Abstract
Transformation to a large cell lymphoma may occur during the course of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) in approximately 5% of the cases. This is known as Richter's transformation. A much less frequent transformation to Hodgkin lymphoma may occur. We report a case of CLL/SLL in which a transformation to Hodgkin lymphoma occurred, and we review previously published reports of this transformation. Transformation to Hodgkin lymphoma in CLL/SLL has a poor outcome compared to de novo cases of Hodgkin lymphoma.
During the course of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), a transition to an aggressive large cell lymphoma may occur. This is referred to as Richter's syndrome and occurs in about 5% of cases of CLL/SLL (1, 2). Transformation to Hodgkin lymphoma has infrequently been described as the “Hodgkin variant of Richter transformation.” It might be more appropriately termed Hodgkin transformation of CLL/SLL. We report a man with chronic lymphocytic leukemia who developed Hodgkin lymphoma during the course and treatment of his primary disease and review previously published reports of this transformation.
CASE REPORT
A 44-year-old man was well until September 2011, when he presented with massive lymphadenopathy and a white cell count of over 300 K/μL (Figure 1). He was subsequently diagnosed with CLL/SLL by morphology and flow cytometry. He underwent plasmapheresis and was started on rituximab and bendamustine. He showed a good response to chemotherapy and by February 2012 had only minimal residual disease. He completed eight cycles of chemotherapy up to May 2012. He then started having watery diarrhea and became febrile (up to 105°F). He was admitted to Baylor Regional Medical Center at Grapevine in May 2012 for evaluation and treatment of his symptoms. Blood cultures were negative. His stool culture was positive for Giardia lamblia. He was then treated with metronidazole, nitazoxanide, and octreotide with control of the diarrhea. However, he remained febrile. An abdominal computed axial tomography study showed hepatosplenomegaly and mild lymphadenopathy. A complete blood count revealed pancytopenia. Additionally, his lactate dehydrogenase level was normal.
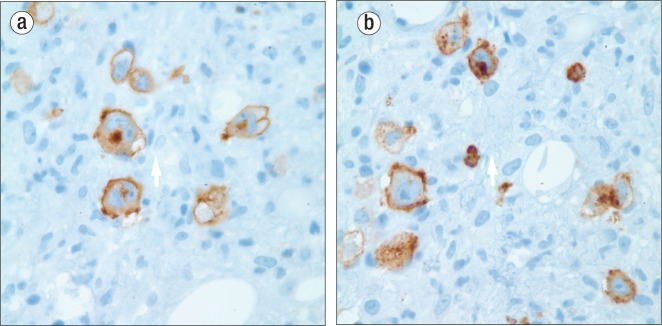
Figure 1.
Peripheral blood showing chronic lymphocytic leukemia (Wright stain ×200).
A bone marrow biopsy showed two small focal areas containing atypical cells suspicious for involvement by Hodgkin lymphoma. There was no evidence of residual CLL/SLL. To establish a definitive diagnosis, an additional bone marrow biopsy was performed a week later and showed several atypical cellular areas containing Reed-Sternberg–like cells (Figure 2). Immunohistochemical stains revealed the large cells to be positive for CD30 and CD15 (Figure 3) and negative for Oct2 and Bob.1. An in situ stain for Epstein-Barr virus was also positive in these cells (Figure 4). These findings supported the diagnosis of Hodgkin lymphoma. There was no morphologic or flow cytometric evidence of residual bone marrow involvement by CLL/SLL. The patient underwent treatment with BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, prednisone, and procarbazine). Unfortunately, he died from his disease in September 2012, about 4.5 months after the diagnosis of Hodgkin lymphoma.
