Abstract
BACKGROUND:
Coblation tonsillectomy is a new surgical technique and demands further research to be proven as a suitable and standard method of tonsillectomy. This study compares coblation and traditional tonsillectomy techniques in view of their advantages and complications.
METHODS:
In a prospective double-blind randomized controlled trial information on operation time, intraoperative blood loss, postoperative pain, time needed to regain the normal diet and activity and postoperative hemorrhage were gathered and compared between two groups containing 47 patients in each group.
RESULTS:
We found statistically significant differences in operation time (p < 0.05), intraoperative blood loss (p < 0.05), postoperative pain (p < 0.001), time needed to find back the normal diet (p < 0.001) and normal activity (p < 0.001). However, post operation hemorrhage (p > 0.5) was not significantly different between two groups.
CONCLUSIONS:
This study revealed a significantly less intraoperative or postoperative complications and morbidity in coblation tonsillectomy in comparison with traditional method. Coblation was associated with less pain and quick return to normal diet and daily activity. These findings addressed coblation tonsillectomy as an advanced method.
KEYWORDS: Coblation, Tonsillectomy, Complications
Tonsillectomy is the most routinely performed surgical operation in the recent years.1 There have been lots of controversies about tonsillectomy techniques to provide better conditions with more benefits and less complications.
For more than a century, traditional dissection tonsillectomy has remained the gold standard for tonsil removal.2 Traditional tonsillectomy leaves the wound open to heal by secondary intention, thus causes pain and bleeding as two major postoperative complications. This is the reason pioneers usually concentrate to decrease these two problems with comparing various techniques.3 Long periods of wound recoveries, taking up to fifteen days, are not so uncommon. This may bear the risk of bleeding from tonsillar bed.4,5 Postoperative pain can cause severe limitation in regaining the activities and diet. Considering the mentioned morbidities, attempts have been made to improve the outcome by developing new techniques with less postoperative pain and short recovery period. Available techniques include cold-knife dissection, guillotine excision, electrocautery, cryosurgery, the harmonic scalpel, laser tonsillectomy, bipolar diathermy dissection, radiofrequency and coblation methods.6–9
Coblation tonsillectomy was initially introduced in 200110 following which a great amount of articles have been published either to confirm its efficacy11,4 or to reject that because of unsatisfactory or unproven outcomes with undesirable cost-effectiveness.12,13 However, more studies are still required to reveal a clear conclusion.14,15 Even though some former studies showed a reduced postsurgical pain4,10 and no significant morbidities like postoperative hemorrhage, they have not been considered due to their small sample size. Quick return to normal diet was also reported.10 A study observed healing process of the tonsillar bed in 10 patients and concluded that coblation method would be more preferable than bipolar dissection.4 A recent study defended use of coblation surgery because of decreased bleeding and pain, but cases in the study were only 14 patients.16 Another study in the UK found no benefits for coblation method comparing with conventional tonsillectomy, indicating that traditional tonsillectomy is superior to coblation method.17 The NICE guidelines have suggested that coblation is probably associated with decreased postoperative pain comparing with bipolar diathermy; however, the outcomes may be different for that of the monopolar diathermy or cold dissection.18 Our study aimed to compare coblation and traditional tonsillectomy, regarding the postoperative morbidities and time required to regain the normal diet and activity with larger number of cases.
Methods
In a prospective double-blind randomized controlled trial, we tried to find out whether coblation technique decreases the postoperative morbidity compared to traditional dissection tonsillectomy. Operation time, intraoperative blood loss, postoperative pain, number of days needed to return to work and normal diet and postoperative hemorrhage were compared between two groups.
The study design was approved by the local ethics committee of Sadi Hospital in Isfahan. 94 candidates for tonsillectomy were recruited between June 2007 and December 2008, 47 of which in control (traditional tonsillectomy) group and 47 in intervention (coblation) group (Figure 1). Informed and consent was obtained from each subjects allowing randomization, using random number table, prior to surgery.
Figure 1.
