Abstract
Objectives:
Most of the morbidity and mortality in human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) result from opportunistic infections (OIs). Although the spectrum of OIs in HIV infected patients from developing countries has been reported, there is a paucity of data on the natural history, pattern of disease, and survival of hospitalised patients with HIV/AIDS, particularly in Arab countries. The aim of this study was to study retrospectively the spectrum and frequency of various OIs in a cohort of hospitalised HIV-infected Omani patients.
Methods:
Included in the study were 77 HIV-infected Omani patients admitted to a tertiary care teaching hospital in Muscat, Oman, between January 1999 and December 2008. They were diagnosed on their first admission and hence were not on highly active antiretroviral therapy (HAART) at presentation. The frequency of various clinical and laboratory findings and individual OIs were analysed.
Results:
In total, 45 patients (58%) had one or more AIDS-defining OIs. Pneumocystis jiroveci pneumonia (PCP) was commonest (25%), followed by cryptococcal meningitis (22%), cytomegalovirus (CMV), retinitis (17%), disseminated tuberculosis (15%), and cerebral toxoplasmosis (12.5%). Only one patient with Mycobacterium avium-intracellulare (MAI) was identified and one patient had disseminated visceral leishmaniasis. The majority of patients (77%) had CD4+ counts <200 cells/μL. Ten patients (22%) died during hospital stays, with five deaths (50%) being caused by disseminated CMV infection.
Conclusion:
A wide spectrum of OIs is seen in hospitalised HIV-infected patients in Oman. P. jiroveci pneumonia and cryptococcal meningitis were the commonest OIs, while disseminated CMV was the commonest cause of death. We hope these results will advance the knowledge of specialists treating HIV in Oman and the Gulf region.
Keywords: HIV, AIDS, Opportunistic infections, Oman
Advances in Knowledge
- This study provides a scientific account of the epidemiology of AIDS defining opportunistic infections (OIs) and their burden on Omani HIV-infected patients.
Application to Patient Care
- This study provides guidance for developing local guidelines on prophylaxis and management of these infections.
- The results can be used to guide the HIV/AIDS programme in Oman on future directions in HIV care and how to address the issues relating to late diagnoses.
- Recommendations for primary prophylaxis for AIDS-defining OIs can be made on the basis of these findings, which may be different from those used in industrialised countries.
The emergence and pandemic spread of human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) constitutes the greatest health challenge in modern times. According to estimates by the World Health Organization and the Joint United Nations Programme on HIV/AIDS (UNAIDS), 34 million people were living with HIV at the end of 2010. That same year, some 2.7 million people became newly infected, and 1.8 million died of AIDS.1
Infections associated with severe immunodeficiency are known as opportunistic infections (OIs) because they take advantage of a weakened immune system. Some of these OIs are used to mark the stages of HIV/AIDS.2 Before the widespread use of potent combination antiretroviral therapy (ART), OIs were the principal cause of morbidity and mortality in HIV-infected patients worldwide. In one study, the mortality rate among individuals with a history of preventable OIs was 66.7 per 100 people per year compared with 2.3 per 100 people per year for those without a history of preventable OIs.3
The first case of HIV/AIDS in Oman was reported in 1984.4 As of 31st December 2009, 1,119 Omanis were living with HIV/AIDS with more than 50% of them between 15 and 35 years of age. Around 100 new cases of HIV/AIDS are diagnosed annually in Oman.5 During 2009, 116 new cases of HIV infection were reported by the Ministry of Health in Oman, which makes it the highest annual number reported since 1995.5
Many organisms responsible for OIs in patients with HIV/AIDS have similar clinical presentation and the type of pathogen responsible for morbidity and mortality can vary from region to region. The identification of such pathogens in Oman is essential for clinicians providing care for these patients. Hence, the present retrospective study was performed to evaluate the spectrum of various OIs and determine their relative frequencies in a cohort of hospitalised HIV-infected Omani patients.
