Abstract
The purpose of this study was to evaluate for differences in occurrence and severity ratings of sleep disturbance, fatigue, and decreased energy in women who reported breast pain prior to surgery for breast cancer. Of the 390 women who completed self-report measures for each symptom, 28.2% reported pain in their breast prior to surgery. A higher percentage of women in the pain group (i.e., 66.7% versus 53.5%) reported clinically meaningful levels of sleep disturbance. However, no between group differences were found in the severity of sleep disturbance, fatigue, or decreased energy. Findings from this study suggest that sleep disturbance, fatigue, and decreased levels of energy are significant problems for women prior to breast cancer surgery. Future studies need to evaluate for specific characteristics that place women at greater risk for these symptoms as well as the mechanisms that underlie these symptoms.
Keywords: pain, fatigue, energy, sleep disturbance, breast cancer, surgery
INTRODUCTION
While numerous studies have evaluated fatigue,1-4 sleep disturbance,5-7 and pain1,8-10 in breast cancer patients during adjuvant treatment, studies on the occurrence and severity of sleep disturbance,11-14 fatigue,12,15,16 and pain17-20 prior to surgery are more limited. In studies of preoperative sleep disturbance,11-14 between 36% and 88% of patients reported this symptom and 55% noted that their cancer diagnosis triggered the sleep disturbance.21 In a study of the association between preoperative levels of sleep disturbance and postoperative outcomes, patients with poorer sleep efficiency scores reported significantly higher levels of postoperative pain and greater pain interference with function.11
Only three studies evaluated preoperative levels of fatigue.12,15,16 In one study,16 patients with higher levels of preoperative fatigue anticipated higher levels of postoperative fatigue. In addition, between 32.5%15 and 77%12 of patients reported fatigue prior to breast cancer surgery. No studies have evaluated both the occurrence and severity of preoperative fatigue in breast cancer patients and its relationship to other symptoms.
Preoperative pain in the breast or arm was evaluated in only six studies.17-20,22 In one study,17 10% of women reported preoperative pain in the ipsilateral arm. In a follow-up study of this sample,18 30% of women reported preoperative breast pain. In another study,19 87.8% of patients reported preoperative breast tenderness. Finally, two studies20,22 found that 28% of women reported preoperative breast pain. None of these studies evaluated the relationships between preoperative pain and sleep disturbance or fatigue.
Given the large number of women who undergo surgery for breast cancer, little is known about the occurrence of clinically meaningful levels of preoperative sleep disturbance, fatigue, and breast pain in women prior to surgery. In addition, no data are available on the impact of preoperative breast pain on sleep disturbance and fatigue. Given the paucity of research, the purposes of this study were to evaluate for differences in occurrence and severity of sleep disturbance and sleep interference, as well as fatigue and energy in patients with breast cancer who did and did not have preoperative breast pain.
METHODS
All of the study procedures are described in detail elsewhere.22-23 In brief, 410 breast cancer patients were recruited prior to surgery, signed an informed consent, and completed the enrollment questionnaires. Patients completed a demographic questionnaire, Karnofsky Performance Status (KPS) score,24 and Self-Administered Comorbidity Questionnaire.25 Medical records were reviewed for disease and treatment information.
Occurrence of preoperative breast pain was determined by asking “Are you experiencing pain in your affected breast?”. If yes, women rated the severity of their pain using 0 (no pain) to 10 (worst pain imaginable) numeric rating scales (NRS).26 Women were asked how many days a week and how many hours a day they experienced significant pain.
General Sleep Disturbances Scale (GSDS) was used to evaluate overall sleep disturbance over the past week. GSDS total score that can range from 0 (no disturbance) to 147 (extreme sleep disturbance).5,23,27-29
Sleep Interference Scale (SIS) evaluated the level of interference that sleep disturbance had on seven aspects of daily living. A mean interference score was calculated for the 7 items.
