Abstract
Study Design
This prospective cohort study investigated personal goal achievement and satisfaction with progress in patients with chronic disabling spinal disorders (CDSD).
Objective
This study examined the relationships between satisfaction with progress and several alternative outcome measures for CDSD patients at least 1 year after completing a functional restoration program (FRP).
Summary of Background Data
Treatment outcome measures for CDSD commonly include pain, physical capacities, and functional/vocational status. These factors are weakly correlated and may not reflect individual patients’ perspectives and priorities.
Methods
Upon enrollment in the FRP, patients’ pre-treatment functional, work, and recreation goals were recorded. Pre- and end-of-program clinical measures included: pain, disability, fear avoidance, lifting, trunk flexibility, and treadmill endurance. At least 1 year after program completion surveys were mailed to consecutive FRP graduates. Non-responders were surveyed by telephone when possible. Surveys included each patient’s personal pre-treatment goals, and assessed Average Pain, SF-36 Physical Function, and satisfaction “with the progress made with your pain problem.” Each patient indicated levels of importance and achievement for each personal goal, and these scores were integrated to yield a goal achievement score (GAS). Linear regression was used to test the relationships between 1-year satisfaction with progress and the following variables: baseline to end-of-program change in clinical measures, and 1-year pain, physical function, and GAS.
Results
Of the 106 surveys mailed, 89 (84%) were returned and 86 (81%) had complete data for analysis. None of the pre-post program clinical measures was significantly correlated with satisfaction (overall R2=0.013, p<0.74). In contrast, year-end Average Pain (R2=0.28), Physical Function (R2=0.29), and GAS (R2=0.29) were each significantly correlated (p<.0001) with satisfaction, with a combined R2=0.43, p<.0001. Of these variables, GAS had the highest unique contribution to satisfaction.
Conclusions
For CDSD patients one year after completing rehabilitation, compared to more traditional outcomes, goal achievement scores provided the greatest unique contribution to patient satisfaction. Goal achievement may be a valuable patient-centered measure of treatment outcome.
INTRODUCTION
For many years treatment outcomes for people with chronic disabling spinal disorders (CDSDs) have included pain, physical capacities, socioeconomic well-being, and work status. Recently, there has been a shift toward using patient self-assessments, and patient satisfaction has emerged as a widely used treatment outcome measure. The diversity of outcome measures used in research studies of spinal disorders has complicated the comparison of study results, prompting recommendations to develop a standardized panel of measures including back-specific function, generic health status, pain, work disability, and patient satisfaction. (1, 2)
Although standardization of measurement may provide important benefits for the interpretation of group studies, the fundamental problem of choosing a patient-centered measure to evaluate treatment success per individual remains unsolved. Correlations between clinical variables (e.g., pain, physical impairment and disability) before and after treatment are generally weak. (1, 3–9) Generic health indexes such as the SF-36 may obscure important personal differences in pain and functional outcomes, and none of the traditional measures accounts for patients’ preferences or priorities regarding outcomes. Patient satisfaction with progress may come closest to this target. However, it is by definition retrospective, and therefore has limited capacity to guide treatment decision-making in real time.
Previous studies have shown that patient satisfaction following rehabilitation for CDSDs correlates weakly with pain, physical capacity and work outcomes, and that satisfaction relates more closely to the extent to which individuals retrospectively feel they have achieved their goals regarding pain relief and physical capacity gains. (4, 5) Simply having a return to work goal was the best predictor of eventual work status in a sample of patients participating in a chronic pain management program. (10)
This study examines the relative contributions of personal functional goal achievement and more traditional clinical measures to patient satisfaction with progress for people with CDSDs one year after completing a Functional Restoration Program (FRP). The central hypothesis is that personal functional goal achievement will demonstrate the strongest relationship with patient satisfaction with progress.
