Abstract
Collecting quality of life (QOL) data longitudinally from burn survivors is difficult; especially if they live in geographically distant areas from the burn center. Although mailed surveys can be used, response rates to these surveys may be low. The purpose of this feasibility study was to examine the use of the videophone to collect QOL data from burn patients over 5 time points after discharge from the U.S. Army Institute of Surgical Research Burn Center. Twenty-five patients agreed to participate, using the Starview 2000 Pro II videophone. Participant satisfaction with the technology was measured using the Telemedicine Perception Questionnaire. Qualitative comments from participants and the researchers conducting the videophone data collection sessions also were collected. Military participants were approximately 20 years younger than civilian participants. Most burns were from a thermal cause and civilian patients had a slightly shorter length of stay in the burn center than military participants. The majority of participants were relatively happy with the telehealth technology, rating it with a mean score of 61.84 out of a possible total score of 85. Qualitative comments also reflected a positive attitude about the use of the videophone for research data collection; 60% of the participants said they remained in the study because they were allowed to use the videophone rather than using only the telephone or a mailed survey. The researchers collecting the data also commented about the ease of using the videophone. Negative comments were related to dropped calls or lack of audio or video at certain times. Findings from this study are consistent with the two other studies that reported use of telemedicine to clinically evaluate burn patients. With the rapid advancement of technology, QOL research data could be collected longitudinally from burn patients by using laptops with high resolution, portable video cameras.
Keywords: Burns, telemedicine, videophone, quality of life, outcomes studies
Introduction
Telemedicine has been defined as the use of telecommunications technologies to provide medical services and information [1]. To date, telemedicine has primarily been used for diagnostic purposes [2-4], delivering psychiatric [5,6] and chronic illness [7,8] interventions, and providing physician consultation [9-11]. The technology, however, is available to all providers within the healthcare team, to include researchers. Through the use of telehealth, nurses, physicians, and researchers have the ability to reach patients at home, especially in rural communities [12]. Frequent, immediate access to patients and their families at home provides the opportunity for assessment, education, compliance monitoring, early identification of patient problems, and unprecedented access to people that are otherwise geographically remote [13].
In general, patient satisfaction with telemedicine-delivered health care and information was demonstrated to be high [4,14-17]. Patients consistently rated involvement with both telemedicine-based consultations and home telemedicine-delivered care as positive. This is a consistent theme throughout the telemedicine literature; however, Mair & Whitten [18] pointed out the generalizability of these studies is limited due to a failure to fully explain the reasons underlying patient/family satisfaction or dissatisfaction with telehealth. Only one study [19] was found that examined the suitability of the use of telemedicine technology (videophones) for conducting research. Although the utility of the telephone as a vehicle for collecting clinical research has been explored [20], no studies have examined the use of telemedicine to obtain research data concerning quality of life (QOL) experienced by burn patients.
The purpose of this paper is to report a feasibility study directed at examining the utility and acceptance of the videophone to collect QOL data from burn patients for 18 months after being discharged from the burn center. Specifically, the research questions for this study were: 1) Will the use of telemedicine technology allow enhanced communication and data collection for researchers? 2) What are the patients’ perceptions of the use of telemedicine technology for research purposes? and 3) What are the researchers’ perceptions of the use of telemedicine technology for the collection of research data?
Materials and methods
This feasibility study, consisting of 25 participants, was part of a larger prospective, descriptive, repeated-measures study examining the QOL of burn patients over 18 months after discharge from the U.S. Army Institute of Surgical Research (USAISR) Burn Center, Fort Sam Houston, TX. This unit serves both U.S. Department of Defense beneficiaries from around the world, and civilians from the South Texas region. The study was approved by the institutional review boards of Brooke Army Medical Center and The Uniformed Services University of the Health Sciences. All participants were recruited for the study within 72 hours of discharge from the Burn Center and met the following inclusion criteria: hospitalization for a burn injury requiring excision and grafting, at least 18 years of age, and the ability to speak/read English and provide informed consent. Additional inclusion criteria for the telemedicine aspect of the study included access to a telephone landline and the capability to operate simple technological equipment. The insertion of telemedicine technology, specifically the videophone, in the ongoing larger study was expected to enhance data collection activities from burn patients that were living in areas away from the Burn Center.