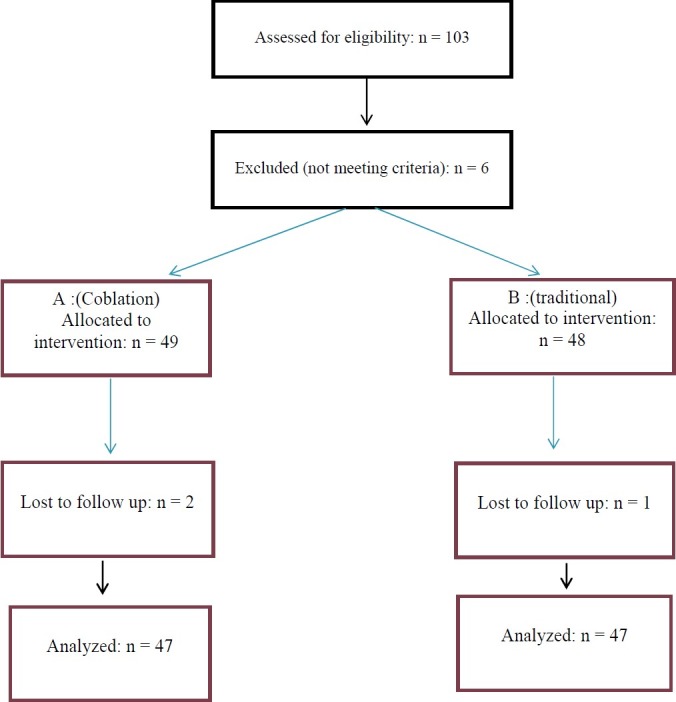
Participants retention vs. attrition
Indications for tonsillectomy in our study were chronic recurrent tonsillitis (without any history of tonsillitis within 4 weeks prior to surgery) and snoring with sleep apnea. Patients with a history of a peritonsillar abscess, ongoing analgesic use for medical conditions and bleeding disorders were excluded. No antibiotics, topical or local anesthesia, or other medications were administered before surgery. The anesthetic approach was the same for all patients as follows: induction was performed using intravenous fentanyl, propofol 2 mg/kg, and atracurium 0.5 mg/kg following intubation. Maintenance of anesthesia was achieved by a mixture of nitrous oxide, oxygen, and propofol. Fentanyl boluses of 25 mcg were given when blood pressure and heart rate increased by 20% or more during surgery, following reversal and in recovery status. After beginning of anesthesia, the patient was allocated in each group by surgeon based on a randomly generated number sequence.
The operation was performed in the standard way using either the ArthroCare 2 assisted Evac-70 coblator wand or steel cold dissection instruments. The coblation device was made by ArthroCare Company, Sunnyvale, CA, USA. All procedures were done by first author to lower any probable skill related bias. Our surgeon had performed more than a hundred coblation assisted tonsillectomies prior to trial to eliminate a learning curve related disturbance. Postoperative analgesic was only acetaminophen in suppository, tablet or elixir form. Operation time, from insertion till removal of Crow-Davis blade, was recorded for each case. Operation scrub evaluated and recorded intraoperative blood loss by checking volume of blood in suction bottle after the operation. Postoperative cares were the same in both groups.
Data including age, volume of blood loss, operation time, postoperative pain score, postoperative hemorrhage, days needed to return to work and normal diet were gathered in both groups. Patients were examined for the following postoperative complications during post surgical visits: primary hemorrhage, secondary hemorrhage, and readmission due to postoperative pain. On discharge, the patients were advised to call the medical group for any complications especially bleeding. Follow up of all patients was performed by a second colleague to make the surgeon blind. On the other hand, none of patients were aware of type of procedure.
The primary hemorrhage was defined as bleeding occurring within 24 hours after surgery and secondary hemorrhage as bleeding after 24 hours postoperatively. Each of patients completed a questionnaire concerning the time to return to normal activity. Visual analog scale was used for the pain severity, ranging from 0 to 10. Zero indicated no pain and 10 revealed an extreme pain.
Data were entered into a database and analyzed using SPSS software (SPSS, Windows, version 16). Chi-squared tests were used to compare graded scores for pain. Data of day of return to work and normal diet were analyzed using student's t-test.
Results
There was no significant difference between the mean age of two groups (p > 0.05), being 11.2 years in coblation and 11.8 years in traditional group. Intraoperative blood loss turned out to be 103.4 ± 28.7 ml for the coblation and 161.5 ± 46.4 for the traditional group (p < 0.001). Mean operation time was 27.3 ± 4.8 minutes (ranging from 18 to 42) in coblation group and 31.0 ± 5.4 minutes (ranging from 20 to 45 minutes) in traditional group. The mean operation time was thus significantly less for coblation group (p < 0.001).
