Abstract
Objective
To analyze the effect of market-level changes in assisted living supply on nursing home utilization and resident acuity.
Data Sources
Primary data on the supply of assisted living over time were collected from 13 states from 1993 through 2007 and merged with nursing home-level data from the Online Survey Certification and Reporting System and market-level information from the Area Resource File.
Study Design
Least squares regression specification incorporating market and time-fixed effects.
Principal Findings
A 10 percent increase in assisted living capacity led to a 1.4 percent decline in private-pay nursing home occupancy and a 0.2–0.6 percent increase in patient acuity.
Conclusions
Assisted living serves as a potential substitute for nursing home care for some healthier individuals with greater financial resources, suggesting implications for policy makers, providers, and consumers.
Keywords: Assisted living, nursing homes, utilization, acuity
Over the last two decades, assisted living has rapidly emerged as a housing and long-term care option for older Americans (Hawes, Rose, and Phillips 1999).1 Despite general agreement about the broader goals of assisted living—round-the-clock service; aging-in-place; consumer independence, dignity, autonomy, and choice; and a homelike environment—heterogeneity exists in the range of services offered and the populations served across facilities and markets (Hawes et al. 2003). Assisted living has also evolved over time, as facilities provide a more disabled resident population with an increasingly complex array of services (Morgan, Gruber-Baldini, and Magaziner 2001; Spillman, Liu, and McGillard 2002).
The growth in assisted living has coincided with dramatic changes in the market for nursing home care (Bishop 1999). The national mean occupancy rate for nursing homes declined from 93 percent in 1977 to 87 percent by 1995 (Strahan 1997), and further down to 83 percent by 2003 (Gibson et al. 2004). At the same time, resident acuity and the share of long-stay residents who rely on Medicaid have increased. Previous work has attributed declining nursing home utilization to changing demographics among the elderly (Lakdawalla and Philipson 2002) and to the growth of home and community-based care (Bishop 1999). Research generally has not attempted to link the growth in assisted living to changes in the nursing home sector, in part because data to track assisted living growth across markets has not been available to researchers. In this study, we use novel data on assisted living supply in 13 states over the period 1993–2007 to analyze trends in the assisted living and nursing home sectors.
Background
The growth of the assisted living industry has occurred largely in the absence of government financing or regulation. As such, no single regulatory or licensure category exists for assisted living facilities, and the industry's size is hard to determine with precision. With this caveat, one recent study estimated that there were approximately 11,276 assisted living facilities with 839,746 units nationwide in 2007 (Stevenson and Grabowski 2010). By comparison, the nursing home industry had approximately 16,100 facilities and 1.7 million beds nationwide in 2004 (Jones et al. 2009).
Advocates have cited both moral and economic reasons in favor of expanding access to publicly financed care in assisted living facilities and other nursing home alternatives. Since the 1970s, the disability rights movement has challenged the institutional bias of public long-term care services, positing that it limits personal autonomy, reinforces segregation from the community, and perpetuates standardized services that fail to account for individual needs. Consistent with this view, the Supreme Court's Olmstead ruling found in 1999 that states have an obligation to administer services in the most integrated setting appropriate to individuals' needs. In part, this ruling obligated states to further develop and finance nursing home alternatives such as assisted living. In economic terms, simple consumer preference can be used to justify the expansion of assisted living, given that individuals prefer to receive care in the least institutional—and most homelike—setting possible (Brodie and Blendon 2001). Some individuals who have less intensive care needs may also be able to purchase assisted living care at lower prices relative to nursing home care. Although the cost of assisted living can vary considerably depending on the locality and by the amenities and services provided, industry surveys estimated the average annual cost of assisted living care at $37,572 in 2010, compared to $79,935 per year for a private room in a nursing home (MetLife Mature Market Institute 2010).
The above rationales appeal to state Medicaid programs, but they are accompanied by important caveats. Policy makers are concerned that offering a broad array of publicly financed long-term care options might lead to increased overall consumption of services (known as moral hazard or the woodwork effect), especially given the difficulty of targeting home- and community-based services only to individuals who would otherwise enter a nursing home (Grabowski 2006). In part for this reason, state Medicaid programs have been slow to offer comprehensive coverage for assisted living care. Many states have small, experimental programs under which Medicaid pays the personal care and medical services portion of the monthly assisted living charge, but not for room and board. These expenses—which Medicaid reimburses in hospitals and nursing homes—typically are financed from a resident's income, including Social Security, Supplemental Security Income (SSI) and state supplements, private pensions, and, in some states, family contributions (Stevenson et al. 2000).
Two recent studies help illuminate these issues to a degree. One empirical study used the Medicare Current Beneficiary Survey to estimate hazard models of the transition from the community to either a nursing home or an assisted living facility, finding that individuals who transitioned to nursing homes had lower incomes, were older, and were more disabled than individuals who transitioned to assisted living facilities. The study also identified considerable overlap in the determinants of both transitions, especially on functional health measures, suggesting the possibility of some substitution between settings (Waidmann and Thomas 2003). In a similarly focused, qualitative study, families and residents of assisted living facilities and nursing homes in Oregon were interviewed about individual circumstances prior to the transition and factors that were important in choice of setting (Reinardy and Kane 2003). The study likewise found many similarities across settings, although also identifying some key differences. Nursing home residents were considerably more disabled, were more likely to come from the hospital with a physician serving a prominent role in the placement, were less likely to consider paid care in the home as an alternative, and placed less emphasis on private space and more on rehabilitation in their choice process.