Procedure
Twenty-five Starview Videotelephone 2000 Pro II Portable videophones (Figure 1) were purchased as commercial off-the-shelf (COTS) telemedicine technology. The videophone used the patients’ existing home telephone lines and regular 110 volt power plugs. Customized, ruggedized cases were provided to accommodate transport in a car, truck, or on an airplane when patients were discharged home or to a military duty station. All necessary phone cables and plugs were provided along with 100 feet of telephone line in case the phone jack in the patient’s home was away from a window or light source, which was needed for high quality viewing. The videophones were configured and readied for use within 90 days of the initiation of the feasibility study. Patient user manuals were developed, edited, piloted with 3 patients, and printed. Additionally, telemedicine training was provided on site for the research staff to facilitate integration of the feasibility study participants into the larger research protocol. After providing consent, participants were asked to complete all instruments at the time of hospital discharge, as well as 3, 6, 12, and 18 months after discharge from the Burn Center.
Figure 1.
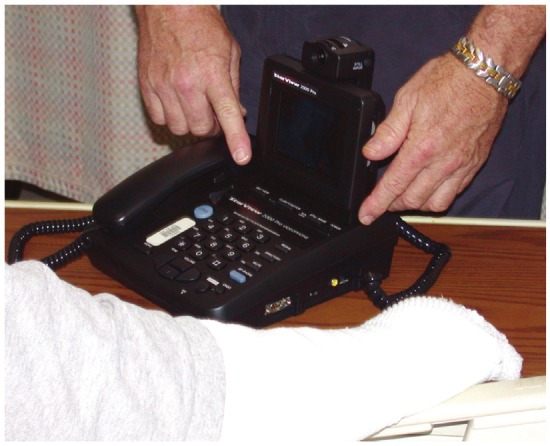
Starview Videophone.
Instruments
All participants completed an instrumentation booklet consisting of several QOL instruments, a demographic data sheet, a clinical data sheet, and the Telemedicine Perception Questionnaire (TMPQ). The demographic data sheet was used to collect pertinent information concerning the demographic characteristics of the participants such as age, gender, ethnicity, education, marital status, employment prior to burn etc. The clinical data sheet was used to collect information from the patients and their medical records, such as: burn severity, body burn site, amputations, type of rehabilitation needed as an out-patient, and AMA disability score.
Telemedicine Perception Questionnaire (TMPQ)
To determine the participants’ experiences regarding the use of the videophone for data collection, the TMPQ was administered. Permission was obtained from the researchers who developed the TMPQ at the University of Minnesota [21,22]. The TMPQ measures perceptions of telemedicine use in the home. It includes 17 items that address various components to include ease of equipment use, acceptability of virtual visits, time and cost savings, issues of privacy and confidentiality, and general perceptions of home use of telemedicine. The response categories for the TMPQ consist of a five point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree. Scores are summed and can range from 17-85, with higher scores indicating higher positive perceptions of satisfaction with telemedicine in the home. Cronbach’s alpha was reported at .80, indicating good internal consistency and reliability [21,22]. The TMPQ has been used in studies of elderly patients with either congestive heart failure, chronic obstructive pulmonary disease, or those requiring wound care [22]. It has since been used in several home-based tele-health studies [23,24]. In this study the TMPQ was used to determine participants’ perceptions regarding the use of the videophones for research data collection.
Qualitative comments
Participants’ qualitative comments concerning their experiences with the videophone also were obtained. Furthermore, qualitative data were obtained from the research team members obtaining the data from the participants. Research team members were asked about the quality of audio and video transmissions as well as the overall ease of use, number of dropped calls, and number of calls needed to obtain a good connection with the participant.
