Abstract
Background
Hawaii has the highest incidence of hepatocellular cancer (HCC) in the U.S. and the largest proportion of Asian/Pacific Islanders(PI). HCC studies generally combine these groups into one ethnicity and we sought to examine differences between Asian/PI subpopulations.
Methods
Demographic, clinical, and treatment data for 617 HCC cases ( 420 Asian, 114 white, and 83 PI patients) were reviewed. Main outcome measures included HCC screening and liver transplant.
Results
Asian/PI subgroups had significantly more immigrants and age was different between groups. Compared to Whites, the PI and Filipinos had less HCC screening and liver transplants, fewer met Milan criteria and a smaller proportion of those with Milan criteria actually underwent transplant.
Conclusion
There were significant differences in risk factors, clinical presentation, treatment and access to care between Asian, PI and White patients with HCC. Future HCC studies may benefit from differentiating subgroups within Asian/PI populations to better focus these efforts.
Keywords: hepatocellular cancer, screening, liver transplant
Introduction
Hepatocellular cancer (HCC) is the fourth most common cause of cancer death worldwide with an estimated 652,000 deaths in 2008. An estimated 340,000 of these deaths were due to hepatitis B- related HCC.1 In the US, an estimated 22,620 people were diagnosed with liver cancer and 18,160 HCC deaths occurred 2009. HCC is one of only two cancers in the U.S. that had increases in both in incidence and mortality rates over the time period 2002–2006. SEER data from 2006 indicated that incidence of liver cancer was 10.2 per 100,000 in all males, 3.6 per 100,000 in females; however, incidence was highest in Asian/Pacific Islander males at 21.4 per 100,000. Hawaii has the highest incidence (9.5 per 100,000) and second highest death rate (6.6 per 100,000) of HCC in the U.S.2
The major risk factors for development of HCC are viral hepatitis B and C and an estimated 3.5 to 5.3 million people (1–2%) in the US are living with chronic hepatitis B or C infections. Of these, an estimated 800,000 to 1.4 million have chronic hepatitis B and 65% are unaware that they have this infection.3,4 Although routine vaccination for hepatitis B is practiced in the US, the continued high prevalence of hepatitis B may be due to the influx of immigrants from highly endemic areas - including Asia and the Pacific Islands. In Hawaii, 38.7% of the population is Asian and 8.8% are Native Hawaiian or Other Pacific Islander.5 The prevalence of Hepatitis B based on mass screening at health fairs and clinics is estimated at 3.6%. The prevalence was particularly evident in the Vietnamese, Chinese and Pacific Islanders compared to Whites with odds ratio of 3.24, 4.13 and 7.47 respectively.6
Unfortunately, much of the U.S. data on ethnic specific data for many chronic diseases combines Asians and Pacific Islanders into a single category for analysis. Few studies separate these two potentially disparate groups or analyze the specific Asian subpopulations. The purpose of this study is to characterize HCC in Pacific Islanders, Asians and Whites as 3 separate ethnic groups and further describe demographic and outcome data on HCC in Asian subpopulations in Hawaii.
Methods/Materials
Patients
This is a retrospective analysis of 618 HCC cases referred to the Liver Center or a group of surgeons (LW) at Hawaii Medical Center-East (formerly St. Francis Medical Center) from August 1992 to December 2009. This medical center is a tertiary center with the only clinic dedicated to liver diseases in Hawaii, the only liver transplant center in the State, and the only referral center for liver diseases and surgery for American territories of the Pacific Basin (including American Samoa, Guam, Saipan, and the Marshall Islands). In addition, a number of patients were foreign nationals from Asian countries, including China, Japan, Korea, and the Philippines, who sought medical care in the US. This center sees about 60–70% of the HCC cases in the State of Hawaii.