Lee Fatigue Scale (LFS) consists of 18 items designed to assess physical fatigue and energy.30 Each item is rated on a 0 (not at all) to 10 (extremely) NRS. Total fatigue and energy scores were calculated as the mean of the 13 fatigue items and the 5 energy items, respectively. Higher scores indicate greater fatigue severity and higher levels of energy.
Descriptive statistics and frequency distributions were generated on sample characteristics and symptom severity scores. Clinically meaningful cutpoints for sleep disturbance (i.e., GSDS total score ≥43), fatigue (i.e., LFS fatigue severity score ≥4.4), and energy (i.e., LFS energy score ≤4.8) were used to determine the occurrence rates for these symptoms.5,31 Women were categorized into breast pain (n=110; 28.2%) and no breast pain (n=280; 71.8%) groups. Differences in demographic and clinical characteristics between the pain and no pain groups were determined using parametric and nonparametric tests.
Based on these initial analyses, significant differences in age, KPS scores, menopausal status, and ethnicity were found between the two pain groups. Because differences in sleep disturbance and fatigue are associated with age,32-34 KPS scores,35-37 ethnicity,11 and menopausal status,38,39 age and KPS score (as continuous variables) as well as ethnicity (white versus nonwhite) and menopausal status (yes/no; as dichotomous variables) were entered as covariates and pain group (as a dichotomous variable) was entered as a fixed factor in the univariate analyses of covariance that evaluated for differences in symptoms between women with and without breast pain. A p-value of <0.05 was considered statistically significant.
RESULTS
Differences in Demographic and Clinical Characteristics
Differences in demographic and clinical characteristics between women with and without preoperative breast pain are summarized in Tables 1 and 2, respectively. Women with preoperative breast pain were significantly younger and a significantly higher percentage was non-white. No differences in education, marital status, living arrangements, employment status, and income were found between the two pain groups.
Table 1.
Differences in demographic characteristics between women with (n=110) and without (n=280) breast pain prior to breast cancer surgery
| Characteristic | No Breast Pain 71.8% (n=280) Mean (SD) |
Breast Pain 28.2% (n=110) Mean (SD) |
Statistics | |
|---|---|---|---|---|
|
| ||||
| Age (years) | 56.5 (11.8) | 50.9 (9.8) | t=4.81, p<0.0001 | |
|
| ||||
| Education (years) | 15.8 (2.7) | 15.4 (2.6) | n.s. | |
|
| ||||
| % (n) | % (n) | |||
|
| ||||
| Ethnicity | Non-white | 31.9 (89) | 45.0 (49) | F.E.=0.018 |
|
| ||||
| Marital status | Married | 41.9 (117) | 43.0 (46) | n.s. |
|
| ||||
| Lives alone | 24.1 (67) | 25.2 (27) | n.s. | |
|
| ||||
| Works for pay | 48.4 (134) | 50.0 (55) | n.s. | |
|
| ||||
| Annual income | <$30,000 | 12.6 (29) | 25.3 (23) | n.s. |
|
| ||||
| $30,000-$99,999 | 47.4 (109) | 40.7 (37) | ||
|
| ||||
| =$100,000 | 40.0 (92) | 34.1 (31) | ||
n.s. = not significant
Table 2.