These earlier studies highlight the potential substitution of assisted living for nursing home care but do not quantify it directly. With the exception of one previous study finding that the growth in adult foster care services in Oregon was related to a reduction in the number of nursing home residents (Nyman et al. 1997), we are not aware of any studies addressing this important policy issue. To address this gap in the literature, we examine this issue using data from 13 states, accounting for nearly 20 percent of the elderly (85+) U.S. population.
Conceptual Model
In a standard economic model of long-term care decision making (Pezzin, Kemper, and Reschovsky 1996), utility is a function of private goods, leisure, the elderly person's functioning, and the household's preferences (e.g., for independence). Under this framework, households jointly choose their long-term care services and living arrangements. Households are assumed to maximize their utility subject to constraints on their budget and their time. Prior to the emergence of assisted living, individuals typically chose between receiving care at home and receiving care in a nursing home. The effect of assisted living capacity on overall long-term care utilization depends on how assisted living influences the choice of long-term care services and living arrangement. The primary factors influencing this decision will include household wealth, the elderly person's functioning, leisure, and the household's preferences (see Figure 1).
Figure 1.
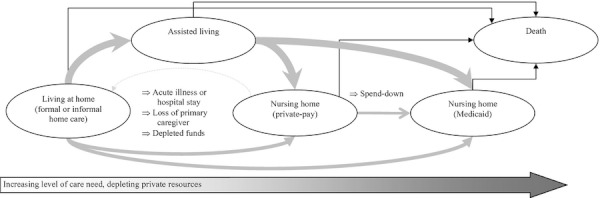
Transitions among Long-Term-Care Options
In terms of household wealth, certain long-term care services may be normal goods (i.e., demand increases with income) while others may be inferior (i.e., demand declines with income), due, perhaps, to the levels of independence associated with different types of services (Goda, Golberstein, and Grabowski 2011). Paid home care and assisted living are typically considered normal goods, suggesting higher household wealth is expected to increase the use of these services. However, given the disutility (i.e., diminished satisfaction) associated with nursing home entry, nursing home care is likely an inferior good, suggesting higher wealth will lead to less nursing home care, ceteris paribus. In terms of impairment, individuals will generally have increasingly complex care needs as they transition from paid home care to assisted living care to nursing home care. The family trades off leisure time in terms of producing these services within the household against purchasing these services in a more intensive setting. Finally, the majority of households have a strong preference for residing in the least restrictive care setting possible.
Thus, with the introduction of assisted living, some less disabled and wealthier individuals—who can no longer live at home and otherwise would have entered a nursing home—are predicted to enter assisted living facilities. If they do eventually need nursing home care, it will typically be because of declining functioning or an acute illness, or because they have exhausted personal resources and choose to enter a nursing home care under the Medicaid entitlement. As such, we hypothesize that an increase in the local supply of assisted living will be associated with fewer private-pay residents and higher patient acuity levels in nursing homes.
Study Data and Methods
Assisted Living Data
No national source of longitudinal data on the supply of assisted living facilities is currently available. However, unique sources of assisted living data, such as licensure registries, are available across different states. Thus, in every state, we contacted the state Medicaid office, state licensure office, or other responsible agency to request their assisted living data. We followed a recent report prepared for the Assistant Secretary for Planning and Evaluation (ASPE) in requesting data for particular classes of facilities within each state (Mollica, Johnson-Lamarche, and O'Keefe 2005). All states were able to provide 2007 data, but we identified only 13 states with detailed longitudinal supply data through 2007 that included facility name, location, and capacity (units). These states were Arizona (data beginning in 2002), Arkansas (2001), California (1993), Colorado (2000), Delaware (2000), Florida (2002), Georgia (2000), Massachusetts (2000), New Jersey (2003), New York (1997), Oregon (1998), South Dakota (2003), and Tennessee (1998).
Reflecting its imprecise definition, assisted living across states includes a wide range of licensure categories for congregate residential facilities beyond just those specifically designated “assisted living” (e.g., residential care facilities, community living arrangements, and personal care homes). Similarly, state definitions for “units” can vary, with some states including only one bed per unit and others including more than one. To construct our sample of “assisted living facilities,” we followed the definition used in the ASPE report surveying states about assisted living facilities (Mollica, Johnson-Lamarche, and O'Keefe 2005). We constructed a market-based measure of assisted living supply at the county level as the number of units per 1,000 residents age 65 and older. In the Appendix, we provide more information about our data collection procedures and the licensure categories across states (see Appendix Table S1).
Nursing Home Data
We obtained nursing home data from two sources. The first source was the Online Survey Certification and Reporting (OSCAR) system for all Medicaid and Medicare certified facilities in our sample states for the period 1993–2007. Certified homes represent almost 96 percent of all facilities nationwide (Strahan 1997). Collected and maintained by the Centers for Medicaid and Medicaid Services (CMS), the OSCAR data indicate whether nursing homes are in compliance with federal regulatory requirements. Every facility is required to have an initial survey to verify compliance. Thereafter, states are required to survey each facility no less often than every 15 months, and the average is about 12 months. Because facilities may be surveyed multiple times or not at all in a given calendar year, we constructed calendar-year estimates by using the most recent OSCAR survey for each facility in operation in a particular calendar year, regardless of whether that survey occurred in an earlier year.