MATERIALS AND METHODS
Patient Selection
This study involved CDSD patients at least one year following completion of a three-week FRP. Patients were initially referred from community-based medical practices in Vermont and New Hampshire for evaluation by practitioners in the Dartmouth- Hitchcock Medical Center’s Spine Center. These practitioners in turn referred patients to the FRP on the basis of meeting the following criteria: 1) more than 3 months’ disabling back pain; 2) absence of a clear surgically correctable lesion or cardiovascular co-morbidity restricting activity; 3) psychological capacity to engage in group activities; and 4) treadmill, lifting and flexibility tests indicating significant deficits compared to the patient’s personal functional goals. Pre-admission evaluations focusing on these inclusion criteria were conducted by a medical doctor or nurse practitioner. The study was approved and monitored by the Committee for the Protection of Human subjects at the Dartmouth-Hitchcock Medical Center and Dartmouth College.
FRP Protocol
The FRP consisted of 13 eight-hour sessions over three weeks. Each session included physical training, educational classes, and cognitive therapy as previously described.(11) On the first day of the treatment program, all patients completed the following questionnaires: a pain visual analog scale (VAS);(12–14) the Oswestry Disability Index (ODI);(15, 16) Physical Function subscale (PF) of the Medical Outcomes Study SF-36; (17) the Center for Epidemiologic Studies Depression Scale (CESD);(18, 19) and the Fear Avoidance Beliefs Questionnaire (FABQ).(20, 21)
The following physical capacity tests were also conducted: sagittal trunk flexibility measured by inclinometer (ROM);(22) Progressive Isoinertial Lifting Evaluation (PILE), (23) in which the patient performed a repetitive lifting task; and aerobic performance (METS), in which the patient walked on a treadmill, with speed and inclination increased per protocol to maximum tolerance or target heart rate (0.8 × 220-age).
On the first day of the FRP an occupational therapist recorded each patient’s response to the question, “What is your goal for work 3 months from now?” This question was repeated and response recorded for recreation and for activities of daily living. On the second day the program director reviewed the test results and the goals with each patient, confirming the accuracy of the stated goals or editing them according to the patient’s request. All of the first-day tests and measures were repeated on day 13 of the FRP. On the final day, the program director met with each patient to review the final results relative to initial results and goals. Initial and end-of-program clinical measures were entered into a computer database by administrative staff.
Follow-up Protocol
A survey was developed to evaluate health status and patient satisfaction one year after completing the FRP. Surveys were customized using a mail merge feature to insert each patient’s personal goals as recorded verbatim during the FRP into separate boxes within the survey for the Work, Recreational and Daily Activities domains.
Survey Content assessed
Pain magnitude: worst pain in the last week, average pain over the last week, and current pain using the Iowa Pain Thermometer, a 13-point modified Likert scale (24)
The Physical Function subscale of the SF-36
Current work status, level (full v. part time), and capacity
Worker’s Compensation and Social Security Disability status
“Satisfaction with the progress made with your pain problem” using a 6-point Likert scale ranging from “strong satisfaction” to “strong dissatisfaction”
Goal Achievement: the patient’s assessment of how completely they had met their goals for work, recreation and daily activities on a 7-point Likert scale ranging from “completely met” to “not at all met”
Goal Importance: the patient’s assessment of how important each goal was on a 7-point Likert scale ranging from “very high importance” to “no importance”
Goal Achievement Scoring
The 7-point goal achievement scale was scored as 7, 5, 3, 1, −1, −3, −5 and the 7-point goal importance scale was scored as 7, 6, 5, 4, 3, 2, and 1. For each of the three goal domains (work, recreation, activities of daily living) the achievement and importance scores were multiplied to produce a domain score. Multiplying these two scales could produce up to 49 unique domain scores with a directional range from +49 (7 × 7, indicating a very important goal completely met) to −35 (−5 × 7, indicating an very important goal not at all met). Linear transformation [(score + 35) / 84) × 100] gave positive scores ranging from 0 to 100. For each patient the three domain scores were averaged yielding a composite goal achievement score (GAS). For patients who did not provide a goal for all three domains, the GAS was the average of the two domain scores they did have.
Recruitment Protocol
The individualized surveys were mailed to 106 consecutive graduates from the FRP who had completed the program at least 1 year prior to the inception of the study. A second survey was mailed to all non-responders after two weeks. Clinical research staff attempted to contact all remaining non-responsive subjects by phone to read the survey to the subjects and record their responses.
Statistical Analyses
Data Entry
Clinical data from the FRP program were entered monthly during the treatment portion of the study into an Excel™ spreadsheet. Data from the follow-up survey were entered into a separate Excel™ spreadsheet. All of these values were entered by FRP administrative personnel. Double data entry was done to ensure accuracy.
