Abstract
Objectives:
The aim of this study was to estimate the proportion of women undergoing Papanicolaou (Pap) smear examinations, and the frequency of epithelial cell abnormalities in a teaching hospital in one emirate of the United Arab Emirates (UAE) during a three-year period.
Methods:
A retrospective study of 602 patient records from July 2007 to July 2010 was done in a teaching hospital in Ajman, UAE. The variables studied were age, ethnicity, menopausal status, and abnormalities in the Pap smear. Data were analysed using the Statistical Package for the Social Sciences and presented mainly as percentages; to assess associations, the chi-square test was used.
Results:
The total number of outpatients who attended the Obstetrics & Gynaecology Department from July 2007 to July 2010 was 150,111 patients, of which 602 (0.4% of the total) had a Pap smear test. The sample was 50.1% Arabs and 49.9% other nationalities. While 73% of the outpatients had specific complaints, 27% came for a routine screening. Epithelial cell abnormalities were seen in 3.3% of the sample, with atypical squamous cells of undetermined significance (ASCUS) found in 1.8%, low-grade squamous intraepithelial lesions (LSILs) found in 1.2%, and high-grade squamous intraepithelial lesions (HSILs) found in 0.3%. There were no cases of squamous cell carcinoma.
Conclusion:
Voluntary routine Pap smear screening was remarkably low in the study group. ASCUS was the most common epithelial cell abnormality. Community health education and opportunistic screening for cervical cancer are recommended for both national and expatriate women in the region.
Keywords: Papanicolaou smear, Cervix cancer, Cancer screening, United Arab Emirates
Advances in Knowledge
- This paper contributes to assessing current levels of cervical screening in the United Arab Emirates (UAE). The rate of opportunistic screening with Papanicolaou smear was only 0.4% in women attending the Obstetrics & Gynaecology Department of a teaching hospital in the UAE.
- The overall frequency of cervical intraepithelial abnormalities was 3.3%, out of which 1.8% had atypical squamous cells of undetermined significance (ASCUS), 1.2% had low-grade squamous intraepithelial lesion (LSILs), and 0.3% had high-grade squamous intraepithelial lesions (HSILs).
Application to Patient Care
- The proportion of women who underwent an opportunistic Pap smear was very low. This indicates a major problem of missed opportunities for actively offering Pap smear testing.
- Educational efforts can be targeted toward gynaecologists, nurses, and other health care workers to play an active role in educating patients on the importance of Pap smear testing, and to offer it whenever possible.
- Community health awareness campaigns on the importance of cervical screening are recommended for women in the reproductive age group.
- Organised, cost-effective cervical screening can be introduced to encourage more women to undergo Pap smear testing.
Cervical cancer is the second most common cancer in women worldwide, with about 500,000 new cases and 250,000 deaths each year.1 Globally, it is estimated that over one million women currently have cervical cancer, most of whom have not been diagnosed, or have no access to treatment that could cure them or prolong their lives.2 Cervical cancer is the third most common cancer in women—both in citizens and non-citizens—in the United Arab Emirates (UAE).3 Screening for cervical cancer is not mandatory in the UAE.
Secondary prevention of cervical cancer goes beyond the laboratory test. It calls for the establishment of a comprehensive screening programme targeting appropriate age groups. This helps to identify asymptomatic women with precursor lesions of cervical cancer as well as to create effective links between all levels of care, including appropriate follow-up for definitive diagnosis and the treatment of women with positive screening results.2
Cervicovaginal cytology screening with Papanicolau (Pap) smears has been used in many regions of the world since the last century. Dr. Papanicolau, the innovator of Pap smear testing, emphasised the need for a simple inexpensive method that could be applied on a large scale for the early diagnosis of cancer. This test is crucial for the detection of early changes like dysplasia in the cervical cells which lead to cancer. Over time, cervical dysplasia can gradually develop into squamous cell carcinoma of the cervix.2
In developed countries where cervical screening programmes are implemented and encouraged, new cases are not as advanced as those in developing countries.4 One possible explanation is that in countries with no screening programmes, women usually present to the clinic only when they have symptoms, such as pain, discharge, and/or abnormal bleeding. Cervical cancer, being a slow-growing cancer, can take up to 10 and sometimes 20 years for abnormal changes to develop into cancer.5 For this reason, cervical cancer is more frequent in women in their fourth, fifth or sixth decade of life.6,7 Cervical screening can help save lives, and that is why many countries are encouraging and adopting cervical screening programmes.