The second source of nursing home data was facility-level case-mix measures generated from the Minimum Data Set (MDS), which were downloaded from Brown University's “Long-Term Care: Facts on Care about the US” (LTCfocUS) website in our sample states for the period 2000–2007. The MDS is a resident-level assessment instrument related to clinical and functional status that is collected at time of admission and then at least quarterly thereafter. The LTCfocUS website provided annual prevalence estimates based on all residents in a facility on the first Thursday in April.
From the OSCAR, we constructed calendar-year estimates of the total number of residents, and the number of residents by payer source. The OSCAR has three primary payer categories: Medicaid, Medicare, and other. Similar to previous OSCAR-based nursing home studies, we identify the private-pay population based on the “other” category, but we recognize that a minority of residents with other payer sources such as the Veteran's Administration are included in this category.
From the aggregate MDS information on the http://LTCfocUS.org website, we obtained three case-mix measures. The first measure was the average Nursing Case Mix Index (NCMI), which approximates the relative staff time associated with caring for different residents. Thus, the higher the NCMI score, the more severe the average acuity profile of the residents in a facility. Second, we obtained the average activities of daily living (ADL) score for all residents in the facility, which ranged from 0 to 28 based on a score of 0 to 4 across seven different ADL categories (bed mobility, transfer, locomotion on unit, dressing, eating, toilet use, and personal hygiene). A score of 0 indicates complete independence, while a score of 28 indicates complete dependence. The final measure relates to the Cognitive Performance Score (CPS), which ranges from 0 (intact) to 6 (very severe impairment). At the facility level, we used a measure indicating the proportion of residents in the nursing home with low (=0, 1, 2) CPS scores. Thus, this measure indicates the share of individuals with better cognitive functioning (i.e., less impairment).
As right-hand variables, we obtained nursing home characteristics from the OSCAR, including non-profit/government and chain ownership status and location within a hospital. Our final OSCAR sample included 5,970 unique nursing homes in 613 counties across 13 states, while our final aggregate MDS sample included 5,289 unique facilities in 612 counties across 13 states.
County Data
Following a number of previous studies, we used the county to approximate the long-term care market (Grabowski 2008). We included time-varying county characteristics from the Bureau of Health Professions Area Resource File (Stambler 1988), which integrates data from the Census Bureau, CMS, Bureau of Labor Statistics, and National Center for Health Statistics. From this file, we obtained median and average household income, unemployment rates, and population estimates for the age groups 65–74, 75–84, and 85 and older to control for population growth. We used the county population age 65 and older as the denominator for the measure of assisted living capacity.
Empirical Specification
Our analysis estimates the effect of market-level assisted living capacity on nursing home utilization by payment type and physical impairment using separate regressions for each facility measure with the nursing home as the unit of observation. (Importantly, the results presented in this article are robust to aggregating the data and employing the county as the unit of observation; see Appendix Table S2.) We employed county and year fixed effects to control for time-invariant, county-specific differences, and for national trends in nursing home utilization. We specified the model as follows:
where NH refers to nursing home outcome i in county c in year t, AL refers to the county-level assisted living capacity, X is a vector of time-varying characteristics at the nursing home and market levels, α and λ are year and county fixed effects, and ε is the randomly distributed error term. This model, which is a common generalization of the most basic differences-in-differences setup, exploits within-county variation over time in the rate of assisted living capacity expansion. That is, the model compares the difference over time in nursing home outcomes in markets with greater growth in assisted living capacity relative to the difference over time in markets with less growth in assisted living capacity.
The nursing home utilization outcomes are the total count of residents and the count of residents by payer source. The key outcome of interest is the number of private-pay residents. We also examined the count of Medicaid and Medicare residents as potential “falsification tests” of our identification strategy. Because assisted living is rarely covered by Medicaid, we expect a minimal effect of assisted living supply on the Medicaid census. Similarly, because assisted living facilities are not a substitute for post-acute Medicare services, we should not observe an effect of assisted living supply on the Medicare census. We examine three aggregate facility case-mix outcomes: a NCMI score, an ADL score, and percent with low CPS (better cognitive functioning).
All models were estimated using least squares, with the standard errors clustered at the market (county) level to adjust for within-county correlation. Importantly, the one outcome expressed as a share of residents in the facility—the percent of low CPS residents—is robust to the use of a logit transformation model. In addition, in the case-mix models, we assigned each facility an analytic weight equal to its total residents, an adjustment which allowed each observation to reflect an average over individuals and put more weight on larger nursing homes.
Results
Growth in Assisted Living Sector
Between 1993 and 2007, the average annual growth rate in county-level assisted living capacity across the 13 states is 6.3 percent (Table 1). The annual growth rate varied considerably between the states in the study sample, from a 2 percent decrease (New York, from 1997 to 2007) to a 12 percent increase (Florida, from 2002 to 2007).
Table 1.