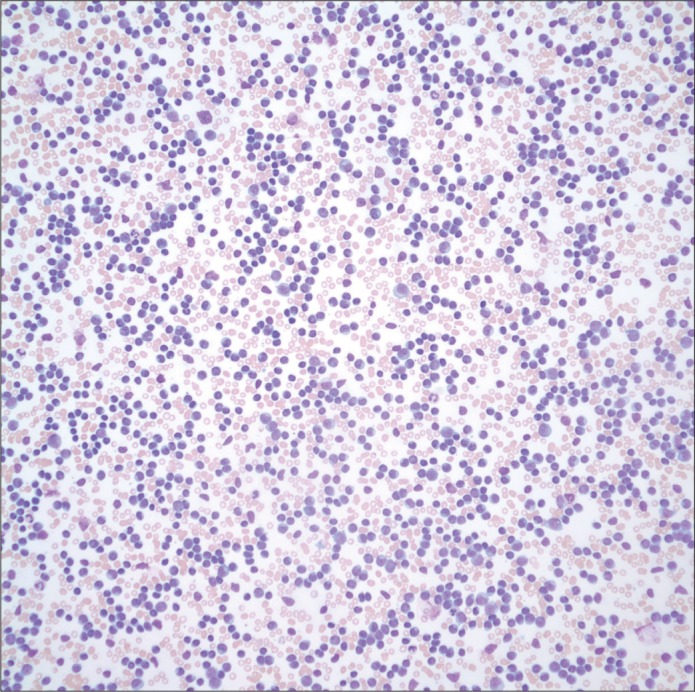
Figure 2.
Bone marrow showing Hodgkin lymphoma. The arrow points to a Hodgkin-Reed Sternberg cell (hematoxylin and eosin, ×400).
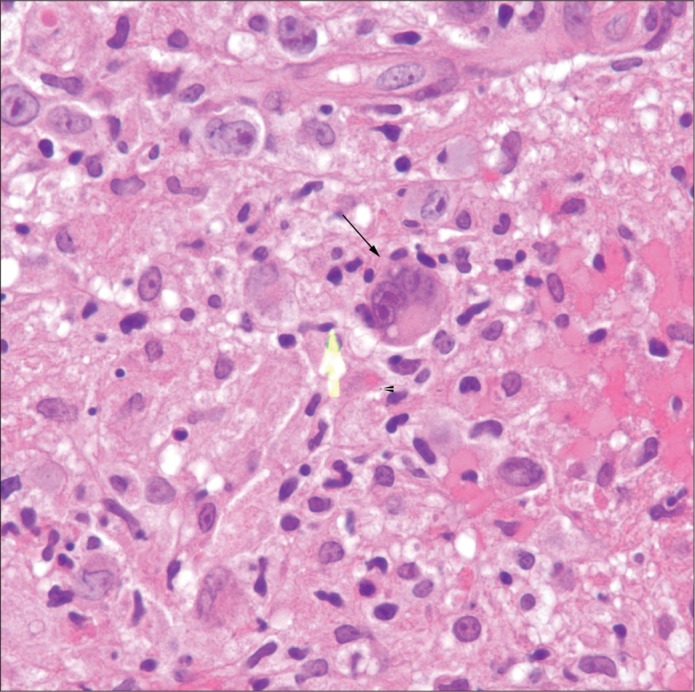
Figure 3.
Positive membranous and Golgi positivity (×1000) shown by (a) CD30 stain and (b) CD15 stain.
Figure 4.
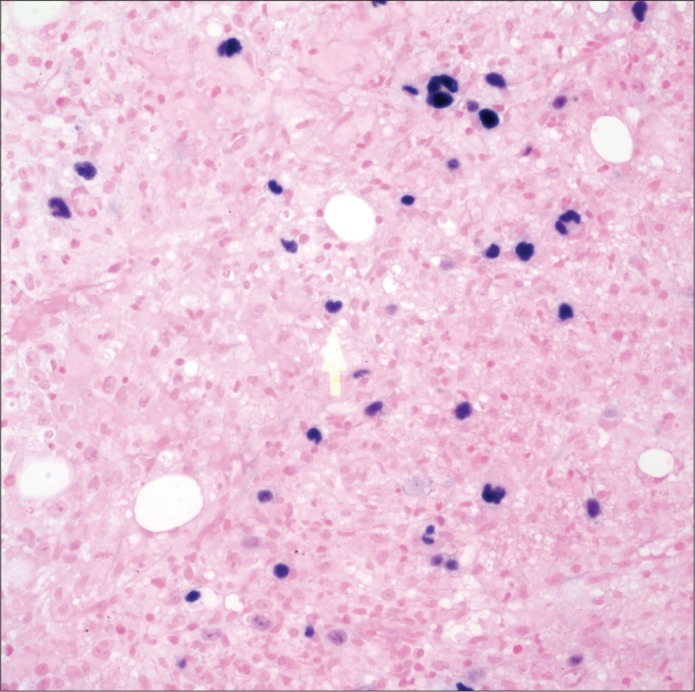
A positive stain by interpreted Epstein-Barr virus–encoded RNA (EBER) in situ hybridization (×1000).
