Abstract
Fibromatosis arising from the breast, also referred to as desmoid tumor, aggressive fibromatosis, or low-grade fibrosarcoma, is a rare benign entity, accounting for only 0.2% of all breast tumors. Associations with familial multicentric fibromatosis and trauma, including that resulting from surgical intervention, have been reported. Awareness of this lesion is important, as the diagnosis has often been confused with that of breast carcinoma. We present the case of a 30-year-old white woman who presented with a palpable mass within the medial portion of her right breast. She reported breast carcinoma in both her paternal grandmother and maternal aunt. Subsequent mammographic and sonographic evaluation demonstrated an irregular solid mass within the posteromedial portion of the right breast. Ultrasound-guided core needle biopsy revealed low-grade myofibroblastic proliferation consistent with breast fibromatosis. The lesion was surgically resected via wide local excision. Follow-up mammograms performed 1 and 2 years after resection demonstrated no radiographic evidence of recurrence.
CASE REPORT
A 30-year-old white woman presented to Baylor University Medical Center at Dallas (BUMC) with a palpable mass in the medial portion of her right breast. Past medical history disclosed migraine headaches. Breast carcinoma had occurred in her paternal grandmother at age 58 and maternal aunt at age 52. She reported the onset of menarche at age 11 and had never been pregnant.
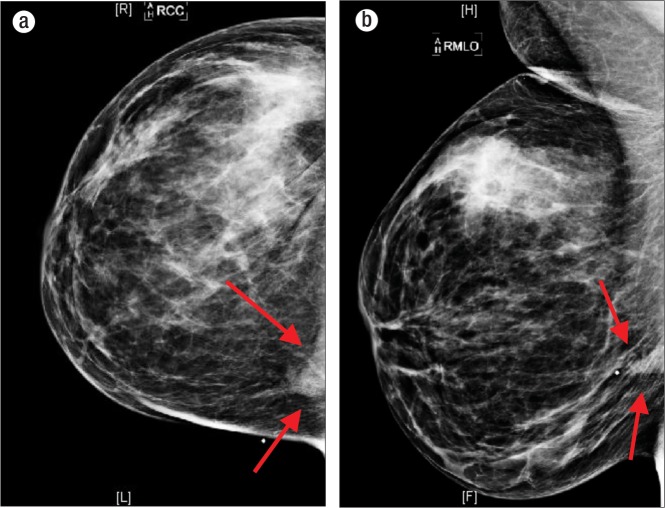
Bilateral diagnostic mammogram at BUMC demonstrated an ill-defined 2-cm mass at the 3 o'clock position at the palpable area of concern within the right breast. Associated distortion and tenting of the underlying pectoralis muscle were also noted (Figures 1 and 2). Subsequent sonographic evaluation of the right breast demonstrated a 1.9 × 1.6 cm irregular hypoechoic lesion extending to the pectoralis muscle at the 3 o'clock position of the right breast, 9 cm from the nipple (Figure 3).
Figure 1.
Routine (a) craniocaudal view and (b) mediolateral oblique view of the right breast demonstrate an ill-defined 2-cm mass (arrows) at the 3 o'clock position posteriorly at the palpable area of concern, as designated by a metallic marker.
Figure 2.
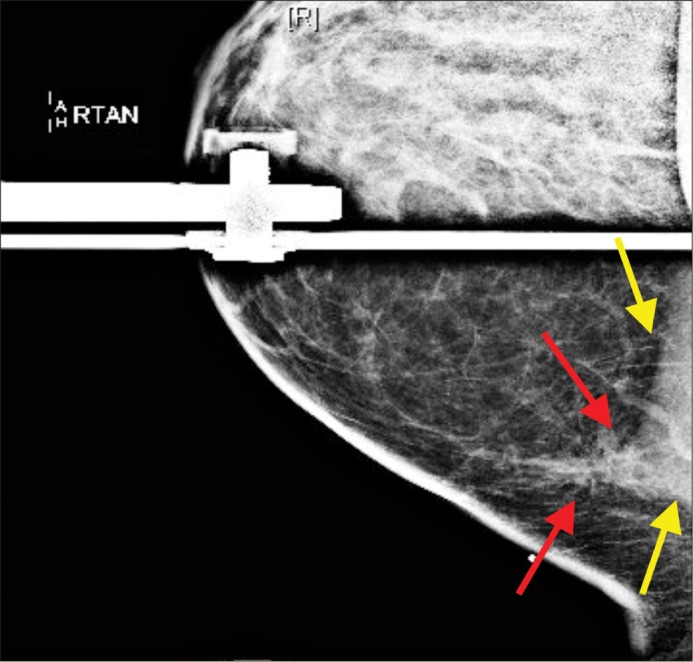
Spot tangential view over the patient's palpable area of concern demonstrates persistence of a 2-cm mass (red arrows), with associated distortion and tenting of the underlying pectoralis muscle (yellow arrows).
Figure 3.