Methods
This was a retrospective chart review study. A total of 77 Omani patients with HIV/AIDS who were admitted to Sultan Qaboos University (SQU) Hospital, Muscat, Oman, between January 1999 and December 2008 were investigated for a variety of AIDS-defining OIs at the time of their HIV diagnosis. All patients were diagnosed on their first admission and hence were not on highly active antiretroviral therapy (HAART) at presentation. Appropriate clinical samples, including sputum, bronchoalveolar lavage (BAL), cerebrospinal fluid (CSF), and bone marrow aspirates, as indicated by the clinical presentation, were collected. Computed tomography (CT) and magnetic resonance imaging (MRI) scans of the brain, and high resolution CT chest scans were performed as per symptoms and clinical presentations. The following criteria were used to define an OI concern. In the case of cryptococcal meningitis, OI was defined by the demonstration of Cryptococcus sp. yeast cells in the CSF by India ink staining, antigen presence by latex agglutination, or growth of cells in a culture. In the case of cerebral toxoplasmosis, OI was defined by the demonstration of multiple ring-enhancing cerebral parenchymal lesions on contrast-enhanced CT or MRI scans in the presence of anti-toxoplasma antibody in serum and clinical response to anti-toxoplasma therapy. In the case of Pneumocystis jiroveci pneumonia (PCP), OI was proven through bilateral, diffuse, interstitial infiltrates on chest radiograph or high-resolution CT, with hypoxaemia (PaO2 <12 kPa) and/or demonstration of P. jiroveci in induced sputum. In the case of disseminated tuberculosis, OI was defined by clinical features suggestive of tuberculosis (TB) with concurrent involvement of at least two non-contiguous organs, in the presence of bacteriological and/or histopathological evidence of TB and improvement with anti-tuberculosis therapy. Entry and analysis of all available data were performed using the Statistical Package for the Social Sciences (SPSS), Version 16.0, (IBM, Chicago, IL, USA). Entered data were double-checked for discrepancies. The frequency of various clinical and laboratory findings and the frequencies of individual OIs are expressed as percentages.
Ethical approval was obtained from the SQU Ethics and Research Committee before starting this study. Patients’ consent was not required as the study was retrospective.
Results
A total of 77 HIV-positive Omani patients were included. Their demographic data is presented in Table 1. Of those participating in the study, 45 patients (58%) (38 ± 12 years, males = 62%) presented with one or more AIDS-defining OIs. In these patients, 72 episodes of AIDS-defining OIs were diagnosed (1.6 OI episodes/patient). During the same hospitalisation period, 24 patients (53%) presented with two or more AIDS-defining OIs. Of the patients who presented with one or more OI, 73% were male. As shown in Table 2, PCP was the commonest AIDS-defining OI (25%), followed by cryptococcal meningitis (22%), invasive CMV disease/retinitis (17%), disseminated TB (15%), and cerebral toxoplasmosis (12.5%). Only one patient suffered infection with Mycobacterium avium-intracellulare (MAI). Cryptosporidiosis, microsporidiosis, and invasive Candida infections presented in 3%, 1.5% and 1.5% of cases, respectively. In addition, one patient had disseminated visceral leishmaniasis.
Table 1:
Demographic characteristics of HIV-infected patients
| Total number of patients | 77 |
| Age in years, mean (range) | 37.5 (13–66) |
| Male gender, number (%) | 48 (62%) |
| CD4 at diagnosis of HIV infection, mean (range) | 167 cells/mm3 (1 cell/mm3–1200 cells/mm3 |
| Viral load at diagnosis of HIV infection, mean (range) | 330,000 RNA copies/ml (60 RNA copies/ml–5,000,000 RNA copies/ml) |
RNA = ribonucleic acid; HIV = human immunodeficiency virus
Table 2:
AIDS-defining opportunistic infections (OIs) and their frequencies
| AIDS-defining OI | Number of OI events | % out of all OI events |
|---|---|---|
| PCP | 18 | 25 |
| Cryptococcal meningitis | 16 | 22 |
| CMV (retinitis/disseminated) | 12 | 17 |
| Tuberculosis (disseminated) | 11 | 15 |
| Toxoplasmosis (cerebral) | 9 | 12.5 |
| Cryptosporidiosis | 2 | 3 |
| Microsporidiosis | 1 | 1.5 |
| Candidiasis (invasive/gastrointestinal) | 1 | 1.5 |
| MAI | 1 | 1.5 |
| Leishmaniasis (visceral/disseminated) | 1 | 1.5 |
| Total | 72 | 100 |
AIDS = acquired immune deficiency syndrome; OI = opportunistic infection; PCP = Pneumocystis jiroveci pneumonia ; CMV = cytomegalovirus; MAI = Mycobacterium avium-intracellulare.