DISCUSSION
The largest series of Hodgkin transformation in CLL/SLL has been reported from M. D. Anderson Cancer Center (3). Among their series of 4121 patients with CLL/SLL, only 18 patients (0.4%) transformed to Hodgkin lymphoma. Only a handful of other cases of Hodgkin transformation of CLL/SLL have been reported (3–10). Two types of Hodgkin transformation of CLL/SLL have been described. Type 1 is characterized by Hodgkin-Reed Sternberg (H-RS) cells scattered in a background of CLL cells (6, 11). In the type 2 transformation, H-RS cells are present in a typical polymorphous, inflammatory background separate from CLL cells (9–11). Our case fits the type 2 pattern. In the type 1 transformation, histologic and immunophenotypic findings suggest that the H-RS cells represent histologic progression of the underlying CLL cells, especially when the H-RS cells express B cell markers (12). Although in the type 2 transformation, two different disease types are considered to be present, the two lesions may be related. It is unknown whether the two types of Hodgkin transformation in CLL/SLL are associated with distinct clinical and prognostic features. The H-RS cells and the CLL cells seem to have a clonal relationship using single-cell polymerase chain reaction analysis and DNA sequencing (12).
In the M. D. Anderson series, the median overall survival was 0.8 years (range 0.03–6.7+). The median failure-free survival duration was 0.4 years. Fourteen of the 18 patients were treated with chemotherapy. Nine patients received Hodgkin lymphoma–type therapy, including five patients who received ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine), three patients who received CVPP (cyclophosphamide, vinblastine, procarbazine, and prednisone), and one patient who received CVPP/ABVD. Five other patients received other cytotoxic regimens with or without rituximab. All patients died from disease recurrence or progressive disease without responding to therapy. Most of the other papers report an equally poor response. Although the number of patients in the M. D. Anderson series was small (although it is still the largest series reported), the authors suggested that newer, more effective intensified combined-modality regimens may be more effective.
One paper reported a partially successful treatment (5). This patient was treated with lomustine, mitoxantrone, and vinblastine and achieved a complete response but relapsed and died 2 years and 2 months after the diagnosis of Hodgkin disease. Another short correspondence from 2000 described three cases of patients with CLL who subsequently developed Hodgkin disease and had a good response with complete remission (13). Two patients were treated with intensive chemotherapy (Stanford V regimen) followed by radiotherapy, and one patient received three courses of MOPP (mechlor-ethamine, vincristine, procarbazine, prednisone)/ABVD (14). The authors also stated that such an outcome was rare. One piece of information that is not consistently available in the papers is the stage of Hodgkin lymphoma at the time of diagnosis, which may have some influence on the outcome. Our case was stage IV. An association with Epstein-Barr virus (also present in our case) has been noted; it is important to determine whether this virus is present and, if so, antiviral therapy might be incorporated in combination with chemotherapy (6, 14).
Although Hodgkin lymphoma transformation is infrequent in CLL/SLL, the prognosis is unfavorable. It will be important to evaluate any newer innovative regimens developed for Hodgkin lymphoma.