Analysis Plan
Potential differences between responders and non-responders were evaluated by comparing patient demographics and functional capacities during the program. Continuous variables were compared using analysis of variance and categorical variables using chi-square tests. The internal consistency of the GAS was assessed using Cronbach’s alpha (25) for those patients who had provided goal attainment scores in all three domains.
We used linear regression analyses to evaluate the relationship between satisfaction at one year and three sets of variables: 1) Clinical Measures: pre-post FRP changes in Pain, Oswestry, CESD, FABQ, lifting, treadmill endurance, and trunk flexibility; 2) Pain and Physical Function as reported on the 1-year follow-up survey; and 3) Goal Achievement Score (GAS). Simple and multiple regression of satisfaction on each outcome assessed the relationship between satisfaction and each variable, by comparing the amount of satisfaction variance explained by each variable and combinations of variables.
All analyses were computed using SAS™ (SAS Institute, Cary, North Carolina) version 9.1.3 running under the Windows XP® Professional operating system.
RESULTS
Data Quality
The overall inconsistency rate from the double data entry per datum entered was 0.18%. All inconsistencies were resolved by referring back to the source document.
Sample and Non-response
Of the 106 patients who had completed the FRP program at least 1 year prior to this study, 83.9% (89/106) agreed to participate in the study. Of the 17 remaining: 3 declined to participate; 5 could not be reached by phone; and 9 could not be located. Table 1 summarizes patient characteristics for responders and non-responders. For these 89 patients, the average length of follow-up was 1.8 years and ranged from 1.05 to 2.57 years. No significant differences were observed between responders and non-responders for pre-post FRP changes in clinical measures or in gender, but non-responders were significantly younger than responders [37.3 (8.64) vs. 42.2 (9.15), p < .048]. Three of the 89 were excluded from year-end analysis because of missing responses in their follow-up surveys.
Table 1.
Patient demographics and pre/post FRP changes in clinical measures.
| Responders | Non-Responders | ||||
|---|---|---|---|---|---|
| Variable/Statistic | N | Statistic | N | Statistic | p < |
| Age: mean (sd) | 89 | 42.2 (9.15) | 17 | 37.3 (8.64) | 0.048 |
| Gender: Females % | 89 | 49.40% | 17 | 47.10% | 0.86 |
| Program Change in: | |||||
| Pain mean (sd) | 88 | 0.50 (2.46) | 17 | 0.96 (3.17) | 0.51 |
| BP mean (sd) | 88 | 4.27(6.81) | 17 | 4.69(7.06) | 0.82 |
| ROM mean (sd) | 79 | 26.8(17.7) | 16 | 26.2(22.9) | 0.91 |
| PILE mean (sd) | 88 | 30.3(16.0) | 17 | 34.1(19.0) | 0.40 |
| MET mean (sd) | 88 | 2.31(2.43) | 17 | 3.18(2.48) | 0.19 |
| ODI mean (sd) | 88 | 12.7(11.4) | 17 | 12.7(14.6) | 0.99 |
| FABQ mean (sd) | 88 | 9.95(12.5) | 17 | 11.35(8.77) | 0.67 |
All program change scores were scaled so that positive values indicated improvement
The personal and health demographics for the 86 patients who made up the 1 year post FRP cohort are summarized in Table 2 and Table 3 displays their work and compensation status. Table 4 presents summary statistics for the dependent variable of patient satisfaction and the relative contributions of pain, physical function and GAS.
Table 2.
Personal and Health Demographics for the 1-Year Post FRP Cohort
| Variable | Levels | N | Pct | χ 2 | df | p < |
|---|---|---|---|---|---|---|
| Age Groups | 18–35 | 18 | 20.9 | 31.14 | 2 | .0001 |
| 36–50 | 53 | 61.6 | ||||
| 51–62 | 15 | 17.4 | ||||
| Female | 43 | 50.0 | 0 | 1 | - | |
| Gender | Male | 43 | 50.0 | |||
| No | 76 | 89.4 | 52.8 | 1 | .0001 | |
| Surgery Following FRP | Yes 1 | 6 | 7.1 | |||
| Yes 2 | 2 | 2.4 | ||||
| Yes 3 | 1 | 1.2 | ||||
| Missing* | 1 | |||||
| Medical Visits since FRP | No | 24 | 27.9 | 12.37 | 4 | .015 |
| Yes (1–5) | 26 | 30.2 | ||||
| Yes (6–10) | 12 | 13.9 | ||||
| Yes (11–20) | 10 | 11.6 | ||||
| Yes (21+) | 14 | 16.3 | ||||
| New Health Problems since FRP | Yes | 20 | 23.8 | 23.05 | 1 | .0001 |
| No | 64 | 76.2 | ||||
| Missing* | 2 |
missing not including in the computation of the chi-square statistic reported
Table 3.