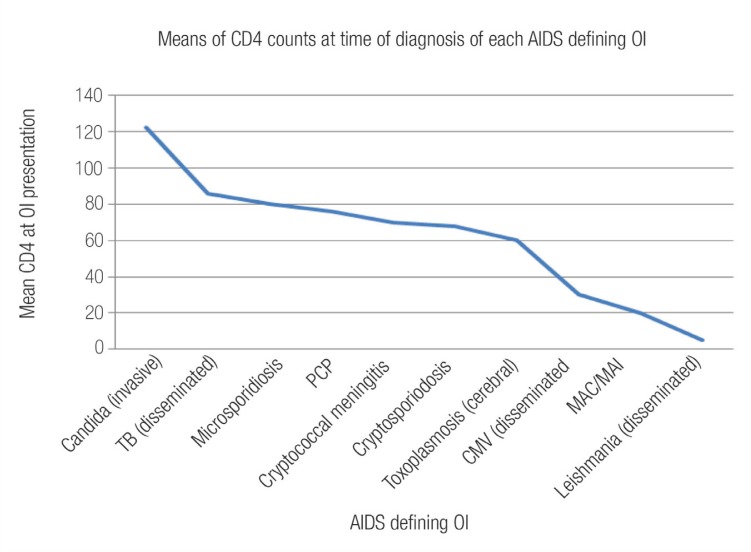
CD4+ cell counts were performed in all 77 patients. The majority of patients (77%) had CD4+ counts of <200 cells/μL at their initial presentation to the hospital. The mean CD4+ cell count was 72 cells/μL in those with AIDS-defining OIs versus 301 cells/μL in the group not suffering from an AIDS-defining OI. Figure 1 shows mean CD4+ cell counts at the time of diagnosis of each AIDS-defining OI.
Figure 1:
Mean CD4 counts at time of diagnosis of each AIDS-defining OI.
AIDS = acquired immune deficiency syndrome; OI = opportunistic infection; TB = tuberculosis; PCP = Pneumocystis jiroveci pneumonia; CMV = cytomegalovirus; MAC/MAI = Mycobacterium avium complex/Mycobacterium avium-intracellulare
A total of 10 patients with AIDS-defining OIs (22%) died during their hospital stays. Five deaths (50%) were caused by disseminated CMV infections. The remaining 5 deaths were caused by cryptococcal meningitis (2 patients), cerebral toxoplasmosis (2 patients), and disseminated MAI (1 patient). Although PCP was the commonest AIDS-defining OI, no death was attributed to this infection in our cohort.
Discussion
Before the widespread use of potent combination ART, OIs were the principal cause of morbidity and mortality in this population. In the early 1990s, the use of chemoprophylaxis and better strategies for managing acute OIs contributed to improved quality of life and patient survival.6 However, the widespread use of ART starting in the mid-1990s has had the most profound influence on reducing OI-related mortality in HIV-infected persons in countries where therapies are accessible and affordable.6–8
Combination ART was offered to <10% of HIV-infected individuals in Oman in 2004.9 An estimated 500 Omani patients received ART in 2008.10 Despite the availability of ART in Oman, OIs continue to cause considerable morbidity and mortality for three primary reasons: 1) many patients are unaware of their HIV infection and seek medical care when an OI becomes the initial indicator of their disease; 2) certain patients are aware of their HIV infection, but do not take ART, and 3) some patients are prescribed ART, but fail to attain adequate virologic and immunologic response because of factors related to adherence, pharmacokinetics, or other unexplained biologic factors.11 Thus, although hospitalisation and death from OIs have decreased in those countries in which ART is accessible and affordable, OIs remain a leading cause of morbidity and mortality in HIV-infected persons.12 Clinicians should be aware of the epidemiology of such infections in Oman in order to provide comprehensive high-quality care for these patients. A wide variety of these infections are encountered in the HIV/AIDS population, including bacteria, fungi, viruses, and protozoa. Very often, these represent not new infections but the reactivation of an old infection.
