Abstract
Background
Surgical Site Infections (SSI) is the third most commonly reported nosocomial infection which has an adverse impact on the hospital as well as on the patient. A continuous surveillance is called for, to keep a check on the occurrence of SSI.
Objectives
to study the incidence of SSI in our hospital.
to study the risk factors of SSI in our hospital.
to identify the areas in our hospital, which need to be strengthened and dealt with proactive measures to curb the incidence of SSI, which is an indicator of health care system in a given set up.
Methodology
We conducted a one year study of SSI in our hospital. 300 cases of Surgery and Obstetrics and Gynaecology were included in the study. A few host factors, wound factors and surgery related factors that cause SSI were studied. Swabs were collected from the infected surgical wounds and processed by the conventional microbiological methods. Antimicrobial susceptibility was done by Kirby-Bauer disc diffusion method.
Results
Prolonged surgery (>2hours) and insertion of drain were found to be significantly associated with occurrence of SSI and the clean surgeries showed minimum risk of infection. Escherichia coli (31.25%) was the commonest pathogen, followed by Pseudomonas aeruginosa (25 %) and Staphylococcus aureus 22%. The incidence of SSI in our set up is 6%.
Conclusions
The outcome of the SSI surveillance in our hospital revealed that in order to decrease the incidence of SSI we would have to: a) decrease the duration of the surgeries performed b) focus on regular and intensive drain care c) identify poor risk patients and ensure their proper management d) conduct periodic surveillance to keep a check on SSI.
Keywords: SSI, incidence, risk factors, clean surgery, pathogen
Introduction
Surgical site infections (SSI) are the third most commonly reported nosocomial infection and they account for approximately a quarter of all nosocomial infections. It has an adverse impact on the hospital as well as on the patient. It is responsible for increasing length of stay of patient which results in social and economic loss to the patients and family. Host factors, wound factors and surgery related factors are implicated in the causation of SSI. (1)
The present study was aimed at obtaining the incidence of SSI in our set up and to evaluate the risk factors as well as to formulate an antibiotic policy for patients posted for any surgery in our hospital.
Background
SSI is the index of the health care system of any hospital. With the increase in incidence of nosocomial infections and multi drug resistance, a meticulous and periodic surveillance of various hospital acquired infections is called for.
With an active Infection Control team operating in the hospital, SSI is naturally one of the topmost priorities on the agenda. Hence the following study was undertaken.
Materials and Methods
The present study was conducted in the Dept. of Microbiology, Padm. Dr D Y Patil Medical College, Pune. 300 operated cases in Surgery and Obstetrics and Gynaecology were included in this study. Certain risk factors like – type of surgical wound, elective or emergency surgery, antibiotic prophylaxis, duration of surgery, presence or absence of drain and any underlying or predisposing conditions were noted. Swabs were obtained from the post operative infected wounds and processed by the conventional microbiological methods. (2) Antimicrobial susceptibility testing was done by Kirby-Bauer disc diffusion method (3) and interpretation was done according to CLSI guidelines. (4)
CDC criteria were used to define the type of surgical wound i.e. Class I- Clean, Class II- Clean contaminated, Class III- Contaminated, Class IV- Dirty.(5) The statistical significance of the relative importance of various parameters affecting SSI has been tested using ‘p’ test at 95% confidence level (p< 0.05).
Results
300 surgical wounds (from General Surgery wards and Obstetrics and Gynaecology wards) were studied over a period of one year.
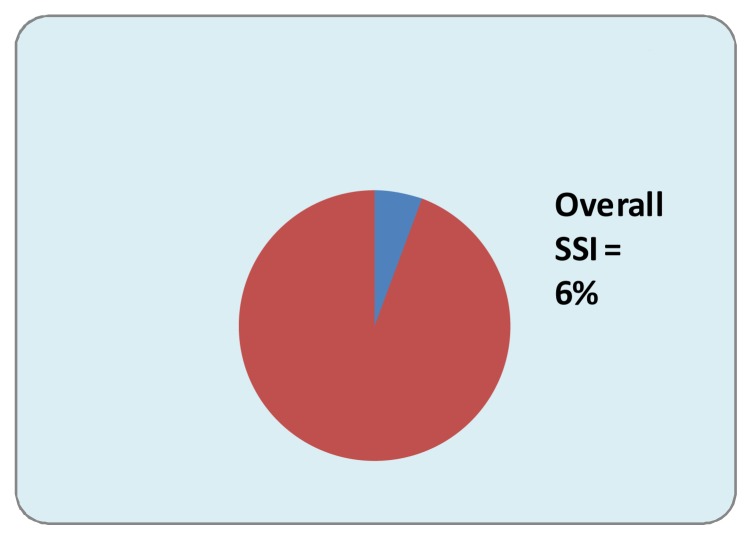
The overall infection rate was 6%.