The World Health Organization (WHO) recommends that women should start screening for cervical cancer at 30 years or above, and include younger women only when the higher-risk groups have been covered. If a woman can be screened only once in her lifetime, then the best age is between 35 and 45 years. In 25–49 year olds, a three-year screening interval should be considered if resources are available. For women over 50 years, a five-year interval is appropriate, but for those over 65, it is not deemed necessary provided the two previous smears were negative.2 The incidence of cervical cancer in the UAE would significantly decrease if we were to adopt such an effective screening programme.
There is a shortage of studies in the Arabian Gulf region on the rates and results of Pap smear testing. The present study addresses this issue with the aim of estimating the proportion of women undergoing Pap smear examinations and the frequency of epithelial cell abnormalities in a teaching hospital in an emirate of the UAE during a three year period.
Methods
A record-based study was conducted at the Gulf Medical College Hospital and Research Center (GMCHRC) in Ajman, UAE. GMCHRC is a teaching hospital that caters not only to the patients of the Emirate of Ajman, whose adult female population is ∼88,000, but also attracts patients from the neighbouring emirates because of its subsidised rates.8 Access to the Obstetrics & Gynaecology Clinic is by self-presentation. The clinic actively offers Pap smear screening at the cost of ∼$100 per test.
The Cytology Unit of the Histo/Cyto-Pathology Laboratory of GMCHRC is run by three pathologists and one cytotechnologist. ThinPrep liquid-based cytology was the method used for the collection and preparation of all Pap smear test samples. All three pathologists were involved in interpreting the Pap smear tests results with each slide double-checked by two different pathologists to verify the results. No mismatch was recorded during the verification of the results of this study. Specimen adequacy and reporting was done according to the revised Bethesda System 2001.9
The study sample included a series of Pap smears taken from women attending the Obstetrics & Gynaecology Clinic between July 2007 and July 2010. The information was entered in a proforma designed specifically for this study. Variables selected for the study included abnormalities in the Pap smear, age, ethnicity, and menopausal status. Data were analysed using the Statistical Package for the Social Sciences, Inc. (SPSS), Version 19, (IBM, Chicago, Illinois, USA). Tables and graphs were created using SPSS, Microsoft (MS) Excel, and MS Word. Data were presented mainly as percentages and, to verify associations, the chi-square test was used.
All specimens with epithelial cell abnormalities were referred back to the Obstetrics & Gynaecology Department for further follow-up. This follow-up was done according to the 2001 Consensus Guidelines for Management of Women with Cervical Cytological Abnormalities, which recommends repeat cervical cytology, colposcopy, and human papilloma virus (HPV) testing for patients with atypical squamous cells of undetermined significance (ASCUS).10
Results
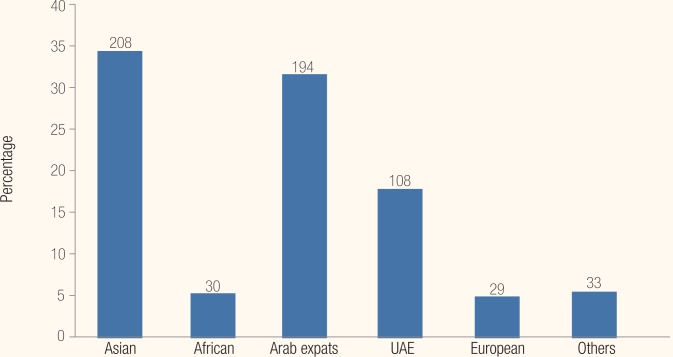
The total number of outpatients who attended the GMCHRC Obstetrics & Gynaecology Clinic from July 2007 to July 2010 was 150,111, of which 632 underwent a Pap smear test. Therefore the proportion of women who underwent this screening test at GMCHRC was 0.4%. Further analysis was done on 602 reports as 30 (4.9%) reports had to be excluded from the study due to inadequate or hypo-cellular smears. The age range of the women who underwent the Pap smear test was 20–71 years (mean ± standard deviation (SD) = 37 ± 9). Arabs constituted 50.1% of the study sample and 49.9% were from Asian and other countries [Figure 1].