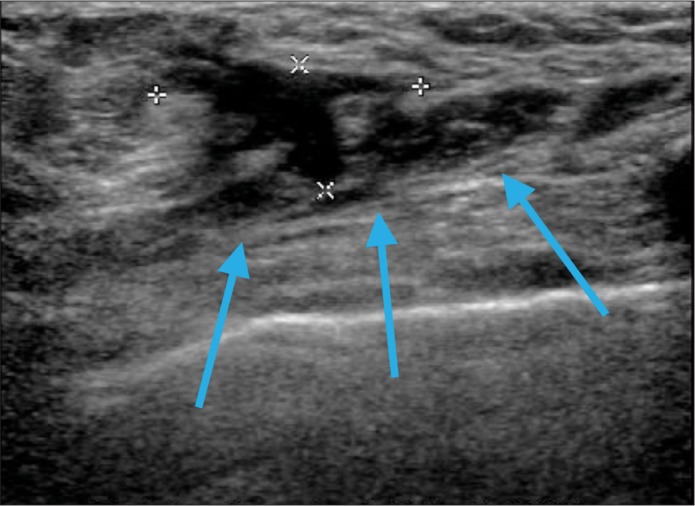
Single sonographic view of the right breast within the palpable area of concern at the 3 o'clock position, 9 cm from the nipple, demonstrates a 1.9 × 1.6 cm irregular hypoechoic lesion extending to the pectoralis muscle (arrows).
The patient underwent a sonographic-guided core needle biopsy of the lesion, which demonstrated a low-grade myofibroblastic proliferation consistent with breast fibromatosis (Figure 4). The patient subsequently underwent wide local excision of the lesion from the right breast and subsequent bilateral mammoplasty. Follow-up mammograms performed at 1 and 2 years following the excision demonstrated no evidence of lesion recurrence.
Figure 4.
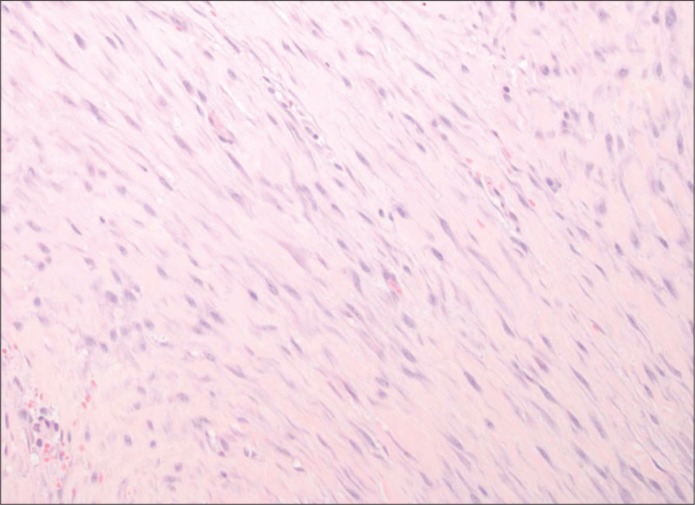
Photomicrograph from the right breast lumpectomy specimen demonstrates low-grade myofibroblastic proliferation, consistent with fibromatosis.
DISCUSSION
Fibromatosis arising from the breast, also referred to as desmoid tumor, low-grade fibrosarcoma, or aggressive fibromatosis, is a rare benign entity characterized histologically by low-grade spindle cell proliferations composed of interlacing fibroblastic bundles and fascicles with varying degrees of collagen. The lesions are noted to have irregular, finger-like margins, with spindle cells infiltrating and surrounding normal breast parenchyma. Grossly, the lesion appears as a rubbery, poorly vascularized grayish-white mass (1–3). Although cellular atypia may be present, the spindle cells are typically uniform with a low mitotic index (1, 4). The histopathologic differential diagnosis includes scar formation, fibrosarcoma, and fibromatosis-like metaplastic spindle cell tumor (4).
Fibromatosis is a benign entity without metastatic potential but carries a significant risk for local recurrence (5). It accounts for only 0.2% of all breast tumors and 0.3% of all solid tumors (4). The calculated lesion occurrence at BUMC is also 0.2% of all breast tumors. Between January 1, 2009, and March 31, 2011, there were four documented cases of breast fibromatosis among the 2174 breast tumors biopsied. The patients ranged in age from 13 to 83 years. Most cases occurred in young, premenopausal women, but cases have also been reported in men (3, 4, 6).
The etiology of this lesion is not well understood, but an association with Gardner's syndrome was initially delineated in 1964 in the first reported case of breast fibromatosis (3, 7). Since then, few cases of breast fibromatosis have been associated with Gardner's syndrome. Additional associations include familial multicentric fibromatosis, silicone and saline breast implants, and incidental and surgical trauma (1, 4).
Although some reports have suggested an association with sex steroid hormones, a 2000 study by Devouassoux-Shisheboran et al refuted this association. Of the 33 reported cases of breast fibromatosis in their study, only one case demonstrated estrogen receptor (ER) and progesterone receptor (PR) positivity within a tumor localized to the chest wall (8). Similarly, a case study performed by Reis-Filho et al assessed the immunohistochemical expression of ER and PR in one patient who developed simultaneous mammary fibromatosis and abdominal fibromatosis. While cells from the abdominal desmoid tumor specimen demonstrated immunoreactivity for both receptors, the cells from the primary breast tumor were deemed negative (9).