Differences in clinical characteristics between women with (n=110) and without (n=280) breast pain prior to breast cancer surgery
| Characteristic | No Breast Pain 71.8% (n=280) Mean (SD) |
Breast Pain 28.2% (n=110) Mean (SD) |
Statistics | |
|---|---|---|---|---|
|
| ||||
| Body mass index (kg/m2) | 27.0 (6.3) | 26.1 (5.7) | n.s. | |
|
| ||||
| Karnofsky performance status score | 94.0 (10.3) | 90.9 (10.1) | t=2.66, p=0.008 | |
|
| ||||
| Self-administered comorbidity questionnaire score | 4.3 (2.8) | 4.2 (3.1) | n.s. | |
|
| ||||
| Number of biopsies in the last year | 1.5 (0.8) | 1.6 (0.8) | U= 12887.0, p=0.006 | |
|
| ||||
| % (n) | % (n) | |||
|
| ||||
| Stage of Disease | Stage 0 | 17.7 (47) | 16.0 (17) | n.s. |
|
| ||||
| Stage I | 39.6 (105) | 31.1(33) | ||
|
| ||||
| Stage IIA/IIB | 34.7 (92) | 40.6 (43) | ||
|
| ||||
| Stage IIIA-IV | 7.9 (21) | 12.3 (13) | ||
|
| ||||
| Mastitis | 11.6 (32) | 14.0 (15) | n.s. | |
|
| ||||
| Fibrocystic or cystic breast disease | 17.8 (48) | 22.9 (24) | n.s. | |
|
| ||||
| Non-cancer surgery on the affected breast | 10.0 (28) | 12.7 (14) | n.s. | |
|
| ||||
| Non-cancer surgery on the affected arm | 4.3 (12) | 1.8 (2) | n.s. | |
|
| ||||
| Non-cancer surgery on the affected hand | 5.0 (14) | 6.4 (7) | n.s. | |
|
| ||||
| Injury on the affected arm | 15.0 (42) | 14.5 (16) | n.s. | |
|
| ||||
| Injury on the affected hand | 9.6 (27) | 10.9 (12) | n.s. | |
|
| ||||
| Gone through menopause | 67.9 (186) | 53.8 (57) | F.E.=0.012 | |
|
| ||||
| Received neoadjuvant therapy | 21.1 (59) | 17.3 (19) | n.s. | |
kg/m2 = kilograms/meter squared; n.s. = not significant
No significant differences were found in the majority of clinical characteristics between the two pain groups. Significantly fewer women with breast pain had gone through menopause. Women with breast pain reported a significantly lower mean KPS score and had significantly more biopsies in the previous year.
A complete description of the pain problem is reported elsewhere.22 In brief, among the women with preoperative breast pain, the mean worst and average pain scores were 3.6±2.4 and 2.2±2.1, respectively. These women had significant pain an average of 6.2±7.9 hours per day on 2.9±2.8 days per week.
Differences in Symptom Occurrence Rates
As shown in Figure 1, a significantly higher percentage of patients with breast pain (66.7%) had a total GSDS score of ≥43 than patients without breast pain (53.5%, p=.02). No between group differences were found in the percentage of patients who reported clinically meaningful levels of fatigue (≥4.4) or decrements in energy (≤4.8).
Figure 1.
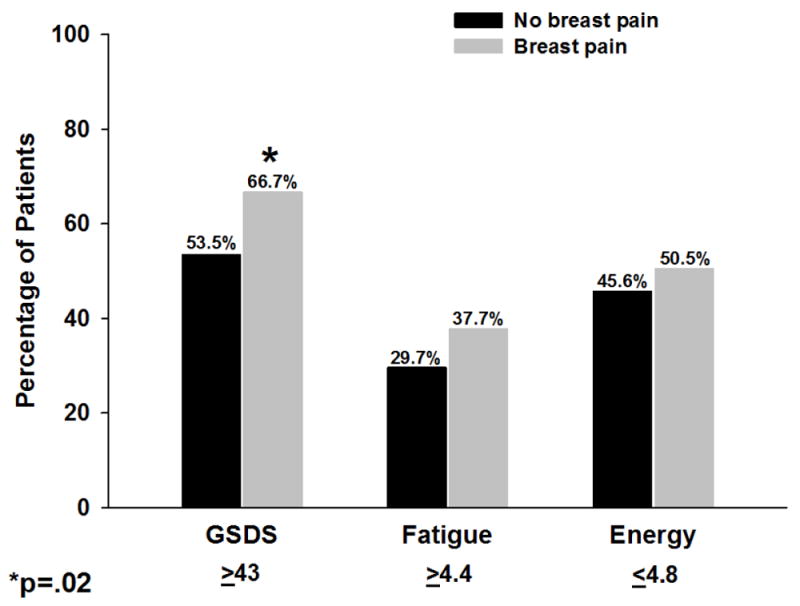
Differences in occurrence rates for sleep disturbance (i.e., General Sleep Disturbance Scale ≥43), fatigue (i.e., Lee Fatigue Scale (LFS) Score ≥4.4), and decreased levels of energy (i.e., Energy subscale of LFS ≤4.8) by pain group. All values are plotted as percentages by pain group.
