Abstract
Zidovudine is an important component of first-line antiretroviral treatment (ART) regimens used to manage pediatric HIV. Nail pigmentation with zidovudine is a well-documented occurrence in adults, especially dark-skinned individuals. But it has so far not been reported in children. Here, we report a pediatric case of zidovudine-induced nail pigmentation. A 12-year-old boy receiving ART with zidovudine, lamivudine, and nevirapine presented to dermatology OPD with complaint of diffuse bluish-brown discoloration of all fingernails. The pigmentation was noticed by the patient after 3 months of initiating zidovudine-based regimen. It first appeared in thumb nails, gradually involved all fingernails, and increased in intensity over time. Though harmless and reversible, psychological aspects of this noticeable side effect may hamper adherence to therapy and may lead to unnecessary investigations and treatment for misdiagnosis such as cyanosis or melanoma.
KEY WORDS: HIV, nail pigmentation, zidovudine
Introduction
In India, 23.9 lakh people were living with HIV/AIDS (PLHA) in 2009 and children under 15 years accounted for 3.5% of all infections.[1] According to WHO/UNAIDS estimates, 450,000 children were receiving antiretroviral therapy (ART) and more than 2 million children still needed ART in 2010.[2]
Zidovudine (AZT), being an important component of standard regimen for first-line ART in children,[3] is widely used for managing pediatric HIV. As more and more children are exposed to this drug, the range of adverse reactions can also be expected to expand. Nail pigmentation with AZT is a well-documented occurrence in adults,[4] especially dark-skinned individuals. But so far, it has not been reported in children.
Here, we report a case of zidovudine-induced nail pigmentation in a 12-year-old boy.
Case Report
In December 2011, a 12-year-old boy was brought by guardians to dermatology OPD for nail pigmentation involving all fingernails. About 4 years back, ART was started for him with stavudine-based regimen (12 mg stavudine + 60 lamivudine + 100 mg nevirapine) because of too low hemoglobin level. But after improvement in hemoglobin level, he has been shifted to zidovudine-based regimen (zidovudine 300 mg + lamivudine 150 mg + nevirapine 200 mg) since last 1 year. After 3 months of initiating the new regimen, he noticed bluish-brown discoloration of thumbnails that gradually spread to other fingernails [Figure 1a and b] and grew in intensity over time [Figure 1c and d]. The discoloration began proximally and progressed distally to involve free edge of nails. There was no history of trauma, use of coloring agents, any triggering factor, or abnormal skin or mucosal pigmentation. He was not taking drugs other than antiretrovirals. Past history was not significant. His parents had died due to AIDS.
Figure 1.
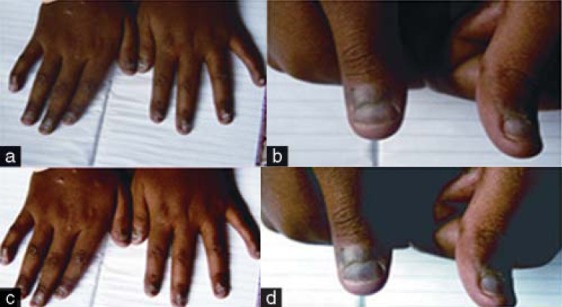
(a) Pigmentation involving all nails (December 2011); (b) thumbnail involvement (December 2011); (c) increased pigmentation in all nails (March 2012); (d) increased pigmentation in thumbnails (March 2012)
On examination, he was averagely built, nourished, and fully immunized. His general and systemic examinations were normal. Local examination revealed diffuse bluish-brown discoloration of all fingernails, but it was more marked in thumbnails. It did not disappear on compression of nail plate. Nails were brittle with loss of lunulae and periungual changes [Figure 1c and d].
Complete blood count revealed low hemoglobin level (9 gm %). His CD4 count was 755/mm3. No specific treatment was given for nail pigmentation. The patient and guardians were counseled about harmless nature of this adverse drug reaction (ADR) and he is receiving the same regimen at present.
Discussion
Nail pigmentation with zidovudine was first described by Furth and Kazakis[5] in two black patients in whom progressive hyperpigmentation of all fingernails developed. Since then, several such case reports have been published from various parts of the world.[6–8] But all these patients were adults, and we did not come across any case report on pediatric patients.