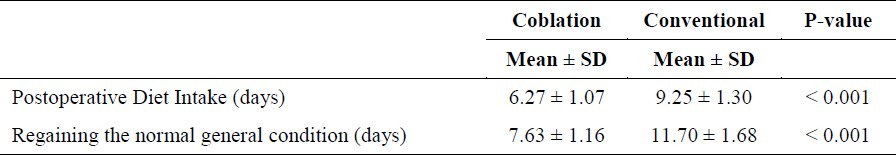
Postoperative pain scores were evaluated for both groups and compared using chi-square test. A lower postoperative pain score in coblation group was statistically significant (p < 0.000). Mean return to normal diet of both groups are summarized in table 1. Diet recovery period was significantly shorter in the coblation group (6.2 vs. 9.2 days p < 0.001). Otherwise, return to normal general condition was significantly earlier in the coblation group (7.6 vs. 11.0 days p < 0.001).
Table 1.
Postoperative diet intake and regaining the normal general condition of patients
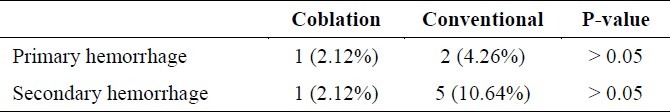
Furthermore, it was revealed that postoperative primary and secondary hemorrhage rate was slightly higher in traditional group. However, there was no statistically significant difference (p > 0.05) (Table 2). During follow up period, no other major or minor complications occurred in our study.
Table 2.
Postoperative hemorrhage in patients
Discussion
In this study we compared two techniques of tonsillectomy, the coblation and traditional. Some significant differences were shown between outcomes of these two methods. Tonsillectomy is one of the most common operations performed in otolaryngology worldwide.19,20 Tonsillectomy with steel forceps (as traditional) consumes longer time than coblation tonsillectomy does as a slower dissection.21
Coblation (cold ablation) is a newly introduced technique of surgery. The use of this new technique has received remarkable research attention.22 Results in small study groups have been encouraging; however, they have requested for evaluation with larger numbers and evidences from other centers.18–23 One large-scale trial performed to date, found a 1% hemorrhagerate24 using the coblation technique. In our study, we found 4.3 % which is rather close to mentioned trial. Coblation assisted tonsillectomy can result in less blood loss and tissue damage, which may minimize the postoperative recovery period and earlier return to normal activity.
First studies on coblation tonsillectomy have shown a significant decrease in postoperative pain scores comparing with traditional method with no more complications4,10 that is compatible with our results. These promising results based up different studies revealed similar outcomes when comparing coblation and electrosurgery or ultrasonic tonsillectomy.25,26 On the other hand, there are some studies which reported no significant reductions in pain with coblation surgery comparing with cold dissection or electrosurgery.17,15
Noon, et al. demonstrated a significantly higher hemorrhage rate in the coblation group comparing with diathermy (22.2% versus 3.4%) from a study arranged for 64 patients.13 Our data opposed this study as we found only 4.3% hemorrhage rate. Our study showed significant difference in post-operative morbidities in favor of coblation assisted method.
Need for analgesics, perhaps due to a significantly longer operating time, was significantly higher in the control group. The pain on the day of the operation was significantly different between groups. Removal of the tonsils and achievement of good homeostasis was more difficult in traditional group. A statistically significant difference was found in postoperative hemorrhage rate in favor of coblation. The incidence of postoperative hemorrhage matched favorably with the published rates of 0-20 percent for other series,27–30 which confirmed our findings. We found that the postoperative hemorrhage including primary and secondary hemorrhages was generally more frequent in the control group; the difference was not statistically significant though.
In order to evaluate the return to normal activities, the patients were asked the postoperative day they would be able to return to work. Another factor which assessed the clinical recovery was retrieving normal diet. The results were significantly different. In our study, the intraoperative blood loss and operation time were significantly less in the coblation group. The reduction of intraoperative blood loss and operation time in coblation tonsillectomy was obvious and reduction of the postoperative pain and early return to normal diet and activities without increasing the postoperative complications were clinically and statistically significant. Therefore, we believe that the coblation tonsillectomy is an effective and cost-effective method.
Conclusion
We consider coblation tonsillectomy to be a safe and effective alternative to traditional tonsillectomy. Our study showed a significant difference in postoperative morbidity and complications between patients undergoing coblation tonsillectomy and those undergoing traditional technique. Coblation tonsillectomy significantly reduced the operation time, intraoperative blood loss and postoperative pain, and was associated with early recovery of dietary routine. We recommend this instrument as a suitable alternative method of tonsillectomy.