Clinically, desmoid tumors of the breast present as firm, painless, movable masses, and skin retraction and/or dimpling may be present. Nipple retraction is often seen in tumors that are close to the nipple. Nipple discharge and palpable lymphadenopathy are not associated with breast fibromatosis. Desmoid tumors are often irregularly shaped, high-density lesions with spiculated margins that closely mimic breast carcinoma on mammography. Rarely do these tumors demonstrate calcific deposition. Sonographically, breast fibromatosis presents as a poorly defined, hypoechoic mass with posterior acoustic shadowing and an echogenic rim, findings that make it indistinguishable from breast cancer (3–5, 10). Desmoid tumors are heterogeneous on magnetic resonance imaging and may be hypointense to isointense on T1-weighted images and hypointense to hyperintense on T2-weighted images. Moderate to strong enhancement is noted following the administration of intravenous contrast (10, 11). Mutations of alterations in the adenomatous polyposis coli and beta-catenin pathway are implicated in the development of sporadic and familial adenomatous polyposis–associated breast fibromatosis (4).
Management of desmoid tumors includes wide local surgical excision despite high local recurrence rates ranging from 24% to 77% over the course of 10 years. Radiation therapy is used in patients with unresectable tumors or lesions that would require extensive surgical resection, to include amputation or major chest or abdominal wall resection. Medical therapy for breast fibromatosis includes three major classes of drugs: hormonal agents, antiinflammatory agents, and cytotoxic agents (2).
References
- 1.Greenberg D, McIntyre H, Ramsaroop R, Arthur J, Harman J. Aggressive fibromatosis of the breast: a case report and literature review. Breast J. 2002;8(1):55–57. doi: 10.1046/j.1524-4741.2002.08013.x. [DOI] [PubMed] [Google Scholar]
- 2.Privette A, Fenton SJ, Mone MC, Kennedy AM, Nelson EW. Desmoid tumor: a case of mistaken identity. Breast J. 2005;11(1):60–64. doi: 10.1111/j.1075-122X.2005.21679.x. [DOI] [PubMed] [Google Scholar]
- 3.Schwarz GS, Drotman M, Rosenblatt R, Milner L, Shamonki J, Osborne MP. Fibromatosis of the breast: case report and current concepts in the management of an uncommon lesion. Breast J. 2006;12(1):66–71. doi: 10.1111/j.1075-122X.2006.00187.x. [DOI] [PubMed] [Google Scholar]
- 4.Erguvan-Dogan B, Dempsey PJ, Ayyar G, Gilcrease MZ. Primary desmoid tumor (extraabdominal fibromatosis) of the breast. AJR Am J Roentgenol. 2005;185(2):488–489. doi: 10.2214/ajr.185.2.01850488. [DOI] [PubMed] [Google Scholar]
- 5.Nakazono T, Satoh T, Hamamoto T, Kudo S. Dynamic MRI of fibromatosis of the breast. AJR Am J Roentgenol. 2003;181(6):1718–1719. doi: 10.2214/ajr.181.6.1811718. [DOI] [PubMed] [Google Scholar]
- 6.Goel NB, Knight TE, Pandey S, Riddick-Young M, de Paredes ES, Trivedi A. Fibrous lesions of the breast: imaging-pathologic correlation. Radiographics. 2005;25(6):1547–1559. doi: 10.1148/rg.256045183. [DOI] [PubMed] [Google Scholar]
- 7.Simpson RD, Harrison EG, Jr, Mayo CW. Mesenteric fibromatosis in familial polyposis: a variant of Gardner's syndrome. Cancer. 1964;17:526–534. doi: 10.1002/1097-0142(196404)17:4<526::aid-cncr2820170414>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 8.Devouassoux-Shisheboran M, Schammel MD, Man YG, Tavassoli FA. Fibromatosis of the breast: age-correlated morphofunctional features of 33 cases. Arch Pathol Lab Med. 2000;124(2):276–280. doi: 10.5858/2000-124-0276-FOTB. [DOI] [PubMed] [Google Scholar]
- 9.Reis-Filho JS, Milanezi F, Pope LZ, Fillus-Neto J, Schmitt FC. Primary fibromatosis of the breast in a patient with multiple desmoid tumors—report of a case with evaluation of estrogen and progesterone receptors. Pathol Res Pract. 2001;197(11):775–779. doi: 10.1078/0344-0338-00158. [DOI] [PubMed] [Google Scholar]
- 10.Cardenosa G. Clinical Breast Imaging: A Patient-Focused Teaching File. Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 297–299. [Google Scholar]
- 11.Mesurolle B, Leconte I, Fellah L, Feger C, Nakazono T, Kudo S. Dynamic breast MRI in recurrent fibromatosis. AJR Am J Roentgenol. 2005;184(2):696–697. doi: 10.2214/ajr.184.2.01840696. [DOI] [PubMed] [Google Scholar]