In this study, 58% of people who were diagnosed with HIV presented with an AIDS-defining OI and more than half of them (53%) had two or more OIs. The proportion of persons with a CD4+ cell count of <200 cells/μL at the time of HIV infection diagnosis was 77%. This finding is consistent with data from India where 83.4% of patients were late presenters.13 However, data from Europe show that only one-third of patients were defined as late HIV presenters.14 Both the above findings were interesting. Whatever the underlying causes, reducing the number of late-stage diagnoses of HIV infection through earlier and more widespread testing, and promoting early introduction and adherence to ART will substantially reduce the burden of OIs. As mentioned earlier, 73% of the Omani patients who presented with one or more OIs were male; this warrants a second mention in order to reference the national percentage and its association with the epidemiology of HIV infections in Oman, where males accounted for 74% of all reported HIV/AIDS cases in 2008.10
PCP was the commonest AIDS-defining OI, accounting for 25% of all diagnosed OI events in our study. A total of 18 patients (23%) with HIV/AIDS had PCP as an AIDS-defining OI at their first presentation. The prevalence of PCP in our cohort was higher than that reported in Lebanon (10.9%), and is very much higher than in Europe where only 2–3% of PCP cases were reported among HIV/AIDS patients.15,16 Before the widespread use of primary PCP prophylaxis and ART, PCP occurred in 70–80% of patients with AIDS.17 All cases in this cohort occurred among patients with CD4+ counts of <200 cells/μL.17 A definitive diagnosis of PCP with a demonstration of organisms in induced sputum samples or BAL fluid was made in 11 patients. A presumptive diagnosis of PCP was made in the remaining 7 patients.
Oral candidiasis was the most common OI (59%) and our finding is similar to that reported in Nepal by Sharma et al.18 Some investigators from India, have reported oral candidiasis as the second most common infection in AIDS patients, while others have reported very low incidence of candidiasis (27.7%).19,20
Mycobacterium TB was the commonest isolate reported in a few studies from Hong Kong21 and India.22 Pulmonary TB was observed in 35% and extra-pulmonary TB in 21% of Omani cases. This is similar to data from Brazil where pulmonary TB was the commonest OI (52.9%).23 HIV infection is a strong risk factor for active TB in persons with latent M. tuberculosis infection. Disseminated TB accounts for 15% of all OI events (14% of all HIV patients). Disseminated TB, on the other hand, was reported in 7.8% of the cohort from Lebanon.15
In 2008, there were an estimated 1.5 million new cases of tuberculosis among persons with HIV infection, and TB accounted for 26% of AIDS-related deaths.24 In the same year, 1.4 million patients with TB were tested globally for HIV, and 81 countries tested more than half of their patients with TB for HIV. Only 4% of all persons infected with HIV were screened for TB in the same year.25 TB is endemic in some countries like India, and is the commonest cause of death in AIDS patients.26 HIV patients are at increased risk of developing active TB because of the high rate of reactivation of latent infection and the high degree of susceptibility to new infection.27
Cryptosporidium infection was observed in only 3% of Omani cases. This is in contrast to data from Ethiopia where 21% of HIV patients had Cryptosporidium.28Cryptosporidium parvum is an enteric pathogen and a common cause of gastroenteritis in humans. In patients with HIV, cryptosporidiosis may cause potentially fatal complications, including bile duct damage.29 The rate of infection among individuals with HIV/AIDS in many countries has subsided considerably because of the use of ART.30
Cryptococcus neoformans is the most important cause of invasive fungal disease in patients with HIV worldwide. Meningitis is the commonest clinical manifestation of invasive cryptococcosis in patients with HIV. In our study, Cryptococcus meningitis accounted for 22% of OI events (21% of all HIV patients). Indian reports show the incidence of cryptococcal infection (including meningitis) to be only 6–8%, whereas it is about 5–11% in the USA, 33% in Africa, and 28.5% in Thailand.31 Interestingly, none of the patients in the Lebanese cohort developed cryptococcal meningitis.15 The exact explanation for such high incidence in Oman is unclear. As a result, primary prophylaxis for invasive cryptococcal disease is widely practised by many physicians caring for HIV-infected patients in Oman.