Though our patient was receiving three antiretroviral drugs, zidovudine was thought to be the most likely cause of nail pigmentation, as pigmentation developed after 3 months of initiating zidovudine-based regimen. The causality assessment by Naranjo algorithm[9] showed that this ADR was “probable” with zidovudine. In previous studies, patients taking zidovudine had noticed nail changes in 4–8 weeks or even after 5–6 months.[10–11] Dark-skinned individuals are at higher risk of this adverse effect[12] and it appears to be reversible and dose dependant.[3,6,10]
Nail pigmentation occurs in variety of medical conditions and is also associated with use of several drugs, especially chemotherapeutic agents.[13] The pattern of nail pigmentation may be transverse bands, longitudinal bands, or diffuse discoloration.[6] Occasionally, skin and mucus membranes are also involved.[7]
The underlying mechanism of nail pigmentation is not clear. Animal studies show that there are increased numbers of melanosomes within epidermal keratinocytes.[14] Histopathologic findings of nail biopsy show deposits of brown pigmented granules containing melanin throughout the epidermis.[4,10]
As more patients receive zidovudine, it is important to alert patients about nail pigmentation. Though it is harmless and reversible, psychological aspects of this noticeable side effect may hamper adherence and efficacy of therapy. This may also lead to unnecessary investigations and treatment for misdiagnosis such as cyanosis and melanoma. Physicians should also focus on preventing adverse effects and distinguishing serious ADRs from self-limiting ADRs in order to manage prejudiced and fearful patients with available ART.
Footnotes
Source of Support: Nil.
Conflict of Interest: No.
References
- 1.National AIDS Control Organization (NACO) Annual Report 2010-11. [Last accessed on 2012 Apr 08]. Available from: http://www.nacoonline.org/ upload/REPORTS/NACO Annual Report 2010-11 .
- 2.Data and statistics: Antiretroviral therapy. [Last accessed on 2012 Apr 08]. Available from: http://www.who.int/hiv/topics/treatment/data/en/index.html .
- 3.Antiretroviral therapy for HIV infection in infants and children: Towards universal access. Recommendations for public health approach, 2010 Revision. [Last accessed on 2012 Apr 08]. Available from: http://www.whqlibdoc.who.int/publications/2010 . [PubMed]
- 4.Rahav G, Maayan S. Nail pigmentation associated with zidovudine: A review and report of a case. Scand J Infect Dis. 1992;24:557–61. doi: 10.3109/00365549209054640. [DOI] [PubMed] [Google Scholar]
- 5.Furth P, Kazakis A. Nail pigmentation changes associated with azidothymidine. Ann Intern Med. 1987;107:350. doi: 10.7326/0003-4819-107-2-350. [DOI] [PubMed] [Google Scholar]
- 6.Groak SP, Hood AF, Nelson K. Nail pigmentation with zidovudine. J Am Acad Dermatol. 1989;21:1032–3. doi: 10.1016/s0190-9622(89)80384-6. [DOI] [PubMed] [Google Scholar]
- 7.Greenberg RG, Berger TG. Nail and mucocutaneous hyperpigmentation with azidothymidine therapy. J Am Acad Dermatol. 1990;22:327–30. doi: 10.1016/0190-9622(90)70039-k. [DOI] [PubMed] [Google Scholar]
- 8.Anders KH, Abelle DC. Development of nail pigmentation during zidovudine therapy. J Am Acad Dermatol. 1989;21:792–3. doi: 10.1016/s0190-9622(89)80271-3. [DOI] [PubMed] [Google Scholar]
- 9.Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–45. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 10.Grau-Massanes M, Millan F, Febrer MI, Pujol C, Alegre VA, Salavert M, et al. Pigmented nail band and mucocutaneous pigmentation HIV positive patients treated with zidovudine. J Am Acad Dermatol. 1989;21:687–8. doi: 10.1016/s0190-9622(08)81046-8. [DOI] [PubMed] [Google Scholar]
- 11.Benedick C, Rasokat H, Steigleder GK. Azidothymidine induced hyperpigmentation of skin and nails. Arch Dermatol. 1989;125:1285–6. [PubMed] [Google Scholar]
- 12.Cheemah PE, Grimes RM, Rowan P, Huang YJ, Essein EJ, Lewis ST. Melanonychia in patients infected with human immunodeficiency virus original communication. AIDS. 2011;1:15–9. [Google Scholar]
- 13.Zaiac MN, Daniel CR. Pigmentation abnormalities. In: Scher RK, Daniel CR, editors. Nails: Therapy, diagnosis, surgery. 3rd ed. Philadelphia: Elsevier Saunders; 2005. pp. 73–89. [Google Scholar]
- 14.Obuch ML, Baker G, Roth RI, Yen TS, Berger TG. Selective cutaneous hyperpigmentation in mice following zidovudine administration. Arch Dermatol. 1992;128:508–13. [PubMed] [Google Scholar]