References
- 1.Richter MN. Generalized reticular cell sarcoma of lymph nodes associated with lymphatic leukemia. Am J Pathol. 1928;4(4):285–292. [PMC free article] [PubMed] [Google Scholar]
- 2.Harousseau JL, Flandrin G, Tricot G, Brouet JC, Seligmann M, Bernard J. Malignant lymphoma supervening in chronic lymphocytic leukemia and related disorders. Richter's syndrome: a study of 25 cases. Cancer. 1981;48(6):1302–1308. doi: 10.1002/1097-0142(19810915)48:6<1302::aid-cncr2820480609>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 3.Tsimberidou AM, O'Brien S, Kantarjian HM, Koller C, Hagemeister FB, Fayad L, Lerner S, Bueso-Ramos CE, Keating MJ. Hodgkin transformation of chronic lymphocytic leukemia: the M. D. Anderson Cancer Center experience. Cancer. 2006;107(6):1294–1302. doi: 10.1002/cncr.22121. [DOI] [PubMed] [Google Scholar]
- 4.Reddy N, Thompson-Arildsen MA. Hodgkin's lymphoma: Richter's transformation of chronic lymphocytic leukemia involving the liver. J Clin Oncol. 2010;28(29):e543–e544. doi: 10.1200/JCO.2010.29.3050. [DOI] [PubMed] [Google Scholar]
- 5.Adiga GU, Abebe L, Wiernik PH. Partially successful treatment of a patient with chronic lymphocytic leukemia and Hodgkin's disease: case report and literature review. Am J Hematol. 2003;72(4):267–273. doi: 10.1002/ajh.10300. [DOI] [PubMed] [Google Scholar]
- 6.Momose H, Jaffe ES, Shin SS, Chen YY, Weiss LM. Chronic lymphocytic leukemia/small lymphocytic lymphoma with Reed-Sternberg-like cells and possible transformation to Hodgkin's disease. Mediation by Epstein-Barr virus. Am J Surg Pathol. 1992;16(9):859–867. doi: 10.1097/00000478-199209000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Fayad L, Robertson LE, O'Brien S, Manning JT, Wright S, Hagemeister F, Cabanillas F, Keating MJ. Hodgkin's disease variant of Richter's syndrome: experience at a single institution. Leuk Lymphoma. 1996;23(3-4):333–337. doi: 10.3109/10428199609054836. [DOI] [PubMed] [Google Scholar]
- 8.Butts C, Drouin J, Taylor R, McLeish W. Hodgkin's disease in CLL. Am J Hematol. 1995;48(2):134–135. doi: 10.1002/ajh.2830480220. [DOI] [PubMed] [Google Scholar]
- 9.Weisenberg E, Anastasi J, Adeyanju M, Variakojis D, Vardiman JW. Hodgkin's disease associated with chronic lymphocytic leukemia. Eight additional cases, including two of the nodular lymphocyte predominant type. Am J Clin Pathol. 1995;103(4):479–484. doi: 10.1093/ajcp/103.4.479. [DOI] [PubMed] [Google Scholar]
- 10.Choi H, Keller RH. Coexistence of chronic lymphocytic leukemia and Hodgkin's disease. Cancer. 1981;48(1):48–57. doi: 10.1002/1097-0142(19810701)48:1<48::aid-cncr2820480112>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 11.Williams J, Schned A, Cotelingam JD, Jaffe ES. Chronic lymphocytic leukemia with coexistent Hodgkin's disease. Implications for the origin of the Reed-Sternberg cell. Am J Surg Pathol. 1991;15(1):33–42. doi: 10.1097/00000478-199101000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Ohno T, Smir BN, Weisenburger DD, Gascoyne RD, Hinrichs SD, Chan WC. Origin of the Hodgkin/Reed-Sternberg cells in chronic lymphocytic leukemia with “Hodgkin's transformation.”. Blood. 1998;91(5):1757–1761. [PubMed] [Google Scholar]
- 13.Serratrice De Roux C, Coso D, Bouabdallah R, Serratrice J, Disdier P, Weiller PJ. Chronic lymphocytic leukemia and Hodgkin's disease. Clinicopathologic study of three cases with good prognosis. Haematologica. 2000;85(8):878–879. [PubMed] [Google Scholar]
- 14.Rubin D, Hudnall SD, Aisenberg A, Jacobson JO, Harris NL. Richter's transformation of chronic lymphocytic leukemia with Hodgkin's-like cells is associated with Epstein-Barr virus infection. Mod Pathol. 1994;7(1):91–98. [PubMed] [Google Scholar]