Toxoplasmosis, caused by the protozoon Toxoplasma gondii, is one of the major OIs afflicting HIV patients. Serological tests play a crucial role in the diagnosis of toxoplasmosis in immune-competent persons.32 The prevalence rate of latent toxoplasmosis in HIV/AIDS vary from 3–97% based on ethnicity and other factors.33 Cerebral toxoplasmosis is the most common cause of focal neurological disorders in HIV patients. In our cohort, cerebral toxoplasmosis accounted for 12.5% of all AIDS-defining OIs (12% of all HIV patients). In a study from Lebanon, neurotoxoplasmosis was reported in 21.9% of the HIV-infected patients.15 This striking difference probably reflects differences in social behaviour between the two populations. In our cohort, all patients with cerebral toxoplasmosis had positive IgG for toxoplasmosis, CT/MRI evidence of compatible brain lesions, and clinical and radiological response to therapy for toxoplasmosis.
Both MAI and leishmaniasis were uncommon in our cohort, accounting for only 1.5% of all AIDS-associated OIs (1.3% of the cohort). Primary prophylaxis for MAI is not routinely practised in Oman.
Conclusion
This study shows clearly the necessity of specific measures to prevent OIs. Although many patients benefit from ART, not all patients are willing to take it. Many patients cannot tolerate or adhere to the complex drug regimes that constitute this therapy, and immunity may not be restored to a level that substantially reduces the risk of OIs in all patients. With better knowledge and diagnosis of OIs in HIV patients, clinicians and health planners can tackle the AIDS epidemic in a more effective manner. Specific antimicrobial prophylaxis by itself or in combination with ART can reduce the substantial morbidity and mortality caused by OIs in patients with HIV infections. Early diagnosis of OIs and prompt treatment definitely contributes to increased life expectancy among infected patients, thus delaying the progression to AIDS.
References
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS) UNAIDS World AIDS Day Report. From: wwwunaidsorg/en/media/unaids/contentassets/documents/unaidspublication/2011/JC2216_WorldAIDSday_report_2011_en.pdf Accessed: May 2012. [PubMed] [Google Scholar]
- 2.Centers for Disease Control Revised Surveillance Case Definitions for HIV Infection among Adults, Adolescents, and Children aged <18 Months and for HIV Infection and AIDS among Children aged 18 Months to <13 Years—United States, 2008. MMWR. 2008;57:RR-10. [PubMed] [Google Scholar]
- 3.Seage GR, 3rd, Losina E, Goldie SJ, Paltiel AD, Kimmel AD, Freedberg KA. The relationship of preventable opportunistic infections, HIV-1 RNA, and CD4 cell counts to chronic mortality. J Acquir Immune Defic Syndr. 2002;30:421–8. doi: 10.1097/00042560-200208010-00008. [DOI] [PubMed] [Google Scholar]
- 4.Ministry of Health, Oman . 1. Vol. 17. Muscat: Ministry of Health; Community Health Disease Surveillance Newsletter. From: www.unaids.org/.../2010progressreportssubmittedbycountries/oman_2010_country_progress_report_en.pdf. Accessed Jul 2010. [Google Scholar]
- 5.Walensky RP, Paltiel AD, Losina E, Mercincavage LM, Schackman BR, Sax PE, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194:11–9. doi: 10.1086/505147. [DOI] [PubMed] [Google Scholar]