Differences in Sleep Parameters
After controlling for significant covariates, no differences were found in any subscale or the total GSDS scores between the two pain groups (Supplemental Figure 1). Except for the interference with sexual activity item, no differences were found in any individual item or total sleep interference scores (Supplemental Figure 2). Women without breast pain reported significantly higher sleep interference scores with sexual activity.
Differences in Fatigue and Energy Scores
After controlling for significant covariates, no differences were found in fatigue and energy scores between the two pain groups (Supplemental Figure 3).
DISCUSSION
This study is the first to evaluate the effects of preoperative breast pain on sleep disturbance, fatigue, and energy levels in a large sample of breast cancer patients. While the occurrence of clinically meaningful levels of sleep disturbance was significantly higher in the pain group, 53.5% of women in the no pain group reported sleep disturbance. This finding is consistent with previous reports12,13 and suggests that preoperative sleep disturbance is a common problem in these patients. In contrast, the occurrence rates for clinically meaningful levels of fatigue and decreased energy were similar between the two groups. Consistent with one study,15 but lower than occurrence rates reported in another study,12 32% of the sample reported fatigue. Taken together, the high rates of sleep disturbance and fatigue suggest that regardless of preoperative pain, a substantial percentage of women experience clinically meaningful levels of these symptoms prior to surgery.
No studies have evaluated preoperative energy levels in breast cancer patients. While the concept of energy may appear to be the inverse of fatigue, it is a unique concept. Energy was assessed with LFS items that evaluated levels of activity, feeling lively, and efficiency. In comparison, the questions that assessed fatigue included ratings of exhaustion and difficulty concentrating. The hypothesis that diminished energy is a distinct concept is further supported by the fact that while 32% of the patients reported clinically meaningful levels of fatigue almost 50% of the patients reported clinically meaningful decrements in energy.
No differences were found, between women with and without breast pain, in any GSDS subscale or total scores. However, except for the “use of sleep medications” subscale, scores on the other six GSDS subscales ranged from 2.1 to 4.8. These scores are interpreted as the number of days per week a patient experiences a particular problem and a score of ≥3 indicates a clinically meaningful problem. Women in this study experienced problems with sleep quality, quantity, mid-sleep awakenings, and early awakenings on three or more days per week, which suggests a problem with sleep maintenance. In addition, the very low scores on the use of sleep medications subscale suggests that women are not prescribed or are not taking medications to alleviate sleep disturbance.
This study is the first to report sleep interference scores in women prior to surgery for breast cancer. With the exception of sexual activity, pain group membership did not influence sleep interference scores. The individual item and total SIS scores ranged from 1.4 to 3.7. These findings suggest that on average these women had mild to moderate levels of sleep interference. Finally, women without breast pain reported that their level of sleep disturbance interfered more often with their sexual activity than women with breast pain. While no studies were found on the impact of sleep disturbance on sexual activity in women with breast cancer, in women with fibromyalgia sleep disturbance and/or pain may diminish sexual activity.40 Additional research is warranted on the impact of sleep disturbance on patients’ ability to function.
Several study limitations need to be acknowledged. Sleep disturbance was assessed using only a subjective measure. Future studies need to evaluate both objective and subjective measures and evaluate for the existence of a sleep problem prior to the diagnosis of breast cancer. In addition, one of the major reasons for refusal was being overwhelmed with the cancer experience. Therefore, this study may underestimate the occurrence and severity of preoperative sleep disturbance and fatigue, as well as psychosocial characteristics (e.g., stress associated with the diagnosis of cancer, anxiety associated with impending surgery) in these women. Finally, since the majority of the sample was well educated, findings cannot be generalized to individuals with lower levels of education.