Work and Compensation Variables for the FRP Cohort
| Variable | Levels | N | Pct | χ 2 | df | p < |
|---|---|---|---|---|---|---|
| Work Status** | Not Working | 35 | 40.7 | 2.98 | 1 | .085 |
| Disabled | 11 | 12.8 | ||||
| Retired | 5 | 5.8 | ||||
| Student | 1 | 1.2 | ||||
| Not Looking | 5 | 5.8 | ||||
| Looking for | 13 | 15.1 | ||||
| Full time | 3 | 3.5 | ||||
| Part time | 1 | 1.2 | ||||
| Anything | 9 | 10.5 | ||||
| Working | 51 | 59.3 | ||||
| Part Time | 13 | 15.1 | ||||
| Severity Modified | 1 | 1.2 | ||||
| Moderately Modified | 5 | 5.8 | ||||
| Slightly Modified | 4 | 4.7 | ||||
| Full duty | 3 | 3.5 | ||||
| Full Time | 38 | 44.2 | ||||
| Moderately Modified | 2 | 2.3 | ||||
| Slightly Modified | 9 | 10.5 | ||||
| Full Duty | 27 | 31.4 | ||||
| Worker’s Compensation Status*** | Eligible | 31 | 39.7 | 3.28 | 1 | .07 |
| Received | 25 | 32.1 | ||||
| Awaiting result | 6 | 7.7 | ||||
| Denied | 0 | 0.0 | ||||
| Not Eligible | 47 | 60.3 | ||||
| Missing* | 8 | |||||
| Social Security Disability*** | Eligible | 28 | 37.8 | 4.38 | 1 | .037 |
| Received | 14 | 18.9 | ||||
| Awaiting result | 4 | 5.4 | ||||
| Plan to apply | 2 | 2.7 | ||||
| Denied | 8 | 10.8 | ||||
| Not Eligible | 46 | 62.2 | ||||
| Missing* | 12 |
Missing responds are not included in the computation of the chi-square statistic reported
For this variable, the Chi-square test is comparing Working vs. Non-working only
For these variables, the Chi-square test is comparing Eligible vs. Not Eligible
Table 4.
Satisfaction, Average Pain, Physical Function and Goal Achievements at least 1 year after completing the FRP
| Variable | Scale and Interpretation | N | Mean | SD | Min | Max |
|---|---|---|---|---|---|---|
| Satisfaction | (1–6) Higher Values Greater Satisfaction | 86 | 4.1 | 1.72 | 1 | 6 |
| Average Pain | (0–12) Higher Values Greater Pain | 86 | 5.5 | 2.50 | 0 | 11 |
| Physical Function (PF) | Standardized to Mean 50 and SD 10, Higher Values Greater Function | 86 | 42.2 | 12.03 | 14.9 | 57.0 |
| Goal Attainment: Work | (0–100) Higher Values Greater Attainment | 84 | 58.0 | 36.73 | 0 | 100 |
| Goal Attainment: Recreation | 77 | 54.9 | 33.00 | 0 | 100 | |
| Goal Attainment Home | 72 | 67.3 | 29.41 | 0 | 100 | |
| Goal Attainment: Composite | 86 | 59.7 | 28.41 | 0 | 100 |
Relationships Between Outcomes and Patient Satisfaction with Progress
Pre-post FRP Changes in Clinical Measures
Changes in pre-post FRP clinical measures, individually or in combinations, were not significantly related to satisfaction with progress at one-year (overall R2 = 0.013, p<0.74).
