Abstract
INTRODUCTION:
Cystic lesions of the adrenals are rare with an incidence of 0.06% in autopsies, and the most frequently found are either the endothelial cysts or the pseudocysts. We report our series of patients presenting with adrenal cysts.
MATERIALS AND METHODS:
The case records of patients presenting with adrenal cysts were reviewed and analyzed. Age, gender, presenting symptoms, physical examination findings, laboratory investigations and imaging records were all noted and analysed.
RESULTS:
During the 10-year study period, 14 patients, with a mean age of 41.36 ± 5.57 years, were diagnosed to have adrenal cysts. Laparoscopic excision of cysts was performed in three and laparoscopic adrenalectomy in the remaining eleven.
CONCLUSIONS:
Adrenal cysts are rare, and intervention is indicated whenever they are large (>5 cm), symptomatic, functional, and potentially malignant. Laparoscopic management of these cysts in the form of either decortication/excision is safe, effective, minimally invasive, with minimal blood loss and shorter duration of hospitalization.
Keywords: Adrenal cyst, adrenalectomy, laparoscopy
INTRODUCTION
Adrenal cysts are usually unilateral lesions discovered incidentally during imaging procedures or surgery and at autopsy. Endothelial or lymphangiomatous cysts account for nearly 45% of these lesions and are usually small, measuring 0.1 to 1.5 cm in diameter. Adrenal pseudocysts that lack an epithelial lining are the next most common variety (39%) and most likely represent encapsulated residual of previous adrenal haemorrhages. Pseudocysts may become massive and may cause symptoms because of the compression of adjacent structures. The acute haemorrhage is readily distinguished by magnetic resonance imaging (MRI). Traumatic rupture of adrenal cysts has also been reported.[1] Calcifications may be found in approximately 15% of cases and need not imply malignancy. Parasitic cysts due to echinococcal disease (7%) and true epithelial cysts (9%) account for the remainder of adrenal cysts.[2,3] Most cystic adrenal lesions are found incidentally and can be observed; symptomatic cysts can be percutaneously drained or laparoscopically decorticated.[4] We report our series of patients presenting with adrenal cysts.
MATERIALS AND METHODS
We retrospectively reviewed the case records of patients presenting with adrenal lesions and managed at our centre during the period April 2000 to December 2010. Age, gender, presenting symptoms, physical examination findings, laboratory investigations and imaging records were all noted and analysed. Operative findings, postoperative outcome and histopathological reports were all similarly noted.
RESULTS
During the 10-year study period, 14 patients, with a mean age of 41.36 ± 5.57 years, were diagnosed to have adrenal cysts. Eleven of them were females and the remaining three males. Twelve of these patients presented with pain in abdomen. In two patients, the pain was acute and associated with vomiting and fever. In these two patients, a vague abdominal mass was felt. In the remaining 10, the pain was mild, and positional. At times the pain was more of discomfort. Two women were evaluated for vague abdominal discomfort and both had high blood pressure. Ultrasound imaging picked up the adrenal cysts in all. The mean size was 9.57 ± 1.55 cm. The contents of these cystic masses were clear in 12 of these patients. The cyst wall was thin and well demarcate. Computerized tomography (CT) was done in all to determine the nature of the cyst and its relation to the surrounding structures. MRI was done in two patients who had demonstrated unclear contents on ultrasonography. MRI signals were diagnostic of haemorrhage. Three of the patients were diabetic on medication. None of the patients showed any elevation of urinary VMA levels.
Operative intervention was done in all. Transperitoneal laparoscopic excision of cysts was done in three and laparoscopic adrenalectomy in the remaining eleven. The mean operating time was 76.43 ± 11.05 min, and the mean blood loss was 27.43 ± 3.98 cm3. The mean postoperative hospital stay was 3.07 ± 0.73 days. No major intra- or post-operative complications were noted in any of the patients. Nine of these cysts were endothelial cysts, whereas the remaining five were adrenal pseudocysts.