Despite these limitations, findings from this study suggest that sleep disturbance, fatigue, and decreased levels of energy are significant problems for women prior to breast cancer surgery. Future studies need to evaluate for specific characteristics that place women at greater risk for these symptoms. In addition, future studies need to determine the mechanisms that underlie sleep disturbance, increased fatigue, decreased energy, and breast pain prior to surgery, as well as evaluate for changes in these symptoms over time. This type of detailed characterization of these symptoms in women prior to and during treatment for breast cancer will facilitate the development and testing of interventions to relieve these symptoms.
Supplementary Material
Differences in total and subscale scores on the General Sleep Disturbance Scale between women with and without breast pain. All values are plotted as means ± standard errors of the mean.
Differences in the total and item scores on the Sleep Interference Scale between women with and without breast pain. All values are plotted as means ± standard errors of the mean.
Differences in the fatigue and energy subscale scores on the Lee Fatigue Scale between women with and without breast pain. All values are plotted as means ± standard errors of the mean.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Siefert ML. Fatigue, pain, and functional status during outpatient chemotherapy. Oncol Nurs Forum. 2010;37:E114–23. doi: 10.1188/10.ONF.114-123. [DOI] [PubMed] [Google Scholar]
- 2.Dhruva A, Dodd M, Paul SM, Cooper BA, Lee K, West C, et al. Trajectories of fatigue in patients with breast cancer before, during, and after radiation therapy. Cancer Nurs. 2010;33:201–12. doi: 10.1097/NCC.0b013e3181c75f2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrykowski MA, Donovan KA, Jacobsen PB. Magnitude and correlates of response shift in fatigue ratings in women undergoing adjuvant therapy for breast cancer. J Pain Symptom Manage. 2009;37:341–51. doi: 10.1016/j.jpainsymman.2008.03.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bower JE, Ganz PA, Tao ML, Hu W, Belin TR, Sepah S, et al. Inflammatory biomarkers and fatigue during radiation therapy for breast and prostate cancer. Clin Cancer Res. 2009;15:5534–40. doi: 10.1158/1078-0432.CCR-08-2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miaskowski C, Lee K, Dunn L, Dodd M, Aouizerat BE, West C, et al. Sleep-wake circadian activity rhythm parameters and fatigue in oncology patients before the initiation of radiation therapy. Cancer Nurs. 2011;34:255–68. doi: 10.1097/NCC.0b013e3181f65d9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beck SL, Berger AM, Barsevick AM, Wong B, Stewart KA, Dudley WN. Sleep quality after initial chemotherapy for breast cancer. Support Care Cancer. 2010;18:679–89. doi: 10.1007/s00520-009-0662-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berger AM, Farr LA, Kuhn BR, Fischer P, Agrawal S. Values of sleep/wake, activity/rest, circadian rhythms, and fatigue prior to adjuvant breast cancer chemotherapy. J Pain Symptom Manage. 2007;33:398–409. doi: 10.1016/j.jpainsymman.2006.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andersen KG, Kehlet H. Persistent pain after breast cancer treatment: A critical review of risk factors and strategies for prevention. J Pain. 2011;12:725–46. doi: 10.1016/j.jpain.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Starkweather AR, Lyon DE, Schubert CM. Pain and inflammation in women with early-stage breast cancer prior to induction of chemotherapy. Biol Res Nurs. 2011 doi: 10.1177/1099800411425857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montazeri A. Persistent pain following breast cancer surgery: correlates and determinants. Womens Health. 2010;6:175–7. doi: 10.2217/whe.10.6. [DOI] [PubMed] [Google Scholar]