Pain, Function and Goal Achievement after at least 1 year
Table 5 summarizes the univariate regression model of satisfaction with progress on the pain, function and GAS variables, as well as intercorrelations among these variables. Average Pain and Physical Function scores at 1-year had weak to moderate and statistically significant relationships with satisfaction (R2 = 0.28, p < 0.0001 and R2 = 0.30, p < .0001, respectively). Some patients did not provide a goal for all three domains: work(n=2), recreation(n=9) and activities(n=14). The internal consistency based on Cronbach’s alpha(25) for those patients who did have GAS in all three domains was 0.78. GAS also demonstrated weak to moderate and statistically significant association with satisfaction (R2 = 0.29, p < .0001).
Table 5.
Intercorrelations and variance explained (R2) for Satisfaction, and Patient’s reported Average pain, Physical function and Goal Achievement at least 1 year after completing the FRP
| Goal Achievement | |||||||
|---|---|---|---|---|---|---|---|
| Satisfaction N = 86 |
Avg. Pain N = 86 |
PF N = 86 |
Work N = 84 |
Recreation N = 77 |
Home N = 72 |
Composite N = 86 |
|
| Satisfaction | 1.00 | −0.530 | 0.547 | 0.364 | 0.509 | 0.554 | 0.542 |
| Average Pain | 0.281 | 1.00 | −0.607 | −0.432 | −0.411 | −0.408 | −0.460 |
| PF | 0.299 | 1.00 | 0.279 | 0.512 | 0.525 | 0.406 | |
| GA: Work | 0.132 | 1.00 | 0.552 | 0.372 | 0.824 | ||
| GA: Recreation | 0.259 | 1.00 | 0.690 | 0.885 | |||
| GA: Home | 0.307 | 1.00 | 0.807 | ||||
| GA: Composite | 0.293 | 0.299 | 0.132 | 0.259 | 0.307 | 0.294 | 1.00 |
Pearson Correlations between variables are above the diagonal.
All correlations in the table were statistically significant at p < .05
Bolded scores in the Satisfaction column are the simple regression R2 values
Combined Model and Unique Contributions to Patient Satisfaction
In the multiple regression model, Average Pain, SF-36 Physical Function and GAS after 1 year together explained 43.5% of the variance in satisfaction (p < .0001). The unique contributions of each variable to 1-year satisfaction are illustrated in Figure 1. GAS made the greatest unique contribution to satisfaction: GAS 7.35%, Physical Function 4.21%, and Average Pain 2.90%.
Figure 1.
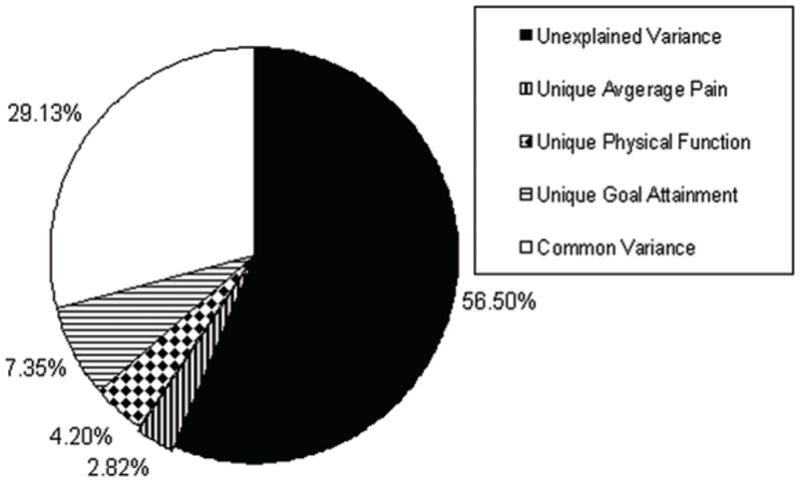
Variance explained in 1-year satisfaction by Average Pain, Physical Function, and GAS at 1 year (n=86).