DISCUSSION
Cysts of the adrenal gland are rare, but today, with the wider application of sonography and computed tomography more and more adrenal cysts are being detected incidentally. The reported incidence in clinical series is of 5.4%.[5] In the autopsy series, they count less than 0.064-0.18%.[6] Adrenal cysts are usually asymptomatic, and most of them are diagnosed incidentally during ultrasound or CT examination. Some of these patients present with acute abdominal pain and can rarely mimic an acute abdomen whenever bleeding occurs into the cyst. Very rarely they can present as a huge abdominal mass causing discomfort.[7] There are also a small number of cases in the literature in which the adrenal cysts were hormonally active (Cushing's syndrome, Pheochromocytoma).[5] Most commonly these cysts either present or are diagnosed in the fourth/fifth decade of life.[8] El-Hefnawy et al.[8] reported of an adrenal cyst being diagnosed in a female infant of 1 month and a 1-year-old male child. Iuchtman et al.[9] reported a case of an antenatally diagnosed cystic abdominal mass in a fetus, which on exploration after birth turned out to be an adrenal cyst [Figures 1 and 2].
Figure 1.

Coronal section CT abdomen showing huge left adrenal cyst pushing left kidney inferiorly
Figure 2.
Axial section CD abdomen showing a huge left-sided adrenal cyst with well defined
The rubric of adrenal cysts comprises a broad differential diagnosis, rendering definitive diagnosis and subsequent management difficult. These cysts are categorized into four subtypes: endothelial, pseudocyst, epithelial, and parasitic. Endocrine workup should rule out the functional status. Radiologic differentiation is helpful; however, imaging characteristics, such as haemorrhage in a pseudocyst, can confound identification of benign versus malignant lesions. Any functional lesion, potentially malignant lesion, or benign lesion more than 5 cm in diameter deserves surgical treatment.[10] Cyst aspiration has been one of the options for smaller cysts; however, recurrence is a possibility. Open surgical excision of cysts has been described by several authors.[7] Since the introduction of laparoscopy, it has become a popular and procedure of choice, whenever dealing with small adrenal masses or cysts. Several studies have demonstrated a clear advantage of laparoscopic surgery over open surgery in terms of analgesia, hospital stay, blood loss, and complication rate [Figures 3 and 4].
Figure 3.
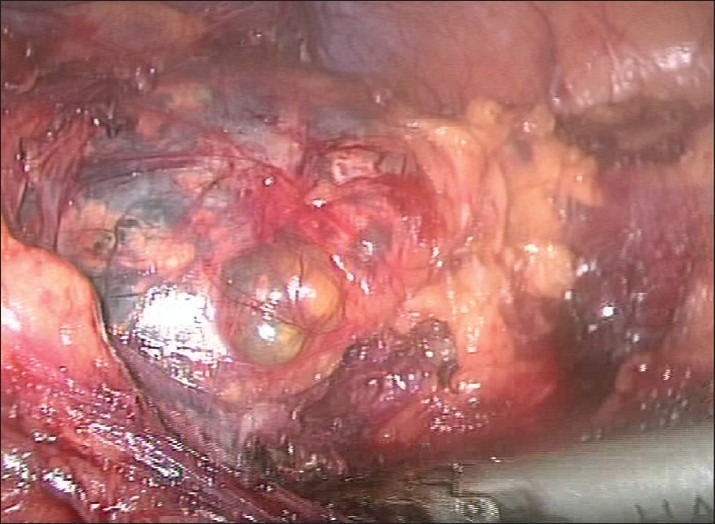
Left adrenal cyst being dissected all around
Figure 4.