Authors’ Contributions
MO Design, case gathering, operational surgeon. BB Supervision and drafting, operational surgeon. NO Litrature review, data Gathering, analysis, design consultantation. ARO Technical consultation. SAGH Coworker.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Lowe D, van der Meulen J, Cromwell D, Lewsey J, Copley L, Browne J, et al. Key messages from the National Prospective Tonsillectomy Audit. Laryngoscope. 2007;117(4):717–24. doi: 10.1097/mlg.0b013e318031f0b0. [DOI] [PubMed] [Google Scholar]
- 2.Pinder DK, Wilson H, Hilton MP. Dissection versus diathermy for tonsillectomy. Cochrane Database Syst Rev. 2011;(3):CD002211. doi: 10.1002/14651858.CD002211.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raut V, Bhat N, Kinsella J, Toner JG, Sinnathuray AR, Stevenson M. Bipolar scissors versus cold dissection tonsillectomy: a prospective, randomized, multi-unit study. Laryngoscope. 2001;111(12):2178–82. doi: 10.1097/00005537-200112000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Timms MS, Temple RH. Coblation tonsillectomy: a double blind randomized controlled study. J Laryngol Otol. 2002;116(6):450–2. doi: 10.1258/0022215021911031. [DOI] [PubMed] [Google Scholar]
- 5.Tan AK, Hsu PP, Eng SP, Ng YH, Lu PK, Tan SM, et al. Coblation vs electrocautery tonsillectomy: postoperative recovery in adults. Otolaryngol Head Neck Surg. 2006;135(5):699–703. doi: 10.1016/j.otohns.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Wiatrak BJ, Willging JP. Harmonic scalpel for tonsillectomy. Laryngoscope. 2002;112(8 Pt 2 Suppl 100):14–6. doi: 10.1002/lary.5541121406. [DOI] [PubMed] [Google Scholar]
- 7.Derkay CS, Maddern BR. Innovative techniques for adenotonsillar surgery in children: introduction and commentary. Laryngoscope. 2002;112(8 Pt 2 Suppl 100):2. doi: 10.1002/lary.5541121401. [DOI] [PubMed] [Google Scholar]
- 8.Plant RL. Radiofrequency treatment of tonsillar hypertrophy. Laryngoscope. 2002;112(8 Pt 2 Suppl 100):20–2. doi: 10.1002/lary.5541121408. [DOI] [PubMed] [Google Scholar]
- 9.Lee KC, Bent JP, III, Dolitsky JN, Hinchcliffe AM, Mansfield EL, White AK, et al. Surgical advances in tonsillectomy: report of a roundtable discussion. Ear Nose Throat. 2004;83(8)(Suppl 3):4–13. [PubMed] [Google Scholar]
- 10.Temple RH, Timms MS. Paediatric coblation tonsillectomy. Int J Pediatr Otorhinolaryngol. 2001;61(3):195–8. doi: 10.1016/s0165-5876(01)00553-5. [DOI] [PubMed] [Google Scholar]
- 11.Polites N, Joniau S, Wabnitz D, Fassina R, Smythe C, Varley P, et al. Postoperative pain following coblation tonsillectomy: randomized clinical trial. ANZ J Surg. 2006;76(4):226–9. doi: 10.1111/j.1445-2197.2006.03700.x. [DOI] [PubMed] [Google Scholar]
- 12.Burton MJ, Doree C. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev. 2007;(3):CD004619. doi: 10.1002/14651858.CD004619.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Noon AP, Hargreaves S. Increased postoperative haemorrhage seen in adult coblation tonsillectomy. J Laryngol Otol. 2003;117(9):704–6. doi: 10.1258/002221503322334521. [DOI] [PubMed] [Google Scholar]
- 14.Back L, Paloheimo M, Ylikoski J. Traditional tonsillectomy compared with bipolar radiofrequency thermal ablation tonsillectomy in adults: a pilot study. Arch Otolaryngol Head Neck Surg. 2001;127(9):1106–12. doi: 10.1001/archotol.127.9.1106. [DOI] [PubMed] [Google Scholar]
- 15.Shah UK, Galinkin J, Chiavacci R, Briggs M. Tonsillectomy by means of plasma-mediated ablation: prospective, randomized, blinded comparison with monopolar electrosurgery. Arch Otolaryngol Head Neck Surg. 2002;128(6):672–6. doi: 10.1001/archotol.128.6.672. [DOI] [PubMed] [Google Scholar]