Discussion
This study showed that for CDSD patients at least one year completing a functional restoration program, satisfaction with progress was more strongly related to personal functional goal achievement than to more traditional outcome measures including pain, disability, fear avoidance, lifting, trunk flexibility, and treadmill endurance. These findings are consistent with previous work that assessed treatment goal achievements short-term, with a smaller sample (six weeks, n= 59). (5) Similarly, Tan et al. found that return-to-work goals were predictive of return to work in a sample of patients participating in a chronic pain management program. (10)
Although goal-setting has been used for several decades in the field of psychology to provide feedback and motivation to patients, and for program evaluation, (26) most applications include provider-nominated goals. In contrast, our rehabilitation practice emphasizes the patient’s role in clinical decision-making and program evaluation processes, and therefore targets patient-nominated goals.
Research in other health areas has examined the performance of goal attainment scaling as an outcome measure compared to more traditional measures. (27, 28) Oldridge, et al. compared goal attainment (yes or no) to generic and specific health-related quality of life measures and exercise tolerance in post-myocardial infarction patients randomized to rehabilitation or usual care. In that study, there were no differences between those outcomes for patients who did and did not attain their goals. The authors suggested that goal attainment might not be a valid measure of outcome, disregarding the possibility that the goal priorities and degree of achievement could have detected important changes from the patients’ perspectives.
Two studies investigated the measurement properties of patient-nominated goal attainment in the area of pain management programs, and found preliminary evidence for validity and reliability. (29, 30) Similarly, Gordon, et al. (27) found weak correlations between goal attainment and traditional measures of health status among geriatric patients with dementia. However, effect size analysis revealed that goal attainment scaling was the more sensitive measure of change among these patients. All three studies concluded that goal attainment scaling provides different and critical information about the value of treatment in these populations. It should be noted that Gordon, et al. used provider-nominated goals due to the challenge of patient-nominated goal-setting in the presence of dementia. Our study results are consistent with Oldridge and Gordon’s work in that traditional clinical outcome measures (pre-FRP to end of FRP changes demonstrated very low correlation with satisfaction and goal achievement. measured at least 1 year after FRP completion.
These prior studies provided insight into the relationship between goal attainment and traditional health measures, but they did not examine the relationship between goal attainment and patient satisfaction with outcome. Elkadry, et al. assessed the relationship between patient-nominated goals and satisfaction for patients undergoing surgery for pelvic reconstructive surgery.(31) They reported that although goal achievement strongly correlated with satisfaction (r=0.57, p<0.001), objective clinical and urodynamic outcomes did not. Their findings are consistent with those of our study, however, interpretation of this study is limited by the use of “overall satisfaction.” Although satisfaction is relatively new to the health care outcome measurement arena, it is already very clear that satisfaction is a multi-dimensional construct.(32–35) It is likely that overall satisfaction questions measure many dimensions of care such as the patient-provider interaction.(32) We focused on “satisfaction with progress you have made with your pain problem” in order to avoid measuring satisfaction with care received. The follow-up survey contained 3 satisfaction questions regarding: 1) progress with your pain problem; 2) care received in the FRP; and 3) living the rest of your life with your current symptoms. Scores for questions 1 and 3 were highly correlated, and combined responses to questions 1 and 3 were highly consistent with responses to question 1 alone, so question 3 responses were eliminated in our final analysis.
In this study final pain, physical function and GAS together explained 43.5% of the variance in satisfaction with progress. The unique contribution of goal achievement was approximately twice that of either pain or function, indicating that goal achievement adds information beyond the more traditional measures of outcome and deserves further study.
Limitations and Future Research
Although many of the components of our follow-up survey have been studied, the entire survey has not been validated in its current form. Future work will include refinement and validation. We are particularly interested in comparing the impact on satisfaction from symptom vs. functional goal achievement.
This study design did not allow assessment of changes of goal content or importance over time. Future research will provide for on-going monitoring of these changes.
As illustrated in Figure 1, a little more than half of the variance in patient satisfaction remains unexplained even after combining the traditional measures and the GAS. From our discussions with hundreds of CDSD patients in the FRP, it is clear that they vary widely in prioritizing symptom and functional outcomes. Clarifying pre-treatment goals in both symptom and functional domains and assessing goal achievement outcomes accordingly may provide a new model for guiding treatment choices and assessing patient-centered outcomes. This approach would give patients and their health care providers a powerful tool in finding the “right treatment for the right patient” and assessing how well the treatment really worked for that patient. For example, a patient who rates pain relief as very important and functional goal achievement as not important may be more satisfied with treatment aimed at pain relief (medication, modalities, etc.). A patient who values functional recovery over pain relief may be more satisfied with outcomes from intensive rehabilitation.