Assisted Living Capacity by State, 1993–2007*
| Facilities/(Units)/Units per 1,000 Elderly | Average Annual Growth† | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1993 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | ||
| AR | 70 (2,833) 10.4 | 87 (3,314) 11.1 | 91 (3,416) 11.4 | 94 (3,674) 12.0 | 97 (3,914) 12.3 | 104 (4,246) 12.6 | 126 (5,108) 15.6 | 8.3% | |||||
| AZ | 945 (17,658) 25.5 | 1,236 (21,911) 31.1 | 1,666 (26,692) 36.6 | 2,040 (29,079) 38.6 | 2,130 (29,578) 38.1 | 1,906 (27,416) 34.6 | 7.1% | ||||||
| CA | 4,475 (106,095) 32.2 | 6,354 (134,342) 38.5 | 6,705 (141,757) 40.3 | 6,941 (154,133) 43.5 | 6,887 (152,913) 42.5 | 6,923 (156,116) 42.7 | 6,951 (159,405) 43.4 | 7,154 (163,014) 43.6 | 7,516 (170,072) 44.9 | 7,757 (171,387) 44.7 | 8,096 (173,863) 45.2 | 7,947 (167,984) 43.2 | 2.4% |
| CO | 469 (11,560) 28.8 | 469 (11,896) 29.1 | 471 (12,488) 29.8 | 478 (12,350) 29.1 | 477 (12,972) 29.7 | 474 (12,896) 28.8 | 459 (12,616) 27.4 | 450 (11,973) 27.2 | −0.8% | ||||
| DE | 25 (1,510) 14.8 | 30 (1,711) 16.6 | 30 (1,711) 16.3 | 31 (1,801) 16.9 | 32 (1,850) 17.0 | 32 (1,848) 16.6 | 32 (1,848) 16.1 | 34 (1,938) 16.4 | 1.5% | ||||
| FL | 1,622 (45,204) 15.9 | 1,649 (47,914) 16.8 | 1,740 (52,448) 18.1 | 1,910 (57,738) 19.6 | 2,248 (67,716) 22.8 | 2,518 (75,547) 25.3 | 11.8% | ||||||
| GA | 1,747 (23,974) 32.3 | 1,795 (25,533) 34.0 | 1,817 (25,825) 33.5 | 2,027 (26,840) 33.7 | 2,168 (27,048) 33.4 | 2,333 (28,084) 33.2 | 2,414 (28,319) 32.2 | 2,402 (26,241) 32.7 | 0.2% | ||||
| MA | 147 (8,962) 10.5 | 152 (9,473) 11.2 | 162 (10,130) 12.0 | 165 (10,277) 12.1 | 175 (10,772) 12.8 | 181 (11,189) 13.3 | 188 (11,518) 13.6 | 192 (11,682) | 4.2% | ||||
| NJ | 192 (16,207) 14.5 | 197 (16,585) 14.8 | 205 (17,355) 15.5 | 210 (17,825) 15.9 | 209 (17,906) 15.8 | 2.2% | |||||||
| NY | 604 (46,650) 19.4 | 629 (49,065) 20.5 | 650 (51,037) 21.1 | 642 (51,288) 21.0 | 660 (53,097) 21.7 | 634 (50,733) 20.6 | 623 (49,361) 19.9 | 586 (46,286) 18.6 | 565 (44,975) 17.9 | 540 (42,397) 16.9 | 509 (39,065) 15.6 | −2.0% | |
| OR | 256 (12,500) 28.9 | 299 (14,757) 34.0 | 351 (17,226) 39.5 | 389 (19,136) 43.6 | 413 (20,650) 46.4 | 433 (21,471) 47.7 | 431 (21,371) 46.9 | 436 (21,742) 46.9 | 437 (22,209) 46.9 | 435 (21,252) 46.6 | 6.8% | ||
| SD | 155 (3,241) 32.4 | 156 (3,340) 33.0 | 160 (3,540) 34.1 | 155 (3,537) 33.5 | 156 (2,723) 32.0 | −0.3% | |||||||
| TN | 190 (6,935) 11.9 | 250 (10,402) 17.4 | 279 (12,156) 19.6 | 294 (12,877) 20.3 | 296 (13,194) 20.3 | 299 (13,290) 20.2 | 303 (13,562) 20.4 | 318 (14,014) 20.6 | 325 (14,304) 20.4 | 332 (14,254) 20.5 | 8.0% | ||
Data for California in years 1994–1996 not shown but included in the analysis. See Appendix Table S3 for full series.
Calculated using log difference in units per 1,000 elderly.
Nursing Home Characteristics and Assisted Living Capacity
A total of 5,790 unique nursing facilities in 613 counties were included in this study, with an average of 7.4 observations per facility. On average, facilities had 99 residents including 20.40 private-pay, 11.57 Medicare, and 67.34 Medicaid residents (Table 2). The mean resident NCMI score was 0.84 and the average ADL score was 16.24. The average facility had 43.7 percent of residents with a low CPS score. Facilities were predominantly for-profit owned and approximately half were part of a nursing-home chain. During the study period, 1.2 percent of facilities closed (excluding nominal closures for re-licensing). Mean county-level assisted living capacity was 29 units per 1,000 elderly persons.
Table 2.