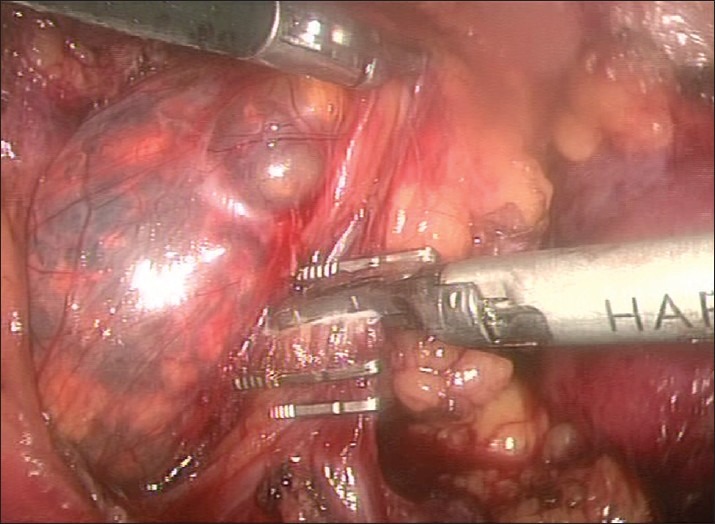
Left adrenal vein being clipped
Castillo et al.[11] reported on the feasibility and safety of laparoscopic management of symptomatic and large adrenal cysts. During the period June 1993 to April 2004 they performed 149 laparoscopic adrenalectomies; out of which, 8 patients with symptomatic adrenal cysts or pseudocysts were treated laparoscopically. Six patients underwent laparoscopic adrenal cyst decortication and marsupialization, one underwent laparoscopic partial adrenalectomy, and one underwent laparoscopic adrenalectomy. Mean operative time was 77.5 min. There were no intraoperative or postoperative complications. Mean hospital stay was 1.7 days. At a mean follow-up of 18.5 months, all patients were asymptomatic and without radiographic evidence of cyst recurrence [Figure 5].
Figure 5.
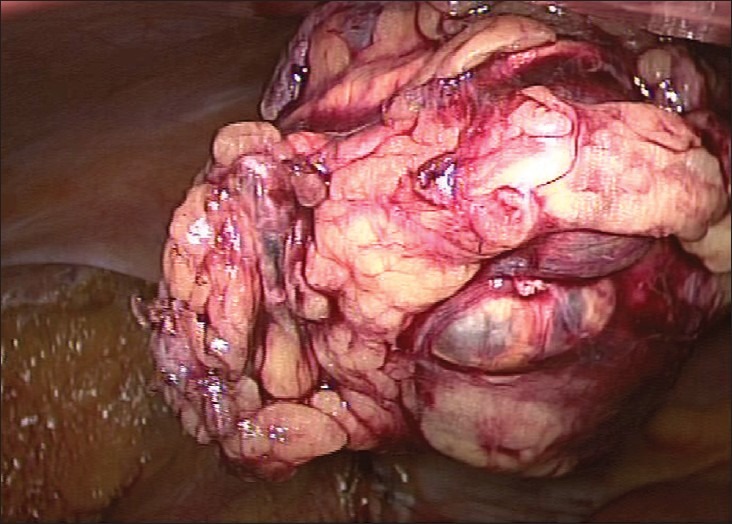
Left adrenal cyst excised
During the period April 2000 to December 2010, 62 patients underwent laparoscopic adrenalectomy which included 11 large pheochromocytomas[12] and 18 children.[13] The mean operating time of laparoscopic adrenalectomy was significantly less when the lesion was a cyst as compared to solid lesions in our experience. Similarly the intraoperative blood loss was also less whenever dealing with a cystic lesion. There were no cases of conversion to open irrespective of the lesion being solid/cystic.
El-Hefnawy et al.[8] assessed the safety and efficacy of different surgical procedures used for managing benign adrenal cysts. Eleven patients underwent open adrenalectomy, whereas 10 patients underwent laparoscopic adrenalectomy. At 90 months follow-up, there were no recurrences in both the groups. In our series, all the 14 patients were symptomatic and were referred to our centre for further management. It was possible to treat all these cystic lesions laparoscopically with minimal invasion, decreased blood loss, and shorter hospitalization.
Twelve of the patients in our series presented with abdominal pain. The mean size of the cyst was 9.57 ± 1.55 cm, which might have been the reason that these lesions were symptomatic in our series. Most cysts that are asymptomatic are of smaller size and are usually incidentally diagnosed. Voluminous cysts have also been reported, which can rupture and lead to massive bleed in the retroperitoneum.[1] Adrenal cysts very rarely have functional rests, or have malignant potential; however, one always need to look out for them especially when dealing with complex cysts.