HCC was diagnosed histologically by percutaneous biopsy, liver biopsy at the time of surgery, or examination of the resected liver. Consistent with the United Network for Organ Sharing policy regarding transplant for HCC, patients without histologic confirmation were included if they had a history of chronic liver disease and a mass at least 2 cm in size seen on two imaging studies (ultrasound, CT scan or MRI) and one of the following: (1) a vascular blush seen on CT scan or MRI (2) Alpha-feto protein (AFP) > 200 ng/ml or (3) an arteriogram confirming the tumor.7
Information on demographics, medical history, laboratory results, tumor characteristics, treatment, and survival data was collected via a clinical interview. Demographic data included age, sex, birthplace, and the pateint’s self-reported ethnicity. Ethnicity was then categorized as “White”, “Asian” (including Filipinos), or “Pacific Islander.” Patients who did not fit into one of these categories or were of mixed ethnicity were subsequently classified as “Other.” Patients of mixed race with 50% Pacific Islander ethnicity were categorized as “Pacific Islander”. Data collected on medical history included information on diabetes mellitus, hyperlipidemia, smoking, family history of HCC, and risk factors for HCC including viral hepatitis, alcohol abuse (defined as greater than two alcoholic beverages daily for at least ten years), and other chronic liver diseases. Information was recorded based on interview by a single physician, without the use of a structured questionnaire. Diabetes mellitus and hyperlipidemia were identified based on patient interview and referring physicians' records. Patients who did not report hyperlipidemia but had a lipid-lowering agent on their current medication list were also classified as having hyperlipidemia. Measured height and weight were used to determine body mass index (BMI). Obesity was defined as BMI ≥ 30
Laboratory data collected included bilirubin level, albumin level, prothrombin time, creatinine, alanine aminotransferase, aspartate aminotranferase (AST), platelet count and AFP. Laboratory data that was used for the study had been obtained within 2 weeks of initial visit or drawn at the time of the visit if not available at the visit. The presence of ascites and encephalopathy was recorded in order to calculate Childs-Turcotte-Pugh scores. Bilirubin, prothrombin time with international normalized ratio (INR) and creatinine were used to calculate the Model for End-stage Liver Disease (MELD) score. AST and platelet count were used to calculate the AST/platelet ratio index (APRI) as a measure of fibrosis. The size, number, and location of the tumor(s) was used to determine the Tumor Node Metastases stage according to the American Joint Commission on Cancer (AJCC) staging manual.8
The proportion of patients with HCC detected by screening was noted. Although the Liver Center at our institution recommends that community physicians screen viral hepatitis and chronic liver disease patients with AFP and liver ultrasound every six months, there was no uniform screening protocol used in the cohort. Referring physicians used a combination of AFP and/or imaging (either ultrasound, CT scan or MRI) at various intervals, ranging from three to twelve months. HCC was deemed to be found on "screening" if the referring physician stated that screening was done and/or the patient had a previous imaging study from three to twelve months prior. HCC not found on screening was either found with symptoms (pain, abdominal mass, weight loss, jaundice) or asymptomatically with imaging done for an unrelated reason.
Treatments
Treatments included liver resection, transplantation, systemic chemotherapy and ablative therapies (including radiofrequency ablation, cryosurgery, transarterial chemoembolization, and percutaneous ethanol injection). Liver resection was considered in Child’s A patients and early Child’s B patients (Childs Turcotte Pugh score of 7, without any evidence of ascites or encephalopathy). Liver transplants were considered in patients who were unresectable but met Milan criteria (single tumor less than 5 cm or 2 to 3 tumors, each less than 3 cm). Liver transplant was also performed in patients who underwent resection but had a recurrence more than six months after surgery, provided the recurrent tumor met Milan criteria and there was no disease progression while awaiting transplant. Since 2007, liver transplant was considered in single tumors less than 6.5 cm that were down-staged to meet Milan criteria. All liver resections and transplants were performed by members of our surgical group. The majority of patients on the transplant list underwent either percutaneous radiofrequency ablation or transarterial chemoembolization while waiting for a donor.
Patients were followed long-term with imaging every 3 months after surgery or locally ablative therapies. Of 618 patients in the cohort, 418 expired during the 17 year study period, 189 are currently alive and are being actively followed and 11 patients (1.8%) have been lost to follow-up. Deaths were also confirmed using the Social Security Death Index and local newspaper obituaries
Access to Care
Access to medical care for hepatocellular cancer was measured by access to screening and liver transplant. This did not account for differences in specific screening practices by various primary care physicians, gastroenterologists and hepatologists. Factors which may have indirectly been related to screening and liver transplant that were included were age, tumor size, MELD score and meeting Milan criteria as well as ethnicity and birthplace.