Results
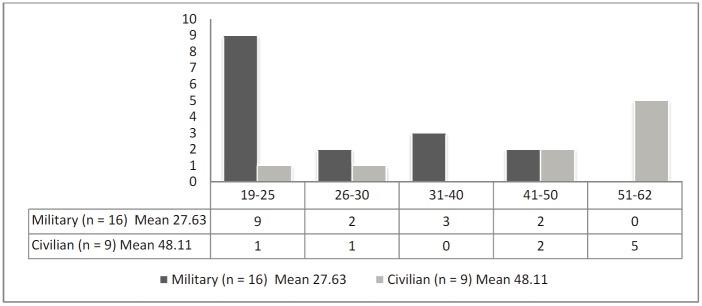
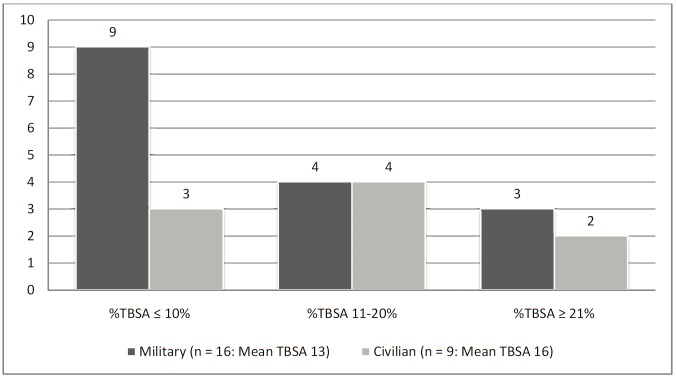
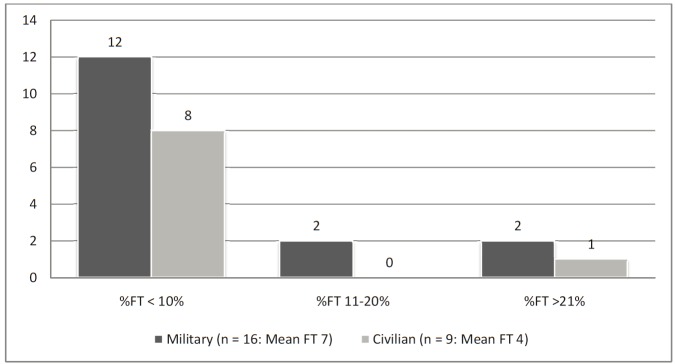
Because this was a feasibility study, all findings are reported descriptively using measures of central tendency, graphical display, and content analyses of qualitative comments. The demographic characteristics of the 25 participants in the study are depicted in Table 1 based on their status as a military service member or civilian emergency patient treated in the Burn Center. In the aggregate, the participants ranged from 19-62 years (Figure 2), were primarily male, and came from a variety of racial/ethnic backgrounds. Table 2 depicts clinical information about the participants based on their status as a military service member or civilian emergency patient. The percentage of total body surface area burned (TBSA) ranged from 2% to 51% with an average of 14% (Figure 3). Most participants were categorized as “assistance needed” in their discharge summary (80%; n = 20), and 92% required some type of compression garment. Participants’ average length of stay was 48 days, with a range of 9-241 days. The results clearly indicated that civilian emergencies were older, had a shorter length of stay, and had a slightly smaller percentage of full-thickness burns (Figure 4).
Table 1.