Mean Values for Analysis Variables, 1993–2007 (N = 42,581)
| Dependent Variables | Mean (SD) | Data Source |
|---|---|---|
| Total residents at facility | 99.31 (74.31) | OSCAR |
| Private-pay residents | 20.40 (20.75) | OSCAR |
| Medicare residents | 11.57 (15.66) | OSCAR |
| Medicaid residents | 67.34 (62.28) | OSCAR |
| Nursing Case-Mix Index (NCMI)* | 0.84 (0.12) | MDS (via http://LTCfocUS.org) |
| Activities of Daily Living score* | 16.24 (3.21) | MDS (via http://LTCfocUS.org) |
| % Low Cognitive Performance Score† | 43.67 (15.87) | MDS (via http://LTCfocUS.org) |
| Independent variables | ||
| Assisted living units (per 1,000 elderly) | 29.27 (14.79) | Collected by authors |
| Nursing home: Government owned | 0.05 | OSCAR |
| Nursing home: Non-profit owned | 0.26 | OSCAR |
| Nursing home: Hospital-based | 0.12 | OSCAR |
| Nursing home: Part of a chain | 0.51 | OSCAR |
| Median household income (000's) | 44.87 (12.11) | ARF |
| Median per-capita income (000's) | 31.74 (10.21) | ARF |
| % persons in poverty | 0.13 (0.05) | ARF |
| Percent unemployed | 5.61 (2.37) | ARF |
| County population, millions | 1.93 (3.01) | ARF |
| County population aged 65–74, thousands | 107.71 (157.93) | ARF |
| County population aged 75–84, thousands | 71.34 (101.17) | ARF |
| County population age 85 and older, thousands | 24.88 (34.79) | ARF |
Standard deviations are reported in parentheses below means for continuous variables.
N = 29,867.
N = 28,292.
ARF, area resource file; MDS, minimum data set; OSCAR, Online Survey Certification and Reporting System.
Effect of Assisted Living Capacity on Nursing Home Utilization
Table 3 shows the estimated effect of changes in assisted living capacity (i.e., the number of assisted living units per 1,000 persons over 65) on nursing home occupancy. Assisted living is negatively associated with total nursing home occupancy, which is consistent with its posited role as a substitute for nursing home care. Consistent with our expectation that assisted living facilities attract primarily private-pay residents, the results indicate that an additional unit of assisted living capacity per 1,000 persons over 65 is associated (p < .01) with a 0.099 decrease in private-pay nursing home census. Put differently, a 10 percent increase in the county-level assisted living capacity leads to a 1.4 percent decline in private-pay nursing home occupancy at the mean.
Table 3.
Effect of Assisted Living Capacity on Nursing Home Characteristics†
| Dependent variable | Coeff (SE) | N |
|---|---|---|
| Utilization models | ||
| Total residents at facility | −0.145* (0.057) | 42,581 |
| Private-pay residents | −0.099** (0.026) | 42,581 |
| Medicare residents | −0.001 (0.018) | 42,581 |
| Medicaid residents | −0.044 (0.047) | 42,581 |
| Case-mix models‡ | ||
| Nursing Case-Mix Index | 0.00059** (0.00013) | 29,867 |
| Activities of Daily Living score | 0.0334** (0.0056) | 29,867 |
| % Low Cognitive Performance Score | −0.044* (0.023) | 28,292 |
Statistical significance noted as follows: **p < .01, * p < .05
Robust standard errors, reported in parentheses below estimates, are calculated using clustering at the market (county) level.
All the regressions include the independent variables listed in Table 2 as well as year and county fixed effects.
Assisted living capacity is defined herein as county units per 1,000 persons over age 65.
Case-mix models are weighted by number of residents per facility.
Given that assisted living has relatively little Medicaid coverage and is not a substitute for Medicare-financed post-acute nursing home care, we would not expect the emergence of assisted living to have an effect on the number of Medicaid or Medicare nursing home residents. Indeed, when we conduct this falsification test, the association between assisted living supply and the number of Medicare or Medicaid residents is not statistically significant.
Another possible implication of assisted living growth is nursing home closure. In a sensitivity analysis (not shown), we found no statistically significant association between assisted living growth and the likelihood of nursing home closure. As an additional robustness check (see Appendix Table S4), we estimated the utilization models with data only from 1999 to 2007. This check addresses any possible bias from the introduction of the Medicare skilled nursing facility (SNF) prospective payment system in 1998. The results were nearly identical to those presented in the article.
Effect of Assisted Living Capacity on Nursing Home Case-Mix
Based on our conceptual framework, assisted living should attract lower case-mix (i.e., less physically impaired) residents from the nursing home population. Indeed, across all three case-mix outcomes, we found support for this relationship. Specifically, a one-unit capacity increase (per 1,000 elderly) is associated (p < .01) with a 0.00059 increase in NCMI score and a 0.0334 increase in ADL score. Similarly, this one-unit increase was associated (p < .05) with a 0.044 percentage point decline in low CPS residents. At the mean values, a 10 percent increase in assisted living capacity is associated with a 0.2 percent increase in NCMI score, a 0.6 percent increase in ADL score, and a 0.3 percent decrease in low CPS residents. From a clinical perspective, these effect sizes are relatively modest, given that a 0.6 percent increase in ADL score translates into a 0.1 increase in the ADL score (relative to a mean of 16.24).
Discussion
Understanding the factors that affect where consumers receive long-term care and how it is financed are important aspects of maintaining a system that meets the needs of elderly and disabled individuals. Although descriptive aspects of the growth in assisted living have been explored, little empirical work has assessed how these market changes affect the volume and acuity of care in nursing homes. This study presents new data on the potential linkage between the emergence of assisted living and changes in nursing home utilization. We examine the effect of assisted living growth on nursing homes using panel data techniques to control for national trends and time-fixed nursing home and regional characteristics.
Our main findings suggest that assisted living capacity has a modest but significant impact on who uses nursing home care and how it is financed. Specifically, a 10 percent increase in assisted living capacity led to a 1.4 percent decline in private-pay occupancy and a 0.2–0.6 percent increase in overall patient acuity. The acuity effects are relatively modest, but they should be viewed in light of the fact that the OSCAR measures reflect case-mix across all residents in the facility (and not simply the private-payers). Although demographic and policy factors may partially explain these changes, our results suggest that growth in the assisted living sector contributed to changes in the nursing home sector. The vast majority of individuals who receive care in an assisted living facility most likely would not otherwise reside in a nursing home; however, at the margin, our results suggest assisted living attracted away some private-pay, lower acuity nursing home residents. This finding has implications for policy makers, providers, and consumers.