Data Analysis
All analyses were performed using SAS 9.2 and SPSS statistical software. From the database of 624 patients, a total of 618 were retained for the present analysis. These patients were divided into 3 ethnic groups: Asian (n=420), White (n=114) and Pacific Islander (n=83). Six patients were excluded from the analysis because they were in the “Other” ethnic category or their ethnicity could not be determined.
Characteristics of ethnic groups were compared using analysis of variance (continuous variables) and chi-squared analysis (categorical variables). Asian subpopulations and Pacific Islanders were compared to Whites using logistic regression. P-values < 0.05 were considered to be significant.
Survival time was calculated as the period of time from the date of HCC diagnosis to the date of death. Death was defined based on all causes of mortality. The Kaplan-Meier method was used to calculate overall survival and survival for each patient group. Predictors of survival were evaluated among 601 patients diagnosed through September 1, 2009 with at least 1 year of follow-up by Cox proportional hazards modeling. Age (continuous), gender (M, F), ethnicity (Caucasian, Japanese, Filipino, Chinese, Other Asian, Pacific Islander), and screening prior to diagnosis (yes, no) were included as covariates and transplantation (yes, no) was included as strata. Variables not meeting the proportionality assumption based on Schoenfeld residuals were also included in the model using time-dependent coefficients. All variables with a p-value of ≤ 0.20 in univariate analysis were entered into multivariate Cox regression hazards models. Variables with p ≤ 0.05 in the multivariate models were considered significant.
Results
In the overall cohort, 74.9% of patients were male and their mean age was 61.5 years (standard deviation 11.97 years and range 22–94 years). Hepatitis B surface Ag was positive in 33.2% and 9.4% had only hepatitis B core Ab positive. Hepatitis C was positive in 35.8%. Other risk factors included: alcohol use (41.9%), smoking (54.2%), diabetes (27.7%) and hyperlipidemia (16.3%). In terms of birthplace, 53.6% were born in the US and 39% were born in an Asian or Pacific Island nation. (remaining 7.4% had unknown birthplace) HCC was found on screening in 17.3% and 43.7% had reported symptoms associated with HCC. The remaining patients had HCC found incidentally while undergoing other medical care. Mean size of the largest tumor was 6.25 cm.Cirrhosis was identified in 73.8% of the patients. Milan criteria was met in 38.3% of all patients. Treatment included: liver transplant (n=57, 8.6%), liver resection (n=130, 19.3%), ablative therapies (n=245, 36.2%) and no treatment (N=191, 29.3%).
Significant differences between the groups were identified for all demographic, clinical, and treatment parameters on the basis of ANOVA (Table 1). In pairwise analysis, there were significant differences between all combination of groups in terms of Hepatitis C, BMI and MELD score. Other pairwise comparisons showed that Asians and Pacific Islanders had similar hepatitis B incidence but both were higher than Whites. Asians and Pacific Islanders had similar tumor size at presentation but were both larger than Whites. There was no difference in presence of symptoms or HCC screening between Asians and Whites but Pacific Islanders were more likely to have symptoms and less likely to be screened for HCC than these two groups. Similar proportions of Asians and Pacific Islanders underwent liver transplant, but these were both lower than Whites.
Table 1.