CONCLUSIONS
Adrenal cysts are rare, but with the use of ultrasonography and other imaging techniques many of these are being diagnosed incidentally. Laparoscopic adrenalectomy is a safe and effective treatment for symptomatic and large benign adrenal cysts. It has the advantages of a shorter hospital stay, less blood loss and enhanced cosmesis. The recurrence of adrenal cysts after surgical removal is less likely.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Favorito LA, Lott FM, Cavalcante AG. Traumatic rupture of adrenal pseudocyst leading to massive hemorrhage in retroperitoneum. Int Braz J Urol. 2004;1:35–6. doi: 10.1590/s1677-55382004000100008. [DOI] [PubMed] [Google Scholar]
- 2.Kazam E, Engel IA, Zirinsky K, Auh JH, Rubenstein WA, Reckler JA, Markisz JA. Sectional imaging of the adrenal glands, computed tomography and ultrasound. In: Vaughan ED Jr, Carey RM, editors. Adrenal Disorders. New York: Thieme Medical; 1989. [Google Scholar]
- 3.Sroujieh AS, Farah GR, Haddad MJ, Abu-Khalaf MM. Adrenal cysts: Diagnosis and management. Br J Urol. 1990;65:570–5. doi: 10.1111/j.1464-410x.1990.tb14822.x. [DOI] [PubMed] [Google Scholar]
- 4.Yoder BM, Wolf JF., Sr Long-term outcome of laparoscopic decortication of peripheral and peripelvic renal and adrenal cysts. J Urol. 2004;171:583–7. doi: 10.1097/01.ju.0000103642.29044.71. [DOI] [PubMed] [Google Scholar]
- 5.Pradeep PV, Mishra AK, Aggarwal V, Bhargav PR, Gupta SK, Agarwal A. Adrenal cysts: An institutional experience. World J Surg. 2006;30:1817–20. doi: 10.1007/s00268-005-0307-3. [DOI] [PubMed] [Google Scholar]
- 6.Bellantone R, Ferrante A, Raffaelli M, Boscherini M, Lombardi CP, Crucitti F. Adrenal cystic lesions: Report of 12 surgically treated cases and review of the literature. J Endocrinol Invest. 1998;21:109–14. doi: 10.1007/BF03350324. [DOI] [PubMed] [Google Scholar]
- 7.Poiana C, Carsote M, Chirita C, Terzea D, Paun S, Beuran M. Giant adrenal cyst: Case study. J Med Life. 2010;3:308–13. [PMC free article] [PubMed] [Google Scholar]
- 8.El-Hefnawy AS, El Garba M, Osman Y, Eraky I, El Mekresh M, Ibrahim el-H. Surgical management of adrenal cysts: Single-institution experience. BJU Int. 2009;104:847–50. doi: 10.1111/j.1464-410X.2009.08537.x. [DOI] [PubMed] [Google Scholar]
- 9.Iuchtman M, Abudi Z, Yurman S, Koren I, Kessler FB. Giant adrenal cyst in the newborn: Perinatal diagnosis and management. Eur J Pediatr Surg. 1994;4:122–4. doi: 10.1055/s-2008-1066084. [DOI] [PubMed] [Google Scholar]
- 10.Wedmid A, Palese M. Diagnosis and treatment of the adrenal cyst. Curr Urol Rep. 2010;11:44–50. doi: 10.1007/s11934-009-0080-1. [DOI] [PubMed] [Google Scholar]
- 11.Castillo OA, Litvak JP, Kerkebe M, Urena RD. Laparoscopic management of symptomatic and large adrenal cysts. J Urol. 2005;173:915–7. doi: 10.1097/01.ju.0000152177.35204.70. [DOI] [PubMed] [Google Scholar]
- 12.Ravish R, Nerli RB, Reddy MN, Siddappa SN, Thakkar R. Laparoscopic adrenalectomy for large pheochromocytoma. Br J Urol. 2007;100:1126–9. doi: 10.1111/j.1464-410X.2007.07179.x. [DOI] [PubMed] [Google Scholar]
- 13.Nerli RB, Reddy MN, Guntaka A, Patil S, Hiremath M. Laparoscopic adrenalectomy for adrenal masses in children. J Pediatr Urol. 2011;7:182–6. doi: 10.1016/j.jpurol.2010.04.006. [DOI] [PubMed] [Google Scholar]


