations if they are available for all dependent variables and found no marked differences in the results. Also, as mentioned, we reran all of the models without the logarithmic time trend and found that the time trend did not noticeably alter the observed effect of economic crises (Appendix S2). Second, as mentioned, the data on source of spending reflect national organizational structures but do not necessarily capture the complexity of the original sources of funds (Kutzin 2001). It is very likely, for example, that some funds that appear to be from social insurance funds may ultimately be derived from budget transfers that originated as tax revenue. Thirdly, these models can only imply correlation but not causality. We were unable to identify any method that would enable us to state definitively that changes in health expenditure have occurred explicitly as a result of policy changes in response to economic crisis, although factors such as the strength, timing, and coherence of the relationships increase the likelihood that the associations are causal and that some sort of process has consistently slowed health expenditure growth in the year after a crisis across countries (Hill 1965).
We also experimented with a simpler model specification that separately includes lagged real GDP growth rates when they are positive and when they are negative to allow asymmetry in the effects. Although the explanatory power of the model is weaker (R2 = 0.18), the expectation that public health expenditure would grow more slowly in the year after an economic crisis persisted. Likewise, the findings for SHI and tax-based spending remain consistent (Appendix S3).
The observed associations between economic crises and growth in health care expenditure indicate that, in the past, growth in public health care expenditure has slowed in the year following a crisis from that which would otherwise be predicted in European countries given general economic conditions. The models reveal that alteration in growth and the types of policy responses that may have been used differ depending on whether expenditure is derived from tax or SHI. Whereas growth in tax-derived health expenditure is shown to vary after economic crises in conjunction with cost-shifting and other policy responses, SHI expenditure growth is found to be altered only in conjunction with policy responses that shift costs and may be less likely to slow following an economic crisis. The coefficients on the short-run average economic growth term are markedly lower in magnitude for all three stages of Model 3 than for the other models, indicating that the rate of SHI expenditure growth may simply be less closely correlated with macroeconomic growth in general, although this should be explored further.
As mentioned, it is not possible, using OECD data, to ascertain whether countries are actually instituting new cost-sharing arrangements in response to crises, although we are currently examining this for the current crisis by means of a survey of key informants in countries. However, we find that the out-of-pocket share of total health expenditure is in fact increasing in 38 post-crisis observations (67 percent) (Table 1). The mean difference in the out-of-pocket share of total health expenditure in the year after a crisis is also positive (0.17 percent). This indicates that in the majority of instances patients have paid a greater portion of their health expenditure at the point of service in the year following economic crises than they did in the previous year, an occurrence which is found to be associated with slower public expenditure growth, regardless of whether that shift is the explicit result of changes to health policy.
The reasons why different policy tools may have been used to alter expenditure growth by those with control over different financing institutions are necessarily speculative. Most likely, countries that take steps to affect health expenditure growth rates after a crisis do so using a mix of policy tools. However, intuitively, tax-based financing may have been more susceptible to government decisions to reduce health budgets through, for example, reductions in health worker salaries or across-the-board budget cuts. This may have been particularly the case in systems with a high degree of integration of purchasing and provision of health services. On the other hand, it may be more difficult for governments and insurance funds to reduce SHI expenditure through these sorts of interventions due to the need for agreement among multiple stakeholders, including government, employers, and trade unions, and health service providers themselves, which can be expected to slow decision making.
In addition, governments may have had to step in and subsidize SHI to substitute for declines in SHI contributions due to reduced wages and/or increased unemployment, emphasizing the role of governments as insurers of last resort. This would not be reflected in the data, as we are not able to identify the original source of SHI funds; however, it may be a reason that despite the likelihood of lower SHI contributions, expenditure growth appears less likely to slow.
These data reveal changes in the out-of-pocket share of total spending and the association with total public expenditure growth, but they cannot definitively conclude that user charges are increasing in response to economic crises in an effort to slow aggregate expenditure growth. Nevertheless, the possibility of increased user charges raises concerns for the equity and efficiency of the health financing system as, unless they are carefully designed, increased user charges may reduce the utilization of necessary care and disproportionately affect access to health services by poorer population groups (Thomson, Foubister, and Mossialos 2010). The results of Model 4 tentatively suggest that after a crisis the percentage of government expenditure spent on health is likely to decline relative to what it would otherwise have been, regardless of whether total government outlays are increasing or decreasing. This appears to demonstrate that health care expenditure has not historically been protected, but rather, that countries may have used economic crises as an opportunity to reduce or slow growth in the health share of their government budgets.