Clinical and treatment data by ethnic group and pairwise comparison of clinical and treatment data by ethnic group
| Ethnic groups | Pairwise comparison |
|||||
|---|---|---|---|---|---|---|
| Asians (n=420) | PacIslanders (n=83) |
Whites (n=114) |
Asians vs Pacific Islander |
Asians vs Whites |
Pacific Islanders vs Whites |
|
| Demographics | ||||||
| Age (years) | 63.1 | 54.9 | 60.3 | P<0.001 | NS | P<0.001 |
| Males | 298 (71%) | 68(81.9%) | 97(85.1%) | P=0.04 | P=0.003 | NS |
| Foreign-born | 231(55%) | 41(49.4%) | 15(13.2%) | NS | P<0.001 | P<0.001 |
| Hepatitis B | 165(39.3%) | 33(39.8%) | 7(6.1%) | NS | P<0.001 | P<0.001 |
| Hepatitis C | 75(27.4%) | 33(39.8%) | 73(64%) | P<0.0001 | P<0.001 | P=0.0009 |
| Etoh | 143(34.0%) | 51(61.4%) | 65(57.0%) | P<0.0001 | P<0.001 | NS |
| Smoking | 213(50.7%) | 51(61.4%) | 71(62.3%) | NS | P=0.034 | NS |
| Presentation | ||||||
| Symptomatic | 180(42.6%) | 47(56.6%) | 44(38.6%) | P=0.022 | NS | P=0.014 |
| Screened | 76(18.1%) | 6(7.1%) | 25(21.9%) | P=0.014 | NS | P=0.005 |
| BMI | 24.7 | 30.6 | 27.1 | P<0.001 | P<0.001 | P<0.001 |
| Tumor size (cm) | 6.3 | 7.2 | 5.4 | NS | NS | P=0.007 |
| Met Milan Criteria | 160(38.1%) | 28(33.7%) | 49(43%) | NS | NS | P=0.014 |
| Stage I | 246(58.6%) | 45(54.2%) | 60(52.6%) | NS | NS | NS |
| Cirrhosis | 299(71.2%) | 64(77.1%) | 93(81.6%) | NS | P=0.03 | NS |
| MELD score | 10.1 | 13.3 | 11.6 | P<0.001 | P=0.002 | P=0.001 |
| No treatment | 113 (26.9%) | 35(42.2%) | 33(28.9%) | P=0.008 | NS | NS |
| Liver transplant | 31 (7.4%) | 3(3.6%) | 19(16.7%) | NS | P=0.006 | P=0.005 |
In Table 2, the risk factors for the 5 main Asian patient subgroups and PI patients were compared with White patients. (see odds-ratios using Whites as referrent category). All of the Asian subpopulations and Pacific Islanders had significantly more hepatitis B and less hepatitis C, except Southeast Asians who had similar amounts of hepatitis C compared to Whites.
Table 2.
Risk factors by ethnicity (Odds-ratio computed relative to Whites)
| Ethnicity | # patients |
Positive Hepatitis B |
Positive Hepatitis C |
Etoh user |
|---|---|---|---|---|
| Japanese | 172 | 15.7% | 30.8% | 37.8% |
| (3.35, 95%CI: 1.34–8.4) | (0.24,95%CI:0.14–0.40) | (0.44, 95%CI:0.27–0.72) | ||
| Filipino | 97 | 49.5% | 15.5% | 46.4% |
| (17.6, 95%CI: 7.07–44.0) | (0.09, 95%CI:0.05–0.19) | (0.63, 95%CI; 0.38–1.13) | ||
| Chinese | 83 | 62.7% | 19.3% | 15.7% |
| (30.2, 95%CI: 11.8–66.9) | (0.13, 95%CI: 0.06–0.25) | (0.13, 95%CI:0.07–0.27) | ||
| Korean | 43 | 67.4% | 30.2% | 30.2% |
| (37.3, 95% CI: 13.2–105.5) | (0.23,95%CI:0.11–0.50) | (0.31, 95%CI:0.15–0.67) | ||
| South East | 21 | 47.6% | 57.1% | 19% |
| Asian | (5.45, 95%CI: 1.84–16.1) | (0.72, 95%CI: 0.29–1.93) | (0.17, 95%CI:0.05–0.54) | |
| Pacific | 83 | 39.8% | 39.8% | 61.4% |
| Islander | (10.1, 95%CI: 4.18–24.4) | (0.37, 95%CI: 0.21–0.66) | (1.20, 95%CI: 0.67–2.14) | |
| Whites | 114 | 6.1% | 64.0% | 57.0% |
| (1.00) | (1.00) | (1.00) | ||
values are % (Odds-ratios 95% confidence interval relative to Whites), significant values are bolded
With respect to factors affecting access to care, all Asian subgroups and Pacific Islanders had significantly more immigrants and the age at diagnosis was signicantly different between groups (Table 3). There were no significant differences between Japanese, Chinese, Koreans and Southeast Asians for HCC, presentation with symptoms, meeting Milan criteria, and treatment. These Asian subgroups were were equally likely to undergo liver transplant and have a similar proportion of those that met Milan criteria actually undergo transplant when compared to Whites.
Table 3.