- 11.Wright CE, Bovbjerg DH, Montgomery GH, Weltz C, Goldfarb A, Pace B, et al. Disrupted sleep the night before breast surgery is associated with increased postoperative pain. J Pain Symptom Manage. 2009;37:352–62. doi: 10.1016/j.jpainsymman.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cimprich B. Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nurs. 1999;22:185–94. doi: 10.1097/00002820-199906000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Savard J, Villa J, Ivers H, Simard S, Morin CM. Prevalence, natural course, and risk factors of insomnia comorbid with cancer over a 2-month period. J Clin Oncol. 2009;27:5233–9. doi: 10.1200/JCO.2008.21.6333. [DOI] [PubMed] [Google Scholar]
- 14.Wright CE, Schnur JB, Montgomery GH, Bovbjerg DH. Psychological factors associated with poor sleep prior to breast surgery: an exploratory study. Behav Med. 2010;36:85–91. doi: 10.1080/08964280903521305. [DOI] [PubMed] [Google Scholar]
- 15.De Vries J, Van der Steeg AF, Roukema JA. Determinants of fatigue 6 and 12 months after surgery in women with early-stage breast cancer: a comparison with women with benign breast problems. J Psychosom Res. 2009;66:495–502. doi: 10.1016/j.jpsychores.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Schnur JB, Hallquist MN, Bovbjerg DH, Silverstein JH, Stojceska A, Montgomery GH. Predictors of expectancies for post-surgical pain and fatigue in breast cancer surgical patients. Pers Individ Dif. 2007;42:419–29. doi: 10.1016/j.paid.2006.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tasmuth T, Estlanderb AM, Kalso E. Effect of present pain and mood on the memory of past postoperative pain in women treated surgically for breast cancer. Pain. 1996;68:343–7. doi: 10.1016/s0304-3959(96)03219-8. [DOI] [PubMed] [Google Scholar]
- 18.Tasmuth T, von Smitten K, Kalso E. Pain and other symptoms during the first year after radical and conservative surgery for breast cancer. Br J Cancer. 1996;74:2024–31. doi: 10.1038/bjc.1996.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baron RH, Fey JV, Borgen PI, Van Zee KJ. Eighteen sensations after breast cancer surgery: a two-year comparison of sentinel lymph node biopsy and axillary lymph node dissection. Oncol Nurs Forum. 2004;31:691–8. doi: 10.1188/04.ONF.691-698. [DOI] [PubMed] [Google Scholar]
- 20.Poleshuck EL, Katz J, Andrus CH, Hogan LA, Jung BF, Kulick DI, et al. Risk factors for chronic pain following breast cancer surgery: a prospective study. J Pain. 2006;7:626–34. doi: 10.1016/j.jpain.2006.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bower JE. Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol. 2008;26:768–77. doi: 10.1200/JCO.2007.14.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCann B, Miaskowski C, Koetters T, Baggott C, West C, Levine JD, et al. Associations between pro- and anti-inflammatory cytokine genes and breast pain in women prior to breast cancer surgery. Journal of Pain. 2012;13:425–37. doi: 10.1016/j.jpain.2011.02.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Onselen C, Cooper BA, Lee K, Dunn L, Aouizerat BE, West C, et al. Identification of distinct subgroups of breast cancer patients based on self-reported changes in sleep disturbance. Support Care Cancer. 2012 doi: 10.1007/s00520-012-1381-3. [DOI] [PubMed] [Google Scholar]
- 24.Karnofsky D, Abelmann WH, Craver LV, Burchenal JH. The use of nitrogen mustards in the palliative treatment of carcinoma. Cancer. 1948;1:634–56. [Google Scholar]
- 25.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–63. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 26.Jensen MP. The validity and reliability of pain measures in adults with cancer. J Pain. 2003;4:2–21. doi: 10.1054/jpai.2003.1. [DOI] [PubMed] [Google Scholar]