Discussion
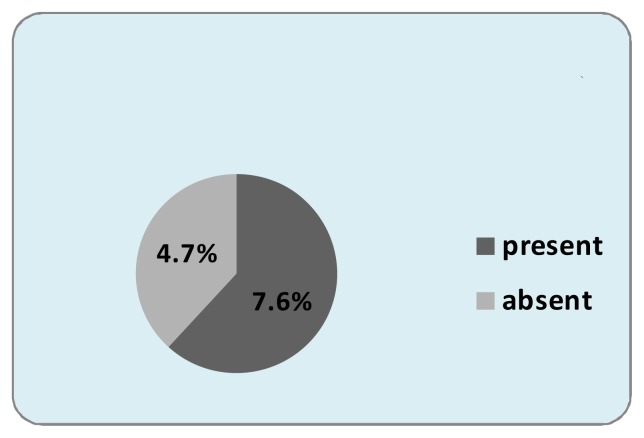
The incidence of SSI in our set up was 6%. (Fig 1) This is in agreement with the SSI incidences in other studies. (6, 7) However, infection rates varying from 20% to as high as 76.9% have also been reported. (8–12)
Fig. 1.
Incidence of SSI at DYPMC and Hospital
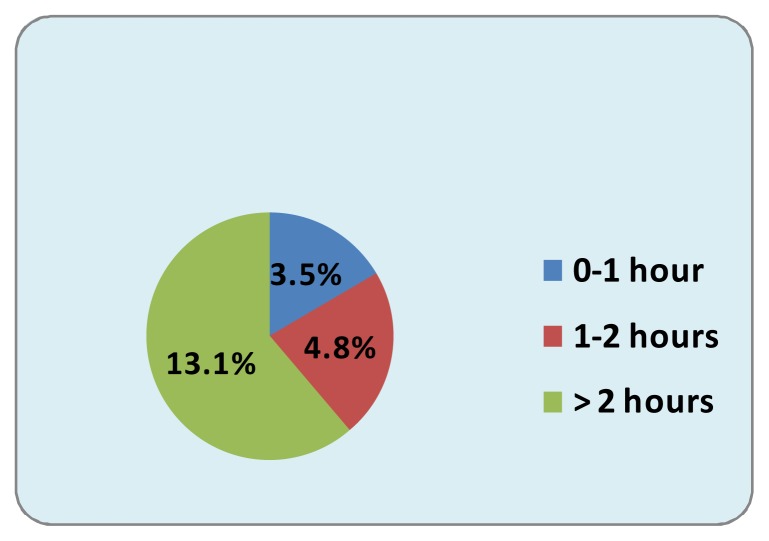
Prolonged duration of operation results in increased exposure of operation site to air, prolonged trauma, stress of prolonged anaesthesia and sometimes blood loss. (13) Our study reveals a clear cut increased number of SSI cases i.e.13.1% cases, where surgery has been prolonged ≥ 2 hours. (Fig 2). Studies conducted on SSI in Aurangabad, (6) Mumbai, (7) Hyderabad, (9) and Orissa (10) have reported a similar observation. In fact, this correlation has been established since 1964 by the Public health laboratory services (PHLS) in England and Wales. (13)
Fig. 2.