Characteristics of HCC that may affect access to healthcare by ethnicity
| Ethnicity | Number Foreign Born (%) |
Age (years ± standard deviation) |
Tumor size * (cms ± standard deviation) |
MELD** (score ± standard deviation) |
Number Screened for HCC (%) |
Number Presented w/symptoms (%) |
Number meeting Milan Criteria (%) |
Number Liver Transplant (%) |
Liver transplant/ met Milan (%) |
|---|---|---|---|---|---|---|---|---|---|
| Japanese | 34 | 65.0 ± 11.0 | 6.08 ±4.66 | 10.6±4.2 | 25 | 63 | 73 | 16 | 16/73 |
| (n=172) | |||||||||
| (19.8%) | (14.5%) | (36.6%) | (42.4%) | (9.3%) | (21.9%) | ||||
| Filipino | 63 | 60.5 ±13.0 | 7.71±4.71 | 10.7±5.2 | 10 | 9 | 22 | 2 | 2/22 |
| (n=97) | |||||||||
| (64.9%) | (10.3%) | (9.1%) | (22.6%) | (2.1%) | (9.1%) | ||||
| Chinese | 50 | 65.2 ±11.8 | 6.45±4.85 | 9.3±3.2 | 17 | 29 | 35 | 6 | 6/35 |
| (n=83) | |||||||||
| (60.2%) | (20.5%) | (34.9%) | (42.2%) | (7.2%) | (17.1%) | ||||
| Korean | 38 | 59.7 ± 12.9 | 4.80±3.13 | 9.1±2.9 | 17 | 12 | 19 | 5 | 5/19 |
| (n=43) | |||||||||
| (88.4%) | (39.5%) | (27.9%) | (44.1%) | (11.6%) | (26.3%) | ||||
| SouthEast | 20 | 59.5 ± 12.4 | 4.83±2.8 | 9.3±2.9 | 5 | 8 | 9 | 2 | 2/9 |
| Asian | |||||||||
| (n=21) | (95.2%) | (23.8%) | (38.1%) | (42.9%) | (9.6%) | (22.2%) | |||
| White | 15 | 60.3 ± 9.5 | 5.32±3.81 | 11.7±5.0 | 26 | 44 | 50 | 19 | 19/50 |
| (n=114) | (13.2%) | (22.8%) | (38.6%) | (43.9%) | (16.7%) | (38.0%) | |||
| Pacific | 41 | 54.9 ±12.0 | 7.19±5.17 | 13.3±6.9 | 6 | 47 | 28 | 3 | 3/28 |
| Islanders | |||||||||
| (n=83) | (49.4 %) | (7.2%) | (56.6%) | (33.7%) | (3.6%) | (10.7%) | |||
p=0.001
p<0.00
Table 3 highlights the main differences between the ethnicity with regards to factors that may potentially affect access to care. Pacific Islanders and Filipinos were both less likely to have their HCC found on screening compared to Whites. More often, they presented with symptoms and did not meet Milan criteria at the time of presentation. Significantly fewer Filipinos and Pacific Islanderss underwent liver transplant and smaller proportions of those that would have qualified for liver transplant (with Milan criteria) actually underwent liver transplant. There was no significant difference in the percentage of patients who underwent no therapy between the ethnic groups.