- 6.Mocroft A, Vella S, Benfield TL, Chiesi A, Miller V, Gargalianos P, et al. Changing patterns of mortality across Europe in patients infected with HIV-1. EuroSIDA Study Group. Lancet. 1998;352:1725–30. doi: 10.1016/s0140-6736(98)03201-2. [DOI] [PubMed] [Google Scholar]
- 7.McNaghten AD, Hanson DL, Jones JL, Dworkin MS, Ward JW. Effects of antiretroviral therapy and opportunistic illness primary chemoprophylaxis on survival after AIDS diagnosis. Adult/Adolescent Spectrum of Disease Group. AIDS. 1999;13:1687–95. doi: 10.1097/00002030-199909100-00012. [DOI] [PubMed] [Google Scholar]
- 8.Al Dhahry SH, Scrimgeour EM, Al Suwaid AR, Al Lawati MR, El Khatim HS, Al Kobaisi MF, et al. Human immunodeficiency virus type 1 infection in Oman: Antiretroviral therapy and frequencies of drug resistance mutations. AIDS Res Hum Retroviruses. 2004;20:1166–72. doi: 10.1089/aid.2004.20.1166. [DOI] [PubMed] [Google Scholar]
- 9.Kaiser Family Foundation Reported Number of People Receiving Antiretroviral Therapy. From: http://www.globalhealthfacts.org/topic.jsp?i=10&dsp=c. Accessed: Jul 2010.
- 10.Perbost I, Malafronte B, Pradier C, Santo LD, Dunais B, Counillon E, et al. In the era of highly active antiretroviral therapy, why are HIV-infected patients still admitted to hospital for an inaugural opportunistic infection? HIV Med. 2005;6:232–9. doi: 10.1111/j.1468-1293.2005.00282.x. [DOI] [PubMed] [Google Scholar]
- 11.Bonnet F, Lewden C, May T, Heripret L, Jougla E, Bevilacqua S, et al. Opportunistic infections as causes of death in HIV-infected patients in the HAART era in France. Scand J Infect Dis. 2005;37:482–7. doi: 10.1080/00365540510035328. [DOI] [PubMed] [Google Scholar]
- 12.Mojumdar K, Vajpayee M, Chauhan NK, Mendiratta S. Late presenters to HIV care and treatment, identification of associated risk factors in HIV-1 infected Indian population. BMC Public Health. 2010;10:416. doi: 10.1186/1471-2458-10-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antinori A, Coenen T, Costagiola D, Dedes N, Ellefson M, Gatell J, et al. Late presentation of HIV infection: A consensus definition. HIV Med. 2011;12:61–4. doi: 10.1111/j.1468-1293.2010.00857.x. [DOI] [PubMed] [Google Scholar]
- 14.Naba MR, Kanafani ZA, Awar GN, Kanj SS. Profile of opportunistic infections in HIV-infected patients at a tertiary care center in Lebanon. J Infect Public Health. 2010;3:130–3. doi: 10.1016/j.jiph.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Furrer H, Egger M, Opravil M, Bernasconi E, Hirschel B, Battegay M, et al. Discontinuation of primary prophylaxis against Pneumocystis carinii pneumonia in HIV-1-infected adults treated with combination antiretroviral therapy. Swiss HIV Cohort Study. N Engl J Med. 1999;340:1301–6. doi: 10.1056/NEJM199904293401701. [DOI] [PubMed] [Google Scholar]
- 16.Phair J, Munoz A, Detels R, Kaslow R, Rinaldo C, Saah A, et al. The risk of Pneumocystis carinii pneumonia among men infected with human immunodeficiency virus type 1. Multicenter AIDS Cohort Study Group. N Engl J Med. 1990;322:161–5. doi: 10.1056/NEJM199001183220304. [DOI] [PubMed] [Google Scholar]
- 17.Sharma S, Dhungana GP, Pokhrel BM, Rijal BP. Opportunistic infections in relation to CD4 level among HIV seropositive patients from central Nepal. Nepal Med Coll J. 2010;12:1–4. [PubMed] [Google Scholar]