Duration of Surgery of SSI cases
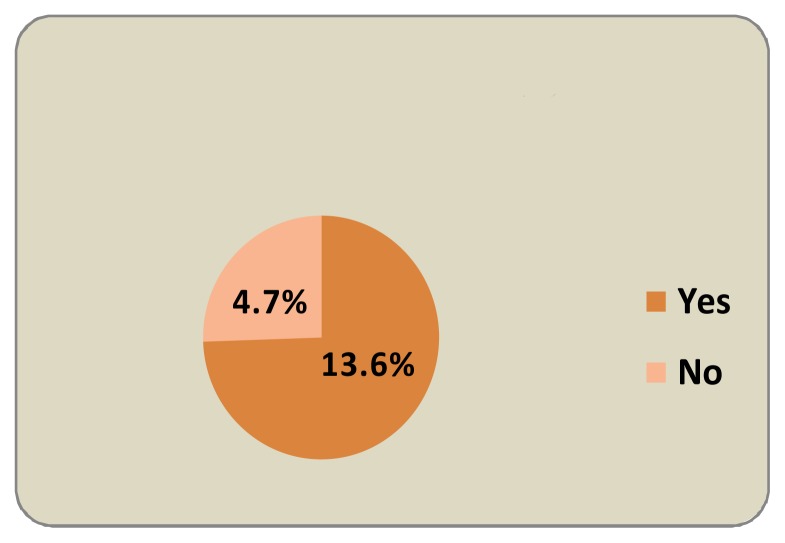
The use of drains has contributed significantly as a risk factor in causing SSI in this study i.e. 13.6% (Fig 3). This could be due to the fact that they are more likely to be used in contaminated or dirty wounds and in emergency and prolonged operations which increases the probability of the wound getting infected.(13) Mumbai (7) has also observed 22.4% cases of drained and 3% undrained wounds getting infected while Aligarh (8) reported 30% and 11.6% respectively.
Fig. 3.
Insertion of Drain in SSI cases
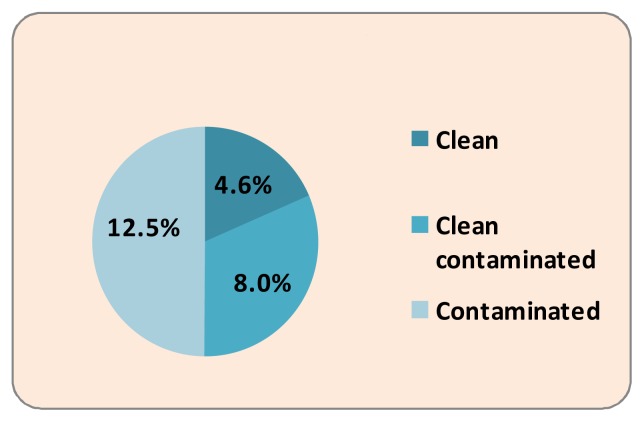
The rate of infection was highest in contaminated type of wounds-12.3%, followed by clean contaminated wounds-8.0% and least in clean wounds-4.6% (Fig 4). This is an expected observation. In Aurangabad, (6) similar rates were noted i.e. percentage of infection rate was 10.6 % and 4% in clean contaminated and clean cases respectively, in Mumbai (7) 22.4% and 3.0% respectively and in England (13) 10.8% and 3.0% respectively. However, in Orissa, (10) the difference between the rate of infection in clean contaminated (25%) and in clean surgeries (30%) was not statistically significant.
Fig. 4.
Type of Surgery in SSI cases
Certain underlying conditions like anaemia, diabetes, and smoking may alter or decrease the immune status thus significantly increasing the risk of SSI. They also are an important cause of increasing the pre operative stay of the patient which steeply increases the risk of SSI in such patients. (13) In our study, 7.6% of patients with SSI had some underlying conditions, anaemia and diabetes mellitus being the commonest (Fig. 5). Each day of extra hospitalization adds to the risk of acquiring SSI and this has been confirmed by studies in Aurangabad, (6) Mumbai, (7) Hyderabad (9) and in Orissa. (10) In Aligarh (8) however, it was noted that diabetes mellitus and dehydration did not contribute to the occurrence of SSI.
Fig. 5.