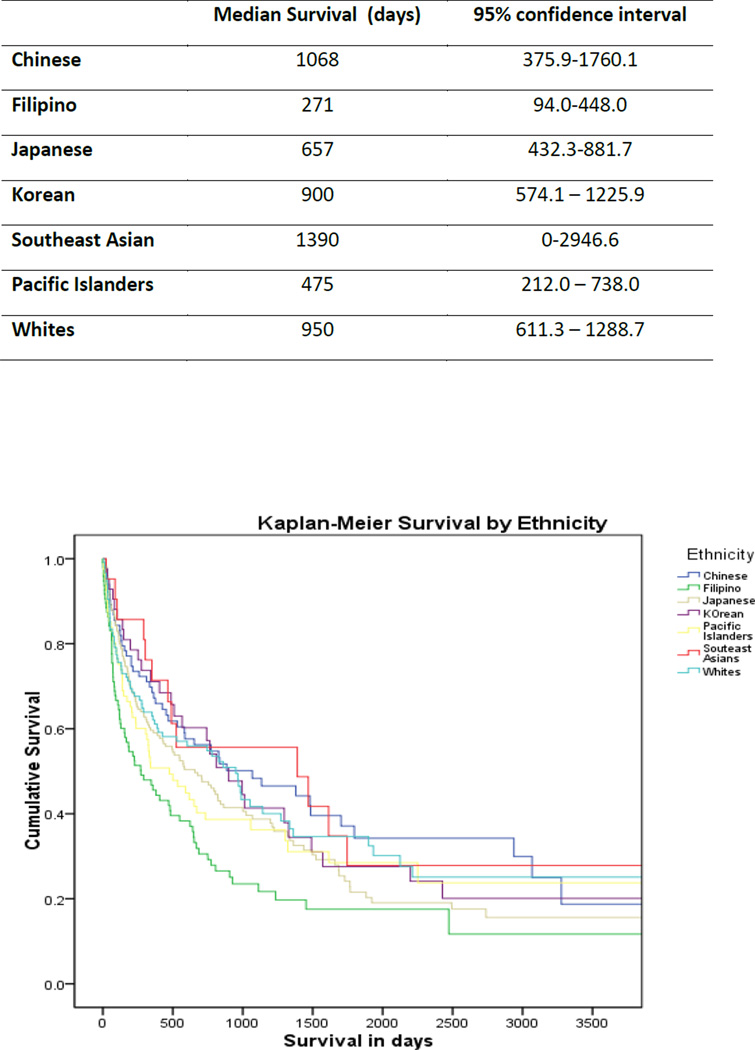
Survival did not differ significantly between the three main groups: Asians – 650 days (95% Confidence Interval 499.7 – 800.2), Pacific Islanders – 475 days (95%CI 212.0 – 738.0 days) and Whites- 950 days (95% CI 605.3 –1294.7) (p= 0.61). However, when survival of Asian subpopulations were compared against Pacific Islanders and Whites, there is a significant difference (p=0.005). In a pairwise analysis, Filipinos appeared to have a significantly lower survival compared to Whites. (table 5)
Subgroups of Pacific Islanders included the following: Hawaiian- 45 (with 27 part Hawaiian), Samoan – 13, Micronesian – 11, Tongan 5, Marshallese – 4, Chamorro – 4, and unspecified – 1. Two Micronesians were known to be from Chuuk but the other 9 were from unspecified islands in the Federated States of Micronesia. Screening was not an independent predictor of survival when adjustment was made for age, gender, ethnicity, and transplantation.
Discussion
Asian Americans and Pacific Islanders are one of the fastest growing and most heterogeneous ethnic groups. Currently these ethnic groups comprise 4% of the US population, but are expected to comprise 15.3% of the population by 2050. Native Hawaiians and other Pacific Islanders constituted 0.1% (399,000) of the US population in 2000, with 75% of them living in California or Hawaii. There are 23 subgroups of Pacific Islanders with the three largest of these being Native Hawaiians (211,014), Samoans (62,964), and Chamorros (49,345).9 Although the U.S. census bureau has been reporting on 25 different Asian and 23 Pacific Islander subgroups, national health organizations and the medical studies frequently combine this into one ethnic category. Many studies on diseases in ethnic minorities concentrate on Hispanic and African-Americans and report their data from Asians and Pacific Islanders as insufficient to compare, much less divide these two ethnicities into subpopulations.5
Socioeconomic disparities in Native Hawaiians and Pacific Islanders have been associated with a higher rate of high-risk health behaviors including smoking, alcohol abuse, obesity, and high fat diet.10 In addition, access to health care and cancer prevention programs can be limited in these populations. Because of these factors, Native Hawaiians in Hawaii had the second highest overall incidence of cancers and the highest incidence of age-adjusted cancer mortality rates when compared to other ethnic groups.11 Information on specific cancers in individual Pacific Island nations (outside of Hawaii) is rather lacking due to undeveloped tumor registries and cancer databases. 10
Racial disparities have been described in HCC but none have detailed information on Pacific Islanders as a separate group or specific Asian subgroups. Several studies have indicated that Asians have a better survival than Whites. 12,13 Yu et al in 462 patients showed that Blacks were much less likely to undergo liver transplant than Whites. Race and insurance status were associated with undergoing transplant but were not predictors of mortality in HCC. 14
This study very clearly demonstrates that Asians and Pacific Islanders with HCC are significantly different with regards to risk factors, as well as a range of clinical measures. Pacific Islanders present with HCC at a significantly younger age and with similar proportion of hepatitis B and C. Alcohol and tobacco use is also more prevalent in this group. Pacific Islanders are more likely to present with symptoms and are less likely to have their HCC found on screening. In addition, a smaller proportion of Pacific Islanders met Milan criteria for transplant at the time of presentation so they would not have qualified. However, of the 28 patients that actually qualified for transplant only 3 received a liver transplant. Many of these patients were likely eliminated during the evaluation process due to active alcohol use, morbid obesity, smoking, noncompliance and possibly insurance coverage. Hawaii has recently seen a large influx of patients from the Federated States of Micronesia and the Republic of the Marshall Islands. These patients can obtain Hawaii’s Medicaid but with limited services and as of July 2010, liver transplant is no longer a covered service.