Figure 1:
Percentage distribution and number of subjects of the study according to location.
UAE = United Arab Emirates.
Of the 602 women who had a Pap smear, 73% had specific complaints such as itching, vaginal discharge, pain, menorrhagia, and post-coital bleeding. The remaining 27% were asymptomatic and came for a routine screening. Post-coital bleeding and discharge were the most common symptoms in non-menopausal women when compared to menopausal women, as seen in Table 1.
Table 1:
Presenting symptoms in non-menopausal and menopausal women
| Presenting Symptoms | Non-menopausal n (%) | Menopausal n (%) | Total n (%) |
|---|---|---|---|
| Routine Pap smear (asymptomatic) | 134 (25) | 29 (41) | 163 (27) |
| Menorrhagia | 33 (6) | 4 (6) | 37 (6) |
| Vaginal discharge | 152 (29) | 13 (18) | 165 (27) |
| Post-coital bleeding | 102 (19) | 6 (8) | 108 (18) |
| Itching | 21 (4) | 6 (8) | 27 (4) |
| Abdominal pain | 43 (8) | 6 (8) | 49 (8) |
| Others | 46 (9) | 7 (10) | 53 (9) |
| Total | 531 (100) | 71 (100) | 602 (100) |
Table 2 shows the results were positive for intraepithelial lesions in 3.3% of the total of 602 samples. Intraepithelial lesions occurred in 7% of the menopausal and 2.8% of the non-menopausal women. The median age of patients with positive intra-epithelial lesions was 40 years with an age range of 24–56 years.
Table 2:
Epithelial cell abnormality in non-menopausal and menopausal women
| Epithelial Cell Abnormality | Non-menopausal n (%) | Menopausal n (%) | Total n (%) |
|---|---|---|---|
| Negative for intraepithelial lesion/malignancy | 516 (97.2) | 66 (93) | 582 (96.7) |
| Positive for intra epithelial lesion | 15 (2.8) | 5 (7) | 20 (3.3) |
| Total | 531 (100) | 71 (100) | 602 (100) |
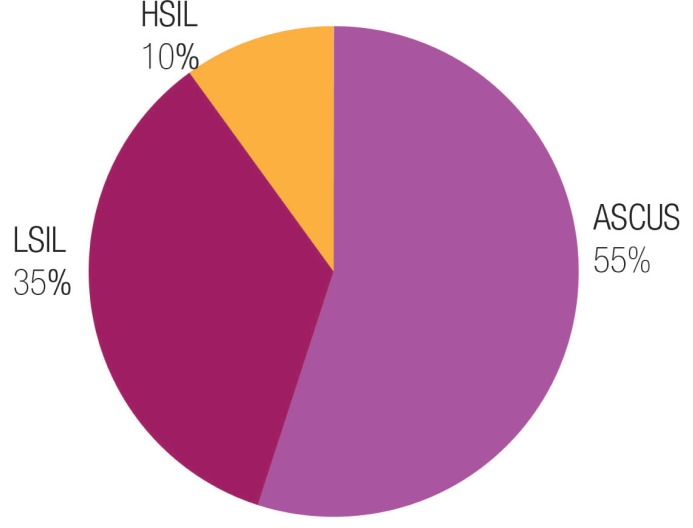
Figure 2 shows that out of the 20 samples positive for intra-epithelial lesions, 55% were ASCUS, 35% were low-grade squamous intraepithelial lesions (LSILs), and 10% were high-grade intraepithelial lesions (HSIL). Out of the 602 samples, ASCUS represented 1.8% of the total; LSIL 1.2%, and HSIL 0.3%.
Figure 2:
Distribution of Pap smear according to abnormalities.
ASCUS = atypical squamous cells of undetermined significance; LSIL = low-grade squamous intraepithelial lesions; HSIL = high-grade squamous intraepithelial lesions.
Discussion
In this study, the proportion of women who underwent an opportunistic Pap smear was very low. The rate of opportunistic screening with Papanicolaou smear was only 0.4%. The overall frequency of cervical intraepithelial abnormalities was 3.3%, out of which 1.8% had atypical squamous cells of undetermined significance (ASCUS), 1.2% had low-grade squamous intraepithelial lesion (LSILs), and 0.3% had high-grade squamous intraepithelial lesions (HSILs).