Predisposing Condition/s in SSI cases
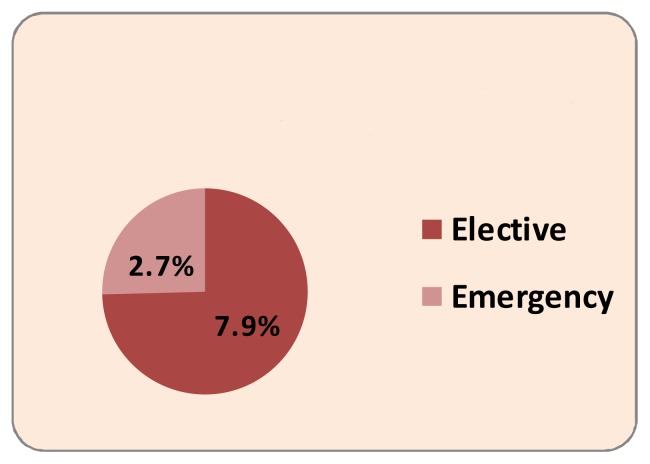
SSI have occurred more in elective surgeries-7.9%, than in emergency surgeries-2.7% (Fig 6). This observation may seem very surprising, as emergency cases have known to land up in SSI more than the elective ones.(10,13–16) However, in our study, there have been more number of elective cases (63%) over the year than emergency cases (37%).
Fig. 6.
Category of Surgery in SSI cases
Also, the presence of underlying conditions like anaemia, diabetes mellitus etc was more in patients who had undergone elective surgery (38%) than in those who had emergency operations done (33%). These two factors could have been responsible for this unexpected outcome. In Aurangabad, (6) the infection rate in emergency surgeries was not statistically higher than in elective surgeries.
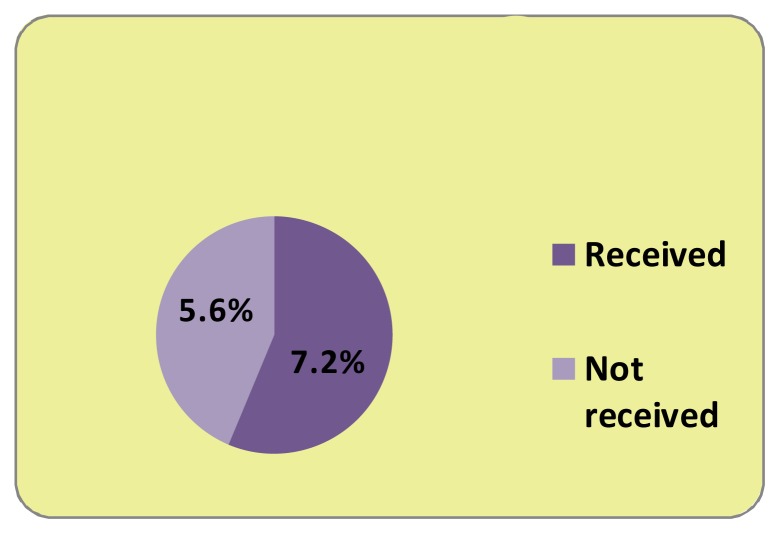
Pre operative antibiotics are known to decrease incidence of SSI cases.(1,6,13) However, prophylactic antimicrobials are more frequently given to patients who are poor risks from the stand point of susceptibility to infection.(13) This could explain our finding of a marginal increase of SSI in patients who have received prophylaxis (7.2%) than those who had not (5.6%) (Fig 7).
Fig. 7.