Some of the differences between the Asian subgroups may represent differences in access to medical care. Japanese, Chinese, Korean, and Southeast Asian patients have a similar proportion of HCC found with screening and similar proportion that meet transplant criteria and undergo liver transplant compared to Whites. Filipinos and Pacific Islanders with HCC have a lower proportion found on screening and fewer undergo liver transplant. Filipinos in particular had a significantly lower survival than Whites. Diagnosis at an advanced stage and fewer liver transplants are likely contributing factors in this group. These differences highlight the importance of recording and tracking these Asian subgroups separately. Although Filipinos are categorized by the US Census data as “Asians”, this study demonstrates that their access to liver cancer screening and treatment, as well as outcome is different and more similar to Pacific Islanders than other Asian groups and Whites.
Despite apparent differences in screening and liver transplant, these factors were not independent factors affecting survival in our study. It is well accepted that survival from in HCC is very dependent on treatment and a liver transplant is the best treatment for long-term disease free survival in those patients that meet transplant criteria. Siegel et al in using the Surveillance, Epidemiology and End Results (SEER) data of 1156 adults with small (< 5 cm) HCC determined that 21% of patients received a transplant.15 Only 8.6% of our cohort underwent liver transplant and results from a previous study from our group showed that only 15% would have actually qualified based on age, meeting Milan criteria and insurance status.16 Hawaii has a great burden of HCC and liver disease and yet it is the state with the second lowest absolute number of available donors and a longer median waiting time compared to the rest of the U.S. (13 vs 11 months). 17 Perhaps organ availability is limiting our ability to see the true benefit of liver transplant for HCC.
This study is limited in that it is a single center study that represents the HCC cases seen in a state with a high population of Asians and Pacific Islanders and thus the findings may not necessarily apply to other parts of the U.S. We do not have information on level of education, insurance status, number of years that immigrants had been in the US, or their native language, which may be contributing factors in access to medical care. Specific views on health care, screening and prevention likely differ in these Asian subgroups and these beliefs may originate in their native country. More studies will be needed to explore these differences and other health care disparities.
However, our study does represent 60–70% of Hawaii’s HCC patient population and few areas in the U.S. will have sufficient numbers of Asians and Pacific Islanders to test for differences on multiple outcomes. Insurance claims databases and tumor registries will likely not have detailed data on birthplace and risk factors or have consistent reporting of treatment and survival. Asians and Pacific Islanders are the most rapidly growing ethnic groups and federal government, community and academic groups have a greater awareness of the need for a “National Health Care Agenda” for these groups to eliminate health disparities.18 Our data clearly demonstrated the need to categorize and track these various ethnic groups separately in order to identify their divergent risks. This study has demonstrated a greater need for community and physician education, hepatitis B/liver cancer screening, and hepatitis B vaccination, especially in the Filipino and Pacific Islander populations in Hawaii. This will also become increasingly important as these and other Asian subgroups increase in number and migrate across the US.
Figure 1.
Median Survival by Asian subpopulations compared to Pacific Islanders and Whites
Table 4.