Demographic Characteristics of Participants
| Variable | Civilian n = 9 | Military n = 16 | ||||
|---|---|---|---|---|---|---|
| Age | Mean 48.11 | Median 54 | SD 14.64 | Mean 27.63 | Median 24.50 | SD 7.67 |
|
| ||||||
| Frequency | % | Frequency | % | |||
|
| ||||||
| 19-25 | 1 | 4 | 9 | 36 | ||
| 26-30 | 1 | 4 | 2 | 8 | ||
| 31-40 | 0 | 0 | 3 | 12 | ||
| 41-50 | 2 | 8 | 2 | 8 | ||
| 51-62 | 5 | 20 | 0 | 0 | ||
|
| ||||||
| Gender | ||||||
|
| ||||||
| Female | 1 | 4 | 1 | 4 | ||
| Male | 8 | 32 | 15 | 60 | ||
|
| ||||||
| Race/Ethnicity | ||||||
|
| ||||||
| Caucasian | 6 | 24 | 10 | 40 | ||
| African American | 0 | 0 | 2 | 8 | ||
| Hispanic | 3 | 12 | 3 | 12 | ||
| American Indian | 0 | 0 | 1 | 4 | ||
|
| ||||||
| Marital Status | ||||||
|
| ||||||
| Married | 7 | 28 | 6 | 24 | ||
| Single | 2 | 8 | 8 | 32 | ||
| Other | 0 | 0 | 2 | 8 | ||
|
| ||||||
| Social History: Number of Dependents | ||||||
|
| ||||||
| 0 | 3 | 12 | 8 | 32 | ||
| 1 | 2 | 8 | 3 | 12 | ||
| 3 | 2 | 8 | 4 | 16 | ||
| 4 | 2 | 8 | 1 | 4 | ||
|
| ||||||
| Currently Employed | ||||||
|
| ||||||
| Yes | 9 | 36 | 16 | 64 | ||
|
| ||||||
| Income Level | ||||||
|
| ||||||
| 19,999 or less | 2 | 8 | 2 | 8 | ||
| 20K-39,999 | 3 | 12 | 11 | 44 | ||
| 40K-59,999 | 2 | 8 | 3 | 12 | ||
| 60K or greater | 2 | 8 | 0 | 0 | ||
|
| ||||||
| Education Level | ||||||
|
| ||||||
| Some HS | 2 | 8 | 1 | 4 | ||
| HS Graduate | 1 | 4 | 7 | 28 | ||
| Vocational/Tech | 0 | 0 | 2 | 8 | ||
| Some College | 2 | 8 | 5 | 20 | ||
| College Graduate | 3 | 12 | 1 | 4 | ||
| Graduate School | 1 | 4 | 0 | 0 | ||
Figure 2.
Ages of Participants.
Table 2.
Clinical Characteristics of Participants
| Variable | Civilian n = 9 | Military n = 16 | ||||
|---|---|---|---|---|---|---|
| Days Post Burn | Mean 25 | Median 19 | SD 18 | Mean 65 | Median 23 | SD 77 |
|
| ||||||
| Frequency | % | Frequency | % | |||
|
| ||||||
| 10-15 | 3 | 12 | 3 | 12 | ||
| 16-20 | 3 | 12 | 5 | 20 | ||
| 21-50 | 2 | 8 | 2 | 8 | ||
| 51-100 | 1 | 4 | 3 | 12 | ||
| 101-247 | 0 | 0 | 3 | 12 | ||
|
| ||||||
| Length of Stay (Days) | Mean 23 | Median 14 | St. Deviation 18 | Mean 62 | Median 20 | St. Deviation 77 |
|
| ||||||
| 9-12 | 3 | 12 | 3 | 12 | ||
| 13-15 | 2 | 8 | 3 | 12 | ||
| 16-20 | 1 | 4 | 2 | 8 | ||
| 21-50 | 2 | 8 | 2 | 8 | ||
| 51-100 | 1 | 4 | 3 | 12 | ||
| 101-241 | 0 | 0 | 3 | 12 | ||
|
| ||||||
| %TBSA | Mean 16 | Median 11 | St. Deviation 15 | Mean 13 | Median 8 | St. Deviation 12 |
|
| ||||||
| < 10% | 3 | 12 | 9 | 36 | ||
| 11-20% | 4 | 16 | 4 | 16 | ||
| 21% or > | 2 | 8 | 3 | 12 | ||
|
| ||||||
| % Full Thickness | Mean 4 | Median 0 | St. Deviation 10 | Mean 7 | Median 2 | St. Deviation 11 |
|
| ||||||
| < 10% | 8 | 89 | 12 | 75 | ||
| 11-20% | 0 | 0 | 2 | 13 | ||
| 21% or > | 1 | 11 | 2 | 12 | ||
|
| ||||||
| % Partial Thickness | Mean 12 | Median 11 | St. Deviation 8 | Mean 6 | Median 5 | St. Deviation 5 |
|
| ||||||
| < 10% | 3 | 33 | 13 | 81 | ||
| 11-21% | 5 | 56 | 3 | 19 | ||
| 21% or > | 1 | 11 | 0 | 0 | ||
|
| ||||||
| Inhalation Injury | n | % | n | % | ||
|
| ||||||
| Yes | 0 | 0 | 15 | 60 | ||
| No | 9 | 36 | 1 | 4 | ||
|
| ||||||
| Cause of Burn | ||||||
|
| ||||||
| Thermal | 9 | 36 | 15 | 60 | ||
| Electrical | 0 | 0 | 1 | 4 | ||
Figure 3.