Many reports have shown that mortality from cervical cancer occurs primarily in developing countries, reflecting the grim reality of the lack of effective control measures in the developing world.5,11,12 The high rate of incidence in these countries is mainly due to the lack of screening programmes, or their inefficacy.9 In this study, it was important to determine first the rates of opportunistic screening in the UAE, where organised cervical screening programs are not in place, and second to assess the proportion of Pap smears with epithelial cell abnormalities.
The fact that merely 0.4% of the women underwent Pap smear testing is worrisome because cervical dysplasia is an asymptomatic ongoing change in the cervical epithelium. It can go unnoticed for many years and progress to cancer. If a woman presents to the clinic only when she has a gynaecological problem and regular Pap smears have not been done, the disease can easily take its natural course to full-blown cancer. The low number of Pap smear tests in our study could be attributed to a lack of patient awareness, absence of a nationwide screening programme, or a lack of initiative from many of the insurance companies to cover Pap smear testing in their basic packages. The latter results in patients having to pay for their own tests.
There is a shortage of studies from the region regarding the practice of cervical screening. One study, done in Kuwait among 300 married Kuwaiti women, showed that only 23.8% of women underwent Pap smear testing, and the main reason given among the rest of the women for not having the test was that it was not suggested by a doctor.13 Another study in Qatar among 500 women showed that almost 40% of women had had a Pap smear test at least once in their lifetime and the rest of them mentioned that they would have undergone the test if they were told that the procedure was painless and simple.14
In this context, educational efforts should be targeted toward gynaecologists, nurses, and other health care workers to encourage them to play an active role in educating the patients on the importance of Pap smear testing and its convenience, and to offer this test whenever possible.
Research regarding risk factors and likelihoods of different minorities to develop invasive carcinoma has been studied extensively in Western countries; however, few studies have been performed in the Arabian Gulf region to assess the effects of dysplasia on the development of carcinoma. Studies regarding cervical dysplasia in the region show that the percentage of abnormal Pap smears was 4.7% in a prospective study in Saudi Arabia, much higher than the 1.6% reported in the compounded literature by Altaf.15 A 13-year study in Kuwait examined the incidence of squamous cells abnormalities at one tertiary hospital. The results indicated that there was an increasing trend in younger women toward developing LSILs and HSILs. From these results it was determined that screening programmes for young women in Kuwait is essential to preventing the disease.16 While the incidence of cervical cancer is generally low in the Arab world, it is the third most common cancer in women in the UAE.3 No published literature is available about the prevalence of cervical abnormalities in the northern emirates of the UAE, the place where this study was performed.
In our study, no cases of squamous cell carcinoma were detected and only 3.3% of the total cases were positive for intraepithelial lesions. This relatively low prevalence is similar to that reported in other studies done in the region. The reported prevalence was as follow: 4.3% in a tertiary hospital in Kuwait,16 5% in a large referral hospital in Saudi Arabia,17 1.66% in the western region of Saudi Arabia,18 7.9% in southwestern Saudi Arabia, and 4.5% in a study in the eastern Saudi Arabia.19 A similar study done by the Faculty of Medicine & Health Science at UAE University reported the prevalence of cervical abnormalities in the UAE as 1.32%, and no cases of squamous cell carcinoma out of the total 2,013 smears were detected.20
The fact that only 20 out of the 602 women had cervical epithelial abnormalities, given that 108 women came with symptoms of post-coital bleeding, can be attributed to the fact that most of the those cases of post-coital bleeding could be due to other causes such as the use of intrauterine contraceptive device and cervicovaginal infections.
Conclusion
Voluntary routine screenings with Pap smears was remarkably low in this study group. ASCUS was the most common epithelial cell abnormality detected. Community health education and opportunistic screening for cervical cancer is recommended for both nationals and expatriate women in the region.
References
- 1.Sexual and reproductive health. Cancer of the Cervix. From: www.who.int/reproductivehealth/topics/cancers/en/index.html. Accessed: Sep 2011.
- 2.World Health Organization . Comprehensive cervical cancer control: A guide to essential practice 2006. From: wwwwhoint/reproductivehealth/publications/cancers/9241547006/en/indexhtml. Accessed Sep 2011. [PubMed] [Google Scholar]
- 3.Ministry of Health, United Arab Emirates, Health Policies Sector . Annual report. 2008. UAE: Ministry of Health; 2008. p. 22. [Google Scholar]
- 4.Cervical Cancer Statistics. From: www.cervicalcancer.org/statistics.html. Accessed: Oct 2011.