Odds-ratios of factors affecting access to care comparison of Pacific Islanders and Filipinos to Whites
| Ethnicity | # patients | Screened for HCC | Presented with symptoms |
Met Milan Criteria |
Liver Transplant | No treatment |
transplant/met Milan |
|---|---|---|---|---|---|---|---|
| Filipino | 97 | 0.30 | 3.39 | 0.33 | 0.11 | 1.58 | 0.16 |
| (0.13–0.71) | (1.91–5.90) | (0.18–0.62) | (0.02–0.46) | (0.89–2.80) | (0.03–0.78) | ||
| White | 114 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Pacific | 83 | 0.32 | 1.47 | 0.65 | 0.19 | 1.79 | 0.28 |
| Islanders | (0.26–0.67) | (1.17–3.69) | (0.36–1.17) | (0.05–0.66) | (0.99–3.24) | (0.05–0.74) | |
Bolded odds-ratios are significant. All other ethnicities were not significant for all values compared to Whites.
Acknowledgments
Funding/support: This research was partially supported by an American Recovery and Reinvestment Act grant #3P30CA071789-12S6
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflicts of interest.
References
- 1.World Health Organization. [accessed September 1, 2010]; at http://who.int.
- 2.National Cancer Institute. [accessed October 1, 2010]; SEER data at http://cancer.gov/statistics.
- 3.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46(4):1034–1040. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 4.Hagan H, Campbell J, Thiede H, et al. Self reported hepatitis C virus antibody status and risk behavior in young injectors. Public Health Rep. 2006;121(6):710–719. doi: 10.1177/003335490612100611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Census Bureau. [accessed September 1, 2010];Fact sheet for Hawaii. http://census.gov.
- 6.Tsai N, Holck PS, Wong LL, Ricalde AA. Seroepidemiology of Hepatitis B Virus Infection: Analysis of Mass Screening in Hawaii. Hepatology International. 2008;2(4):478–485. doi: 10.1007/s12072-008-9103-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Network for Organ Sharing. [accessed May 20, 2009];Policy 3.6.4.4. at www.unos.org.
- 8.Edge SB, Byrd DR, Compton CC, et al. AJCC Cancer Staging Manual. Seventh Edition. New York, NY: Springer; 2009. pp. 191–199. [Google Scholar]
- 9.Honolulu Star Bulletin. Hawaiians, Pacific Islanders tallied. 2001. Mar 13, p. 1. [Google Scholar]
- 10.Native Hawaiians and Pacific Islanders and Cancer. Intercultural Cancer Council Fact Sheets. [accessed November 1, 2010];Intercultural Cancer Council. 2001 at http://iccnetwork.org.
- 11.Chu KC. Cancer data for Asian Americans and Pacific Islanders. Asian American and Pacific Islander Journal of Health. 1998;6(2):130–139. [PubMed] [Google Scholar]
- 12.Artinyan A, Mailey B, Sanchez-Luege N, et al. Race, ethnicity and socioeconomic statutes influence the survival of patients with hepatocellular carcinoma in the United States. Cancer. 2010;116(5):1367–1377. doi: 10.1002/cncr.24817. [DOI] [PubMed] [Google Scholar]
- 13.Davilla JA, El-Serag HB. Racial differences in survival of hepatocellular carcinoma in the United States: a population-based study. Clin Gastroenterol Hepatol. 2006;4(1):104–110. [PubMed] [Google Scholar]
- 14.Yu JC, Neugut AI, Wang S, et al. Racial and insurance disparities in the receipt of transplant among patients with hepatocellular cancer. Cancer. 2010;116(7):1801–1809. doi: 10.1002/cncr.24936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siegel AB, McBride RB, El-Serag HB, et al. Racial disparities in utilization of liver transplantation for hepatocellular carcinoma in the United States 1998–2002. Am J Gastroenterol. 2008;103(1):120–127. doi: 10.1111/j.1572-0241.2007.01634.x. [DOI] [PubMed] [Google Scholar]
- 16.Wong LL, Tsai N, Limm W, Wong L. Liver transplant for hepatocellular cancer: a treatment for the select few. Clin Transplant. 2004;18(4):205–210. doi: 10.1046/j.1399-0012.2003.00157.x. [DOI] [PubMed] [Google Scholar]
- 17. [accessed November 9, 2010];OPTN/SRTR Annual Report 2009: Decreased donors procured by U.S. Organ Procurement Organization 1998–2008. http://ustransplant.org.
- 18.Ghosh C. A national health agenda for Asian Americans and Pacific Islanders. JAMA. 2010;304(12):1381–1382. doi: 10.1001/jama.2010.1358. [DOI] [PubMed] [Google Scholar]