For policy makers, the growth in assisted living alters the implications of several key nursing home policies. Historically, the nursing home market has relied on certificate-of-need (CON) and construction moratoria to hold down the supply of nursing home beds. However, these capacity constraints are no longer binding in many nursing home markets. Indeed, states are shifting their focus from limiting bed expansion to eliminating excess bed capacity. For example, New York State has proposed the elimination of underused nursing home beds, which could result in facility closures (Hernandez and Baker 2005). Another key nursing home policy is the level and method of Medicaid payment for services. Historically, in the context of stringent CON policies, more generous Medicaid payment was not found to increase the quality of care (Nyman 1985; Gertler 1989). However, recent research suggests a more competitive nursing home sector in which homes compete on the basis of quality for the care of Medicaid recipients (Grabowski 2001).
In addition to changes in nursing home policy, state lawmakers have turned their attention to the growing assisted living sector. According to a 2007 study by the National Academy for State Health Policy, 115,000 assisted living residents received some Medicaid assistance (Mollica, Sims-Kastelein, and O'Keefe 2008). As of 2009, 12 states had certificate-of-need requirements for assisted living: Alaska, Arkansas, Connecticut, Georgia, Kentucky, Massachusetts, Mississippi, Missouri, New Jersey, New York, North Carolina, and West Virginia (National Conference of State Legislatures 2009). A central issue for state Medicaid programs will be how to allocate dollars across assisted living and other long-term care settings. The assisted living setting has the potential to serve as a substitute to nursing home care. However, it is also an attractive option for individuals who would not otherwise enter a nursing home. Our results provide evidence that assisted living does substitute for nursing home care, at least for certain individuals. From a budgetary perspective, a key issue is whether coverage for assisted living can be structured to enhance substitution away from Medicaid-financed nursing home care while minimizing substitution away from unpaid care by family and friends.
From the perspective of the nursing home industry, the continued growth in assisted living and other nursing home substitutes has increased competition for potential residents. Nursing homes, which historically have operated near capacity, are now struggling to fill beds. When the reduction in occupancy rates is coupled with other industry trends including Medicaid payment freezes, high liability insurance costs, and a shortage of registered nurses, the nursing home sector faces an uncertain future. In the short-term, facility closures and consolidation will likely occur in many markets. Moving forward, it will be important to continue monitoring quality of care in the context of these changes.
From the consumer perspective, the emergence of assisted living can largely be viewed as a positive development. Given that private-paying consumers continue to “vote with their feet” (and their dollars) in favor of assisted living, a strong preference clearly exists for this care model. However, it is worth noting that the assisted living sector is still a nascent one. Wide variability exists across facilities in the types of services offered and across states in the degree of government involvement as a payer and regulator of services. Presumably, variation is also present in the quality of care provided (Frytak et al. 2001; Zimmerman et al. 2005). Relative to the Nursing Home Compare and Home Health Compare initiatives, however, few government resources are available to guide consumer choice. If Medicaid becomes more involved as a payer of assisted living services in the coming years, the government's role as an overseer and regulator of care presumably will evolve as well. For those consumers whose care needs require more intensive nursing home services, a robust assisted living sector will pose both benefits and costs. On the positive side, as mentioned above, nursing homes have been shown to compete on the basis of quality in the context of a more competitive nursing home market (Grabowski 2001). However, if assisted living is competing away higher revenue private-pay residents, then nursing homes will have fewer resources for direct patient care for all residents (Grabowski, Gruber, and Angelelli 2008).
Importantly, other possible explanations exist for changes in the nursing home sector over the past two decades. From a demographic perspective, elderly individuals are living longer with declining disability rates (Manton, Stallard, and Liu 1993; Cutler 2001). Lakdawalla and Philipson (2002) assert that the narrowing longevity gap among men and women coupled with declining disability explains some of the decline in nursing home utilization. From a policy perspective, several changes may have contributed to the shifts we have observed in the nursing home sector. The expansion of Medicaid home- and community-based services has contributed to lower nursing home occupancy in many parts of the country (Bishop 1999). On the post-acute side of the nursing home market, hospital and nursing home payment changes have led to an increase in the volume and acuity of SNF residents (Grabowski, Afendulis, and McGuire 2011). Finally, some of the increase in acuity over the period of study may be related to the adoption of Medicaid case-mix payment systems, which reward nursing homes for caring for sicker patients (Feng et al. 2006). As of 2004, Medicaid nursing home case-mix reimbursement was available in 35 states, up from 19 states in 1991 (Grabowski et al. 2008).