Clinical Characteristics of Participants - %TBSA*, *%TBSA = Percent Total Body Surface Area.
Figure 4.
Clinical Characteristics of Participants - %FT*, *%FT = Percent Full Thickness.
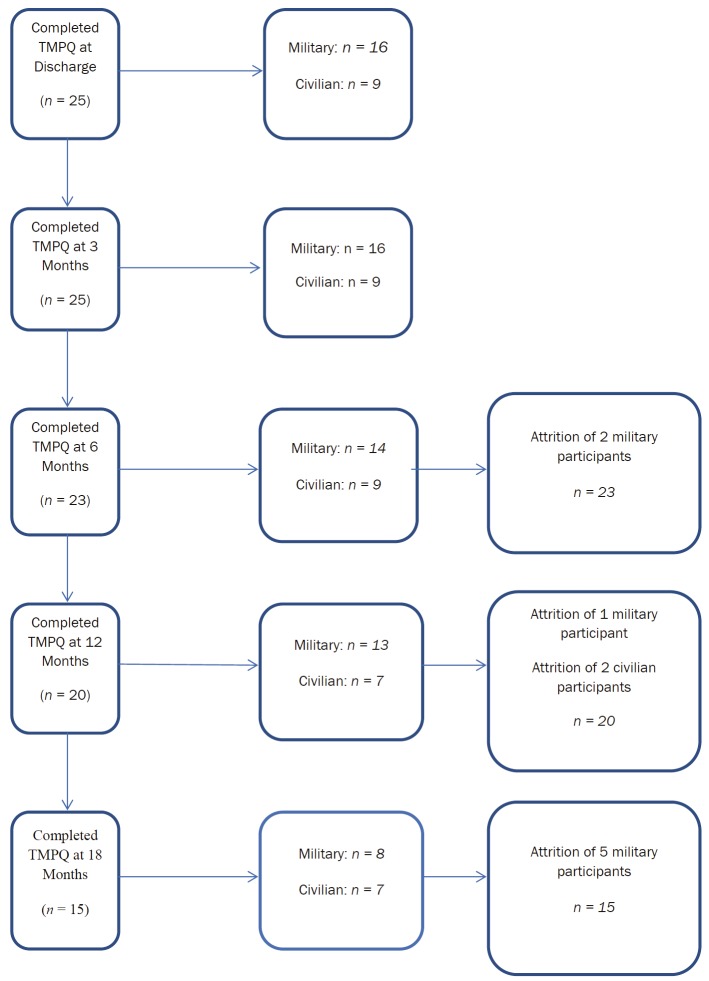
Upon discharge from the USAISR, patients moved to a variety of locations throughout the United States. Figure 5 depicts the geographic locations of the 25 participants throughout the study. Two service members were deployed back to military theaters of conflict during capitalize Operation Iraqi Freedom. Although all participants in the videophone study completed the instruments in the larger burn QOL study at all data collection points, they did not all complete every time point of the telemedicine portion (Figure 6). Six military service members were reassigned to new duty stations; three of them were reassigned to locations close to the burn center, and therefore, they no longer wanted to use the videophone. They completed their instruments in person with a study team member. Two civilian and three military participants decided to not obtain or continue using a telephone land line, they went completely cellular in their telephonic communications. Because the videophone required a land line hook-up it could not be used after the participants discontinued land line services. All videophones were returned to the study team by the participants after completion of data collection.