Acknowledgments
Supported by NIAMS (P60-AR048094) and NICHD (1F32HD056763)
References
- 1.Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, et al. Outcome measures for low back pain research. A proposal for standardized use.[erratum appears in Spine 1999 Feb 15;24(4):418] Spine. 1998 Sep 15;23(18):2003–13. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 2.Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine. 2000 Dec 15;25(24):3100–3. doi: 10.1097/00007632-200012150-00003. [DOI] [PubMed] [Google Scholar]
- 3.Dionne CE, Von Korff M, Koepsell TD, Deyo RA, Barlow WE, Checkoway H. A comparison of pain, functional limitations, and work status indices as outcome measures in back pain research. Spine. 1999;24(22):2339–45. doi: 10.1097/00007632-199911150-00009. [DOI] [PubMed] [Google Scholar]
- 4.Hazard RG, Haugh LD, Green PA, Jones PL. Chronic low back pain. The relationship between patient satisfaction and pain, impairment, and disability outcomes. Spine. 1994;19(8):881–7. [PubMed] [Google Scholar]
- 5.Hazard RG, Osterhoudt C, Haugh L, Simon M. International Society for the Study of the Lumbar Spine. Edinburgh: 2001. Chronic spinal pain: The relationship between patient satisfaction, symptom and physical capacity outcomes, and achievement of personal goals following functional restoration. [Google Scholar]
- 6.Kovacs FM, Abraira V, Zamora J, Gil de Real MT, Llobera J, Fernandez C. Correlation between pain, disability, and quality of life in patients with common low back pain. Spine. 2004;29(2):206–10. doi: 10.1097/01.BRS.0000107235.47465.08. [DOI] [PubMed] [Google Scholar]
- 7.Waddell G, Main CJ, Morris EW, Di Paola M, Gray IC, Waddell G, et al. Chronic low-back pain, psychologic distress, and illness behavior. Spine. 1984 Mar;9(2):209–13. doi: 10.1097/00007632-198403000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Deyo RA, Bass JE, Walsh NE, Schoenfeld LS, Ramamurthy S, Deyo RA, et al. Prognostic variability among chronic pain patients: implications for study design, interpretation, and reporting. Archives of Physical Medicine & Rehabilitation. 1988 Mar;69(3 Pt 1):174–8. [PubMed] [Google Scholar]
- 9.Deyo RA, Deyo RA. Measuring the functional status of patients with low back pain. Archives of Physical Medicine & Rehabilitation. 1988 Dec;69(12):1044–53. [PubMed] [Google Scholar]
- 10.Tan V, Cheatle MD, Mackin S, Moberg PJ, Esterhai JL, Jr, Tan V, et al. Goal setting as a predictor of return to work in a population of chronic musculoskeletal pain patients. International Journal of Neuroscience. 1997 Dec;92(3–4):161–70. doi: 10.3109/00207459708986399. [DOI] [PubMed] [Google Scholar]
- 11.Hazard RG. Functional restoration of the patient with chronic back pain. In: Frymoyer JW, editor. The Adult Spine: Principles and Practice. 2. Philadelphia, PA: Lippincott Raven; 1997. [Google Scholar]
- 12.Hagg O, Fritzell P, Nordwall A, Hagg O, Fritzell P, et al. Swedish Lumbar Spine Study G. The clinical importance of changes in outcome scores after treatment for chronic low back pain.[see comment] European Spine Journal. 2003 Feb;12(1):12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 13.Huskisson EC, Huskisson EC. Measurement of pain. Lancet. 1974 Nov 9;2(7889):1127–31. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 14.Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine. 2008 Jan 1;33(1):90–4. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 15.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–3. [PubMed] [Google Scholar]
- 16.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000 Nov 15;25(22):2940–52. doi: 10.1097/00007632-200011150-00017. discussion 52. [DOI] [PubMed] [Google Scholar]
- 17.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 18.Roberts RE, Vernon SW, Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale: its use in a community sample. American Journal of Psychiatry. 1983 Jan;140(1):41–6. doi: 10.1176/ajp.140.1.41. [DOI] [PubMed] [Google Scholar]