Preoperative Antibiotics in SSI cases
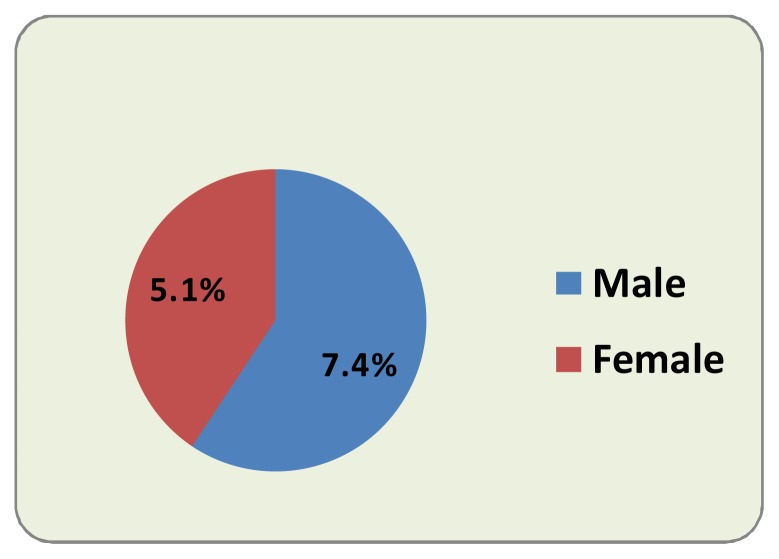
Also, there is a marginal preponderance of male patients developing SSI (7.4%) over female patients with SSI (5.1%) which is not statistically significant (Fig 8). In Aligarh, (8) females (27%) showed preponderance of SSI than males (18%). However, it has been known that sex is not a pre determinant of the risk of SSI. (13)
Fig. 8.
Genderwise SSI
Gram negative bacilli, namely members of enterobacteriaceae, are the predominant pathogens in our setup according to the data provided by the Infection Control Committee of our hospital and our SSI bacteriological profile matched this observation. Of the 18 SSI cases, 4 patients’ swabs yielded no growth (22%) aerobically and anaerobically and showed no organisms on direct smear as well. Mumbai (7) study has also reported 17.6% culture negative SSI cases. The remaining 14 patients’ swabs yielded a total of 16 isolates in our laboratory of which Escherichia coli was 31.25%, Pseudomonas aeruginosa 25% and Staphylococcus aureus was 22%. This trend of gram negative bacilli i.e. enterobacteriaceae dominating the gram positive cocci has been observed in Aurangabad, (6) Orissa (10) and Navi Mumbai (11) also.
Conversely, in some studies (7, 8, 9, 12) Staphylococcus aureus has dominated the scene. Multi drug resistance is a dreaded problem in nosocomial infections. Our study reveals enterobacteriaceae showing highest sensitivity to amikacin (78%) followed by gentamicin (71%). In comparison, very low sensitivity is noted with the cephalosporins and fluoroquinolones (10% and 58% respectively). This could be due to the overuse of these drugs and the high prevalence of extended spectrum beta lactamases (ESBLs) among these organisms. Surprisingly, our Pseudomonas isolates showed good sensitivity to piperacilin-tazobactam, ceftazidime and imipenem (83.5%, 83% and 100% respectively).
Staphylococcus aureus showed maximum sensitivity to linezolid (87.3%), gentamicin (100%), clindamycin (100%) vancomycin (100%).
In other studies, penicillins have shown very poor performance while gentamicin has showed maximum sensitivity (> 90%) against both gram positive cocci as well as gram negative bacilli. (6, 7, 9, 10, 12) Unlike our study, Hyderabad study (9) has shown first generation cephalosporins to be very effective for both.
Similar to our observation, vancomycin and linezolid have shown promise for Staphylococcus aureus in Navi Mumbai (11) too.
To conclude, we have observed that increased duration of surgery (> 2 hours), use of drains, and compromised immunity are responsible for SSI in our set up. Enterobacteriaceae (especially E.coli) and S.aureus are the predominant pathogens showing maximum sensitivity to amikacin and gentamicin.
Conclusion
We can further bring down our SSI rate by implementing the following measures:
○ Efforts to decrease the duration of surgery without compromising the patient’s safety and the beneficial outcome.
○ Regular and intensive drain care
○ A thorough examination and investigations of poor risk patients should be done and accordingly all appropriate care should be taken to enable them to withstand the stress of surgery. Also utmost post operative care and efforts to boost their immunity would help in decreasing further the occurrence of SSI in this group of patients.
○ Periodic surveillance of SSI will guide the Infection Control Committee in laying down strict guidelines to further decrease the SSI incidence in our setup, which is an indicator of health care in a given system.
Undertaking
I, the undersigned, give an undertaking to the following effect with regard to our article entitled “Surgical Site Infections: A one year prospective study in a tertiary care center” submitted for publication in International Journal of Health Sciences.