- 27.Miaskowski C, Cooper BA, Paul SM, Dodd M, Lee K, Aouizerat BE, et al. Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: a cluster analysis. Oncol Nurs Forum. 2006;33:E79–89. doi: 10.1188/06.ONF.E79-E89. [DOI] [PubMed] [Google Scholar]
- 28.Miaskowski C, Paul SM, Cooper BA, Lee K, Dodd M, West C, et al. Predictors of the trajectories of self-reported sleep disturbance in men with prostate cancer during and following radiation therapy. Sleep. 2011;34:171–9. doi: 10.1093/sleep/34.2.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Onselen C, Dunn LB, Lee K, Dodd M, Koetters T, West C, et al. Relationship between mood disturbance and sleep quality in oncology outpatients at the initiation of radiation therapy. Eur J Oncol Nurs. 2010;14:373–9. doi: 10.1016/j.ejon.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee KA, Hicks G, Nino-Murcia G. Validity and reliability of a scale to assess fatigue. Psychiatry Res. 1991;36:291–8. doi: 10.1016/0165-1781(91)90027-m. [DOI] [PubMed] [Google Scholar]
- 31.Fletcher BS, Paul SM, Dodd MJ, Schumacher K, West C, Cooper B, et al. Prevalence, severity, and impact of symptoms on female family caregivers of patients at the initiation of radiation therapy for prostate cancer. J Clin Oncol. 2008;26:599–605. doi: 10.1200/JCO.2007.12.2838. [DOI] [PubMed] [Google Scholar]
- 32.Janz NK, Mujahid M, Chung LK, Lantz PM, Hawley ST, Morrow M, et al. Symptom experience and quality of life of women following breast cancer treatment. J Womens Health. 2007;16:1348–61. doi: 10.1089/jwh.2006.0255. [DOI] [PubMed] [Google Scholar]
- 33.Winters-Stone KM, Bennett JA, Nail L, Schwartz A. Strength, physical activity, and age predict fatigue in older breast cancer survivors. Oncol Nurs Forum. 2008;35:815–21. doi: 10.1188/08.ONF.815-821. [DOI] [PubMed] [Google Scholar]
- 34.Geinitz H, Zimmermann FB, Thamm R, Keller M, Busch R, Molls M. Fatigue in patients with adjuvant radiation therapy for breast cancer: long-term follow-up. J Cancer Res Clin Oncol. 2004;130:327–33. doi: 10.1007/s00432-003-0540-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum. 2001;28:465–70. [PubMed] [Google Scholar]
- 36.Cheng KK, Lee DT. Effects of pain, fatigue, insomnia, and mood disturbance on functional status and quality of life of elderly patients with cancer. Crit Rev Oncol Hematol. 2011;78:127–37. doi: 10.1016/j.critrevonc.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 37.Wielgus KK, Berger AM, Hertzog M. Predictors of fatigue 30 days after completing anthracycline plus taxane adjuvant chemotherapy for breast cancer. Oncol Nurs Forum. 2009;36:38–48. doi: 10.1188/09.ONF.38-48. [DOI] [PubMed] [Google Scholar]
- 38.Woods NF, Mitchell ES. Sleep symptoms during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Sleep. 2010;33:539–49. doi: 10.1093/sleep/33.4.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ward T, Scheid V, Tuffrey V. Women’s mid-life health experiences in urban UK: an international comparison. Climacteric. 2010;13:278–88. doi: 10.3109/13697130903197479. [DOI] [PubMed] [Google Scholar]
- 40.Tristano AG. The impact of rheumatic diseases on sexual function. Rheumatol Int. 2009;29:853–60. doi: 10.1007/s00296-009-0850-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Differences in total and subscale scores on the General Sleep Disturbance Scale between women with and without breast pain. All values are plotted as means ± standard errors of the mean.
Differences in the total and item scores on the Sleep Interference Scale between women with and without breast pain. All values are plotted as means ± standard errors of the mean.
Differences in the fatigue and energy subscale scores on the Lee Fatigue Scale between women with and without breast pain. All values are plotted as means ± standard errors of the mean.