- 5.Peter B, Bernard L. World Cancer Report. Lyon: IARC Press; 2008. pp. 418–23. [Google Scholar]
- 6.Miller AB. Cervical Cancer Screening Programmes: Managerial Guidelines. Geneva: World Health Organization; 1992. p. 17. [Google Scholar]
- 7.Gustafsson L, Adami HO. Natural history of cervical neoplasia: Consistent results obtained by an identification technique. Br J Cancer. 1989;60:132–41. doi: 10.1038/bjc.1989.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Bureau of Statistics . Population and Vital Statistics: Ajman in Figures 2010. Ajman: National Bureau of Statistics; 2011. p. 10. [Google Scholar]
- 9.Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, et al. The 2001 Bethesda System: Terminology for reporting results of cervical cytology. JAMA. 2002;287:2114–9. doi: 10.1001/jama.287.16.2114. Forum Group Members; Bethesda 2001 Workshop. [DOI] [PubMed] [Google Scholar]
- 10.Write TC, Jr, Cox JT, Massad LS, Twiggs LB, Wilkinson EJ, ASCCP-Sponsored Consensus Conference 2001 Consensus Guidelines for the management of women with cervical cytological abnormalities. JAMA. 2002;287:2120–9. doi: 10.1001/jama.287.16.2120. [DOI] [PubMed] [Google Scholar]
- 11.Suba EJ, Raab SS. Viet/American Cervical Cancer Prevention Project. Papanicolaou screening in developing countries: An idea whose time has come. Am J Clin Pathol. 2004;121:315–20. doi: 10.1309/G40X-QBWN-PV7M-K9TY. [DOI] [PubMed] [Google Scholar]
- 12.Suba EJ, Murphy SK, Donnelly AD, Furia LM, Huynh ML, Raab SS. Systems analysis of real-world obstacles to successful cervical cancer prevention in developing countries. Am J Public Health. 2006;96:480–7. doi: 10.2105/AJPH.2004.061606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al Sairafi M, Mohamed FA. Knowledge, attitudes, and practice related to cervical cancer screening among Kuwaiti women. Med Princ Pract. 2009;18:35–42. doi: 10.1159/000163044. [DOI] [PubMed] [Google Scholar]
- 14.Al-Meer FM, Aseel MT, Al-Khalaf J, Al-Kuwari MG, Ismail MFS. Knowledge, attitude and practices regarding cervical cancer and screening among women visiting primary health care in Qatar. East Mediterr Health J. 2011;17:855–61. doi: 10.26719/2011.17.11.856. [DOI] [PubMed] [Google Scholar]
- 15.Altaf F. Cervical cancer screening with pattern of Pap smear. Saudi Med J. 2006;27:1498–502. [PubMed] [Google Scholar]
- 16.Kapila K, George SS, Al-Shaheen S, Al-Ottibi MS, Pathan SK, Sheikh ZA, et al. Changing spectrum of squamous cell abnormalities observed on Papanicolaou smears in Mubarak Al-Kabeer Hospital, Kuwait, over a 13-year period. Med Princ Pract. 2006;15:253–9. doi: 10.1159/000092986. [DOI] [PubMed] [Google Scholar]
- 17.Abdullah LS. Pattern of abnormal Pap smears in developing countries: A report from a large referral hospital in Saudi Arabia using the revised 2001 Bethesda System. Ann Saudi Med. 2007;27:268–72. doi: 10.5144/0256-4947.2007.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jamal AA, Al-Maghrabi JA. Profile of Pap smear cytology in the western region of Saudi Arabia. Saudi Med J. 2003;24:1225–9. [PubMed] [Google Scholar]
- 19.Balaha MH, Al Moghannum MS, Al Ghowinem N, Al Omran S. Cytological pattern of cervical Papanicolaou smear in eastern region of Saudi Arabia. J Cytol. 2011;28:173–7. doi: 10.4103/0970-9371.86343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghazal-Aswad S. Cervical smear abnormalities in the United Arab Emirates: A pilot study in the Arabian Gulf. Acta Cytol. 2006;50:41–7. doi: 10.1159/000325893. [DOI] [PubMed] [Google Scholar]