The article mentioned above is original and has not been published or submitted to or accepted for publication in any form, in any other journal and does not infringe any existing copyright or any other third party rights.
We also vouchsafe that the authorship of this article will not be contested by anyone whose name(s) is/are not listed by us here. Conflict of interests is none.
I am authorized by my co-authors to enter into these arrangements.
The article contains nothing that is unlawful, libelous, or which would, if published, constitute a breach of contract or of confidence or of commitment given to secrecy;
Due care to ensure the integrity of the article has been taken.
Dr. Varsha D.Shahane (Corresponding and main author)
References
- 1.Wong ES. Surgical site infections. In: Mayhall CG, editor. Hospital epidemiology and infection control. 1st ed. USA: Williams and Wilkins; 1996. pp. 154–74. [Google Scholar]
- 2.Koneman EW, Allen SD, Janda WM, Schreckenberger PC, Winn WC Jr, editors. Color Atlas and Textbook of Diagnostic Microbiology. 5th Ed. Lipincott-Raven Publishers; Philadelhia: Pa: 1997. [Google Scholar]
- 3.Bauer AW, Kirby WM, Sherris JC, Turck M. Antibiotic susceptibility testing by a standard single disc method. Am J Clin Pathol. 1966;45:493–6. [PubMed] [Google Scholar]
- 4.Clinical and Laboratory Standards Institute (CLSI) Performance standards for antimicrobial susceptibility testing 17th informational supplement. 2007. pp. M100–S17. [Google Scholar]
- 5.Center for Disease Control. National Nosocomial Infections Study Quarterly Report, First and Second Quarters. Altlanta: CDC; 1973. Jul, 1974. [Google Scholar]
- 6.Anvikar AR, Deshmukh AB, Karyakarte RP, Damle AS, Patwardhan NS, Malik AK, et al. A one year prospective study of 3280 surgical wounds. Indian J Medical Microbiol. 1999;17(3):129–32. [Google Scholar]
- 7.Lilani SP, Jangale N, Chowdhary A, Daver GB. Surgical site infection in clean and clean-contaminated cases. Indian J Medical Microbiol. 2005;23(4):249–52. [PubMed] [Google Scholar]
- 8.Khan MA, Ansari MN, Bano S. Post operative wound infection. Ind. J. Surg. 1985;48:383–86. [Google Scholar]
- 9.Rao AS, Harsha M. Postoperative wound infections. J. Indian M.A. 1975;64(4):90–3. [PubMed] [Google Scholar]
- 10.Tripathy BS, Roy N. Post-operative wound sepsis. Ind. J. Surg. 1984;47:285–8. [Google Scholar]
- 11.Kamath N, Swaminathan R, Sonawane J, Bharos N. Bacteriological profile of surgical site infections in a tertiary care center in Navi Mumbai [abstract]. Proceedings of the 16th Maharashtra Chapter Conference of IAMM; 2010 Sept 24–26; Karad, Maharashtra. p. 61. [Google Scholar]
- 12.Prabhakar H, Arora S. A bacteriological study of wound infections. J Indian Med Assoc. 1979;73(9&10):145–8. [PubMed] [Google Scholar]
- 13.Berard F, Gandon J. Factors influencing the incidence of wound infection. Ann Surg. 1964;160:32–81. [PMC free article] [PubMed] [Google Scholar]
- 14.Cruse PJE. Surgical wound infection. In: Gorbach SL, Bartlett JG, Blacklow NR, editors. Infectious diseases. W.B. Saunders Company, Harcourt Brace Jovanovich Inc; Philadephia. London, Toronto, Montreal, Sydney. Tokyo: 1992. pp. 738–64. [Google Scholar]
- 15.Beck WC, Deshmukh N. Surgical infections. In: Groschel D, editor. Handbook on Hospital Associated Infections in the General Hospital population and specific measures of control. Marcel Dekker, Inc; New York, Basel: 1979. pp. 1–24. [Google Scholar]
- 16.Cruse PJE, Ford R. A five year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206–9. doi: 10.1001/archsurg.1973.01350200078018. [DOI] [PubMed] [Google Scholar]