Conclusion
The finding that countries may alter health care spending growth after economic crises is not necessarily surprising. However, this study reveals that the types of policies associated with these changes in health expenditure vary according to the financing institutions involved. Although changes in tax-derived expenditure are associated with cost-shifting and other policy responses following a crisis, such changes in expenditure derived from social insurance have historically been associated only with shifts in the out-of-pocket share. Although health expenditure data related to the current global crisis are not yet available in many countries, preliminary indications are that countries have taken concrete steps to alter their rates of expenditure growth (Mladovsky et al. 2012). Whether countries have sought to slow or increase health expenditure growth remains to be seen. Going by the historical trends presented in this study, it is likely to be the former.
This study serves as a stark reminder that growth in health care expenditure is susceptible to political decisions after economic crises. The use of cost-shifting toward households to slow growth in public expenditure raises concerns for efficiency and equity, which is especially important in the present crisis, which has been characterized by historically large amounts of household debt. Other types of policies that aim to improve efficiency while maintaining equity and quality are preferable. If the interpretation of Model 4 is accurate, governments may slow growth in health care expenditure after economic crises more than they slow non–health care spending. This is likely to have significant consequences for financial protection, and possibly for health and ultimately for economic growth (Suhrcke et al. 2006). Consequently, it is imperative that countries avoid the temptation to disinvest in health, and thus the productivity of their population, even during economic crises. Future studies should address the magnitude of the consequences for health and future economic performance from slowing expenditure growth after a crisis.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The European Observatory on Health Systems and Policies provided support for the project. We would like to acknowledge Sarah Thomson, Joan Costa-i-Font, Marina Karanikolos, Divya Srivastava, Sotiris Vandoros, David Stuckler, and Pedro Pita Barros for their helpful feedback on previous drafts of this study.
Disclosures: We declare that we have no conflicts of interest.
Note
Calculating a standard Pearson correlation coefficient is appropriate in this context because the Pearson correlation coefficient is for linear covariation and we are using a linear model.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix S1: Model 4 Results.
Appendix S2: Excluding Logarithmic Trend from Models 1, 2, and 3.
Appendix S3: Alternative Model Specification to Investigate Asymmetry in the Effects.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Abel-Smith B. “The World Economic Crisis. Part 1: Repercussions on Health”. Health Policy and Planning. 1986;1(3):202–13. doi: 10.1093/heapol/1.3.202. [DOI] [PubMed] [Google Scholar]
- Appleby J. “What's Happening to NHS Spending across the UK?”. British Medical Journal. 2011;342:d2982. doi: 10.1136/bmj.d2982. [DOI] [PubMed] [Google Scholar]
- Barros PP. “The Black Box of Health Care Expenditure Growth Determinants”. Health Economics. 1998;7(6):533–44. doi: 10.1002/(sici)1099-1050(199809)7:6<533::aid-hec374>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. 2011. “Projections of National Health Expenditures: Methodology and Model Specification” [accessed on June 6, 2011]. Available at http://www.cms.hhs.gov/NationalHealthExpendData/downloads/projections-methodology.pdf.