- 18.Kaur A, Babu PG, Jacob M, Narasimhan C, Ganesh A, Saraswathi NK, et al. Clinical and laboratory profile of AIDS in India. J Acquir Defic Synd. 1992;5:883–9. [PubMed] [Google Scholar]
- 19.Ayyagari A, Sharma AK, Prasad KN, Dhole TN, Kishore J, Chaudhary G. Spectrum of opportunistic infections in HIV infected cases in a tertiary care hospital. Indian J Med Microbiol. 1999;17:78–80. [Google Scholar]
- 20.Chan CK, Alvarez Bognar F, Wong KH, Leung CC, Tam CM, Chan KC, et al. The epidemiology and clinical manifestations of human immunodeficiency virus-associated tuberculosis in Hong Kong. Hong Kong Med J. 2010;16:192–8. [PubMed] [Google Scholar]
- 21.Kumaraswamy N, Solomon S. Spectrum of opportunistic infections among AIDS patient in Tamil Nadu, India. Int J STD AIDS. 1995;6:447–9. doi: 10.1177/095646249500600615. [DOI] [PubMed] [Google Scholar]
- 22.Santos Mde L, Ponce MA, Vendramini SH, Villa TC, Santos NS, Wysocki AD, et al. The epidemiological dimension of TB/HIV co-infection. Rev Lat Am Enfermagem. 2009;17:683–8. doi: 10.1590/s0104-11692009000500014. [DOI] [PubMed] [Google Scholar]
- 23.Harrington M. From HIV to tuberculosis and back again: A tale of activism in 2 pandemics. Clin Infect Dis. 2010;50:S260–6. doi: 10.1086/651500. [DOI] [PubMed] [Google Scholar]
- 24.Getahun H, Gunneberg C, Granich R, Nunn P. HIV infection-associated tuberculosis: The epidemiology and the response. Clin Infect Dis. 2010;50:S201–7. doi: 10.1086/651492. [DOI] [PubMed] [Google Scholar]
- 25.Swaminathan S, Nagendran G. HIV and tuberculosis in India. J Biosci. 2008;33:527–37. doi: 10.1007/s12038-008-0071-2. [DOI] [PubMed] [Google Scholar]
- 26.Cruciani M, Malena M, Bosco O, Gatti G, Serpelloni G. The impact of human immunodeficiency virus type 1 on infectiousness of tuberculosis: A meta-analysis. Clin Infect Dis. 2001;33:1922–30. doi: 10.1086/324352. [DOI] [PubMed] [Google Scholar]
- 27.Assefa S, Erko B, Medhin G, Assefa Z, Shimelis T. Intestinal parasitic infections in relation to HIV/AIDS status, diarrhea and CD4 T-cell count. BMC Infect Dis. 2009;9:155. doi: 10.1186/1471-2334-9-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Hara SP, Small AJ, Gajdos GB, Badley AD, Chen XM, Larusso NF. HIV-1 Tat protein suppresses cholangiocyte toll-like receptor 4 expression and defense against Cryptosporidium parvum. J Infect Dis. 2009;199:1195–204. doi: 10.1086/597387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tzipori S, Widmer G. A hundred-year retrospective on cryptosporidiosis. Trends Parasitol. 2008;24:184–9. doi: 10.1016/j.pt.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Satishchandra P, Nalini A, Gourie-Devi M, Khanna N, Santosh V, Ravi V, et al. Profile of neurological disorders associated with HIV/AIDS from Bangalore, South India (1986–96) Indian J Med Res. 2000;111:14–23. [PubMed] [Google Scholar]
- 31.Machala L, Malý M, Hrdá S, Rozsypal H, Stanková M, Kodym P. Antibody response of HIV-infected patients to latent, cerebral and recently acquired toxoplasmosis. Eur J Clin Microbiol Infect Dis. 2009;28:179–82. doi: 10.1007/s10096-008-0600-9. [DOI] [PubMed] [Google Scholar]
- 32.Nissapatorn V. Toxoplasmosis in HIV/AIDS: A living legacy. Southeast Asian J Trop Med Public Health. 2009;40:1158–78. [PubMed] [Google Scholar]