Figure 5.
Geographic Location of Participants.
Figure 6.
TMPQ Completion by Participants.
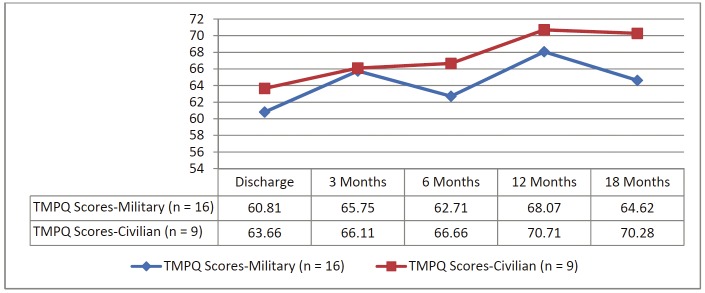
The Telemedicine Perception Questionnaire (TMPQ) scores and perception of videophone use
Participants’ mean TMPQ scores at the time of burn center discharge were relatively high at 61.84 for the aggregate. Over the course of the study, the TMPQ scores showed only slight variability, ranging from the lowest at discharge to the highest at 18-months as depicted in Figure 7. In general, the military participants rated use of the telemedicine technology slightly lower than the civilian participants. The TMPQ performed well in this study with a Cronbach’s alpha of .84.
Figure 7.
TMPQ Scores: Discharge to 18-months.
Overall, qualitative comments from participants and members of the research team collecting the data were highly positive. Qualitative comments from participants supported the high scores on the TMPQ. For example, one participant said “it would have been impossible to do this with a regular phone and be able to describe the skin; the videophone made it work by allowing me to show my skin.” Another participant commented that “communication was enhanced with the videophone because it’s nicer seeing the person you are speaking to. “Several participants emphasized that use of the video phone prevented the necessity of travel to the military burn center regarding compression garment and wound healing issues. These problems were addressed by using the videophone for discussion between the patient and their physician after the research data collection was complete. Additionally, 60% of the participants said they remained in the study because they were allowed to use the videophone rather than only using the telephone or a mailed survey.
Negative comments from participants focused primarily on issues concerning “dropped” calls and loss of video due to band-width issues. After each of the 88 completed videophone visits, the patients were asked about their overall satisfaction with the use of the videophone. In 92% of the cases the participants were very satisfied or satisfied and in 7% of the visits they were very unsatisfied or unsatisfied. In only one case (1%) did a participant indicate there was no difference between a videophone visit versus a regular telephone visit.
When the two research team members conducting the videophone visits were asked about their satisfaction using the technology to collect QOL research data, they stated they were very satisfied 90% of the time. During 6 calls (7%) they were either very unsatisfied or unsatisfied and in only 3 cases (3%) did they believe there was no difference between the videophone visits as compared to telephone visits.
Discussion
This was the first study to examine the use of the videophone to collect QOL data from burn patients after discharge from an American Burn Association verified burn center. Previous studies using telemedicine technology focused on remote burn consultations to provide easier access to burn specialty care and decrease costs [9,25]. Although it was a feasibility study consisting of a small sample, the results clearly demonstrated that use of the videophone for data collection was viewed in a positive manner, because the study participants liked being able to see the research team member asking the questions. This is consistent with findings from two other studies using telemedicine with burn patients, where a high degree of satisfaction from patients and the provider team was demonstrated [9,25]. However, privacy and confidentiality concerns must be kept in mind when using videophone technology. If the patient has physical limitations that require assistance from a family member or significant other to use the technology, they may be reticent to answer sensitive questions, such as those concerning mental health symptoms or sexuality.
Unexpected benefits to patients included the ability to discuss problems with their provider team without having to make long-distance trips to the burn center. Members of the provider team were able to “see” the problem with a wound or a compression garment and solve the problem quickly without inconvenience to the participant. Although it was not a goal to assess the cost of using the videophone technology, it was clear that for at least three participants the technology saved the cost of travel expenditures and lost time from work that more than compensated for the cost of the videophone. Such anecdotal findings are consistent with other studies that clearly demonstrated cost savings when using telemedicine with burn patients [9,25].