Although our results are suggestive of a causal pathway between assisted living capacity and selected nursing home outcomes, we acknowledge that the market-level supply of assisted living may not be exogenous. That is, we may have a case of reverse causality in which changes in nursing home outcomes are leading to changes in assisted living capacity. However, when we estimated a lagged model (see Appendix Table S5), we observed very similar effects to those presented herein, suggesting temporal precedence of assisted living growth to changes in nursing home capacity. In addition, some unobservable (time-varying) factor that is correlated with assisted living supply and our nursing home outcomes of interest may have biased our results. Importantly, our falsification tests using Medicare and Medicaid residents provide strong support for the validity of our identification strategy. Nevertheless, future research on this topic should explore an instrumental variable approach, although the identification of an instrument that predicts assisted living growth and is otherwise unrelated to changes in our nursing home outcomes will be challenging. Another potential limitation is the generalizability of our 13 study states to the entire United States. Although these states are heterogeneous with respect to size, geography, and long-term care utilization, assisted living growth in these states may be different relative to other states. With data from additional localities, we could also examine the role of state policies, market competition and other factors toward modifying the aggregate effects observed in this article. Moving forward, more states should prioritize the collection and reporting of longitudinal assisted living data.
In sum, the results of our analyses provide the first empirical evidence of the impact of assisted living growth on the market for nursing home care. The results confirm the interdependency of different long-term care sectors and highlight the need for policy makers and researchers to consider policies or changes across care settings using a system-based perspective.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by funding from the Changes in Health Care Financing and Organization (HCFO) Initiative of the Robert Wood Johnson Foundation (grant no. 61511). We are grateful to Laura Coots for her assistance in the collection of the assisted living data used in this study.
Disclaimers: No funding source played a role in the design or conduct of the study; the collection, analysis, or interpretation of data; or the preparation, review, or approval of this manuscript.
Note
A commonly cited definition of assisted living is put forward by the Assisted Living Quality Coalition (1998), a group of providers and consumer groups. The Coalition defines assisted living as “a congregate residential setting that provides or coordinates personal services, 24-hour supervision and assistance (scheduled and unscheduled), activities, and health related services” (p. 65). The definition goes on to identify several key objectives, including minimizing residents' need to move; accommodating residents' changing needs and preferences; maximizing residents' dignity, autonomy, privacy, independence, and safety; and encouraging family and community involvement.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Table S1. Assisted Living Facility Types Included in Our Data Collection, by State.
Table S2. County-Level Regressions.
Table S3. California Assisted Living Capacity, 1993–2007.
Table S4. Exclusion of Pre-1999 Observations.
Table S5. Lagged Dependent Variable Models.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Assisted Living Quality Coalition. Assisted Living Quality Initiative: Building a Structure That Promotes Quality. Washington, DC: Assisted Living Quality Coalition; 1998. [Google Scholar]
- Bishop CE. “Where Are the Missing Elders? The Decline in Nursing Home Use, 1985 and 1995”. Health Affairs. 1999;18(4):146–55. doi: 10.1377/hlthaff.18.4.146. [DOI] [PubMed] [Google Scholar]
- Brodie M, Blendon R. National Survey on Nursing Homes. Menlo Park, CA: Kaiser Family Foundation; 2001. [Google Scholar]
- Cutler DM. “Declining Disability among the Elderly”. Health Affairs. 2001;20(6):11–27. doi: 10.1377/hlthaff.20.6.11. [DOI] [PubMed] [Google Scholar]
- Feng Z, Grabowski DC, Intrator O, Mor V. “The Effect of State Medicaid Case-Mix Payment on Nursing Home Resident Acuity”. Health Services Research. 2006;41(4 Pt 1):1317–36. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frytak JR, Kane RA, Finch MD, Kane RL, Maude-Griffin R. “Outcome Trajectories for Assisted Living and Nursing Facility Residents in Oregon”. Health Services Research. 2001;36(1 Pt 1):91–111. [PMC free article] [PubMed] [Google Scholar]
- Gertler PJ. “Subsidies, Quality, and the Regulation of Nursing Homes”. Journal of Public Economics. 1989;38(1):33–52. [Google Scholar]
- Gibson MJ, Gregory SR, Houser AN, Fox-Grade W. Across the States: Profiles of Long-Term Care (Sixth Edition) Washington, DC: AARP Public Policy Institute; 2004. [Google Scholar]
- Goda GS, Golberstein E, Grabowski DC. “Income and the Utilization of Long-Term Care Services: Evidence from the Social Security Benefit Notch”. Journal of Health Economics. 2011;30(4):719–29. doi: 10.1016/j.jhealeco.2011.04.001. [DOI] [PubMed] [Google Scholar]
- Grabowski DC. “Medicaid Reimbursement and the Quality of Nursing Home Care”. Journal of Health Economics. 2001;20(4):549–69. doi: 10.1016/s0167-6296(01)00083-2. [DOI] [PubMed] [Google Scholar]