- Chevreul K, Durand-Zaleski I, Bahrami SB, Hernandez-Quevedo C, Mladovsky P. “France: Health System Review”. Health Systems in Transition. 2010;12(6):1–291. [PubMed] [Google Scholar]
- Costa-i-Font J, Marin G, Rubert G. “Biases in the Healthcare Luxury Good Hypothesis? A Meta-Regression Analysis”. Journal of the Royal Statistical Society, series A. 2011;174(1):95–107. ISSN 0964-1998. [Google Scholar]
- Devarajan S, Swaroop V, Zou H. “The Composition of Public Expenditure and Economic Growth”. Journal of Monetary Economics. 1996;37(2):313–44. [Google Scholar]
- Ellis RP, McGuire TG. “Supply-Side and Demand-Side Cost Sharing in Health Care”. The Journal of Economic Perspectives. 1993;7(4):135–51. doi: 10.1257/jep.7.4.135. [DOI] [PubMed] [Google Scholar]
- Hill AB. “The Environment and Disease: Association or Causation?”. Journal of the Royal Society of Medicine. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- Kutzin J. “A Descriptive Framework for Country-Level Analysis of Health Care Financing Arrangements”. Health Policy. 2001;56(3):171–204. doi: 10.1016/s0168-8510(00)00149-4. [DOI] [PubMed] [Google Scholar]
- Leu R, Rutten F, Brouwer W, Matter P, Rütschi C. “The Swiss and Dutch Health Insurance Systems: Universal Coverage and Regulated Competitive Insurance Markets.” (The Commonwealth Fund) New York: The Commonwealth Fund; 2009. [Google Scholar]
- Manning WG, Newhouse JP, Duan N, Keeler EB, Leibowitz A. “Health Insurance and the Demand for Medical Care: Evidence from a Randomized Experiment”. The American Economic Review. 1987;77(3):251–77. [PubMed] [Google Scholar]
- Mladovsky P, Srivastava D, Cylus J, Karanikolos M, Thomson S, McKee M. Health Policy Responses to the Financial Crisis and Other Health System Shocks in Europe. Copenhagen: Health Evidence Network, World Health Organization; 2012. [Google Scholar]
- National Bureau of Economic Research. “Business Cycle Expansions and Contractions” [accessed on June 6, 2011]. Available at http://web.archive.org/web/20071012231548/http:/www.nber.org/cycles.html.
- Newhouse JP. “Medical Care Costs: How Much Welfare Loss?”. The Journal of Economic Perspectives. 1992;6(3):3–21. doi: 10.1257/jep.6.3.3. [DOI] [PubMed] [Google Scholar]
- OECD. 2010. “Note on General Comparability of Health Expenditure and Finance Data in OECD Health Data 2010.” [accessed on June 6, 2011]. Available at http://www.ecosante.org/OCDEENG/411.html.
- Parkin D, McGuire A, Yule B. “Aggregate Health Care Expenditures and National Income. Is Health Care a Luxury Good?”. Journal of Health Economics. 1987;6(2):109–27. doi: 10.1016/0167-6296(87)90002-6. [DOI] [PubMed] [Google Scholar]
- Schreyögg J, Tiemann O, Stargardt T, Busse R. “Cross-Country Comparisons of Costs: The Use of Episode-Specific Transitive Purchasing Power Parities with Standardised Cost Categories”. Health Economics. 2008;17:S95–103. doi: 10.1002/hec.1327. [DOI] [PubMed] [Google Scholar]
- Shiskin J. “The Changing Business Cycle”. New York Times. 1 December 1974, Sec. 3, p. 12. [Google Scholar]
- Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. “The Public Health Effect of Economic Crises and Alternative Policy Responses in Europe: An Empirical Analysis”. Lancet. 2009;374(9686):315–23. doi: 10.1016/S0140-6736(09)61124-7. [DOI] [PubMed] [Google Scholar]
- Suhrcke M, McKee M, Stuckler D, Sauto Arce R, Tsolova S, Mortensen J. “The Contribution of Health to the Economy in the European Union”. Public Health. 2006;120(11):994–1001. doi: 10.1016/j.puhe.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Suhrcke M, et al. “The Impact of Economic Crises on Communicable Disease Transmission and Control: A Systematic Review of the Evidence”. PLoS ONE. 2011;6(6):e20724. doi: 10.1371/journal.pone.0020724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson S, Foubister T, Mossialos E. Financing Health Care in the European Union. Challenges and Policy Responses. Copenhagen: World Health Organization; 2009. [Google Scholar]
- Thomson S, Foubister T, Mossialos E. “Can User Charges Make Health Care More Efficient?”. British Medical Journal. 2010;341:487–9. doi: 10.1136/bmj.c3759. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