- 19.Sheehan TJ, Fifield J, Reisine S, Tennen H, Sheehan TJ, Fifield J, et al. The measurement structure of the Center for Epidemiologic Studies Depression Scale. Journal of Personality Assessment. 1995 Jun;64(3):507–21. doi: 10.1207/s15327752jpa6403_9. [DOI] [PubMed] [Google Scholar]
- 20.Waddell G, Newton M, Henderson I, Somerville D, Main CJ, Waddell G, et al. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993 Feb;52(2):157–68. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 21.Williamson E, Williamson E. Fear Avoidance Beliefs Questionnaire (FABQ) Australian Journal of Physiotherapy. 2006;52(2):149. doi: 10.1016/s0004-9514(06)70052-6. [DOI] [PubMed] [Google Scholar]
- 22.Mayer TG, Tencer AF, Kristoferson S, Mooney V. Use of noninvasive techniques for quantification of spinal range of motion in normal subjects and in chronic low back dysfunction patients. Spine. 1984;9:588–95. doi: 10.1097/00007632-198409000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Mayer TG, Barny D, Kishino ND, Nicholas G, Gatchell RJ, Mayer H, et al. Progressive isoinertial lifting evaluation I. A standardized protocol and normative database. Spine. 1988;13:993–7. doi: 10.1097/00007632-198809000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Herr K, Spratt KF, Garand L, Li L. Evaluation of the Iowa pain thermometer and other selected pain intensity scales in younger and older adult cohorts using controlled clinical pain: a preliminary study. Pain Med. 2007;8(7):585–600. doi: 10.1111/j.1526-4637.2007.00316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16( 3):297–334. [Google Scholar]
- 26.Cardillo JE, Smith A. Goal Attainment Scaling: Applications, Theory, and Measurement. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1994. [Google Scholar]
- 27.Gordon JE, Powell C, Rockwood K, Gordon JE, Powell C, Rockwood K. Goal attainment scaling as a measure of clinically important change in nursing-home patients. Age & Ageing. 1999 May;28(3):275–81. doi: 10.1093/ageing/28.3.275. [DOI] [PubMed] [Google Scholar]
- 28.Oldridge N, Guyatt G, Crowe J, Feeny D, Jones N, Oldridge N, et al. Goal attainment in a randomized controlled trial of rehabilitation after myocardial infarction. Journal of Cardiopulmonary Rehabilitation. 1999 Jan-Feb;19(1):29–34. doi: 10.1097/00008483-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Fisher K, Hardie RJ. Goal attainment scaling in evaluating a multidisciplinary pain management programme. Clinical Rehabilitation. 2002;16:871–7. doi: 10.1191/0269215502cr554oa. [DOI] [PubMed] [Google Scholar]
- 30.Williams RC, Stieg RL. Validity and therapeutic efficacy of individual patient goal attainment procedures in a chronic pain centre. Clinical Journal of Pain. 1987;2:219–28. [Google Scholar]
- 31.Elkadry EA, Kenton KS, FitzGerald MP, Shott S, Brubaker L. Patient-selected goals: A new perspective on surgical outcome. American Journal of Obstetrics and Gynecology. 2003;189:1551–8. doi: 10.1016/s0002-9378(03)00932-3. [DOI] [PubMed] [Google Scholar]
- 32.Hudak PL, Wright JG, Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine. 2000 Dec 15;25(24):3167–77. doi: 10.1097/00007632-200012150-00012. [DOI] [PubMed] [Google Scholar]
- 33.Kravitz R. Patient satisfaction with health care: critical outcome or trivial pursuit? Journal of General Internal Medicine. 1998 Apr;13(4):280–2. doi: 10.1046/j.1525-1497.1998.00084.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rao JK, Weinberger M, Kroenke K. Visit-specific expectations and patient-centered outcomes: A literature review. Archives of Family Medicine. 2000;9(10):1148–55. doi: 10.1001/archfami.9.10.1148. [DOI] [PubMed] [Google Scholar]
- 35.Ware JE, Jr, Davies-Avery A, Stewart AL. The measurement and meaning of patient satisfaction. Health & Medical Care Services Review. 1978 Jan-Feb;1(1):1, 3–15. [PubMed] [Google Scholar]