Study findings also supported the use of the TMPQ to assess burn patient satisfaction with the use of telehealth technology. The instrument’s internal consistency in this study (α =.84) was similar to that reported by the instrument developers (α=.80) [21]. No single instrument has been used consistently to assess patient satisfaction with telehealth technology and this holds true for burn patients. Therefore, it is recommended that the TMPQ be used in future studies to assess patient satisfaction with telehealth technologies. Moreover, the instrument should be further evaluated for validity and internal consistency among a variety of patient populations.
With the rapid advance of technology, the videophone may now be obsolete technology for the collection of research data or post-discharge burn care consultations. However, laptop computers with high resolution detachable webcams could be purchased to produce results similar to those of the videophone at lower cost. Because burn centers are limited and not all patients can easily return to the centers that provided their treatment, use of such technology is clearly effective for clinical consultations and collection of research data. Additionally, use of a secure patient portal could negate the need for a telephone land line and reduce costs to patients and burn centers while also maximizing the collection of vitally important QOL data.
Acknowledgements
This research was supported by a Triservice Nursing Research Program grant # N99-025 and a Telemedicine and Advanced Technology Research Center (TATRC) Cooperative Research and Development Agreement # DAMD17-03-P-1045. The authors gratefully acknowledge the contributions of the late Michael Yates, MAJ (Ret.), MSN, RN, to the performance of this study.
Disclaimer
This research was sponsored by the TriService Nursing Research Program, Uniformed Services University of the Health Sciences; however, the information or content and conclusions do not necessarily represent the official position or policy of, nor should any official endorsement be inferred by, the TriService Nursing Research Program, the Uniformed Services University of the Health Sciences, the Department of Defense, or the U.S. Government.
This study was conducted under a protocol reviewed and approved by the US Army Medical Research and Materiel Command Institutional Review Board and in accordance with the approved protocol.
References
- 1.Perednia DA, Allen A. Telemedicine technology and clinical applications. Journal of the American Medical Association. 1995 Feb 8;273:483–488. [PubMed] [Google Scholar]
- 2.Doarn CR, McVeigh F, Poropatich R. Innovative new technologies to identify and treat traumatic brain injuries: Crossover technologies and approaches between military and civilian applications. Telemedicine and e-Health. 2010;16:373–381. doi: 10.1089/tmj.2010.0009. [DOI] [PubMed] [Google Scholar]
- 3.Smith AC, Kimble R, Mill J, Bailey D, O’Rourke P, Wootton R. Diagnostic accuracy of and patient satisfaction with telemedicine for the follow-up of paediatric burns patients. Journal of Telemedicine and Telecare. 2004;10:193–198. doi: 10.1258/1357633041424449. [DOI] [PubMed] [Google Scholar]
- 4.Pedersen S, Holand U. Tele-endoscopic otorhinolaryngological examination: Preliminary study of patient satisfaction. Telemedicine Journal. 1995 Spring;1:47–52. doi: 10.1089/tmj.1.1995.1.47. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan EH. Telepsychotherapy: Psychotherapy by telephone, videophone, and computer videoconferencing. The Journal of Psychotherapy Practice and Research. 1997;6:227–237. [PMC free article] [PubMed] [Google Scholar]
- 6.García-Lizana F, Muñoz-Mayorga I. Telemedicine for depression: A systematic review. Perspectives in Psychiatric Care. 2010;46:119–126. doi: 10.1111/j.1744-6163.2010.00247.x. [DOI] [PubMed] [Google Scholar]
- 7.Arnaert A, Delesie D. Effectiveness of videotelephone nursing care for the homebound elderly. Canadian Journal of Nursing Research. 2007;39:20–36. [PubMed] [Google Scholar]