- Grabowski DC. “The Cost-Effectiveness of Noninstitutional Long-Term Care Services: Review and Synthesis of the Most Recent Evidence”. Medical Care Research and Review. 2006;63(1):3–28. doi: 10.1177/1077558705283120. [DOI] [PubMed] [Google Scholar]
- Grabowski DC. “The Market for Long-Term Care Services”. Inquiry. 2008;45(1):58–74. doi: 10.5034/inquiryjrnl_45.01.58. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Afendulis CC, McGuire TG. “Medicare Prospective Payment and the Volume and Intensity of Skilled Nursing Facility Services”. Journal of Health Economics. 2011;30(4):675–84. doi: 10.1016/j.jhealeco.2011.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, Gruber J, Angelelli JJ. “Nursing Home Quality as a Common Good”. Review of Economics and Statistics. 2008;90(4):754–64. doi: 10.1162/rest.90.4.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, Feng Z, Intrator O, Mor V. “Medicaid Nursing Home Payment and the Role of Provider Taxes”. Medical Care Research and Review. 2008;65(4):514–27. doi: 10.1177/1077558708315968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes C, Rose M, Phillips CD. A National Study of Assisted Living for the Frail Elderly: Results of a National Survey of Facilities. Beachwood, OH: Meyers Research Institute; 1999. [Google Scholar]
- Hawes C, Phillips CD, Rose M, Holan S, Sherman M. “A National Survey of Assisted Living Facilities”. Gerontologist. 2003;43(6):875–82. doi: 10.1093/geront/43.6.875. [DOI] [PubMed] [Google Scholar]
- Hernandez R, Baker A. New York Times; 2005. “Close Hospitals, Pataki Says in Medicaid Cost Proposal”. [Google Scholar]
- Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. National Nursing Home Survey: 2004 Overview. Hyattsville, MD: National Center for Health Statistics, Vital Health Statistics; 2009. 13(167) [PubMed] [Google Scholar]
- Lakdawalla D, Philipson T. “The Rise in Old-Age Longevity and the Market for Long-Term Care”. American Economic Review. 2002;92(1):295–306. doi: 10.1257/000282802760015739. [DOI] [PubMed] [Google Scholar]
- Manton KG, Stallard E, Liu K. “Forecasts of Active Life Expectancy: Policy and Fiscal Implications”. The Journal of Gerontology. 1993;48(Special Issue):11–26. doi: 10.1093/geronj/48.special_issue.11. [DOI] [PubMed] [Google Scholar]
- MetLife Mature Market Institute. Market Survey of Long-Term Care Costs. Westport, CT: Metropolitan Life Insurance Company; 2010. [Google Scholar]
- Mollica R, Johnson-Lamarche H, O'Keefe J. State Residential Care and Assisted Living Policy. Portland, ME: National Academy for State Health Policy; 2005. [Google Scholar]
- Mollica R, Sims-Kastelein K, O'Keefe J. Assisted Living and Resisent Care Policy Compendium, 2007 Update. Portland, ME: National Academy for State Health Policy; 2008. [Google Scholar]
- Morgan L, Gruber-Baldini A, Magaziner J. “Resident Characteristics”. In: Zimmerman S, Sloane P, Eckert J, editors. Assisted Living: Needs, Practices, and Policies in Residential Care for the Eldelry. Baltimore, MD: Johns Hopkins University Press; 2001. pp. 144–72. [Google Scholar]
- National Conference of State Legislatures. 2009. “Certificate of Need: State Health Laws and Programs” [accessed on May 25, 2009]. Available at http://www.ncsl.org/IssuesResearch/Health/CONCertificateofNeedStateLaws/tabid/14373/Default.aspx#resources.
- Nyman JA. “Prospective and ‘Cost-Plus’ Medicaid Reimbursement, Excess Medicaid Demand, and the Quality of Nursing Home Care”. Journal of Health Economics. 1985;4(3):237–59. doi: 10.1016/0167-6296(85)90031-1. [DOI] [PubMed] [Google Scholar]
- Nyman JA, Finch M, Kane RA, Kane RL, Illston LH. “The Substitutability of Adult Foster Care for Nursing Home Care in Oregon”. Medical Care. 1997;35(8):801–13. doi: 10.1097/00005650-199708000-00006. [DOI] [PubMed] [Google Scholar]
- Pezzin LE, Kemper P, Reschovsky J. “Does Publicly Provided Home Care Substitute for Family Care? Experimental Evidence with Endogenous Living Arrangements”. Journal of Human Resources. 1996;30(3):650–76. [Google Scholar]
- Reinardy JR, Kane RA. “Anatomy of a Choice: Deciding on Assisted Living or Nursing Home Care in Oregon”. Journal of Applied Gerontology. 2003;22(1):152–74. [Google Scholar]
- Spillman B, Liu K, McGillard C. Trends in Residential Long-Term Care: Use of Nursing Homes and Assisted Living and Characteristics of Facilities and Residents. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2002. [Google Scholar]
- Stambler HV. “The Area Resource File–A Brief Look”. Public Health Reports. 1988;103(2):184–8. [PMC free article] [PubMed] [Google Scholar]
- Stevenson DG, Grabowski DC. “Sizing up the Market for Assisted Living”. Health Affairs. 2010;29(1):35–43. doi: 10.1377/hlthaff.2009.0527. [DOI] [PubMed] [Google Scholar]
- Stevenson DG, Murtaugh CM, Feldman PH, Oberlink MR. Policy Brief. Vol. 3. New York: Center for Home Care Policy and Research, Visiting Nurse Service of New York; 2000. “Expanding Publicly Financed Assisted Living and Other Residential Alternatives for Disabled Older Persons: Issues and Options”; pp. 1–6. [PubMed] [Google Scholar]
- Strahan GW. An Overview of Nursing Homes and Their Current Residents: Data from the 1995 National Nursing Home Survey. Rockville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 1997. [Google Scholar]
- Waidmann T, Thomas S. Estimates of the Risk of Long-Term Care: Assisted Living and Nursing Home Facilities. Washington, DC: Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2003. [Google Scholar]
- Zimmerman S, Sloane PD, Williams CS, Reed PS, Preisser JS, Eckert JK, Boustani M, Dobbs D. “Dementia Care and Quality of Life in Assisted Living and Nursing Homes”. Gerontologist. 2005;45(Spec No 1(1)):133–46. doi: 10.1093/geront/45.suppl_1.133. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