- 16.Arya A, Donne AJ, Nigam A. Double-blind randomized controlled study of coblation tonsillotomy versus coblation tonsillectomy on postoperative pain. Clin Otolaryngol Allied Sci. 2003;28(6):503–6. doi: 10.1046/j.1365-2273.2003.00750.x. [DOI] [PubMed] [Google Scholar]
- 17.Philpott CM, Wild DC, Mehta D, Daniel M, Banerjee AR. A double-blinded randomized controlled trial of coblation versus conventional dissection tonsillectomy on postoperative symptoms. Clin Otolaryngol. 2005;30(2):143–8. doi: 10.1111/j.1365-2273.2004.00953.x. [DOI] [PubMed] [Google Scholar]
- 18.Interventional Procedure Overview of Coblation Tonsillectomy. London: Anonymous; 2002. National Institute For Clinical Excellence. [Google Scholar]
- 19.Leach J, Manning S, Schaefer S. Comparison of two methods of tonsillectomy. Laryngoscope. 1993;103(6):619–22. doi: 10.1288/00005537-199306000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Mann DG, St GC, Scheiner E, Granoff D, Imber P, Mlynarczyk FA. Tonsillectomy--some like it hot. Laryngoscope. 1984;94(5 Pt 1):677–9. [PubMed] [Google Scholar]
- 21.Pizzuto MP, Brodsky L, Duffy L, Gendler J, Nauenberg E. A comparison of microbipolar cautery dissection to hot knife and cold knife cautery tonsillectomy. Int J Pediatr Otorhinolaryngol. 2000;52(3):239–46. doi: 10.1016/s0165-5876(00)00293-7. [DOI] [PubMed] [Google Scholar]
- 22.Powell NB, Riley RW, Troell RJ, Blumen MB, Guilleminault C. Radiofrequency volumetric reduction of the tongue. A porcine pilot study for the treatment of obstructive sleep apnea syndrome. Chest. 1997;111(5):1348–55. doi: 10.1378/chest.111.5.1348. [DOI] [PubMed] [Google Scholar]
- 23.Burton MJ, Towler B, Glasziou P. Tonsillectomy versus non-surgical treatment for chronic / recurrent acute tonsillitis. Cochrane Database Syst Rev. 2000;(2):CD001802. doi: 10.1002/14651858.CD001802. [DOI] [PubMed] [Google Scholar]
- 24.Lee KC, Altenau MM, Barnes DR, Bernstein JM, Bikhazi NB, Brettscheider FA, et al. Incidence of complications for subtotal ionized field ablation of the tonsils. Otolaryngol Head Neck Surg. 2002;127(6):531–8. doi: 10.1067/mhn.2002.129736. [DOI] [PubMed] [Google Scholar]
- 25.Stoker KE, Don DM, Kang DR, Haupert MS, Magit A, Madgy DN. Pediatric total tonsillectomy using coblation compared to conventional electrosurgery: a prospective, controlled single-blind study. Otolaryngol Head Neck Surg. 2004;130(6):666–75. doi: 10.1016/j.otohns.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 26.Parsons SP, Cordes SR, Comer B. Comparison of posttonsillectomy pain using the ultrasonic scalpel, coblator, and electrocautery. Otolaryngol Head Neck Surg. 2006;134(1):106–13. doi: 10.1016/j.otohns.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 27.Siodlak MZ, Gleeson MJ, Wengraf CL. Post-tonsillectomy secondary haemorrhage. Ann R Coll Surg Engl. 1985;67(3):167–8. [PMC free article] [PubMed] [Google Scholar]
- 28.Tami TA, Parker GS, Taylor RE. Post-tonsillectomy bleeding: an evaluation of risk factors. Laryngoscope. 1987;97(11):1307–11. doi: 10.1288/00005537-198711000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Capper JW, Randall C. Post-operative haemorrhage in tonsillectomy and adenoidectomy in children. J Laryngol Otol. 1984;98(4):363–5. doi: 10.1017/s0022215100146742. [DOI] [PubMed] [Google Scholar]
- 30.Carmody D, Vamadevan T, Cooper SM. Post tonsillectomy haemorrhage. J Laryngol Otol. 1982;96(7):635–8. doi: 10.1017/s0022215100092926. [DOI] [PubMed] [Google Scholar]