- 8.Buckley KM, Tran BQ, Prandoni CM. Receptiveness, use and acceptance of telehealth by caregivers of stroke patients in the home. Online Journal of Issues in Nursing. 2004;9:9. [PubMed] [Google Scholar]
- 9.Redlick F, Roston B, Gomez M, Fish JS. An initial experience with telemedicine in follow-up burn care. Journal of Burn Care & Rehabilitation. 2002;23:110–115. doi: 10.1097/00004630-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Wade VA, Karnon J, Elshaug AG, Hiller JE. A systematic review of economic analyses of teleheatlh services using real time video communication. Creative Commons Attribution. 2010 doi: 10.1186/1472-6963-10-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turk E, Karagulle E, Aydogan C, Oguz H, Tarim A, Karakayali H, Haberal M. Use of telemedicine and telephone consultation in decision-making and follow-up of burn patiets: Initial experience from two burn units. Burns. 2011;27:415–419. doi: 10.1016/j.burns.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Cox K, Mahone I, Merwin E. Improving the quality of rural nursing care. In: Kasper CE, editor. Annual Review of Nursing Research. New York, NY: Springer Publishing; 2008. pp. 175–194. [PubMed] [Google Scholar]
- 13.Brewer R, Goble G, Guy P. A peach of a telehealth program: Georgia connects rural communities to better heatlhcare. Perspectives in Health Information Management. 2010:1–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Allen A, Hayes J. Patient satisfaction with tele-oncology: A pilot study. Telemedicine Journal Spring. 1995;1:41–46. doi: 10.1089/tmj.1.1995.1.41. [DOI] [PubMed] [Google Scholar]
- 15.Turecek D. Telemedicine. Wisconsin Medical Journal. 1996 Jun;95:388–389. [PubMed] [Google Scholar]
- 16.Whitten P, Mair F, Collins B. Home telenursing in Kansas: Patients’ perceptions of uses and benefits. Journal of Telemedicine and Telecare. 1997;3(Suppl 1):67–69. doi: 10.1258/1357633971930436. [DOI] [PubMed] [Google Scholar]
- 17.Dansky KH, Bowles KH, Palmer L. How telehomecare affects patients. Caring. 1999;18:10–14. [PubMed] [Google Scholar]
- 18.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ Journal. 2000;320:1517–1520. doi: 10.1136/bmj.320.7248.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Demiris G, Oliver DP, Courtney K. A study of the suitability of videophones for psychometric assessment. Behaviour & Information Technology. 2006;25:233–237. [Google Scholar]
- 20.Tausig JE, Freeman EW. The next best thing to being there: Conducting the clinicla research interview by telephone. American Journal Orthopsychiatric. 1988;58:418–427. doi: 10.1111/j.1939-0025.1988.tb01602.x. [DOI] [PubMed] [Google Scholar]
- 21.Demiris G, Speedie S, Finkelstein S. A questionnaire for the assessment of patients’ impressions of the risks and benefits of home telecare. Journal of Telemedicine & Telecare. 2000;6:278–284. doi: 10.1258/1357633001935914. [DOI] [PubMed] [Google Scholar]
- 22.Demiris G, Speedie SM, Finkelstein S. Change of patients’ perceptions of TeleHomeCare. Telemedine and e-Health Fall. 2001;7:241–248. doi: 10.1089/153056201316970948. [DOI] [PubMed] [Google Scholar]
- 23.Wakefield BJ, Bylund CL, Holman JE, Ray A, Scherubel M, Kienzle MG, Rosenthal GE. Nurse and patient communication profiles in a home-based telehealth intervention for heart failure management. Patient Education and Counseling. 2008;71:285–292. doi: 10.1016/j.pec.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 24.Eminovic N, Wyatt JC, Tarpey AM, Murray G, Ingrams GJ. First evaluation of the NHS Direct Online Clinical Enquiry Service: A nurse-led web chat triage service for the public. Journal of Medical Internet Research. 2004;6:e17. doi: 10.2196/jmir.6.2.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saffle JR, Edelman L, Theurer L, Morris S, Cochran A. Telemedicine evaluation of acute burns is accurate and cost-effective. The Journal of Trauma, Injury, Infection, and Critical Care. 2009;67:358–365. doi: 10.1097/TA.0b013e3181ae9b02. [DOI] [PubMed] [Google Scholar]